Department of Pharmaceutics, Columbia Institute of Pharmacy, Tekari, Raipur, C.G. pin-493111
Article Publishing History
Received: 26/09/2016
Accepted After Revision: 25/11/2016
The present experimental study has been design with an aim to develop a phytoconstitute based mucoadhesive antifungal vaginal gel, for the management of wide range of fungal infections. All formulations were prepared by incorporating optimized concentration of curcumin along with fluconazole, to overcome the problem related to sensitivity of fluconazole on topical application. Different mucoadhesive polymers like carbopol P934, carbopol 940 and HPMC K4M either individually or in suitable combination were used to fabricate mucoadhesive gels. Essential in-vitro studies such as, screening of antifungal activity, rheological property, spreadibility, pH, Content uniformity, capacity of mucoadhesion, drug release etc. were performed to evaluate the performance of prepared gel in respect of safety and efficacy. Results of the study reveal a significant increase in antifungal activity of fluconazole. Among the different formulation batches, F5 & F8 showed significant mucoadhesive property, spreadibility and In-Vitro release pattern as compare to others and at the same time no sign of irritation were observe. On the basis of results it can be concluded that prepared formulations satisfactorily fulfill the desire need as an antifungal vaginal formulation
Roy A, Choudhury A, Bahadur S, Saha S. Phytoconstituent Based Mucoadhesive Antifungal Vaginal Formulation: An Effective and Innovative Approach. Biosc.Biotech.Res.Comm. 2016;9(4).
Roy A, Choudhury A, Bahadur S, Saha S. Phytoconstituent Based Mucoadhesive Antifungal Vaginal Formulation: An Effective and Innovative Approach. Biosc.Biotech.Res.Comm. 2016;9(4). Available from: https://bit.ly/2qzNqPf
INTRODUCTION
Since last few decade fungal infections are very common in all age group patients, but recently its occurrence has increased significantly (Sharma et al., 2010, Choudhury A et al., 2016). Among different fungal infections caused by Candida albicans (C. albicans) namely, oral, rectal or vaginal candidiasis is reported to be most common in human (Kuleta et al. 2009). Approximately 75% women population experience vaginal candidiasis during their whole life and about 40% to 50% of them experience multiple episodes (Choudhury et al., 2011; Choudhury et al., 2014). These infections have an unacceptably high mortality rate may be due to several reasons like, immunological state of the patient, restricted number of commercially available antifungal drugs with many side effects, Delay in diagnosis of the infection and/ or the drug resistance of the therapeutic agents (Martins
et. al., 2009). Therefore, this challenging clinical issue is required to be addressed on priority basis.
In most of the cases it was found that both systemic and topical antifungal therapies are required for effective management of Candida infections.(Hemaiswarya et al. 2008) Fluconazole is reported to be most effective molecule for the treatment of virginal candidiasis, (Tsao et al., 2000) however it shows serious sensitivity issue, when applied topically at high concentration. Again in several cases a high risk of development of fungal resistance was also observed (Annette et al., 2014), and on the other hand if it is introduce in the formulation in very low concentration perhaps may fail to fulfil the desired needs. (Oelkrug et al., 2014).
Therefore, there is an urgent need to establish an alternative way not only to make the existing molecule like fluconazole as effective as they were, rather to make them therapeutically more effective and safe too. Natural products are reported as attractive prototypes for this purpose due to their broad spectrum of biological activities. The promising results of antimicrobial activity of curcumin, a natural compound found in the Curcuma longa plant, active against different bacteria, fungi and parasites, made it a good candidate to enhance the inhibitory effect of existing antimicrobial agents through synergism (Sharma et al., 2009). Curcumin reported to have significant inhibitory effect against Candida albicans due to its membrane-lytic activities as well as the capacity to prevent the adhesion on host epithelial cell (Shyh et al., 2000). On the other hand, popular antifungal are belongs to azoles category mainly works based on the mechanism of target heme protein, cytochrome P450 (Jana et al., 2006 Grossman et al., 2015). Therefore it is expected that, a twofold effect of curcumin and fluconazole combination may improve the therapeutic efficacy against Candida albicans infection.
Therefore, this research work has been designed with a primary objective to improve efficiency of fluconazole against Candia albican and develop a safe and effective antifungal mucoadhesive vaginal gel formulation for the management of wide range of fungal infections. An antifungal screening study has been carried out to establish suitable combination of Curcumin and fluconazole. Mucoadhesive gels were prepared incorporating optimized drug combination using different ratios of polymers like HPMC, Carbopol P934 and Carbopol 940. All the prepared formulations were submitted for different In-vivo and In –vitro evaluation and final formulation was selected based on resultant data.
MATERIAL AND METHODS
Materials
The pathogenic antifungal stain of Candida albicans (MTCC 227) was purchased from MTCC Chandigarh, Materials used for the experimental work such as; fluconazole was obtained as gift sample from Cadila Pharmaceutical ltd. India. Carbopol 940, Carbopol 934 and HPMC were purchased from S.D. fine Pvt. ltd., RPMI 1640 media was and 96 well plates purchased from sigma, Guar gum & Sodium CMC were purchased from loba chemie. Ltd., Triethanolamine & Glycerin was purchased from Loba Chemie Ltd. India.
Determination of minimum inhibitory concentration (MIC) & Fractional inhibitory concentration index (IFCI)
The MIC value of each APIs was evaluated using broth dilution methods as per standard guideline of NCCLS, M27. At first the Candida albicans (MTCC 227) strain was subculture in Sabouraud dextrose agar media to ensure purity and viability. After that a standard pathogenic cell suspension was prepared by suspending few colonies from a freshly prepared culture, in 5 ml of saline solution. Final inoculums of 4 x 106 cells per mL were prepared by vortexes the suspension for 30 sec followed by adjustment the transmittance as per McFarland standard. After that a standard sterile stock solution of fluconazole and curcumin, individually as well as in suitable combination were prepared. MIC value of individual drug and drugs combination was measured on the basis of difference in optical density, through 96 plate method (Mukherjee et al., 2015).
The effect of combination of fluconazole and curcumin was investigated based checkerboard experiments (Gomes et al., 2012; Odds et al., 2003). A 100μl aliquot of working cell suspension were placed into 96-well microtitre plate containing RPMI 1640 medium. Again different concentration of fluconazole and curcumin, alone as well as in combination were placed vertically and horizontally into the plates. Potentiality of combination was measured after proper incubation for 48 hours. The fractional inhibitory concentration index (FICI) value was calculated using the following equation (Gomes et al., Hemaiswarya et al., 2008).
FICI = FIC of curcumin + FIC of Fluconazole
Where,
FIC of curcumin = MIC of curcumin in combination with FLC/ MIC of curcumin alone,
FIC of fluconazole = MIC of fluconazole in combination with CUR / MIC of fluconazole alone.
FICI values= 0.5, represent synergistic interactions, 4.0 antagonistic effect and values in between these two represent no interaction
Preparation Of Mucoadhesive Gel
Mucoadhesive gels were prepared using different gel forming polymers namely Carbopal P943 Carbopol 940, Hydroxy-propyl-methyl cellulose either individual or in combination. Accurately weighted required quantities of polymers as well as selected antifungal combination were transferred to beaker containing desire quantity of hydro-alcoholic solvent system. Whole content were stirred for 5-10 min by means of magnetic stirrer and allowed to hydrate for 12 hours. After that a few drops of triethanolamine as neutralizing agent, glycerin as a moistening agent along with propylene glycol were added to the hydrated mass and mixed slowly with continuous gentle stirring by means of magnetic starrier until the homogenous gel were formed (Basha et al., 2011; Doaa et al., 2012 and Choudhury et al 2016).
Evaluation Of Prepared
Mucoadhesive Gel
Visual and Organoleptic Examination
The prepared gel formulations were visually inspected for their color and appearance. (Choudhury et al., 2016) It was found that gel formulations were slightly yellowish in color, free from any gritty particles and seems to be homogeneous
Compatibility Study
In this study physical mixture of individual drugs and all incorporated polymers in single as well as in combination were analyzed by means of FTIR study (Mekkawy et al2013). The major peaks found in physical mixture of drug with polymer are compared with the peak of individual APIs.
Spreadability Test
The test was performed as per (Doaa et al., 2012) using parallel plate method to determine the spreadability. The prepared formulations were placed in between a set of 20×20 cm glass slides & around 125 g weights were placed upon the upper slide to spread the applied gel uniformly. Then the weight was removed and the excess of gel adhering to the slide was scrapped off. The set of slides were fixed in such a way that only upper slide may slip off freely due to the weight tied with it. The time taken for the upper slide to separate from the lower slide was noted. The experiment was carried out three times and the average of three reading was recorded. Following formula was used for calculation-
S = M.L/T [Where, M = weight tied to upper slide; L = Length of glass slide; T = Time taken to separate the slide]
Percentage Yield
In this study weight of empty container as well as of gel formulation along with container was measured respectively. Then difference between the weight empty container and weight of container with gel formulation were measured, that considered as practical yield where as the total weight of each ingredient used in each formulation was considered as theoretical weight (Nayak
et al., 2010) The percentage yield was calculated using the formula as below-
Percentage yield
Percentage yield × 100
Percentage yield
Drug Content Determination
Around 10 gm of prepared gels were transferred into a 100ml volumetric flask containing 50ml of phosphate buffer pH 4.5., under continuous agitation for 5hr by means of mechanical rotary shaker. Further the mixture was kept aside for 24hrs in order to get complete release of drug from gel base. After that the content was filtered using Millipore filter (0.45μm) and absorbance was measured After suitable dilution using UV- visible spectrophotometer (UV – 1700, Shimadzu, Japan) at ëmax 260 nm and 422 nm respectively using buffer (pH 4.5) as blank (Choudhury et al., 2010; Choudhury et al. 2016) .
Determination of pH
The pH of gels was determined using a digital Electronic pH meter. Initially the pH meter was calibrated using standard buffers of pH 4, 7 and 9. Accurately 5 gm of gel was weighed and dispersed in 50 ml of double distilled water. The electrode of pH meter was dipped in dispersion and the numerical value displayed in pH meter was noted (Bachhav et al., 2009; Nayak et al., 2010).
Viscosity and Rheological Studies
The viscosity of gels was determined with the help of Brookfield viscometer (Enyyoyt et al., 2014) Formulations were placed in the sample holder and suitable spindle attached perpendicularly inside the sample. The spindle was attached to viscometer and allowed to rotate at a constant speed. The reading displayed on viscometer was measured.
| Table 1: Formulation design of Mucoadhesive vaginal gels | ||||||||||
| S. N | Materials | F1 | F2 | F3 | F4 | F5 | F6 | F7 | F8 | F9 |
| 1 | Carbopol 934 | 1 % | – | 0.5 % | 1 % | 1.5 % | – | – | – | |
| 2 | Carbapol 940 | – | – | 1% | – | – | – | 0.5% | 1% | 1.5% |
| 3 | HPMC | – | 1% | – | 1.5 % | 1 % | 0.5 % | 1.5% | 1% | 0.5% |
| 4 | Water | 90ml | 90ml | 90ml | 90ml | 90ml | 90ml | 90ml | 90ml | 90ml |
| 5 | Fluconazole | 0.125% | 0.125% | 0.125% | 0.125% | 0.125% | 0.125% | 0.125% | 0.125% | 0.125% |
| 6 | Curcumin | 0.62% | 0.62% | 0.62% | 0.62% | 0.62% | 0.62% | 0.62% | 0.62% | 0.62% |
| 7 | Ethanol | 5 ml | 5 ml | 5 ml | 5 ml | 5 ml | 5 ml | 5 ml | 5 ml | 5 ml |
| 8 | Propyl paraben | 0.08 % | 0.08% | 0.08 % | 0.08 % | 0.08 % | 0.08 % | 0.08% | 0.08 % | 0.08 % |
| 9 | Methyl paraben | 0.02 % | 0.02 % | 0.02 % | 0.02 % | 0.02 % | 0.02 % | 0.02 % | 0.02 % | 0.02 % |
| 10 | Glycerin | 5 ml | 5 ml | 5 ml | 5 ml | 5 ml | 5 ml | 5 ml | 5 ml | 5 ml |
| 11 | Triethanalamine | 0.18ml | 0.18ml | 0.18ml | 0.18ml | 0.18ml | 0.18ml | 0.18ml | 0.18ml | 0.18ml |
| *Above table shows the composition of different formulations along with the amount individual component in percentage basis. Where F1,F2, F3, F4, F5, F6, F7, F8 & F9 are considered as formulation codes, which represent individual combinations. | ||||||||||
Determination of mucoadhesion capacity
Pig vaginal mucosa was used as a model for mucoadhesion study. Samples from several newly Sacrificed animals were obtained from a local slaughterhouse. Vaginal mucosa was carefully separated from underlying tissues, washed with normal saline and cut in smaller pieces of adequate size. After that a single part of mucosal tissue was attached perfectly to the back side of owing balance such a way that it remain tightly attached till
the completion of study. To complete the study a glass slide was taken and required amount of formulated gels were spread over it in such a manner that may cover the whole area of mucosal tissue when come in contact together. The slide and the tissue attached in the pan were fixed for 1min. On the other hand of the pan a weight of 5gm was applied and determined the time taken by the tissue to detach from the glass slide were measured (Enyyoyt et al. 2014; Andrade et al. 2014; Neves et al. 2016).
| Table 2: FICI of Fluconazole and Curcumin combination | |||||
| Percentage of drug in combination
Fluconazole + Curcumin |
µg/ ml of drug in combination
Fluconazole + Curcumin |
FIC Fluconazole |
FIC Curcumin |
FICI |
Interaction |
| 75%MIC + 25% MIC | 36 + 6.25 | 0.22 | 0.42 | 0.642 | Antagonism |
| 75%MIC + 12.5% MIC | 36 + 3.12 | 0.20 | 0.39 | 0.591 | Antagonism |
| 75%MIC + 6.25%MIC | 36 + 1.56 | 0.38 | 0.73 | 1.11 | Antagonism |
| 50%MIC + 50%MIC | 24 + 12.5 | 0.31 | 0.60 | 0.91 | Antagonism |
| 50%MIC + 25% MIC | 24 + 6.25 | 0.28 | 0.53 | 0.81 | Antagonism |
| 50%MIC + 12.5% MIC | 24 + 3.12 | 0.26 | 0.51 | 0.77 | Antagonism |
| 25%MIC + 75%MIC | 12 + 1.56 | 0.22 | 0.43 | 0.65 | Antagonism |
| 75%MIC + 50% MIC | 12 + 6.25 | 012 | 0.24 | 0.364 | Synergistic |
| 25%MIC + 25% MIC | 12 + 3.12 | 0.15 | 0.30 | 0.452 | Synergistic |
| *Screening of FICI value based on antifungal activity study, using different ratios of curcumin and fluconazole. Concentration used for the development of ratios was as per the individual MIC value of both the component. | |||||
In-Vitro Drug Release Study
The apparatus consists of a glass cylinder with both the ends open, 10 cm in height, 3.8 cm in outer diameter and 3.2 cm in inner diameter was used as a permeation cell. A cellophane membrane previously soaked in distilled water for 24 hours was fixed to the one end of the cylinder. 10 mg of gel was taken in the cell (donor compartment) and the cell was immersed in a beaker containing 100 ml of buffer of pH 4.6 (receptor compartment). The whole assembly was fixed in such a way that the lower end of the cell containing gel was just touched (1-2 mm deep) to the diffusion medium, the medium in the compartment was agitated using a magnetic stirrer at the temperature 37±1ºC (Choudhury et al., 2016; Andrade et al. 2014). Sink condition were maintain throughout the experiment and after suitable dilution; the sample was analyzed by using Shimadzu UV visible spectrophotometer at 260nm and 422 nm respectively.
| Table 3: Result of physicochemical evaluation study of prepared gels. | ||||||
| Formulation code | Viscosity (Cp) | pH | Spreadibility (g.cm/sec) | Muco-adhesion (Dyne/cm2) | Percentage yield% | Drug content |
| F1 | 1300 ± 1.02 | 3.6 ± 0.037 | 0.166 ± 0.0012 | 12.4 ± 0.0387 | 92.59 ± 0.88 | 83 ± 0.645 |
| F2 | 3180 ± 0.90 | 4.05 ± 0.014 | 0.375 ± 0.0027 | 11.49 ± 0.025 | 91.82 ± 0.03 | 86 ± 0.810 |
| F3 | 1013 ± 1.18 | 4.27 ± 0.021 | 0.433 ± 0.0017 | 14.4 ± 0.2081 | 93.59 ± 0.093 | 81 ± 0.391 |
| F4 | 27400 ± 1.54 | 4.2 ± 0.029 | 0.576 ± 0.0018 | 19.06 ± 0.0095 | 93.25 ± 0.051 | 85 ±1.290 |
| F5 | 28350 ± 0.65 | 4.3 ± 0.057 | 0.30 ± 0.170 | 28.52 ± 0.029 | 96.00 ± 1.29 | 83 ±1.290 |
| F6 | 17800 ± 1.17 | 5.3 ± 0.180 | 0.26 ± 0.0250 | 17.92 ± 0.0216 | 98.53 ± 0.012 | 90 ±1.290 |
| F7 | 6400 ±1.35 | 4.2 ± 0.29 | 0.40 ± 0.182 | 18.24 ± 0.017 | 89.52 ± 0.015 | 87 ±1.290 |
| F8 | 52300 ±1.20 | 4.3 ± 0.22 | 0.4 ± 0.182 | 26.34 ± 0.066 | 98.51 ± 0.029 | 85 ±1.290 |
| F9 | 18300 ±1.38 | 3.91 ± 0.032 | 0.2 ± 0.129 | 15.62 ± 0.029 | 83.15 ± 0.031 | 94 ± 0.890 |
| *The above table contains result of essential evaluation parameters. All the data are represented in the format of (Mean ± Standard deviation). | ||||||
Vaginal irritation test
The primary vaginal irritation test was performed on New Zealand white female rabbit (1.5-2.5kg). All the animals were kept under standard laboratory condition. The total numbers of animals were divided into four batches, each batch containing three animals. 1ml of prepared gel was inserted daily, for 10 days, through a lubricated catheter into the vagina of rabbits (Mehta et al. 2012; Rabindranath et al., 2001). The external genitalia are observed regularly for any signs of oedema, erythema or discharge as a reaction to the exposure to the test materials. The experimental protocol of the study was approved by the Institutional Animal Ethics Committee (Regd. No. CIP / IAEC / 2013-14/044).
RESULTS AND DISCUSSION
In-Vitro antifungal effects of pure fluconazole and curcumin alone as well as in combination were tested against Candida albicans. The MIC value of fluconazole and currcumin alone was found 48ug/ml and 128ug/ml where as a remarkable fungal growth inhibition was observer when used in combination of both the APIs. To explore the finding, further the study was extended to determine the mechanism involved behind such effect. The study of fractional inhibitory concentration index shows that, when the curcumin and fluconazole added in suitable concentration results synergistic action as mentioned in (table no-02), which helps improve the potentiality of the combination and efficacy of fluconazole against pathogenic fungi.
The performance and safety issues related to prepared mucoadhesive vaginal gels were investigated on nine formulations based on different in-vitro and in-vivo parameters evaluation. As per visualization evaluation it was found that all the prepared mucoadhesive gel formulations were transparent, smooth, free from any grittiness and homogeneous in nature. The gel formulations were slightly yellowish in color with satisfactory yield value. Compatibility study was performed on physical mixture of APIs and polymer, which reflects no major shift or changes in peak value as well as their location (Fig-1.), hence indicate no interaction. All the prepared formulations reflect good spreadability, which indicate ease of application of formulations in the vaginal cavity. The pH of the prepared formulations were ranges within (3.5-5.3), which complies with pH of vaginal cavities, hence, consider suitable for vaginal application. Viscosity is considered as an important parameter for semisolid dosage form intended for vaginal delivery, since high viscous formulations will better adhere to the mucous wall hence, better will be the retention time. In this contest the viscosity of prepared formulations was found in the range of (1013-52300 Cp). The mark difference in the observed viscosity may be due to the difference in concentration used, again it has been observed that formulation fabricated with single polymer shown less viscosity than the combination of polymer. Among all, F5 and F8 formulation showed higher viscosity 28350cp, 52300cp respectively. The result of mucoadhesion study reflects that formulations F4, F5 & F8 shows higher mucoadhesion capacity as compare to others; in this connection this is to mention that good mucoadhesion property shall improve the residence time of inside vaginal cavity. It has been also notice that results mucoadhesion capacity directly related with viscosity and almost inversely related with spreadibility parameter of investigated formulations. Drug content study indicates that all the prepared formulation contains around 90-96% of drugs, which consider as a sign of good formulation. Results of the all the essential evaluation parameters are shown in (Table no-03)
 |
Figure 1: Graphical representation of FTIR study of pure drug and combination of drug and polymer represented as A, B, C respectively |
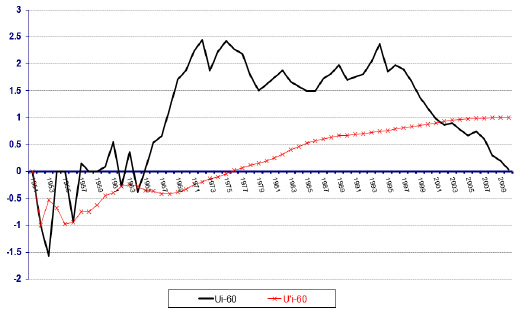 |
Figure 2: Graphical representation of drug release profile of all the prepared formulations |
On the basis of analysis of In-Vitro release data it was observed that almost all the formulation were showing 80-90% of drug release within 6-7 hrs. Clinical signs of irritation include the development of a rash, inflammation, swelling, scaling, and abnormal tissue growth in the affected area was not found after RVI test, that indicate the formulations were safe &free of any kind of irritation, hence, considered not produce any kind of discomfort to the patients during therapy as well as may improve patients compliance.
CONCLUSION
The investigation reveals that, incorporation of curcumin leads to increases the antifungal effect of fluconazole, which may be due to the mechanism synergism. Again the evaluation results of prepared mucoadhesive antifungal gels found to fulfill all the required criteria to be a suitable vaginal formulation. All the prepared formulations were found satisfy in respect of , formulation F5 and F8 shown better performance in respect of their mucoadhesion capacity, property of spreadibility and drug release study, that may facilitate the vaginal application and demand to increase poor patient compliance. The in vivo animal studies indicate no sign of irritation.
ACKNOWLEDGEMENTS
Author would like to acknowledge IPCA laboratories ltd. India for providing Fluconazole as drug sample and Columbia Institute of Pharmacy as research centre for providing the research facilities.
REFERENCES
Andrade O A, Parente E M, Ares G. Screening of mucoadhesive vaginal gel formulations. Braz J Pharm Sci 2014; 50(4): 931-942.
Annette W.F., Deanna A.S., McCarthy DI., Wiederhold N.P.(2014) Impact of New Antifungal Break points on Antifungal Resistance in Candida Species. Journal of Clinical Microbiology. Vol.52 No. 3. Pages 994–997
Bachhav.Y.G., Patravale. V B. (2009) Microemulsion based vaginal gel of fluconazole: formulation, in vitro and in vivo evaluation. International Journal of Pharmaceutics. Vol. 365. No.5. Pages 175–179.
Basha B.N., Kalyani P., Divakar G. (2011) Formulation and evaluation of gel containing fluconazole-antifungal agent. International journal of Drug Delivery Research. Vol.3. No.4. Pages 109-128
Choudhury A, Das S, Kar M.(2011) A review on novelty and potentiality of vaginal drug delivery. Int J Pharm Tech Res. Vol. 3. pages 1033-1044.
Choudhury A., Roy A., Saha S., Bahadur S. (2016) Preparation and evaluation of phytocontituent based mucoadhesive antifungal vaginal gel, Research Journal of Pharmacognosy and Phytochemistry. Vol 8. No.3. Pages 116-120
Choudhury. A., Verma. R., Sinha D., Sahu S., Roy. A. (2014) Development and characterization of topical phyto-formulation for antifungal activity. Vol. 1. No. 2. Pages 18-21
Doaa A.H., Dalia A.E., Sally A.H., Mohamed A.E. (2012) Formulation and evaluation of fluconazole topical gel. International journal pharmaceutical sciences. Vol. 4. No.5, 176-183
Enyyoyt A Z, Karavana Y S, Erac B, Gursel O, Lymoncu M H G, Baloðlu E. Evaluation of chitosan based vaginal bioadhesive gel formulations for antifungal drugs. Acta Pharmaceutica 2014; 64 (2): 139–156.
Gomes S. G., Curvelo J. A. R., Soares R. M. A., Pereira A.F.(2012) Curcumin acts synergistically with fluconazole to sensitize a clinical isolate of Candida albicans showing a MDR phenotype. Medical Mycology. Vol.50. Pages 26–32,
Grossman N.T., Pham C.D., Cleveland A.A., Lockhart S.R. (2015) Molecular mechanisms of fluconazole resistance in Candida parapsilosis isolates from a U.S. surveillance system. Antimicrobial Agents and Chemotherapy. Vol.59. No. 2. Pages 1030-1037.
Hemaiswarya S, Kruthiventi A.K., Doble M. (2008) Synergism between natural products and antibiotics against infectious diseases. Phytomedicine. Vol. 15. Pages 639–652
Jana C., Julius S. (2006) Resistance mechanisms in fluconazole-resistant Candida albicans isolates from vaginal candidiasis. International Journal of Antimicrobial Agents. Vol. 27 Pages 403–408.
Kuleta J.K, Kozik R.M, Kozik A.(2009) Fungi pathogenic to humans: molecular bases of virulence of Candida albicans, Cryptococcus neoformans and Aspergillus fumigatus. Acta Biochim Polon. vol.55 pages 211 – 224.
Martins C. V. B., DaSilva D. L., Neres A. T. M., Magalha T. F. F., Watanabe G. A., Modolo L.V., Sabino A.A., Fatima A.D, and Resende M.A. (2009) Curcumin as a promising antifungal of clinical interest. Journal of Antimicrobial Chemotherapy. Vol. 63. Pages 337–339
Mehta S, Verstraelen H, Peremens K, Villeirs G, Vermeire S. Vaginal distribution and retention of a multiparticulate drug delivery system assessed by gamma scintigraphy and magnetic resonance imaging. Int. J. Pharm 2012; 426: 44-53.
Mekkawy. A., Fathy M., Sohair E. S. (2013) Formulation and In vitro evaluation of fluconazole topical gels. Br J Pharm Res. Vol.3 No. 3. Pages 293-313.
Mukherjee P.K., Sheehan D.J., Hitchcock C.A., Ghannoum M.A.(2005) Combination treatment of invasive fungal infections. Clinical Microbiology Reviews. Vol.18 No.1. Pages163–194
Nayak. B.S., Rout P.K., Nayak. U. K., Bhowmik. B. B.(2010) Development and characterization of bioadhesive gel of microencapsulated metronidazole for vaginal use. Iranian Journal of Pharmaceutical Research. Vol. 9. No.3. Pages 209-219.
Neves J D, Bahia M F. Gels as vaginal drug delivery systems. Int. J. Pharm, 2006; 318: 1–14.
Odds F. C. (2003) Synergy, antagonism, and what the chequer board puts between them, Journal of Antimicrobial Chemotherapy Vol. 52. No.1. Pages 203
Oelkrug. C., Lange C.M., Wenzel E., Fricke S., Hartke M.(2014) Analysis of the tumoricidal and anti-cachectic potential of curcumin. Anticancer Research.Vol.34, pages 4781–4788.
Rabindranath P, Chakraborty M, Rabindra D, Gupta BK. In-vitro In-vivo correlation (IVIVC) study of leflunomide loaded microspheres. Int. J Pharm Sci 2009; 1: 165-170.
Roy A, Choudhury A, Nayak T.K. (2014) Importance and Utility of Vagina as a Route for Drug Delivery System. Asian J. Res. Pharm. Sci. Vol. 4: no. 2. Pages 86-92.
Sharma M, Manoharlal R, Shukla S, Puri N, Prasad T, Ambudkar S V., Prasad R. (2009) Curcumin modulates efflux mediated by yeast ABC multidrug transporters and is synergistic with antifungals, Antimicrobial Agents And Chemotherapy. Vol. 53, No. 8. Pages 3256–3265
Sharma M, Manoharlal Raman, Negi S.A., Prasad R. (2010) Synergistic anticandidal activity of pure polyphenol curcumin-I in combination with azoles and polyenes generates reactive oxygen species leading to apoptosis. FEMS Yeast Research. Vol.10. pages 570–578
Shyh M.T., Mei C. Y.(2000) Enhanced inhibitory effect from interaction of curcumin with amphotericin B or fluconazole against candida species. Journal of Food and Drug Analysis. Vol. 8. Pages 208-212.
Tsao S.M., Yin M.C., (2000) Enhanced Inhibitory Effect from Interaction of Curcumin with Amphotericin B or Fluconazole against Candida Species. Journal of Food and Drug Analysis. Vol. 8 No. 3. Pages 208-212


