1Professor, Department of Prosthetic Dental Sciences, College of Dentistry,
King Saud University, Riyadh, Saudi Arabia.
2Professor, Discipline of prosthodontics, Faculty of Dentistry, University of Toronto, Toronto, Canada.
3Assistant professor, Department of Prosthetic Dental Sciences, College of Dentistry,
King Saud University, Riyadh, Saudi Arabia.
4Private Practice, Riyadh, Saudi Arabia.
5Postgraduate student, Doctorate Program of Restorative Dental Sciences,
College of Dentistry, King Saud University, Riyadh, Saudi Arabia.
6Associate professor, Department of Prosthetic Dental Sciences, College of Dentistry,
King Saud University, Riyadh, Saudi Arabia.
Corresponding author email: saltaweel@ksu.edu.sa
Article Publishing History
Received: 13/07/2020
Accepted After Revision: 23/09/2020
A knowledge of color and surface roughness of denture base materials is important for achieving clinically successful complete dentures. The aim of this study was to evaluate the effects of different salivary pH values on color stability and surface roughness of heat cured, light cured and CAD/CAM fabricated denture acrylic resin materials. Thirty discs with dimensions of (10 × 3 mm) were fabricated from heat-cured, light-cured, and CAD/CAM denture acrylic resin materials. The color (ΔE) and surface roughness (Sa) were measured prior to the conduction of the experiment and after 30 days immersion in saliva using a Reflectance Spectrophotometer and non-contacting Profile-meter, respectively. All the acrylic resin specimens were subjected to brushing and thermocycling according to a standardized protocol. The discs of each type of acrylic resin materials were immersed and incubated in three different salivary pH values (acidic 5.7, neutral 7 and basic 8.3) for 30 days. Results were analyzed by two-way ANOVA followed by independent sample t-test for comparison.
Both, the type of the acrylic resin material and the salivary pH value, have significant effects on color stability (ΔE) and surface roughness (Sa). Both heat cured and CAD/ CAM fabricated acrylic resin materials exhibited clinically acceptable color values (ΔE 3.3) after being subjected to acidic saliva pH (ΔE = 7.29). CAD/CAM fabricated acrylic resin material exhibited the least amount of surface roughness following incubation in different salivary pH values. The study concluded that CAD/CAM fabricated denture acrylic resin material might be the material of choice to construct dentures for patients known to have acidic dietary intake. It demonstrated clinically acceptable color stability and lower surface roughness values in comparison to the other denture acrylic resin materials.
Color Stability, Denture Acrylic Salivary pH, Surface Roughness.
Alfadda S. A, Al-Otaibi H. N, Al-Shaalan N. S, Al-Qarni R, AlMutairi R. M, Al-Taweel S. M, AlFouzan A. The Effects of Salivary pH on Color Stability and Surface Roughness of Different Denture Acrylic Resin Materials. Biosc.Biotech.Res.Comm. 2020;13(3).
Alfadda S. A, Al-Otaibi H. N, Al-Shaalan N. S, Al-Qarni R, AlMutairi R. M, Al-Taweel S. M, AlFouzan A. The Effects of Salivary pH on Color Stability and Surface Roughness of Different Denture Acrylic Resin Materials. Biosc.Biotech.Res.Comm. 2020;13(3). Available from: https://bit.ly/2XmgyH0
Copyright © Alfadda et al., This is an open access article distributed under the terms of the Creative Commons Attribution License (CC-BY) https://creativecommons.org/licenses/by/4.0/, which permits unrestricted use distribution and reproduction in any medium, provide the original author and source are credited.
INTRODUCTION
Complete dentures can be fabricated using different methods. The goal of each method is to produce a prosthesis that shows excellent mucosal adaptation resulting in good retention and stability (Bilgin et al., 2015). Polymethyl methacrylate (PMMA) resin has been successfully used for dentures base materials for many years, due to low cost, good physicochemical properties and acceptable esthetics. Moreover, it is easily processed, repaired and polished (Singh et al., 2013; Zuo et al., 2016).With the development of computer assisted design and computer assisted manufacturing (CAD/CAM) technology, complete dentures can be fabricated without the need for flasking or other processing methods. Additionally it has desired outcomes and great accuracy of fitting (Kattadiyil et al., 2015; Goodacre et al., 2016; Wimmer et al., 2016).
Regardless of the fabrication technique used acrylic resin susceptible to many environmental factors, which may compromise its properties. These factors include temperature changes, humidity, and saliva. Salivary pH changes had been one of the main concerns in field of removable dental prosthesis (Muddugangadhar et al., 2015; Sonthalia et al., 2016; Tango et al., 2018).
The effects of the aforementioned factors on color stability of denture acrylic resin materials were well-established by Liberman et al., (1995) with color stability of dental prosthesis being a concern as it is related closely to aesthetics and patient satisfactions. The color of denture base materials should remain stable during clinical service and any changes in denture base materials color are an indicator of aging and material damage. The color stability of acrylic resin denture base and teeth by different beverages has been investigated (Mutlu-Sagesen et al., 2001; Imirzalioglu et al., 2010; Altinci and Durkaya, 2016; Alp G et al., 2019; Al-Qarni et al., 2020).
The surface roughness (Sa) of denture base materials is affected by material properties, polishing techniques and the dental hygiene habits of patients. The Sa has an impact on patient comfort and esthetics and play a key factor in plaque accumulation that leads to denture stomatitis, staining and halitosis (Kuhar et al., 2005; Mörmann et al., 2013; Gungor H et al., 2014; Sahin et al., 2016; Darwish et al., 2016; Alp G et al., 2019).
Since complete dentures are often subjected to oral saliva with alternating states of alkalinity to acidity, studying the potential effects of the salivary pH on the properties of the acrylic resin is essential. Although the color stability and surface roughness of heat cured and light cured denture base materials have been reported studies of the color changes and surface roughness of CAD/CAM denture base materials are insufficient. The null hypothesis was that different salivary pH values have no effects on color stability, surface roughness of various types of denture acrylic resins materials.
MATERIAL AND METHODS
Three types of denture acrylic resin materials were utilized in this study; Heat cured (SR Ivocap High Impact®, IvoclarVivadentAG, Liechtenstein), Visible-light-activated resin (Eclipse®, Dentsply, United State), and CADCAM fabricated denture acrylic resin materials (IvoBase® CAD, Zenotec,Wieland Dental, Germany). Three groups of thirty discs each were fabricated with dimensions of 10 mm (diameter) × 3 mm (thickness). Each of the three groups was divided into three subgroups, with 10 discs each.
Acrylic Samples preparation :Fabrication of CADCAM denture acrylic resin discs:
The discs were designed and milled using Zenotec® CAD software (Wieland Digital Denture Ivoclar Vivadent, Schaan, Liechtenstein) according to the predetermined dimensions. Poly methyl methacrylate (PMMA) blocks were used. The discs were then finished and polished using dental laboratory polishing machine with vacuum cleaner (ASPYCLEAN+ M2V®, Manfredi, Italy) with the use of Pumice (Pumice, INTERDENT, Slovenia) and rag polishing wheel (Rag Muslin wheel , Kerr, USA).
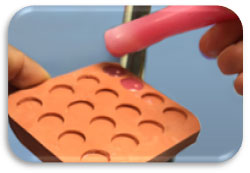
Fabrication of heat cured denture acrylic resin discs: A putty mold of the preferred disc dimensions was fabricated using putty polyvinyl siloxane material (Express STD®, 3M ESPE, United State). The silicone molds were filled by melted base plate wax (Figure 1). A Bantam flask was filled up with a plaster mix and then the putty mold was immersed. After that the flasks were placed in a wax elimination machine for 30 minutes at 90 -100 F◦. The heat cured denture acrylic resin was then mixed for 5 minutes using a cap vibrator (Cap vibrator®, Ivoclar Vivadent, Schaan, Liechtenstein). The mixture was poured into the putty mold and pressed using pressure apparatus (OL 463, Manfredi, Italy). Then, the Flask assembly was placed in a polymerization path (100 C water) for 35 minutes (Electronic Denture Curing System, NevinLabs™, USA ).The discs were finished and polished on the same manner.
Figure 1: The mold filled up with melted base plate wax.
Fabrication of visible-light-activated denture acrylic resin discs:The putty mold made of polyvinyl siloxane material (Express STD®, 3M ESPE, United State) was used to fabricate the light cured acrylic resin discs. According to the manufacturer’s instructions, a thin layer of separator was painted on the mold’s surface and a small amount of visible light activated denture acrylic resin (Eclipse, dentsply, United State) was placed into the disc’s mold. A thin layer of Eclipse Air Barrier (Eclipse Air Barrier Coating, DENTSPLY, USA) was applied to the top of the discs. The discs were then placed in the Eclipse Processing Unit for 10 minutes at +140 F◦, and then it was allowed to bench cool at room temperature. Then, the discs were polished on the same manner.
Measurement of color stability: Reflectance spectrophotometer (color-Eye 7000A®, Gretag Macbeth, NY, USA) was used for the color stability measurements of all the samples before and after incubating the discs in different pH values of artificial saliva. Color reading was performed using an 8-degree observer and illuminant D65. Color stability assessments were conducted in three randomly selected areas near the center of each acrylic sample. The average of the three readings was recorded and the mean color change of each sample was calculated using the CIE Lab uniform color scale. The level of the total color difference was formulated by a single number ΔE.
ΔE=[(ΔL*)2+(Δa*)2+(Δb*)2]1/2ΔE=(ΔL*)2+(Δa*)2+(Δb*)21/2
Where L* stands for lightness, a* for redness-greenness, and b* for yellowness–blueness (Asal et al., 2015).
Measurement of surface roughness:The surface roughness of the denture acrylic resin samples was determined with a non-contacting profile-meter (3D Opticalmicroscope contour GT-K1®, Bruker, United State). A 3D parameters of surface roughness with total of three readings were taken for each sample. The average of three readings of arithmetic mean height (Sa) was recorded in micrometers and the mean surface roughness change of each sample was obtained.
Brushing protocol of the samples:The mechanical brushing test was performed following the recommendations of the International Organization for Standardization (2001). The specimens were brushed with soft tooth brushes mounted on a toothbrush simulator (toothbrush simulator ZM-3.12, SD Mechatromik GmbH,Germany) then the specimens were subjected to linear toothbrush abrasion movement with a rate of 356 brush strokes (back and forth) per minute. The machine provides a 200 g vertical load over each specimen and 5mm path starting from center of each specimen. The total brushing time was 50 minutes with total of 17800 cycles (representing one year). Brushing was carried out in distilled water (23+3 C0) and dentifrice (Crest Cavity Protection Regular Paste, P&G, Germany) (Hussein and Al-Ameer, 2012).
Artificial saliva preparation and incubation of the samples: The artificial saliva was prepared in three different pH values (5.7, 7 and 8.3). An electrolyte composition similar to that of human saliva was used in this study (Pusz et al., 2010). This included the followings:
| Na2HPO4 | 0.260g/l |
| NaCl | 0.700g/l |
| KSCN | 0.330g/l |
| KH2PO4 | 0.200g/l |
| NaHCO3 | 1.500g/l |
| KCl | 1.200g/l |
Buffer solution from KH2PO4 and Na2HPO4 was prepared by dissolving each one in 1 liter of de-ionized distilled water. Basic saliva was prepared by taking 500 ml of Na2HPO4 and adding KH2PO4 gradually to it until the exact pH was reached.
Neutral and acidic saliva were prepared by slightly adding of Na2HPO4 to 500 ml of KH2PO4 until the exact pH was reached. For neutral saliva, greater amount of Na2HPO4 were added to reach the exact pH (Kostić et al., 2015).The discs were assorted into 9 groups, with 10 discs in each group, then stored in the artificial saliva in an incubator (blanket warming cabinet, MALMET, Australia) at 37oC for a total of 30 days.
Thermo-cycling protocol:Using SD Mechatronik GmbH thermo-cycler (SD Mechatronik, Germany), all specimens were stored in distilled water, going through thermo-cycling between 5 0C and 55 0C with a dwell time of 30 seconds, and a transfer time of 12 seconds for 1000 cycles (Oliveira et al., 2010).Data were analyzed using statistical software SPSS (v16, SPSS Inc., Chicago, IL, USA). The effect of acrylic material type and pH values and the interaction between them on color changes and surface roughness were analyzed using two-way ANOVA. Paired sample t-test was used to examine the difference between the pre and post color and surface roughness of all the acrylic material types.
RESULTS AND DISCUSSION
The Effects of pH Value on Post color stability on different denture acrylic resin materials:Two-way ANOVA was used to evaluate the effects of acrylic material type and salivary pH value on ΔE, and it was found that each independent factor had a significant effect on ΔE (Table 1).
Table 1. Two way ANOVA of the effect of two independent variables material type and pH value on ΔE
| Source | Type III Sum of Squares | df | Mean Square | F | Sig. |
| Acrylic disc material | 819.8 | 2 | 409.90 | 156.07 | .000 |
| PH | 117.45 | 2 | 58.72 | 22.36 | .000 |
| Acrylic disc material * pH | 120.50 | 4 | 30.13 | 11.47 | .000 |
| Error | 1394.60 | 531 | 2.63 | ||
| Total | 6840.60 | 540 | |||
| Corrected Total | 2452.35 | 539 |
a R Squared = .431 (Adjusted R Squared = .423)
The mean and standard deviation of each material when soaked in different salivary pH values are presented in (Table 2). When acrylic materials were soaked in acidic pH, the post ΔE of the CAD/CAM and Light Cure materials were higher than the pre ΔE (1.56 ± .56, 7.29 ± 3.14 respectively), while the pre ΔE of the Heat cure was higher than the post ΔE (3.07 ± 1.23).
Table 2. Difference of ΔE of different acrylic material after soaking in different pH values
| pH | Acrylic disc material | ΔE | Mean | Std. Deviation |
| Acidic | CAD/CAM | Pre | 1.49 | .61 |
| Post | 1.56 | .56 | ||
| Heat Cure | Pre | 3.07 | 1.23 | |
| Post | 2.94 | 1.39 | ||
| Light Cure | Pre | 4.66 | 1.87 | |
| Post | 7.29 | 3.14 | ||
| Neutral | CAD/CAM | Pre | 1.35 | .85 |
| Post | 1.23 | .58 | ||
| Heat Cure | Pre | 2.59 | 1.29 | |
| Post | 2.80 | 1.43 | ||
| Light Cure | Pre | 4.28 | 2.33 | |
| Post | 3.42 | 2.25 | ||
| Basic | CAD/CAM | Pre | 1.86 | .78 |
| Post | .82 | .93 | ||
| Heat Cure | Pre | 2.57 | .78 | |
| Post | 2.62 | 1.64 | ||
| Light Cure | Pre | 4.28 | 1.31 | |
| Post | 2.47 | 1.62 |
When the different acrylic materials were soaked in saliva of neutral pH value, the pre ΔE of CAD/CAM and light cure materials were higher than post ΔE (1.35 ± 0.85, 4.28 ± 2.33), while the post ΔE of Heat Cure was higher than the pre ΔE (2.80 ± 1.43). The same pattern was observed when the materials were soaked in saliva of basic pH value (the pre ΔE of CAD/CAM and light cure materials were higher than post (1.86 ± 0.78, 4.28 ± 1.31 respectively), and the post ΔE of the Heat Cure material was higher than pre (2.62 ± 1.64). The independent sample t-test revealed that those differences were found to be statistically significant only in the light cure material when soaked in saliva of acidic pH, and in the CAD/CAM and light cure materials when soaked in saliva of basic pH value (p ≤ 0.05) as shown in (Table 3).
Table 3. Independent Sample T-test between the pre and post ΔE of different acrylic materials under different salivary pH values.
| pH | Acrylic Disc material | |||||
| T-test for Equality of Means | ||||||
| t | df | Sig. (2-tailed) | Mean Difference | |||
| Acidic | CAD/CAM | ΔE | -.48 | 58 | .64 | -.07 |
| Heat Cure | ΔE | .40 | 58 | .70 | .144 | |
| Light Cure | ΔE | -3.94 | 58 | .00* | -2.63 | |
| Neutal | CAD/CAM | ΔE | .64 | 58 | .53 | .12 |
| Heat Cure | ΔE | -.58 | 58 | .56 | -.20 | |
| Light Cure | ΔE | 1.47 | 58 | .15 | .88 | |
| Basic | CAD/CAM | ΔE | 4.67 | 58 | .00* | 1.04 |
| Heat Cure | ΔE | -.16 | 58 | .89 | -.05 | |
| Light Cure | ΔE | 4.79 | 58 | .00* | 1.81 | |
* The mean difference is significant at the .05 level.
The effects of pH value on post surface roughness under different types of denture acrylic resin materials:Two-way ANOVA was used to evaluate the effect of acrylic material type and salivary pH value on Sa, and it was found that each independent factor had a significant effect on surface roughness (Table 4).
Table 4. Two way ANOVA of the effect of two independent variables material type and pH value on Sa values
| Source | Type III Sum of Squares | df | Mean Square | F | Sig. |
| Corrected Model | 233.67(a) | 8 | 29.21 | 158.15 | .00 |
| Intercept | 261.89 | 1 | 261.89 | 1418.02 | .00 |
| Disc material | 230.32 | 2 | 115.16 | 623.55 | .00 |
| pH | 1.25 | 2 | .63 | 3.39 | .04 |
| Disc material * pH | 2.1 | 4 | .52 | 2.84 | .02 |
| Error | 98.07 | 53 | .19 | ||
| Total | 593.63 | 54 | |||
| Corrected Total | 331.74 | 54 |
a R Squared = .704 (Adjusted R Squared = .700)
The mean and standard deviation of Sa of each material when soaked in different salivary pH values are presented in (Table 5). When acrylic materials were soaked in acidic pH, the pre Sa of the Heat cure and CAD/CAM materials were higher than the post Sa (1.59 ± .67, .18± .03 respectively), while the post Sa of the Light cure was higher than the pre Sa (.34±.24). The same pattern was observed when the materials were soaked in saliva of Neutral pH value, the pre Sa value of Heat cure and CAD/CAM materials were higher than post Sa (1.86±.57, .18±.03 respectively), and the post Sa value of the Light cure material was higher than pre Sa (.34± .15). When the different acrylic materials were soaked in saliva of Basic pH value, the pre Sa value of heat cure, light cure and CAD/CAM materials were higher than the post Sa (1.78±.63, .29±.08, .19±.03 respectively).
Table 5. Difference of Surface roughness of different acrylic material after soaking in different pH values
| pH | Acrylic disc material | SR | Mean | Std. Deviation |
| Acidic | CAD/CAM | pre | .18 | .03 |
| post | .15 | .03 | ||
| Heat Cure | pre | 1.59 | .67 | |
| post | 1.51 | .61 | ||
| LIGHT Cure | pre | .30 | .14 | |
| post | .34 | .24 | ||
| Neutral | CAD/CAM | pre | .18 | .03 |
| post | .15 | .02 | ||
| Heat Cure | pre | 1.86 | .57 | |
| post | 1.75 | 1.1 | ||
| Light Cure | pre | .29 | .11 | |
| post | .34 | .15 | ||
| Basic | CAD/CAM | pre | .19 | .03 |
| post | .16 | .03 | ||
| Heat Cure | pre | 1.78 | .63 | |
| post | 1.21 | .59 | ||
| Light Cure | pre | .29 | .08 | |
| post | .26 | .07 |
The independent sample t-test revealed that those differences were found to be statistically significant only in the CAD/CAM material when soaked in acidic, neutral and basic saliva, and in the Heat cure material when soaked in basic saliva (p ≤ 0.05) (Table 6).
Table 6. Independent Sample T-test between the pre and post Surface roughness of different acrylic materials under different salivary pH values.
| pH | Acrylic disc material | T-test for Equality of Means | ||||
| t | df | Sig. (2-tailed) | Mean Difference | |||
| Acidic | CAD/CAM | Sa | 4.35 | 58 | .00* | .03 |
| Heat Cure | Sa | .44 | 58 | .66 | .07 | |
| Light Cure | Sa | -.63 | 58 | .53 | -.03 | |
| Neutral | CAD/CAM | Sa | 5.11 | 58 | .00* | .04 |
| Heat Cure | Sa | .48 | 58 | .63 | .11 | |
| Light Cure | Sa | -1.24 | 58 | .22 | -.04 | |
| Basic | CAD/CAM | Sa | 2.45 | 58 | .02* | .02 |
| Heat Cure | Sa | 3.62 | 58 | .00* | .57 | |
| Light Cure | Sa | 1.14 | 58 | .26 | .02 | |
* The mean difference is significant at the .05 level.
Based upon the results obtained from this study, the null hypothesis was rejected, meaning that the variation in salivary pH values had a significant effect on color stability and surface roughness of the acrylic materials used in the study. Acrylic resin is one of the most popular and extensively used materials in different fields of medicine, especially in dentistry with prosthetic replacement and rehabilitation of missing structures being one of the main benefits gained from this material (Wiatrak et al., 2017). Despite the wide use of acrylic materials, many environmental factors are known to have adverse effects on its physical properties and clinical performance. Salivary pH fluctuation is considered as one of the main factors that might affect the performance of intraoral prosthesis, (Haug et al., 1999a; Haug et al., 1999b; Eleni et al., 2009; Sonthalia et al., 2016).
Effects of Salivary pH Values Alteration on Color of Different denture Acrylic resin Materials:In the current study, color changes of CADCAM and heat cure acrylic materials were considered clinically acceptable (ΔE < 3.3) after subjected to 30 days of immersion in different salivary pH. This did not apply for light cure acrylic (ΔE > 3.3) after being subjected to acidic saliva pH (ΔE = 7.29). The effect of soaking the acrylic materials in acidic solutions- not necessary saliva- were investigated previously. Khan et al., (1987) compared the staining ability of light-cure acrylic and heat-cure acrylic resins when soaked in tea (acid).
Their findings indicate that light-cure acrylic is 4 times more vulnerable to staining due to difference in water sorption between the two materials. Um and Ruyter, (1991) reported that coffee discoloration is due to both surface adsorption and absorption of colorants while with tea only adsorption of colorants was noticed. However, it is worth mentioning that these studies immersed the acrylic materials in colored solutions while in the current study clear artificial saliva was used. Similarly, our results were consistent with studies performed by Mutlu-Sagesen et al., (2001) and Koksal et al., (2008) who investigated the color stability of denture teeth when immersed in different solutions. Light cure acrylic material had the highest amount of color change when soaked in acidic saliva, which indicates that this material is least stable in the acidic environment.
Imirzalioglu et al., (2010) evaluated the effect of different solutions of different pH values on the color stability of acrylic resin. It was concluded that acidic solution such as coffee and tea showed the highest amount of color change. This was attributed to the unfavorable physical properties of the material where changes due to coffee (more acidic) were more than tea (weaker acid). On the contrary, another study that evaluated the effect of peracetic acid and sodium hypochlorite on acrylic resins, and found that there is no significant color changes irrespective of immersion time (Fernandes et al., 2013). However, this lack of difference was contributed to little immersion time/day and the short study period.
As stated before the color changes of CADCAM and heat cure acrylic materials were considered clinically acceptable (ΔE < 3.3) this finding coincide with (Altinci and Durkaya, 2016; Alp et al., 2019; Dayan et al., 2019; Al Qarni et al., 2010). On the other hand this was not apply for light cure acrylic (ΔE > 3.3) after being subjected to acidic saliva pH (ΔE = 7.29) (Koksal et al., 2008; Bonatti et al., 2009; Canadas et al., 2010; Goiato et al., 2013; Fernandes et al., 2013). From the perspective of color stability, CADCAM acrylic materials showed high level of color stability that indicate higher clinical performance in terms of color stability and probably more patient satisfaction, on the other hand, light-cure acrylic showed high level of color deterioration that renders it to be the last choice when seeking high esthetic and color stability over time.
Effects of Salivary pH Values Alteration on Surface Roughness of Different denture Acrylic resin Materials: In the current study, it was found that the surface roughness of heat cure acrylic material significantly increased when soaked in neutral and basic pH values. This could be attributed to the fact that the pH values can affect the degradation rates of the polymers where the breaking strength of the polymer was found to depend markedly on the pH and was found to be highest at neutral pH (Achim, 1996; Hussein and Al-Ameer, 2012)). It was found that in basic pH values there is high number of Hydroxyl ions, which is responsible for accelerating the degradation, thus increasing the surface roughness (Cilli et al., 2012).
Our results demonstrated that the surfaces of the CAD/CAM and light cure acrylic materials were the least affected by changes in the pH values, meaning that both materials’ surface roughness are resistant to environmental pH changes. According to Bagheri et al., (2007) the type of storage solution and the composition of the soaked material are important factors for the polymer degradation of the materials. Factors such as the solubility parameter, the cross-link nature of the resin matrix, and the solvent sorption uptake may influence more directly the polymer’s degradation rate.
Filler-Matrix de-bonding may occur in presence of water as diffusion of water occur at interface between filler particles and the matrix causing hydrolytic degradation and erosion of resin based material. Consequently, the combination of these factors may affect the wear undergone by the material (Ferracane, 2005; Cilli et al., 2012; Munchow et al., 2014). The ability of CAD/CAM to have smooth surfaces might be more material-related (Riccardo, 2016). Industrially fabricated CAD/CAM materials have a less risk of porosities and therefore higher mechanical properties (Stawarczyk et al., 2015).
The light cure acrylic material have the least favorable surface roughness in acidic and neutral pH values. This may be due to loss of structural ions that lead to softened of polymer surface (Gadelmawla et al., 2002). The low pH values can also change the urethane dimethacrylate resin matrix by acting as a catalyst for the ester groups that are present in dimethacrylate monomers. This process lead to a phenomenon known as plasticization formed due to degradation of the polymer network, that may increase the surface roughness of the resin (Ferracane, 2005; Miranda et al., 2011). Generally speaking, the CAD/CAM acrylic material demonstrated the best surface smoothness regardless of the salivary pH values it was soaked in.
To the contrary, heat cure acrylic material demonstrated the worst surface smoothness regardless of the soaking salivary pH value. It is known that the salivary pH value continuously alters in the oral cavity between acidic and basic based on the dietary intake of the patient. Consequently, it might be necessary to subject the same acrylic material to altered salivary pH values and study its effect on surface roughness and color stability.
CONCLUSION
Within the limitations of the current study, it can be concluded that CAD/CAM acrylic materials are best used in patients with acidic dietary intake. CAD/CAM acrylic material exhibited clinically acceptable color stability and the least amount of surface roughness in comparison to the heat and light cure acrylic materials. Based on the results of this study, further studies should be performed to address the effect of different polishing techniques on the color stability and surface roughness of denture base materials.
Conflict of interest: The authors declare that they have no conflict of interests for the present study and all authors have read and approved the final draft.
REFERENCES
Achim G, (1996). Mechanisms of Polymer Degradation and Erosion. Biomaterials. 17(2):103-114.
Alp G, Johnston WM, Yilmaz B, (2019). Optical properties and surface roughness of prepolymerized poly(methyl methacrylate) denture base materials. J Prosthet Dent. 121(2):347-352.
Altinci P and Durkaya P, (2016). Effects of thermocycling and various drinks on the color stability of heat-polymerized acrylic resin. J Istanb Univ Fac Dent. 50 (3): 15–20.
Al-Qarni F , Goodacre C J, Mathew T Kattadiyil M T, Nadim Z Baba N Z, Paravina R D, (2020). Stainability of acrylic resin materials used in CAD-CAM and conventional complete dentures. J Prosthet Dent. 123(6): 880-887.
Asal SA, Fahmi MF, Abdulla SM, (2015) Chromatic stability of light-activated resin and heat-cure acrylic resin submitted to accelerated aging. Saudi J Dent Res. 6(1):41-47.
Bagheri R, Tyas MJ, Burrow MF, (2007). Subsurface degradation of resin-based composites. Dent Mater. 23(8):944-951.
Bilgin MS, Erdem A, Aglarci OS, Dilber E, (2015). Fabricating complete dentures with CAD/CAM and RP technologies. J Prosthodont. 24(7):576-579.
Bonatti MR, Cunha TR, Regis RR, Silva-Lovato CH, Paranhos HF, de Souza RF, (2009). The Effect of Polymerization Cycles on Color Stability of Microwave‐Processed Denture Base Resin. J Prosthodont. 18(5):432-437.
Canadas MD, Garcia LF, Consani S, Pires-de-Souza FC, (2010). Color stability, surface roughness, and surface porosity of acrylic resins for eye sclera polymerized by different heat sources. J Prosthodont. 19(1):52-57.
Cilli R., Pereira JC, Prakki A, (2012). Properties of dental resins submitted to pH catalysed hydrolysis. J Dent. 40(12):1144–1150.
Darwish M, Nassani MZ, (2016). Evaluation of the Effect of Denture Adhesives on Surface Roughness of Two Chemically Different Denture Base Resins. Eur J Dent. 10(3): 321-326.
Dayan C, Guven MC, Gencel B, Bural C,( 2019). A Comparison of the Color Stability of Conventional and CAD/CAM Polymethyl Methacrylate Denture Base Materials. Acta Stomatol Croat. 53(2):158-167.
Eleni PN, Katsavou I, Krokida MK, Polyzois G, Gettleman L, (2009). Mechanical behavior of facial prosthetic elastomers after outdoor weathering. Dent Mater J. 25(12):1493-1502.
Fernandes FH, Orsi IA, Villabona CA, (2013). Effects of the peracetic acid and sodium hypochlorite on the colour stability and surface roughness of the denture base acrylic resins polymerised by microwave and water bath methods. Gerodontology. 30(1):18-25.
Ferracane JL, (2005). Hygroscopic and hydrolytic effects in dental polymer networks. Dent Mater. 22(3):211-222.
Gadelmawla ES, Koura MM, Maksoud TM, Elewa I.M, Soliman H.H, (2002). Roughness parameters. J Mater Process Technol. 123(1):133‑145.
Goiato MC, Dos Santos DM, Baptista GT, Moreno A, Andreotti AM, Bannwart LC, Dekon SF, (2013). Effect of thermal cycling and disinfection on colour stability of denture base acrylic resin. Gerodontology. 30(4):276-282.
Goodacre BJ, Goodacre CJ, Baba NZ, Kattadiyil MT, (2016). Comparison of denture base adaptation between CAD-CAM and conventional fabrication techniques. J Prosthet Dent. 116(2):249-256.
Gungor H, Gundogdu M, Duymus ZY, (2014). Investigation of the effect of different polishing techniques on the surface roughness of denture base and repair materials. J Prosthet Dent. 112(5):1271-1277.
Haug SP, Andres CJ, Moore BK, (1999a). Color stability and colorant effect on maxillofacial elastomers. Part III: weathering effect on color. J Prosthet. 81(4):431-438.
Haug SP, Moore BK, Andres CJ, (1999b). Color stability and colorant effect on maxillofacial elastomers. Part II: weathering effect on physical properties. J Prosthet Dent. 81(4):423-430.
Hussein YA, Al-Ameer SS, (2012). The influence of different pH of saliva and thermal cycling on the adaptation of different denture base materials. J Bagh College Dentistry. 24(3):47-53.
Imirzalioglu P, Karacaer O, Yilmaz B, Ozmen I, (2010). Color stability of denture acrylic resins and a soft lining material against tea, coffee, and nicotine. J Prosthodont. 19(2):118-24.
International Organization for Standardization. ISO/TS 14569-2:2001 Dental materials – Guidance on testing of wear – Part 2: Wear by two- and/or three body contact ISO, Geneva (2001).
Kattadiyil MT, Jekki R, Goodacre CJ, Baba NZ, (2015). Comparison of treatment outcomes in digital and conventional complete removable dental prosthesis fabrications in a predoctoral setting. J Prosthet Dent. 114(6):818-825.
Khan Z, von Fraunhofer JA, Razavi R, (1987). The staining characteristics, transverse strength, and microhardness of a visible light-cured denture base material. J Prosthetic Dent. 57(3):384-386.
Koksal T, Dikbas I, (2008). Color stability of different denture teeth materials against various staining agents. Dent Mater J. 27(1):139-144.
Kostić M, Krunić N, Najman S, Nikolić L, Nikolić V, Rajković J, Petrović M, Igić M, Ignjatović A, (2015). Artificial saliva effect on toxic substances release from acrylic resins. Vojnosanit Pregl. 72(10):899-905.
Kuhar M, Funduk N, (2005). Effects of polishing techniques on the surface roughness of acrylic denture base resins. J Prosthet Dent. 93(1):76-85.
Liberman R, Combe EC, Piddock V, Pawson C, Watts DC, (1995). Development and assessment of an objective method of colour change measurement for acrylic denture base resins. J Oral Rehabil. 22(6):445-449.
Miranda Dde A, Bertoldo CE, Aguiar FH, Lima DA, Lovadino JR, (2011). Effects of mouthwashes on Knoop hardness and surface roughness of dental composites after different immersion times. Braz Oral Res. 25(2):168‑173.
Mörmann WH, Stawarczyk B, Ender A, Ender A Sener B, Attin T, Mehl A,
(2013). Wear Characteristics of Current Aesthetic Dental Restorative CAD/CAM Materials: Two-body Wear, Gloss Retention, Roughness and Martens Hardness. J Mech Behav Biomed Mater. 20:113-125.
Muddugangadhar BC, Sangur R, Rudraprasad IV, Nandeeshwar DB, Kumar BH, (2015). A clinical study to compare between resting and stimulated whole salivary flow rate and pH before and after complete denture placement in different age groups. Indian Prosthodont Soc. 15(4):356-366.
Munchow EA, Ferreira AC, Machado RM, Machado RMRamos TS, Rodrigues-Junior SA, Zanchi CH, (2014). Effect of Acidic Solutions on the Surface Degradation of a Micro-Hybrid Composite Resin. Braz Dent J. 25(4):321-326.
Mutlu-Sagesen L, Ergün G, Ozkan Y, Bek B, (2001). Color stability of different denture teeth materials: an in vitro study. J Oral Sci. 43(3):193-205.
Oliveira JC, Aiello G, Mendes B, Urban V, Campanha N,Jorge J, (2010): Effect of storage in water and thermocycling on hardness and roughness of resin materials for temporary restorations. Materials Research. 13(3):355-359.
Pusz A, Szymiczek M, Michalik K, (2010). Ageing process influence on mechanical properties of polyamide – glass composites applied in dentistry. J Achiev Mater Manufact Eng. 38(1):49-55.
Riccardo FF: A study into mechanical, aesthetic and adhesive aspects of lithia silica-based glass ceramics. Università di Firenze, 2016.
Sahin O, Koroglu A, Dede DÖ, Yilmaz B, (2016). Effect of surface sealant agents on the surface roughness and color stability of denture base materials. J Prosthet Dent. 116(4):610-616.
Singh S, Palaskar JN, Mittal S, (2013). Comparative evaluation of surface porosities in conventional heat-polymerized acrylic resin cured by water bath and microwave energy with microwavable acrylic resin cured by microwave energy. Contemp Clin Dent. 4(2):147-151.
Sonthalia A, Chandrasekaran AP, Mhaske SP, Lau M, Joshy VR, Attokaran G, (2016). Comparative evaluation of effect of complete denture wears on the flow rate of saliva in both medicated and apparently healthy patients. J Int Soc Prev Community Dent. 6(3):219-223.
Sorgini DB, da Silva-Lovato CH, Muglia VA, de Souza RF, de Arruda CN, Paranhos Hde F, (2015). Adverse Effects on PMMA Caused by Mechanical and Combined Methods of Denture Cleansing. Braz Dent J. 26(3):292-296.
Stawarczyk B, Eichberger M, Uhrenbacher J, Wimmer T, Edelhoff D, Schmidlin PR, (2015).
Three unit reinforced polyetherketone composite FDPs: Influence of fabrication method on load-bearing capacity and failure types. Dent Mater. 34(1):7-12.
Tango RN, Arata A, Borges ALS, Costa AKF, Pereira LJ, Kaminagakura E, (2018). The Role of new removable complete dentures in stimulated salivary flow and taste perceotion. J Prosthodont. 27(4):335-339.
Um CM, Ruyter IE, (1991). Staining of resin-based veneering materials with coffee and tea. Quintessence Int. 22(5):377-386.
Wiatrak K, Morawiec T, Rój R, Mertas A, Machorowska-Pieniążek A, Kownacki P, Tanasiewicz M, Skucha-Nowak M, Baron S, Piekarz T, Wrzoł M, Bogacz M, Kasperski J, Niedzielska I, (2017). Oral Health of Patients Treated with Acrylic Partial Dentures Using a Toothpaste Containing Bee Product. Evid Based Complement Alternat Med. 2017.
Wimmer T, Gallus K, Eichberger M, Stawarczyk B, (2016). Complete denture fabrication supported by CAD/CAM. J Prosthet Dent. 115(5):541-546.
Zuo W, Feng D, Song A, Gong H, Zhu S, (2016). Effects of organic-inorganic hybrid coating on the color stability of denture base resins. J Prosthet Dent. 115(1):103-108.