1Prosthetic Department, College of Dentistry, King Khalid University, Abha, KSA
2Prosthodontic and Implant Consultant, Ministry of Health, Najran, KSA
3Department of Maxillofacial Surgery and Diagnostic Sciences, College of Dentistry, Jazan University, Jazan, KSA
4Prosthetic Dental Science Department, College of Dentistry, Jazan University, Jazan, KSA
5Department of Orthodontics, College of Dentistry, University of Hatay Mustafa Kemal, Antakya, Turkey
Corresponding author email: drmoaleem2014@gmail.com
Article Publishing History
Received: 03/01/2020
Accepted After Revision: 26/02/2020
The increasing number of partially dentated patients is the result of changes in the patterns of teeth loss and the ageing of the population. The extent and type of occlusal change may compromise the prostheses of the unopposed tooth and teeth bounding the extraction area. Undesirable tooth movements may be prevented. The purpose of this systematic review is to summarize the different techniques used for the management of unilateral or bilateral supraerupted tooth/teeth in the anterior/posterior and maxillary/mandibular regions. Electronic and manual searches were conducted by an independent reviewer to identify relevant articles, case reports, and case series published up to November, 2019. A pilot checklist consisting of 10 items was implemented to methodologically assess the relevant published studies. Only 30 studies and case reports were included after the exclusion of all irrelevant papers. The majority of cases were related to the supraeruption of maxillary teeth, whereas few cases were related to mandibular supraeruption, and only two cases were related to anterior maxillary and mandibular supraeruption. Most clinical cases of all types of teeth supraeruption were managed semi conservatively by mini-implants or miniscrews, and only a few cases were treated with endocrowns, ameloplasty, removable or fixed appliances, or nonconservative surgical orthodontics. Dentists will obtain a brief idea of the various treatment modalities for managing supraerupted tooth/ teeth discussed in this review.
Ameloplasty, Miniscrew implant, Supraerupted teeth, Teeth intrusion.
Al Ahmari N. M, Aldhalail M. A, Abidi N. H, Mohamed M. S, Alraawi M. A, Al Moaleem M. M. Techniques for Management of Supraerupted Teeth Prior to Prosthetic Treatment: Updated Review. Biosc.Biotech.Res.Comm. 2020;13(1).
Al Ahmari N. M, Aldhalail M. A, Abidi N. H, Mohamed M. S, Alraawi M. A, Al Moaleem M. M. Techniques for Management of Supraerupted Teeth Prior to Prosthetic Treatment: Updated Review. Biosc.Biotech.Res.Comm. 2020;13(1). Available from: https://bit.ly/2TV704J
Copyright © Al Ahmari et al., This is an open access article distributed under the terms of the Creative Commons Attribution License (CC-BY) https://creativecommons.org/licenses/by/4.0/, which permits unrestricted use distribution and reproduction in any medium, provide the original author and source are credited.
INTRODUCTION
If the extraction side is not restored immediately following tooth/teeth loss, the opposing dentition will erupt, and the vertical dimension for prosthetic treatment decreases (Ataoglu et al., 2002). In this case, securing insufficient intermaxillary space for either a fixed or removable prosthesis can be an extremely valuable point in establishing treatment plans (Ataoglu et al., 2002; Joshi et al., 2010).
Supraerupted posterior tooth/teeth are common clinical findings during daily dental practice. Postponing the replacement of the extracted tooth/teeth often leads to the extrusion of the opposing tooth/teeth into the edentulous space; this effect will lead to masticatory insufficiency and temporomandibular disorders. Re-establishing a functional posterior occlusion requires a comprehensive dental treatment plan when a fixed or removable prosthesis is planned for the opposing edentulous arch (Mahoorkar et al. 2010).
In adult patients, if the dentoalveolar extrusion is not severe, the space can be recaptured by performing coronoplasty and intentional endodontic treatment of the supraerupted tooth. When the extrusion is moderate, orthodontic intrusion can be conducted, and if the extrusion is severe, prosthetic rehabilitation is impossible and the removal of the teeth is often proposed (Mahoorkar et al., 2010; Shillingburg et al., 2012; Rosenstiel et al., 2015).
The teeth most likely to become unopposed, and therefore susceptible to supraeruption, are those occluding against edentulous parts. Clinically, the most commonly missing posterior teeth are the first permanent maxillary molars (Djemal et al., 2004; Basutkar et al., 2018; Prakash et al., 2014; Salazar et al., 2018; Al-Fraidi & Zawawi 2010) and teeth in the mandibular arch (Patil et al., 2016; Arslan et al., 2010; Tiago et al., 2016; Baeg et al., 2016), followed by the maxillary premolars (Djemal et al., 2004); the mandibular premolars are rarely missing. The mandibular posterior teeth are more likely to be extracted than the other teeth, and with increasing age, the posterior teeth are more likely to be extracted and lost bilaterally than the other types of teeth (Marcus et al. 1991; Meskin & Brown 1988). Other studies found that maxillary teeth are the most commonly extracted teeth (Craddock et al., 2007a).
The unopposed bilateral maxillary first molars in healthy mouths and in mouths with some periodontal pathology present were studied by Compagnon and Woda 1991. They found that the majority of supraeruption occurs in the early years following opposing tooth/teeth extraction. At later years, the loss of periodontal support may be superimposed on the area. However, in healthy individuals, the gingival margin remains at its original level on the tooth/teeth during occlusal tooth movements. After 10 years of remaining unopposed, periodontal migration reverses and root exposure occurs. This phenomenon was described as passive eruption (Craddock & Youngson 2004).
Most published articles related to the management of supraerupted teeth are mainly in a form of case reports, case series, or clinical and technical reports only. Thus, the aim of this review is to collect these publications in an organized manner and to simplify the methods or techniques for treating cases that may face similar conditions during daily dental practice.
Methodology for Data Collection: This review conformed to the PRISMA review protocol. The database of PubMed/Medline, ScienceDirect, and Scopus was searched using the terms “overerupted teeth, supraerupted tooth, treatment of overerupted teeth, case report, case series, review of literature.” The investigators then screened the titles, cases, and abstracts using English language. Studies that reported the treatment of overeruption through orthodontics only and did not mention prosthetic treatment were excluded. Case reports and case series were mainly shortlisted; full-text articles were then collected, and the same criteria were applied.
Related Definitions (GPT 9., 2017): The supraeruption or overeruption of tooth/teeth is defined as the movement of a tooth or teeth above the normal occlusal/incisal plane.
Occlusal analysis: A systematic examination of the occlusion with special consideration of the interocclusal relations of mounted casts.
Occlusal contact (deflective occlusal contact/initial occlusal contact): The touching of opposing teeth on the elevation of the mandible or any contact relation of the opposing teeth.
Coronoplasty, enameloplasty, or occlusal adjustment: Occlusal or aesthetic reshaping. It can be performed through occlusal correction, which is occlusal adjustment or reshaping.
Aesthetic reshaping: The physical modification of the surfaces of the teeth to improve appearance. These modifications can be performed through axial or occlusal reduction.
Crown lengthening: A surgical procedure designed to increase the extent of supragingival tooth structure for restorative or aesthetic purposes.
Crown–root ratio: The physical relationship between the portions of tooth not within the alveolar bone as determined by a radiograph compared with the portion of tooth within the alveolar bone.
Endocrowns: Indirect monoblock restorations that use the pulp chamber of the ETT for retention (Tzimas et al., 2018).
Osteotomy: The surgical cutting of a bone; this term is also frequently used to describe smoothing, leveling, or altering the external contours of the bone and may include alveolectomy and alveoplasty.
Posterior segmental osteotomy: A surgical procedure for drastically restoring previously diminished vertical dimension following the extraction of opposing molar/molars; dentists recommend this procedure as a treatment method to facilitate prosthetic restoration (Baeg et al., 2016).
Corticotomy: A selective alveolar bone cutting technique using ultrasonic bone surgery to enhance tooth movements (Grenga & Bovi 2013).
Objective of the Occlusal Management of Supraerupted Teeth: In general, all the needed diagnostic data must be prepared and ready for interpretation. These data include X-ray views (preapical, panoramic, and cephalometric). In addition, a maxillary and mandibular cast mounted on an appropriate articulator is necessary before designing the treatment plan needed for a particular case. The objectives of the treatment of supraeruption are as follows (Mahoorkar et al., 2010; Shillingburg et al., 2012; Rosenstiel et al., 2015):
- To direct the occlusal forces along the long axis of the teeth.
- To attain the simultaneous contact of all teeth in centric relation and maximum intercuspation.
- To eliminate any occlusal interference contact on inclined planes to enhance the positional stability of the teeth.
- To coincide centric relation with the maximum intercuspation position during different mandibular movements.
- To arrive at the occlusal scheme selected for a particular patient (Rosenstiel et al., 1998).
Prevalence of Supraerupted Teeth: Craddock et al. (2007a) stated that the average amount of overerupted tooth/teeth ranges from 1.68 mm to 3.99 mm of tooth/teeth without opposing, in which 1.03 and 1.91 mm were in mandible and maxilla, respectively. Kiliaridis et al. (2000) found that 24% of unopposed tooth/teeth had more than 2 mm of supraeruption among 82% of the examined subjects with unopposed tooth/teeth. A conclusion from another study stated that the occlusal change in unopposed teeth is mostly within 2 mm (Faggion et al., 2011).
Causes and Sequences of Supraeruption: Supraerupted posterior tooth/teeth are one of the most common clinical findings in dental practice. The delayed replacement of lost tooth/teeth often leads to the extrusion of the opposing teeth into the edentulous space; this effect leads to masticatory insufficiency and TMJ disorders (Mahoorkar et al., 2010). When the prosthesis is planned on the opposing edentulous area, re-establishing a functional posterior occlusion requires a comprehensive dental treatment plan. The tooth/teeth opposing the extracted sites are usually tilting lingually in the mandibular teeth and buccally in the maxillary teeth. In addition, the teeth adjusent to the extracted tooth/teeth usually drifted to the mesial and distal side. (Shillingburg et al., 2012; Rosenstiel et al., 2015). If the dentoalveolar extrusion is mild, the space can be recaptured by performing coronoplasty and intentional endodontic treatment of the supraerupted tooth. Orthodontic intrusion can be done when the extrusion is moderate, but if the extrusion is severe, prosthetic rehabilitation is impossible, and the removal of the teeth is often proposed (Shafad et al., 2017).
Prevention of Supraeruption: Supraeruption of tooth/teeth can be prevented by the light forces generated during chewing against an antagonist (Gierie et al., 1999). Thus, the replacement of the lost tooth/teeth with a fixed or removable prosthesis that prevents the overeruption of its antagonist is mandatory, and it should be fabricated before vertical movement had occurred (Davenport et al., 1988). Extraction is another option for dealing with an unopposed tooth, provided this tooth is not the key tooth for future restorative options (Kayser 1981). Solnit et al. (1988) demonstrated the use of an etched metal splint to bond the unopposed tooth to its adjacent opposed tooth. This approach may eliminate supraeruption provided that the bond between teeth remains intact. Jepson and Allen (1999) recommended the use of adhesive distal cantilever bridges to stabilize tooth position following tooth removal and to prevent undesirable eruptive movement.
Considerations during the evaluation of supraerupted tooth/teeth: (Craddock & Youngson 2004)
- Is the tooth a key for future prosthesis options?
- Has the tooth remained unopposed for a time without signs of supraeruption?
- Could the supraeruption of the tooth/teeth present prosthetic or occlusal difficulties?
- What is the overall state of the dentition?
- Patient preferences and tolerance in form of aesthetic considerations and the other planned restorative treatments for the unopposed tooth/teeth and the extracted spaces.
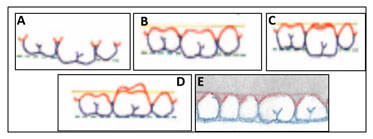
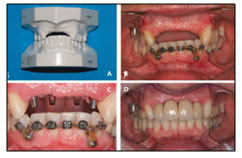
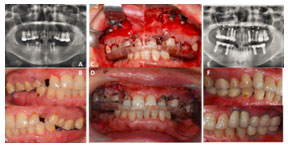
Classification of Supraerupted Teeth: Supraeruption can be classified according to the length of the overerupted tooth/teeth from the occlusal plane (Craddock & Youngson 2004; Graddock et al., 2007a; Carranza et al., 2018) into the following categories (Figs. 1A–1C): Mild, in which the supraerupted tooth extends between 0.1–1.5 mm; moderate, wherein the supraeruption of the occlusal surface is between 1.6–3.5 mm; and severe, wherein the amount of supraerupted tooth/teeth exceeds 3.5 mm in relation to the level of the occlusal plane.
Figure 1. Mild (A), Moderate (B), Severely overerupted teeth (C)
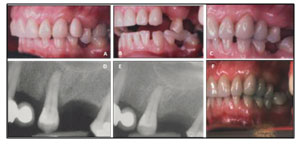
Moreover, supraerupted teeth can be classified in accordance with physiological changes in the position of the gingival margins. The appearance of supraeruption may have several components, including passive and active eruption, periodontal growth, or physiological wear. Compagnon and Woda (1991) described periodontal growth as passive eruption that is distinct from active eruption wherein the tooth/teeth is/are in continuous movement in an occlusal direction in the absence of periodontal growth. Periodontal growth is a process in which the attachment apparatus moves in an occlusal direction with the tooth, whereas in active eruption, the tooth erupts and the attachment apparatus comes to lie apically to its original position. Wear is a physiological sequence that occurs with increasing age (Craddock & Youngson 2004; Craddock et al., 2007a) (Figs. 2A–2E). When a tooth wears down, the occlusal level may remain constant with the alveolar bone becoming closer to the occlusal plane (Fig. 2E) as described by Compagnon and Woda 1991.
Figure 2. Modified classification of overerupted teeth. (A) Tooth erupted beyond the occlusal plane. (B) Gingival margins follow tooth eruption (periodontal growth). (C) Gingival margins remain at original level (active eruption). (D) Gingival margins recede, whereas the tooth remains parallel to the actual plane (passive eruption). (E) Gingival margins remain at the original level but occlusal wear is present (relative wear) (Compagnon & Woda 1991).
Techniques for the Management of Supraerupted Tooth/Teeth Prior to Prosthetic Treatment: Before any correction of supraerupted tooth/teeth, examination and diagnosis must be conducted throughly. A diagnostic cast or model should be made then mounted on an articulator using facebow transfer, and a trial adjustment of occlusion on cast should be done first. Many materials, including occlusal registration strips, occlusal indicator wax, marking ribbon, articulating papers, and T-scan, can be used to examine, diagnose, and detect occlusal interferences (Mahoorkar et al. 2010; Shillingburg et al 2012; Rosenstiel et al., 2015).
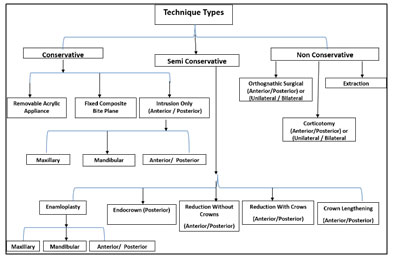
Supraerupted tooth/teeth are preferably adjusted after the treatment of an existing disease, such as gingival inflammation, healing of a pathogenesis, and treatment of trauma from occlusion (Carranza et al., 2018; Rosenstiel et al., 2015). Treatment modalities differ and depend on whether the supraeruption involves a single tooth or a group of teeth, whether it is unilateral or bilateral or in the maxillary or mandibular arch, and on the degree or amount of the occlusal/incisal supraeruption (Basutkar et al., 2018). The types and techniques for the treatment of supraerupted teeth can be divided into three main categories:
Conservative: In this group, the supraerupted tooth/teeth will not be reduced from the occlusal or incisal plane. They are usually extended beyond the occlusal/incisal plane from 0.1 mm to 4 mm. They can be corrected in the following ways:
Removable acrylic appliance: In this approach, the supraerupted tooth/teeth can be corrected using a removable appliance, such as a modified posterior bite plane appliance (MPBP), which is fabricated for retention with a ball-end clasp to manage a supraerupted maxillary molar along with ongoing fixed orthodontic treatment (Shafad et al., 2017). MPBP appliances have numerous advantages. For example, their physiological force generates minimal root resorption, and it is noninvasive and cost-effective compared with mini-implant-assisted intrusion. Moreover, it reduces buccal flaring compared with occlusally placed brackets for intrusion. It may minimize discomfort to patients, is easy to remove and clean with slight bulkiness, and reduces overall treatment time (Figs. 3A–3F). It can intrude more than one tooth at the same time without the need for the special retention of the intruded molar as the same bite plane appliance and can be modified by adding an acrylic tooth to the appliance. Thus, the same appliance can act as a retention appliance, a space maintainer, and a removable partial denture. Finally, the appliance can be reactivated by increasing the height of the appliance by adding self-curing acrylic on its occlusal surface if the required intrusion is increased. However, sometimes the use of removable appliances or splint for the management of supraerupted teeth in a temporomandibular dysfunction-free patient is not preferable because it might exacerbate signs and symptoms related to appliance wearing rather than increasing the occlusal vertical dimension (Abduo & Lyons 2012).
Figure 3. (A) Overeruption measurement. (B and C) Modified Removable Posterior Bite Plane Appliance. (D) MRPBPA with acrylic tooth. (E and F) Appliance in function after months (Shafad et al., 2017).
Fixed composite bite plane: In the case of a small posterior space, the correction of a supraerupted tooth can be adjusted using a reinforced direct composite plate to intrude a maxillary premolar tooth on the basis of the Dahl concept (Dahl et al., 1975). Subsequently, the space can be restored by an FP (Djemal et al., 2004). This type of treatment can be extended for up to a year or more (Figs. 4A–4F).
Figure 4. (A) Supraerupted tooth # 25. (B) Composite occlusal plate on teeth # 34 and 36. (C) RBB replacing tooth # 24 and composite occlusal stop on # 34. (D and E) Radiograph of tooth # 25 showing funneling of coronal crestal bone at end of tooth movements. Complete treatment after year. (F) At the 5th year, tooth # 25 is being held in the occlusal plane by an opposing bridge (Djemal et al., 2004).
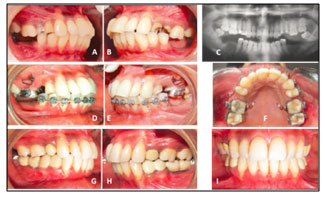
Intrusion only: This type of treatment can be performed using orthodontic intrusion only or in combination with mini-implants for anchorage. This treatment depends mainly on temporary skeletal anchorage devices and miniscrew and microscrew implants for skeletal anchorage. It can be accomplished after orthodontic treatment (Salazar et al., 2018), without orthodontic treatment (Al-Fraidi & Zawawi 2010), or with segmental orthodontic treatment as edge-wise arches (Acar & Ateş 2016). The intrusion can be on a single tooth or a group of teeth, unilateral (Foat et al., 2015), or bilateral (Prakash et al., 2014; Salazar et al., 2018; Al-Fraidi & Zawawi 2010). It is an interdisciplinary approach based on the use of orthodontic, periodontal, restorative, and implant therapy (Arslan et al., 2010). It is considered as a better treatment option for intruding tooth/teeth than prosthodontic reduction or extraction of extruded teeth (Prakash et al., 2014). It demonstrates a low, continuous, well-controlled manner of force without causing reciprocal movements of other teeth in direction and magnitude and creates an adequate interocclusal space for replacing missing tooth/teeth by construction of FPs (Acar & Ateş 2016; Faot et al., 2015; Al-Fraidi & Zawawi 2010). It can be applied for the treatment or correction of the supraerupted tooth/teeth of the maxillary arch (Acar & Ateş 2016; Prakash et al., 2014; Salazar et al., 2018; Faot et al., 2015; Al-Fraidi & Zawawi 2010) as shown in Figs. 5A–5K and Figs 6A–6I, or in the mandibular arch (Arslan et al., 2010; Tiago et al., 2016) as seen in Figs. 7A–7F and Figs. 8A–8H, or in the anterior region (Faot et al., 2015) as presented in Figs. 9A–9D).
Figure 5. (A–C) Preoperative and panoramic views. (D–G) Segmental archwire and miniscrew. (H and K) Views after the removal of minscrew and appliances (Acar & Ateş 2016).
Figure 6. (A–C) Preoperative and panoramic views. (D–F) Intrusion of bilateral maxillary molars using miniscrews with alloy spring. (G–I) Postoperative intraoral views (Faot et al., 2015).
Figure 7. (A) Supraerupted mandibular 2nd molar. (B) Over-trimmed occlusal surfaces of the left mandibular 2nd premolar and 1st molar. (C) Postoperative. (D) Miniscrews and mini-implants attached to the mandibular 2nd molar by coil spring and elastic thread. (E) Partial fixed appliance on mandibular 1st and 2nd premolars and 1st molar to correct the position of the mandibular 2nd molar. (F) Intruded left mandibular 2nd molar (Arslan et al., 2010).
Figure 8. (A) Extrusion of tooth # 47. (B) Orthodontic mini-implant. (C and D) Radiographic of mini-implant and orthodontic abutment cemented and archwire. (E and F) View of intrusion and verticalization. (G) After intrusion and stabilization. (H) With rehabilitation (Tiago et al., 2016).
Figure 9. (A) Model of anterior region of maxilla. (B) Frontal view of clinical evaluation. (C) Interocclusal space available after prosthetic abutment’s selection. (D) Frontal view of final rehabilitation (Faot et al., 2015).
The advantages of this type of treatment are that it is noninvasive and inexpensive. It allows the immediate application of forces to intrude the supraerupted tooth/teeth, requires in-office installation, and stimulates patient cooperation (Choi et al., 2005; McGuire et al., 2006; Mizrahi & Mizrahi 2007). Moreover, this system shows a good biological response of the tooth/teeth and the bony structures and soft tissues surrounding the intrusion. Tooth/teeth appear normal and acceptable, and the vitality and periodontal health of the area surrounding the treatment area are maintained (Arslan et al., 2010; Faot et al., 2015). The overall outcome of this treatment is excellent during different follow-up intervals. In general, orthodontic intrusion techniques are suitable methods for the management of supraerupted tooth/teeth and are unaccompanied by reciprocal effects on anchorage units (Hakami Z 2006).
Semiconservative Treatment: This type of treatment for supraerupted tooth/teeth is mainly dependent on the amount of supraeruption. If the supraeruption is between 0.1–2 mm, it can be managed by enamloplasty or coronoplasty. If the amount of supraeruption exceeds 1.5 mm, it can be corrected by intentional root canal treatment (RCT) followed by endocrown; by intrusion followed by RCT; or by the reduction of the supraerupted tooth/teeth followed by intentional RCT in the maxillary arch or mandibular arch. Finally, it can be assembled by a combination of crown lengthening (CL) and crowning. These approaches are described below:
Enameloplasty or coronoplasty: This approach is a selective reduction of occlusal interferences to influence mechanical contact conditions and the neural pattern of sensory input. It is a direct and irreversible change in the occlusal scheme. The complete function of occlusal adjustment is to eliminate the harmful action of occlusal forces. It provides the functional stimulation necessary to preserve periodontal health during activities (Carranza et al., 2018; Rosenstiel et al., 2015; Shillingburg et al., 2012; Mahoorkar et al., 2010). The objectives of coronoplasty are to mechanically eliminate all occlusal supra contacts in function and parafunction habits. In addition, it prevents trauma from occlusion, provides a stable occlusion and occlusal schema after adjustment, and improves the functional relationship between teeth (Mahoorkar et al., 2010 and Malathi et al., 2014).
Clinical steps of coronoplasty/enameloplasty or dentoplasty: This method can effectively reduce occlusal discrepancy in a slightly to moderately extruded tooth. Approximately 0.1–1.5 mm of enamel can be reduced or reshaped in different clinical situations. This reduction can be polished or reshaped with composite restoration and can be created by the reshaping of a single cusp for improving the occlusal plane (Stewart et al., 1983; Mahoorkar et al., 2010; Malathi et al., 2014). It can be performed through the following methods:
- Removing retrusive prematurities and eliminating the deflective shift from the retruded cuspal position to the intercuspal position (ICP).
- Adjusting the ICP to achieve stable, simultaneous, multipointed, and widely distributed contacts.
- Testing for excessive contacts (fremitus) on incisor teeth.
- Removing posterior protrusive supra contacts and establishing contacts that are bilaterally distributed on anterior teeth.
- Removing or lessening mediotrusive (balancing) interferences.
- Reducing excessive cusp steepness on the laterotrusion (working) contacts.
- Eliminating gross occlusal disharmonies.
- Rechecking tooth contact relationships.
- Polishing all rough surfaces (Carranza et al., 2018; Rosenstiel et al., 2015).
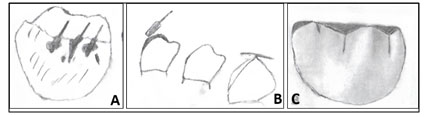
In some cases, the clinician may slightly increase reduction; thus, the minimum amount of dentine should be removed and recovered with a layer of composite or glass ionomer restoration in the usual manner (Mahoorkar et al., 2010). Coronoplasty/enameloplasty or dentoplasty can be performed following a previously reported form (Carranza et al., 2018; Stewart et al., 1983) as illustrated in (Figs. 10A–10C).
Grooving is usually conducted using a tapered diamond and results in the restoration of the depth of developmental grooves. Spheroiding is performed using a light paint brush stroke; this process restores the original tooth contour while reducing supra contacts. Pointing entails restoring cusp point contours.
Figure 10. Types of enamloplasty or coronoplasty, A, Grooving; B, Spheroiding; C, Pointing (Stewart et al., 1983).
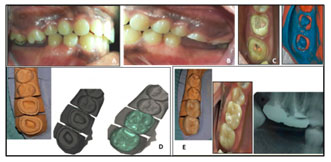
Endocrowns with intentional RCT: Results of clinical trials showed that clinicians can restore teeth by using endocrowns to improve long-term restorations for patients (Sun et al., 2019). Endocrowns after intentional RCTs are a good treatment option for restoring supraerupted endodontically treated posterior tooth/teeth. Its use, especially for endodontically treated teeth with short clinical crowns and for teeth where radicular anatomy eliminates the use of post and core, can also be justified (Basutkar et al., 2018) as shown in Figs. 11A–11E. New enhanced bonding mechanisms and advances in ceramic technology and adhesive techniques have increased the reliability of endocrowns as treatment options (Basutkar et al., 2018; Bindle & Mormann 1999; Sevimli et al., 2015).
Figure 11. (A) Supraerupted tooth # 16 and 17 with ↓ interocclusion. (B) After RCT, occlusal reduction was performed to restore occlusal plane and regain interarch space resulting in short clinical crown. (C) After RCT with shoulder finish line supragingivally and preparation inside the pulp chamber for endocrown. (D) Dies of scanned endocrowns. (E) Cemented endocrowns (Basutkar et al., 2018).
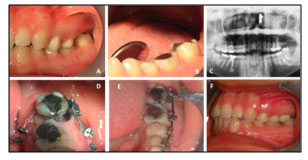
Intrusion with RCT and crowning: In some cases, the successful treatment of overerupted tooth/teeth with severe gingival recession may necessitate a multidisciplinary approach. After initial nonsurgical periodontal therapy and intentional RCT, maxillary molar extrusion can be corrected using a microimplant followed by covering the gingival recession and fixed prostheses to replace the extracted tooth/teeth; intentional RCT is then recommended as seen in Figs. 12A–12I (Mehta et al., 2018).
Figure 12. (A) Supraerupted tooth # 26. (B) Bone checking with periodontal probe. (C) Microimplant placement and postorthodontic intrusion. (D–J) Post endodontic and flap surgery. (H and I) Cemented crown (Mehta et al., 2018).
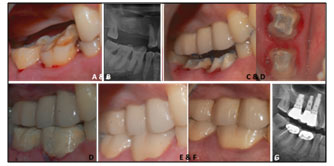
Reduction of teeth with intentional RCT and crowning: The supraerupted teeth in arches are reduced, followed by intentional RCT, CL, and crowning. These steps are done to create a stable, long‑term aesthetic results. The long‑term stability of the marginal bone levels, gingival levels, and status of the teeth subjected to endodontic therapy followed by CLP and final restorations are evaluated. Cases that underwent CL and endodontic therapy for corrections of the supraerupted teeth to regain the lost interocclusal spaces were retrieved, and cases with a complete set of clinical data and radiographs were obtained. The cases were followed by clinical and radiographical recording. The amount of interocclusal space regained was adequate to restore the missing teeth in the opposing arch. CL is a predictive procedure for the correction of supraerupted teeth in the maxilla (Figs. 13A–13E) or in the mandibular arches (Figs. 14A–14F) with a survival rate of 100% over 24–96 months (Patil et al., 2016).
Figure 13. (A and B) Preoperative views of supraerupted tooth # 16, 17, and 18. (C) Intentional RCT of tooth #16 and 17 and extraction of tooth #18. (D) Crowning of tooth # 16 and 17 and implants with crowns of mandibular molars. (E) Postoperative view after 96 months (Patil et al., 2016).
Figure 14. (A and B) Preoperative view of tooth # 46 and 47. (C and D) After occlusal reduction and intentional RCTs. (D) Maxillary and mandibular teeth with final prosthesis. (E–G) Postoperative views after 56 months (Patil et al., 2016).
Crown lengthening with crowning: Tooth/teeth with short clinical crowns and have undergone RCT followed by osseous CL resection and final prostheses with equigingival margins survive for long durations with stable gingival tissue and bone levels. This type of treatment may be predictably used to correct overerupted tooth/teeth and to obtain the necessary interarch space for prosthetic purposes. This treatment results in a favorable long-term prosthesis outcome (Patil et al., 2016).
Nonconservative Treatment: In this category, supraerupted tooth/teeth may be extended by 4 mm or more from the occlusal plain and can be corrected by orthognathic surgery only or removal. This category involves the following treatments:
Orthognathic surgical treatment: In this approach, posterior maxillary segmental osteotomy (PMSO) can be effective in correcting the supraeruption problem by a dentoalveolar extrusion (Meningaud et al., 2006; Punde 2013). This technique is simple, safe, and quick but strict that can achieve a good surgical outcome but a poor final occlusion. Some distortions can occur at any stage of surgery. Thus, using a surgical guide in the form of an acrylic splint is mandatory to achieve an acceptable final occlusion. The placement of an orthodontic arch wire or/and interim denture may prevent the risk of movement in the transverse and vertical dimensions (Erverdi et al., 2006). The PMSO technique is recommended for providing adequate interarch space in the presence of posterior supraerupted tooth/teeth and is usually conducted under general anesthesia. Through this technique, approximately 4 mm or more of interocclusal clearance can be achieved from the existing preoperative clearance; this effect allows the prosthetic restoration of dentition in the opposing arch. The outcome of this technique is stable without complications over 16–18 months postoperatively as presented in Figs. 15A–15H (Punde 2013). Moreover, PMSO can be bilateral (Baeg et al., 2016) as shown in Figs. 16A–16F.
Figure 15. (A) Supraerupted maxillary teeth. (B and C) Preoperative views. (D) Mock surgery and posterior segment repositioned for splint fabrication. (E and F) Osteotomy cuts 5 mm above the apices of molars and superiorly placed segment. (G and H) Postoperative after 6 months (Punde 2013).
Figure 16. (A and B) Preoperative views showing the supraeruption of teeth with 0 mm interdental space. (C and D) During PMSO. (E and F) Postoperative views showing ↑interarch space by implant-supported FPD (Baeg et al., 2016)
Corticotomy: This method is an effective approach for gaining the intrusion of the supraerupted tooth/teeth without any side effects using skeletal anchorage. It is quick and provides highly predictable results when performed through ultrasonic piezoelectric surgery, which is safer and causes less bone trauma than other techniques for osteotomies (Grenga and Bovi., 2013) (Figs. 17A–17L)
Figure 17. (A–C) Preoperative view of tooth # 26. (D–F) During surgery and bone cuts adjacent to tooth. (G and H) Miniscrews inserted mesial and distal to vertical bone cuts with palatal ligature wire. (I and J) During intrusion. (K and L) Postoperative views (Grenga and Bovi 2013).
Tooth extraction: This method is applied for cases of resorption or the loss of the alveolar bone support around the supraerupted tooth/teeth, such as tri/bifurcation involvement, or for cases where supraeruption resulted in inadequate or improper crown/root ratio (Mahoorkar et al., 2010; Baeg et al., 2016; Mehta et al., 2018; Rosenstiel et al., 2015; Shillingburg et al., 2012). The removal of tooth/teeth is recommended if the tooth is not a key tooth for future prosthetic option (Craddok & Youngson 2004).
Concluding Remarks from Previous Clinical Studies and Reviews: During routine examinations and treatment planning for the replacement of extracted teeth and its importance in preventing supraeruption, dentists should be aware and familiar with the occlusal changes following individual tooth/teeth loss. Moreover, they should advise patients on the importance of replacing missing teeth to maintain intact dentition throughout life (Craddock & Franklin 2005).
A series of studies investigated the type and extent of supraeruption and tooth/teeth movements associated with posterior teeth without their antagonist and recorded any relationship between supraeruption and oral or patient factors. The relationship of tooth/teeth positional interferences following posterior tooth loss during different jaw movements were studied (Craddock et al., 2007a; Craddock et al., 2007b; Craddock 2008; Faggion et al., 2011). The following conclusions were obtained:
- The mean supraeruption for subjects without antagonists was between 0–3.99 mm and that for the control group was 0–1.46 mm (Craddock et al., 2007a).
- Supraeruption in the maxillary tooth/teeth was statistically higher than that in the mandibular tooth/teeth and was recorded in 92% of subjects with unopposed teeth.
- Supraeruption is classified on the basis of the form of attachment loss, periodontal growth, and palatal movement of the tooth distal to the extraction position. Three types of supraeruption, which may be recorded alone or in combination, have been identified. Attachment loss is associated with active eruption, whereas periodontal growth is inversely associated with attachment loss. Both conditions are common in the maxillary arch, among young female patients, and in premolar teeth. Wear is directly associated with increasing age and is highly common in unopposed mandibular teeth (Craddock et al., 2007a).
- A statistically significant difference was observed between the subjects and control groups in terms of the degree of tipping of maxillary tooth/teeth mesial and distal to the extraction site (nonvertical movements). Moreover, a significant difference was noted in the rotation of the tooth/teeth mesial to the site (Craddock et al., 2007b).
- Protrusive interferences are associated with the position and presence of tooth/teeth distal to the extraction area, whereas working side interferences are associated with the tipping of the tooth mesial to the extraction area, and many other jaw movements are related mainly to the other types of interferences (Craddock and Youngson 2004; Craddock 2008).
- An intraexaminer agreement using Kappa scores and Spearman’s correlation revealed no statistically significant difference between supraeruption and occlusal interference even in the presence of supraerupted teeth (Craddock & Youngson 2004).
- A single study provided evidence for a statistically significant correlation between supraeruption resulting from the nonreplacement of mandibular first molars and recorded some gradual changes in the occlusal pattern; these interferences even extended to cause temporomandibular dysfunction (Gupta et al., 2014). In the same category, a study recommended that prosthodontic therapy in the presence of supraerupted teeth should be performed even in the presence of temporomandibular dysfunction if needed and indicated (deCarlsson &
- Klineberg 2000a; de Carlsson & Klineberg 2000b).
- An in vitro study measured the amount of the supraeruption of teeth following RPD treatment by comparing data collected from a surface-computer-aided design by dental casts at different time points (before and after RPD treatment). Supraeruption was exhibited by 38.1% of teeth antagonized with RPD and was considerably less than that in teeth that were unopposed by RPD (Matsuda et al., 2014).
Figure 18. Summary of techniques for correction of supraerupted teeth.
CONCLUSION
Supraeruption of tooth/teeth is a serious problem faced by dental practitioners during their daily dental practice. The importance of the treatment of supraerupted teeth is to re-establish the proper occlusal plane and the relation of both arches during different jaw movements to minimize further trauma of the occlusion to the tooth/teeth and their surrounding structures. This problem can be managed through easy and straightforward approaches, such as a conservative technique. This technique can be performed without any reduction of the supraerupted tooth/teeth and can be applied with a removable appliance, composite bite plane, and tooth intrusion. The semiconservative technique can be performed with tooth reduction only or by enamloplasty, which is effective in reducing occlusal discrepancy in a moderately extruded tooth by reducing a single cusp. This approach improves the occlusal plane. The amount of reduction is controlled by the clinical crown length of the tooth or by the size of the dental pulp. In some cases, the reduction can be extended into intentional RCT followed by the crowning of the supraeruption tooth/teeth. Other treatment choices can be surgical orthodontics, corticotomy, or extraction of the severely supraerupted tooth/teeth. A summary of techniques for correction of the supraerupted tooth/teeth before prosthetic treatments is presented in Fig. 22.
Source of support: Nil
Conflict of interest: None
REFERENCES
Abduo J, Lyons K. (2012). Clinical considerations for increasing occlusal vertical dimension: a review. REVIEW. Austr Dent J; 57: 2–10.
Acar YB, Ateş M. (2016). DIRECT USAGE OF MINISCREW ANCHORAGE TO INTRUDE OVERERUPTED MAXILLARY POSTERIOR TEETH BEFORE PROSTHODONTIC PREPARATION: A CASE REPORT. J Istanbul Univ Fac Dent 2016;50(1):43-50.
Al-Fraidi AA, Zawawi KH. (2010). Selective Intrusion of Overerupted Upper First Molars Using a Temporary Anchorage Device: Case Report. JCDA; 76(1): 25-30.
Arslan A, Ozdemir DN, Gursoy-Mert H, Malkondu O, Sencift K. (2010). Intrusion of an overerupted mandibular molar using mini-screws and mini-implants: a case report. Austr Dent J; 55: 457–461.
Ataoglu H, Kucukkolbasi H, Ataoglu T. (2002) Posterior segmental osteotomy of maxillary edentulous ridge: an alternative to vertical reduction. Int J Oral Maxillofac Surg; 31(5): 558–559.
Baeg SW, On SW, Lee JK, Song S. (2016). Posterior maxillary segmental osteotomy for management of insufficient intermaxillary vertical space and intermolar width discrepancy: a case report. Maxillof Plast Recon Surg; 38:28-33.
Basutkar N, Wali O, Ahmad SA-Q, Padala HK, Kumar RS, Sheetal A, Bahru H. (2018). “Management of Severely Supra-Erupted Teeth with Endocrown: Case Report”. Acta Scie Dent Scie: 2(9): 21-24.
Bindl A and Mormann WH (1999). “Clinical evaluation of adhesively placed cerec endocrown after 2 years- preliminary results”. J Adhe Dent; 1(3): 255-265.
Carranza F, Newman M, Glickman I. (2018). Clinical periodontology: WB Saunders Company; 18th Edition; page, 64, 70, 3174, 3208.
Choi BH, Zhu SJ, Han SG, Huh JY, Kim BY, Jung JH. (2005). The need for intermaxillary fixation in sagittal split osteotomy setbacks with bicortical screw fixation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod;100: 292–295.
Compagnon D, Woda A. (1991). Supraeruption of the unopposed maxillary first molar. J Prosthet Dent; 66: 29-34.
Craddock HL, Youngson CC. (2004). A study of the incidence of overeruption and occlusal interferences in unopposed posterior teeth. Br Dent J; 196(6): 341-8.
Craddock HL (2008). Occlusal changes following posterior tooth loss in adults. Part 3. A study of clinical parameters associated with the presence of occlusal interferences following posterior tooth loss. J Prosthodont; 17(1): 25-30.
Craddock HL, Franklin P. (2005). Overeruption–another challenge? Dent Update; 32(10): 605-8, Dent Update; 33(1): 12.
Craddock HL, Youngson CC, Manogue M, Blance A. (2007a). Occlusal changes following posterior tooth loss in adults. Part 1: a study of clinical parameters associated with the extent and type of supraeruption in unopposed posterior teeth. J Prosthodont; 16(6): 485-94.
Craddock HL, Youngson CC, Manogue M, Blance A. (2007b). Occlusal changes following posterior tooth loss in adults. Part2. Clinical parameters associated with movement of teeth adjacent to the site of posterior tooth loss. J Prosthodont; 16(6): 495-501.
Dahl B L, Krogstad O, Karlsen K. An alternative treatment in cases with advanced localised attrition. J Oral Rehab 1975; 2: 209-214.
Davenport JC, Basker RM, Heath JR, Ralph JP. (1988). A colour atlas of removable partial dentures. London: Wolfe Medical Publications: page, 11-13.
de, Carlsson GE, Klineberg IJ. (2000a). Need for occlusal therapy and prosthodontic treatment in the management of temporomandibular disorders. Part I: Occlusal interferences and occlusal adjustment. J Oral Rehabil; 27: 367-78. 15a.
de, Carlsson GE, Klineberg IJ. (2000 b). Need for occlusal therapy and prosthodontic treatment in the management of temporomandibular disorders. Part II: Tooth loss and prosthodontic treatment. J Oral Rehabil; 27(8): 647-59.
Djemal S, Bavisha K, GILMOUR G. (2004). Management of a Supra-Erupted Premolar: A Case Report. Dent Update 2004; 31: 220–222.
Erverdi N, Usumez S, Solak A. (2006). New generation open-bite treatment with zygomatic anchorage. Angle Orthod; 76(3):519-26.
Faggion CM Jr, Giannakopoulos NN, Listl S. (2011). How strong is the evidence for the need to restore posterior bounded edentulous spaces in adults? Grading the quality of evidence and the strength of recommendations. J Dent; 39:108-16.
Faot F, Ribeiro LF, Machado RM, Mello ACM, Del Bel Cury AA. (2015). Case Studies on the Use of Skeletal Anchorage Orthodontic Techniques Prior to Prosthetic Rehabilitation. J Oral Implantology; XLI (3): 332-6.
Gierie WV, Paterson RL, Proffit WR. (1999). Response of erupting human premolars to force application. Arch Oral Biol; 44: 423-428.
Grenga V, Bovi M. (2013). Corticotomy-Enhanced Intrusion of an Overerupted Molar Using Skeletal Anchorage and Ultrasonic Surgery. JCO; XLVII (1): 50- 55.
Gupta SK, Pratibha PK, Bhat KM, Mutalik S, Guddattu V. (2014). Non-replaced Mandibular First Molars and Temporomandibular Joint Dysfunction. Nepal J Medi Scien; 3(1):57-62.
Hakami Z. (2016). Molar Intrusion Techniques in Orthodontics: A Review. J Inter Oral Health; 8(2):302-306.
Jepson NJA, Allen PF. (1999). Short and sticky options in the treatment of the partially dentate patient. Br Dent J; 187: 646-652.
Joshi U, Patil S K Siddiqua A, Thakur N. (2010). Posterior maxillary segmental osteotomy for management of supraerupted teeth. Int J Dent Clin; 2(3):64-67.
Kayser A. (1981). Shortened dental arches and oral function. J Oral Rehabil; 8: 457-462.
Kiliaridis S, Lyka I, Friede H, Carlsson GE, Ahlqwist M. (2000). Vertical position, rotation, and tipping of molars without antagonists. Int J Prosthodont; 13:480-6.
Mahoorkar S, Puranik SN, Moldi A, Chowdhary R, Majge B. (2010). Management of Supra-erupted Posterior Teeth- A Review. Inter J Dent Clins; 2(3)27-30.
Malathi K, Anand AG, Karthikeyan R, Garg S. (2014). Coronoplasty. IOSR-JDMS; 13(9): 64-67.
Marcus SE, Drury TF, Brown LJ, et al. (1996). Tooth retention and tooth loss in the permanent dentition of adults: United States, 1988–1991. J Dent Res;75(Spec): 684-695.
Matsuda K-I, Miyashita Y, Ikebe K, Enoki K, et al. (2014). Overeruption of Teeth Opposing Removable Partial Denture: A Preliminary Study. Int J Prosthodont; 27: 475-6.
McGuire MK, Scheyer ET, Gallerano RL. (2006). Temporary anchorage devices for tooth movement: a review and case reports. J Periodontol; 77:1613–1624.
Mehta S, Gupta K, Sonal S, Lodha S. (2018). “Multidisciplinary Management of Supra-Erupted Periodontally Compromised Maxillary Molar”. Scie Arch Dent Sciences; 1(2): 10-13.
Meningaud J, Pitak-Arnnop P, Corcos L, Bertrand J. (2006). Posterior maxillary segmental osteotomy for mandibular implants placement: case report. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology; 102(5): e1-e3.
Meskin LH, Brown LJ. (1988). Prevalence and patterns of tooth loss in U.S. employed adult and senior populations, 1985– 86. J.Dent Educ; 52: 686-691.
Mizrahi E, Mizrahi B. (2007). Mini-screw implants (temporary anchorage devices): orthodontic and pre-prosthetic applications. J Orthod;34: 80– 94.
Patil SA, Kulkarni S, Thakur S, Naik B. (2016). Crown lengthening procedure following intentional endodontic therapy for correction of supra-erupted posterior teeth: Case series with long-term follow-up. J India Soc Periodontol; 20: 103-8.
Prakash P, Nishanth K, Jasani N, Katyal A, Nayak USK. (2014). Intrusion of overerupted molars using miniscrews and TMA spring: A case report. IJSS Case Reports & Reviews;1(1):4-8.
Punde PA. (2013). Gaining vertical interarch space for implant placement: The surgical protocol – Series of five cases. J Dent Implant; 3: 42-5.
Rosenstiel SF, Land MF, Fujimoto J. (2015). Contemporary Fixed Prosthodontics, 5th Ed. St. Louis (MO): Mosby Elsevier. pp. 40-66, 95-113, 161.
Rosenstiel S, Land M, Crispin B. (1998). Dental luting agents: a review of the current literature. J Prosthetic Dent; 80(3): 280-301.
Salazar G, Serrano AF, Mazzey GO. (2018). Intrusion of an overerupted maxillary molar with orthodontic mini implants for implant restorative purposes. J Int Oral Health; 10:44-6.
Sevimli G., et al. “Endocrowns: review”. J Ista Univ Facu Dent 2015; 49(2): 57-63.
Shafad M, Rahman S, Muddaiah S, Somaiah S, et al. (2017). Management of Supra Erupted Maxillary Molar by Using A Modified Removable Posterior Bite Plane –Two Case Reports. I J Adva Rese Development; 2(12): 1-6.
Shillingburg H, Hobo S, Whitsett LD, Richard J, Susan E. Brackett. (2012). Fundamentals of Fixed Prosthodontics. Chicago (4th Ed), Quintessence Publishing Co; page 21-23, 44-55, 88.
Solnit GS, Aquilino SA, Jordan RD. (1988). An etched metal splint to prevent the supereruption of unopposed teeth. J Prosthet Dent; 59: 381-382.
Stewart K, Rudd K, Kuebker W. (1983). Clinical removable partial prosthodontics. Impl Dent; 2(1): 94-112.
Sun J, Ruan W, He J, Lin X, et al. Clinical efficacy of different marginal forms of endocrowns: study protocol for a randomized controlled trial. BMC Trials 2019; 20: 454-60.
THE GLOSSARY OF PROSTHODONTIC TERMS, Ninth Edition (GPT-9). THE JOURNAL OF PROSTHETIC DENTISTRY 2017; 117(5S): e1- e105.
Tiago CM, Paulo LP, Nouer RA. (2016). Molar intrusion with orthodontic mini-implants: case reports. RGO, Rev Gaúch Odontol, Porto Alegre; 64(3): 327-332.
Tzimas K, Tsiafitsa M, Gerasimou P, Tsitrou E. (2018). Endocrown restorations for extensively damaged posterior teeth: clinical performance of three cases. Restor Dent Endod; 43(4):e38-e46.