1Department of Prosthetic Dental Science, College of Dentistry, Jazan University, Jazan, Saudi Arabia.
2Radiology Department, Sabya General Hospital, Jazan, Saudi Arabia.
3Radiology Department, King Khaled Hospital, Najran, Saudi Arabia.
4Radiology Department, Jedaidat Arar General Hospital, Arar, Saudi Arabia.
5Radiology Department, Psychiatric and Long-Term Care Hospital, Bisha, Saudi Arabia.
6Radiology Department, King Abdullah Medical City, Makkah, Saudi Arabia.
7Dental Intern, College of Dentistry, Jazan University, Jazan, Saudi Arabia.
8General Practitioner, Private Clinic, Jazan, Saudi Arabia.
Corresponding author email: drmoaleem2014@gmail.com
Article Publishing History
Received: 28/09/2021
Accepted After Revision: 11/12/2021
The suspended replacement of extracted teeth may disrupt the structural integrity of the whole dental arch, particularly in posterior maxillary or mandibular tooth/teeth. This phenomenon often has consequences of masticatory deficiency and temporomandibular joint disorders. This work aims to assess and measure the overeruption of posterior teeth from panoramic radiographs (OPGs) and its relation to gender, age, tooth type, arch, sides, and cause of tooth loss. A total of 100 OPGs were included in this in vitro study. The level of posterior overeruption was measured in mm using the panoramic digital radiograph machine and its software systems. Other variables such as gender, tooth/teeth involved, arches, and side were considered. All parameter values were inputted to a software program and assessed. P value < 0.05 was considered as statistically significant. Males accounted for 63% of the OPGs. Age groups 18–30 and 31–45 years had the highest frequency and percentage (34%). Approximately 74% of the patients got their tooth/teeth extracted 4–6 years ago.
The 0.7–1.2 mm overeruption subgroup had the highest proportion of 41%. The rate of overeruption in mandibular molars was 36%, which was the highest among the subgroups. Males had higher percentage than females in ≥60 and 31–45 age groups (84.65% and 76.5%, respectively), 4–6 years post-extraction time (85.7%), with significant differences, also, mandibular molars (85.0%) and mandibular arches (74.3%) were the higher among males. The highest level of overeruption was 0.7–1.2 mm, and mandibular molars were the most affected type. Significant differences between genders were detected in age groups, years after tooth loss, and arch side but not in cause of tooth loss, supra-erupted tooth type, and arch type parameters.
Extraction, Occlusal Interferences, Overeruption, Panoramic-Radiograph, Posterior- Teeth
Al Moaleem M. M, Sultan R. M, Makrami N. M, Mobarki M. M. M, Hakami A. A, Alrefaei M. G, Moafa M. I, Aqeeli O. I. H, Alrefae’i A. M. Y. Radiographical Measurements of Overeruption in Unopposed Posterior Teeth Among the Selected Saudi Arabians. Biosc.Biotech.Res.Comm. 2021;14(4).
Al Moaleem M. M, Sultan R. M, Makrami N. M, Mobarki M. M. M, Hakami A. A, Alrefaei M. G, Moafa M. I, Aqeeli O. I. H,
Alrefae’i A. M. Y. Radiographical Measurements of Overeruption in Unopposed Posterior Teeth Among the Selected Saudi Arabians. Biosc.Biotech.Res.Comm. 2021;14(4). Available from: <a href=”https://bit.ly/3Ghptxh“>https://bit.ly/3Ghptxh</a>
Copyright © Al Moaleem et al., This is an open access article distributed under the terms of the Creative Commons Attribution License (CC-BY) https://creativecommns.org/licenses/by/4.0/, which permits unrestricted use distribution and reproduction in any medium, provide the original author and source are credited.
INTRODUCTION
Overeruption is defined as the degree of excess tooth movement starting from the cusp tip to the carve passing over the canine and posterior teeth. The overeruption of maxillary or mandibular premolars and molar tooth/teeth can be considered as one of the common clinical findings in day-to-day dental practice. Postponing the replacement of lost teeth often leads to the extrusion of the contrasting tooth into the edentulous space, which in turn could result in masticatory insufficiency and temporomandibular joint disorders (Craddock 2010; Gupta et al. 2014 ).
When a prosthesis, either fixed or removable, is planned on the opposing edentulous arch, the function of the posterior occlusion must be re-establishing through a comprehensive dental treatment plan (Craddock and Youngson 2004; Craddock et al. 2007; Mahoorkar et al. 2010; Shillingburg et al. 2012; GPT-9 2017; Ahmari et al. 2020).
Over-erupted tooth/teeth can be categorized intro three types according to the degree of overeruption extending from the occlusal plane: mild (over-erupted tooth ranges 0.1–1.5 mm), moderate (1.6–3.5 mm), and severe (exceeds 3.5 mm) (Compagnon and Woda 1991; Craddock and Youngson 2004; Newman et al. 2018). Another classification is according to the amount of reduction required form the over-erupted tooth/teeth: conservative, semiconservative, and nonconservative (Ahmari et al. 2020).
The most frequently extracted teeth are the first permanent molars either in the maxillary or mandibular arch, followed by the premolars in the maxillary arch (Djemal et al. 2004; Craddock et al. 2007; Tiago et al. 2016; Patil et al. 2016; Baeg et al. 2016; Salazar et al. 2018). Marcus et al. (1996) and Craddock et al. (2007), mentioned that mandibular posterior teeth are more likely to be removed than maxillary posterior teeth; with aging, posterior teeth would probably be extracted and missed in both sides (Marcus et al. 1996; Craddock et al. 2007; Shillingburg et al. 2012; Basutkar et al. 2018; Ahmari et al. 2020).
In relation to the level of over-erupted tooth/teeth (in mm), Craddock et al. (2007) found that the average volume of over-erupted tooth/teeth ranges is 1.68–3.99 mm for the teeth without antagonism, 1.03 mm for mandibular arch, and 1.91 mm for maxillary arch. Kiliaridis et al. (2000) recorded that 24% of unopposed teeth had more than 2 mm overeruption among 82% of the examined subjects without antagonist teeth. Other studies calculated the occlusal change of unopposed teeth within the border of 2 mm (Kiliaridis et al. 2000; Craddock et al. 2007; Faggion et al. 2011; Ahmari et al. 2020).
After examining their overeruption from OPGs, Moaleem et al. (2021) reported no significant differences in overeruption values among different gender or age groups. Significant difference was found between the types and sites of teeth, with a relatively high ratio observed in molar teeth, mandibular arch, and young age group.
Other studies have investigated the relationship of tooth positional interferences following posterior tooth loss during different mandibular arch movements (Craddock et al. 2007; Craddock et al.; 2007b; Craddock 2008). This study aimed to measure and compare the level of posterior tooth overeruption from OPGs and its relation to gender, age group, tooth type, arch, sides, and cause of tooth loss. The hypothesis was as follows: no differences in the level of tooth overeruption exist between genders in relation to other parameters measured from the OPGs.
MATERIAL AND METHODS
A total of 100 OPGs were collected from private dental centers in Jazan, SA, for this cross-sectional radiographic study. All OPGs were obtained from the pool of patients who reported for the replacement of missing posterior maxillary or mandibular molars. The supra-erupted teeth selected from these OPGs were unopposed posterior teeth in the maxillary or mandibular arches. This cross-sectional study was approved by the Research and Ethics Committee at the Authority of Medical Sector in Jazan City and was conducted in accordance with the guidelines of the World Medical Association Declaration of Helsinki.
Non-randomized clinical study design was conducted among OPGs collected from the last 2 years. The sample size of approximately 100 participants was verified based on a G*Power software (http:// www.gpower.hhu.de/en.html) with the self-assurance amount altered at 90%, power adjusted at 85%, and a reasonable outcome amount. This study included patients who attended private dental clinics and had their OPGs taken.
Inclusion criteria were as follows: aged 18 years or above from both genders; a minimum of one supra-erupted posterior maxillary or and mandibular tooth; presence of posterior and anterior vertical stops; the extracted teeth should have been in the posterior zone of any arch and had been removed in the past 4 years or more; and have not received any previous dental treatments (prosthodontic or orthodontic).
Radiographic evaluation and demographic data of subjects were collected as followed. First, individual, and demographic information was collected, such as gender, age groups (18–30, 31–45, 46-59 and ≥ 60 years), years after extraction (4–6 and ≥6 years), and cause of tooth removal (dental caries, periodontal disease, failure in root canal treatment [RCT] and others such as periapical pathosis or dental trauma).
A tooth was classified as extracted due to periodontal disease when it satisfies the eighth criterion of Russell’s periodontal index, i.e., the presence of considerable mobility in accordance with Miller’s mobility index (1995) (McCaul et al. 2001). However, a tooth was labeled as requiring extraction due to dental caries when the clinical crown was broken down by caries and is non-restorable (Gossadi et al. 2015). A failed RCT occurs when retreatment cannot be made due to any reasons under any present condition (Meshni et al. 2018).
Overeruption is defined as the movement of a tooth or teeth above the normal occlusal plane (GPT-9 2017; Kim et al. 2016). The involved over-erupted teeth were recorded as molars and/or premolars, left or right side, and maxillary or mandibular arch. Overeruption values were recorded, measured, and registered into three scales (0.1–0.6, 0.7–1.2, and >1.3 mm) (Craddock and Youngson 2004; Craddock et al. 2007; Kim et al. 2016; Moaleem et al. 2021). This part concerned with the measurements of the extent of over-erupted teeth of participants based on their OPGs. The panoramic digital radiograph machine was a tomography x-ray system model PaX-Flex3D (Germany) operated at 30% magnification.
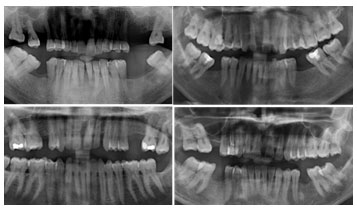
Supra-eruption was calculated by drawing a straight line joining the tips of buccal cusps between the canine and the adjacent or the last tooth of arch on the over-erupted tooth/teeth side. The amount of tooth structure outside or lower than this line was considered as overeruption (in mm) and was calculated as shown in Figures 1 and 2 (Craddock et al. 2007; Kim et al. 2016; Moaleem et al. 2021).
Figure 1 shows the over eruption in mandibula and maxillary arch in right or left side of both arches, and Figure 2 displays a bilateral overeruption in the right and left sides of maxillary or mandibular arch. All measurements for overeruption level were performed by a qualified investigator (Al M.M).
Data were tabulated and summarized in an Excel sheet (Office 2010) on a personal computer. Descriptive statistical analysis including mean, frequency, percentages, and standard deviation (SD) was performed using SPSS software program version 21 (Chicago, Illinois, USA). Assessments and associations among different genders, age groups, and types of overeruption tooth were determined using Chi-square test. p≤ 0.05 was considered as significant. Informed consent was obtained from all participants included in the study. Moreover, the study acquired the ethical approval from the ethical committee at the College of Dentistry, University of Jazan on 20/10/2020
RESULTS AND DISCUSSION
Figure 1: Unilateral overeruption in maxillary or / and mandibular
arch in the right or left side
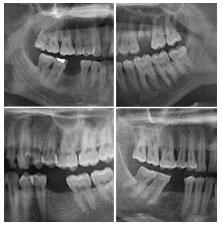
Figure 2: Bilateral overeruption in maxillary or mandibular
arch in the right or left side
A total of 100 over-erupted tooth/teeth in the posterior area of both arches were involved in this in vitro study. The values of overeruption (in mm) from the OPGs were calculated after 30% magnification reduction. Figure 1 offers the descriptive statistics of the subjects, including the gender, age groups, years after tooth loss, cause of tooth loss, arch, and side involved in overeruption.
The means and SD for gender, age groups, years since tooth loss, causes of tooth loss, arch, and sides were 1.370 ± 0.485, 1.775 ± 0.779, 1.275 ± 0.449, 2.220 ± 0.773, 2.030 ± 0.810, and 1.550 ± 0.500, respectively. Most of the OPGs were obtained from male subjects (63%) and patients aged 18–73 years. The highest frequency and percentage were observed in the 18–30 and 31–45 age subgroups (34%) and in the 4–6 years post-extraction subgroup (74%). Other pieces of demographic information are presented in Statistics 1.
Table
| Variable | Subgroups | Percentage (%) |
| Gender | Males | 63% |
| Females | 37% | |
| Age groups (years) | 18–30 | 34 |
| 31–45 | 34 | |
| 46-59 | 19 | |
| ≥ 60 | 13 | |
| Years since tooth loss | 4–6 years | 74 |
| >6 years | 26 | |
| Cause of tooth loss | Periodontal disease | 13 |
| Dental caries | 60 | |
| Failed RCT | 19 | |
| Others | 8 | |
| Arch | Maxilla | 31% |
| Mandibula | 35% | |
| Both arches | 34% | |
| Side | Right | 45% |
| Left | 55% |
Table
| Variable | Subgroups | Number (n) | Percentage (%) | Mean | Standard deviation |
| Gender | Males | 63 | 63% | 1.370 | .485 |
| Females | 37 | 37% | |||
| Age groups (years) | 18–30 | 34 | 34 | 1.775 | .779 |
| 31–45 | 34 | 34 | |||
| 46-59 | 19 | 19 | |||
| ≥ 60 | 13 | 13 | |||
| Years since tooth loss | 4–6 years | 74 | 74 | 1.275 | .449 |
| >6 years | 26 | 26 | |||
| Cause of tooth loss | Periodontal disease | 13 | 13 | 2.220 | .773 |
| Dental caries | 60 | 60 | |||
| Failed RCT | 19 | 19 | |||
| Others | 8 | 8 | |||
| Arch | Maxilla | 31 | 31% | 2.030 | .810 |
| Mandibula | 35 | 35% | |||
| Both arches | 34 | 34% | |||
| Side | Right | 45 | 45% | 1.550 | .500 |
| Left | 55 | 55% |
Statistics 1. Descriptive of demographic data of subjects (OPG=100)
With respect to the overeruption level, 41% of the cases had 0.7–1.2 mm with mean and SD of 0.725 ± 0.64. Slight differences were recorded in the over-erupted cases and tooth types between mandibular (36%) and maxillary (30%) molars with mean and SD of 2.780 ±1.088 (Table 1).
Table 1. Overeruption descriptive of amount (mm) and type of tooth and presence
of occlusal interferences included in this study (OPG=100)
| Variable | Subgroups | Number (n) | Percentage (%) | Mean | SD |
| Overeruption from OPG (mm) | No overeruption | 8 | 8 | 0.725 | 0.464
|
| 0.1–0.6 mm | 29 | 29 | |||
| 0.7–1.2 mm | 41 | 41 | |||
| >1.3 mm | 22 | 22 | |||
| Over-erupted tooth type | Maxillary Premolar | 14 | 14% | 2.780 | 1.088 |
| Maxillary Molar | 30 | 30% | |||
| mandibular premolar | 20 | 20% | |||
| Mandibular Molar | 36 | 36% |
Table 2. Association between the frequency and % of variables in relation to
Different gender groups by Chi-square or Fisher’s exact test (n=100)
| Parameters | Males
N % |
Females
N % |
Total
N and % |
P-Values | |
| Age groups | 18–30 | 17 (50.0) | 17 (50.0) | 34 | 0.018* |
| 31–45 | 26 (76.5) | 8 (23.5) | 34 | ||
| 46-59 | 9 (47.7) | 10 (52.3) | 19 | ||
| ≥ 60 | 11 (84.6) | 2 (15.4) | 13 | ||
| Years since tooth loss | 4–6 year | 54 (85.7) | 20 (54.1) | 74 | 0.007* |
| >6 years | 9 (14.3) | 17 (45.9) | 26 | ||
| Causes of tooth loss | Periodontal disease | 6 (46.2) | 7 (53.8) | 13 | 0.200 |
| Dental caries | 41 (68.3) | 19 (31.7) | 60 | ||
| Failed RCT | 13 (68.4) | 6 (31.6) | 19 | ||
| Others | 3 (37.5) | 5 (62.7) | 8 | ||
| Supraerupted tooth/teeth | Maxillary premolars | 9 (64.3) | 5 (35.7) | 14 | 0.106 |
| Maxillary molars | 17 (56.7) | 13 (43.3) | 30 | ||
| Mandibular premolars | 17 (85.0) | 3 (15.0) | 20 | ||
| Mandibular molars | 20 (55.6) | 16 (44.4) | 36 | ||
| Side | Right | 22 (48.9) | 23 (51.1) | 45 | 0.012* |
| Left | 41 (74.5) | 14 (25.5) | 55 | ||
| Site (Arch) | Maxilla | 18 (58.1) | 13 (41.9) | 31 | 0.261 |
| Mandible | 26 (74.3) | 9 (25.7) | 35 | ||
| Both arches | 19 (55.9) | 15 (44.1) | 34 | ||
*Significant differences
Table 2 shows the association of overeruption with gender groups and other parameters. Males accounted for 52.3% and 50.0% of the ≥60 and 31–45 age groups, respectively. Females accounted for 85.6% and 76.5% of the 46–56 and 18–30 age groups, respectively. The subgroup of 4–6 years post-extraction represented the highest males and females with 85.7% and 54.1%, respectively. In relation to the side, the left side was recorded for 74.3% of males, and the right side was recorded for 51.1% of females. These parameters showed significant differences with gender at p value ˃ 0.050.
Among the males, dental caries, and failure RCT were the most frequent cause of tooth removal with 68.4% for both parameters. For females, other causes and periodontal diseases accounted for the highest percentages with 62.7% and 53.8%, respectively. Maxillary and mandibular molars were the most frequent in males and females with 20 and 16 cases, respectively. Mandibular arches accounted for the highest percentage of 74.3% among males, and both arches were recorded among females (44.1%). All these parameters showed non-significant differences with gender.
Table 3. Association between the frequency and % of gender and over-erupted tooth in
relation to amount of overeruption in mm by Chi-square or Fisher’s exact test (n=100)
| Variable | Overeruption from OPG (mm) | No
Number (%)
|
0.1–0.6 mm
Number (%) |
0.7–1.2 mm
Number (%) |
>1.3 mm
Number (%) |
P values |
| Gender | Males | 2 (3.2) | 21 (26.5) | 25 (40.5) | 15 (29.7) | 0.117 |
| Females | 0 (0.00) | 11 (29.7) | 15 (40.5) | 11 (29.7) | ||
| Over-erupted tooth | Maxillary Premolar | 0 (0.00) | 4 (28.5) | 7 (49.9) | 3 (21.3) | 0.217 |
| Maxillary Molar | 3 (10.0) | 6 (20.0) | 14 (46.7) | 4 (13.2) | ||
| Mandibular Premolar | 0 (0.00) | 11 (55.0) | 6 (30.0) | 3 (15.5) | ||
| Mandibular Molar | 0 (0.00) | 10 (27.8) | 13 (36.1) | 13 (36.1) |
Table 3 shows the relation of the overeruption level (in mm) to gender and tooth type. No significant differences between the overeruption degree and the two parameters with p values of 0.117 and 0.217. For gender, the highest percentages were obtained for the amount of overeruption at 0.1–0.6 mm (40.5%), followed by >1.3 mm (29.7%). Maxillary molar and premolars had the highest percentage in the 0.7–1.2 mm subgroup (49.9% and 36.1%, respectively), mandibular premolars had the highest number in 0.1–0.6 mm subgroup (55.0%), and molar teeth had the highest frequency in the 0.7–1.2 mm subgroup (36.1%).
Assessment was performed on the interclass correlation coefficient for the measurement of supra-eruption (in mm) on the OPGs. Intra-examiner reliabilities were determined by drawing a Bland–Altman plot 7 for continuous data. The two measurements fell between 96% and 98% confidence interval bands (Table 4) (Bland and Altman 1986).
Table 4. Overeruption interclass correlation for OPGs
| Intraclass Correlation Coefficient for PRs | |||||||
| Intraclass Correlationb | 95% Confidence Interval | F Test with True Value 0 | |||||
| Lower Bound | Upper Bound | Value | df1 | df2 | Sig | ||
| Single Measures | .997a | .996 | .998 | 955.937 | 99 | 99 | .000 |
| Average Measures | .999c | .998 | .999 | 955.937 | 99 | 99 | .000 |
When the edentulous space is in the posterior part of the mouth, replacing an extracted tooth is important to patients to maintain the state of dynamic balance with the teeth supporting each other. After a tooth loss, the teeth adjacent to or opposing the edentulous space frequently over-erupt, tilt, and move into the extraction site. The severe overeruption of unopposed teeth into the edentulous space results in an insufficient place to replace the missing tooth. Hence, the tooth opposing the edentulous space must be replaced (Shillingburg et al. 2012). This study aimed to evaluate and measure the overeruption degree of posterior teeth from OPGs and its relation to gender, age, tooth type, arch, sides, and cause of tooth loss.
Results showed 0.7–1.2 mm as the most frequent overeruption level and mandibular molars as the most frequent tooth type for overeruption. These results agreed with previous studies (Craddock et al. 2007; Kim et al. 2016; Moaleem et al. 2021). The null hypothesis was partially rejected because of the significant difference in age groups, years after tooth loss, and right or left side of the mouth between genders.
Other parameters such as cause of tooth loss, type of over-erupted teeth, and maxillary or mandibular showed no significant differences between genders; hence, the null hypothesis was considered as partially accepted. Assessment on intra-examiner reliability to evaluate overeruption by Bland–Altman plot test score was recorded between 96% and 98% confidence interval bands (Table 4). The values indicated respectable and acceptable reliability in this radiographic study (Moaleem et al. 2021).
The effects of gender on the prevalence of periodontal disease are not clearly understood, and research offers conflicting evidence on this matter. In the present study, significant differences between genders were detected in age groups, years after tooth loss, and side of the arch but not in cause of tooth loss, supra-erupted tooth type, and arch type parameters. Such comparison between the degree of overeruption and gender has never been reported.
This finding might be related to the differences in the bone type of maxillary and mandibular arches between genders, muscle activity, cause of teeth extraction, and genetic factors. Previous studies in Jazan concluded significant differences between genders and dental caries, with mandibular first molars accounting for the highest number and percentage (Moaleem et al. 2016; Moaleem MM. 2017; Noman et al. 2019; Moaleem et al. 2021).
Similar parameters percentages were recorded in the current radiographic study. Kim et al. (2016) conducted a clinical study on the use of OBG for the implant replacement of missing teeth. The results showed that the majority of the extracted teeth were mandibular molar teeth 27 out of 35 extracted teeth replaced by implant), followed by maxillary molars with six extracted sites and one each for maxillary and mandibular premolars (Moaleem et al. 2021).
To some extent, this finding was in agreement with the present finding, that is, mandibular molars were the most frequent with 36/100, followed by maxillary molars with 27/100. The previous study recruited only a few patients, and their main objective is to implant replacement for the missing teeth. Meanwhile, the current work aimed to measure the overeruption of posterior teeth. However, marginally similar results were found regarding the number of over-erupted premolar teeth in both arches (Kim et al. 2016; Moaleem et al. 2021).
In the presence of <2 mm overeruption distance, prosthetic replacement, or implant placement with their superstructure prostheses of missing teeth can be performed without addressing the super-erupted opposing tooth. This study determined that the lack of treatment for the super-erupted tooth will have no negative effects on the implant or the opposing tooth. Most of the over-erupted values were between 0.7 and 1.2 mm, which are in parallel with previous results (Faggion et al. 2011; Kim et al. 2016). Craddock et al. 2007 recorded a mean overeruption value of 1.68 mm and observed >1 mm overeruption for 68% of cases and >2 mm in 27% of cases; for the control group, 8% of cases had overeruption of >1 mm and none had supra-eruption of >2 mm (Moaleem et al. 2021).
Gupta et al. (2014) investigated 153 patients with supra-erupted opposing teeth and observed the clicking of the TMJ in 106 patients (69.3%). The drifting of teeth adjacent to the missing molars was also a frequent finding (133 patients). Clicking was observed in 96 patients (72.2%) out of these 133 patients. Once the tooth begins to shift in angle, the vector of force tends to increase tooth tilting and thus induce a different bio mechanical effect on the mandible (Obrez and Gallo 2006). These results agreed with concept of tightly locked occlusion, a kind of secondary change associated with supra eruption, drift, or tipping, and tilting of the posterior teeth associated with TMD (Wang et al. 2007; Moaleem et al. 2021).
Livas et al. (2016) conducted a radiographic study on 65 patients and found no significant eruption in unopposed mandibular second molars bonded with fixed sectional retainers compared with the molars partially occluded with antagonists lacking fixed retention. Therefore, fixed retention should be measured to limit tooth overeruption in unopposed molars. This study also indirectly revealed that the first molar tooth was the most frequently extracted among the samples; this finding agreed with the current results and other previous studies (Craddock et al. 2007; Faggion et al. 2011; Moaleem et al. 2021). In addition, significant differences were observed between genders, which also coincided with the current findings. However, the number of maxillary molar teeth was higher than that of mandibular ones. This result might be related to their study objectives.
In this study, 8% of the examined OPGs had no overeruption. Such status requires only observation with no treatment. A similar pattern of no overeruption of unopposed posterior teeth was previously reported. Craddock and Youngson (2004) recorded over 30 samples, and Craddock et al. 2007b noted no over-eruption in 27% of their samples. Moaleem et al. (2021) verified zero over eruption of the unopposed posterior teeth in 7 (11%) out of 65 samples (Moaleem et al. 2021). This radiographic study has some limitations, such as its cross-sectional design, small number of OPGs, and failure to collect data from different clinics. Further randomized clinical research using dental cone-beam computed topography with long follow-up period is recommended to confirm these results.
CONCLUSION
The finding of the present study suggests that the highest amount of overeruption was 0.7–1.2 mm, and mandibular molars were the most affected type. Significant differences between genders were observed in age groups, years after tooth loss, and arch side with overeruption. No significant differences between genders were detected in the overeruption ratio among cause of tooth loss, supra-erupted tooth type, and arch type. The acceptability of the study method was confirmed by the good relation of the intra-examiner reliability and the good confidence interval band based on the Bland–Altman plot.
ACKNOWLEDGEMENTS
For this study, the sample collection was supported by Professor Mohammed M. Sobhey.
Conflict of Interests: Authors declare no conflict of interests to disclose.
REFERENCES
Ahmari NMA, Aldhalail MA, Abidi NH, et al. (2020). Techniques for management of supraerupted teeth prior to prosthetic treatment: updated review. Biosci Biotechnol Res Commun;13(1):261–273. DOI: 10.21786/bbrc/13.1/43.
Baeg S, On S, Lee J, et al. (2016). Posterior maxillary segmental osteotomy for management of insufficient intermaxillary vertical space and intermolar width discrepancy: a case report. Maxillofac Plast Reconstr Surg; 38(1):28. DOI: 10.1186/s40902-016-0074-0.
Basutkar N, Wali O, Ahmad SAQ, et al. (2018). Management of severely supra-erupted teeth with endocrown: case report. Acta Sci Dent Sci 2018;2(9): 154-9.
Bland JM and Altman DG (1986). Statistical method for assessing agreement between two methods of clinical measurement. The Lancet; 1:307–10.
Compagnon D and Woda A (1991). Supraeruption of the unopposed maxillary first molar. J Prosthet Dent; 66(1):29–34. DOI: 10.1016/0022- 3913(91)90347-y.
Craddock HL (2008). Occlusal changes following posterior tooth loss in adults. Part 3. A study of clinical parameters associated with the presence of occlusal interferences following posterior tooth loss. J Prosthodont; 17(1):25–30. DOI: 10.1111/j.1532-849X.2007.00239.x.
Craddock HL (2010). Consequences of tooth loss: 2. Dentist considerations– restorative problems and implications. Dent Update; 37(1):28-32. DOI: 10.12968/denu.2010.37.1.28.
Craddock HL and Youngson CC (2014). A study of the incidence of overeruption and occlusal interferences in unopposed posterior teeth. Br Dent J;196(6):341–348.
Craddock HL, Youngson CC, Manogue M, et al. (2007). Occlusal changes following posterior tooth loss in adults. Part 1: a study of clinical parameters associated with the extent and type of supraeruption in unopposed posterior teeth. J Prosthodont; 16(6):485–494. DOI: 10.1111/j.1532-849X.2007.00212.x.
Craddock HL, Youngson CC, Manogue M, et al. (2007b). Occlusal changes following posterior tooth loss in adults. Part 2. Clinical parameters associated with movement of teeth adjacent to the site of posterior tooth loss. J Prosthodont; 16(6):495–501. DOI: 10.1111/j.1532- 849X.2007.00223.x.
Djemal S, Bavisha K and Gilmour G (2004). Management of a supra-erupted premolar: a case report. Dent Update; 31(4):220–222. DOI: 10.12968/denu.2004.31.4.220.
Faggion CMJ, Giannakopoulos NN, Listl S (2011). How strong is the evidence for the need to restore posterior bounded edentulous spaces in adults? Grading the quality of evidence and the strength of recommendations. J Dent; 39(2):108–116. DOI: 10.1016/j. jdent.2010.11.002.
Gossadi YI, Nahari H, Kinani H, et al. (2015). Reasons for permanent teeth extraction in Jizan region of Saudi Arabia. IOSR-JDMS;14(1):86– 89. DOI: 10.9790/0853-14178689.
GPT‐9 (2017). Glossary of Prosthodontic Terms NE, The Academy of Prosthodontics Foundation. J Prosthet Dent;117(5S):e1–e105. DOI: 10.1016/j.prosdent.2016.12.001.
Gupta S, Pratibha P, Bhat K, et al. (2014). Non-replaced mandibular first molars and temporomandibular joint dysfunction. Nepal J Med Sci;3(1):57–62. DOI: 10.3126/njms.v3i1.10360.
Kiliaridis S, Lyka I, Friede H, et al. (2000). Vertical position, rotation, and tipping of molars without antagonists. Int J Prosthodont; 13(6):480–486.
Kim YK, Ahn KJ, Yun PY, et al. (2016). The clinical prognosis of implants that are placed against super-erupted opposing dentition. J Korean Assoc Oral Maxillofac Surg; 42(3):139–143. DOI: 10.5125/ jkaoms.2016.42.3.139.
Livas C, Halazonetis DJ, Booij JW, et al. (2016). Does fixed retention prevent overeruption of unopposed mandibular second molars in maxillary first molar extraction cases? Progress in Orthodontics; 17:6-10. DOI 10.1186/s40510-016-0119-z.
Mahoorkar S, Puranik SN, Moldi A, et al. (2010). Management of supraerupted posterior teeth. Int J Dent Clin;2(3): 231-6
Marcus SE, Drury TF, Brown LJ, et al. (1996). Tooth retention and tooth loss in the permanent dentition of adults: United States, 1988–1991. J Dent Res; 75 Spec No:684-95. DOI: 10.1177/002203459607502S08.
McCaul LK, Jenkins WM, Kay EJ (2001). The reasons for extraction of permanent teeth in Scotland: a 15-year follow-up study. Br Dent J; 190(12):658–662. DOI: 10.1038/sj.bdj.4801068.
Meshni AA, Moaleem MM, Mattoo KA, et al. (2018). Radiographic evaluation of post-core restorations fabricated by dental students at Jazan University. J Contemp Dent Pract; 19(1):66–72. DOI: 10.5005/jp-journals-10024-2213.
Moaleem MMA (2017). Patterns of Partial Edentulism and its Relation to Khat Chewing in Jazan Population – A Survey Study. J Clini Diag Research; 11(3): ZC55-ZC59.
Moaleem MMA, Somaili DM, Ageeli TA, et al. (2016). Pattern of Partial Edentulism and Its Relation to Age, Gender, Causes of Teeth Loss in Jazan Population. American Journal of Health Research; 4(5): 121-126.
Moaleem MMA. (2021). Clinical and Radiographical Measurements of Supraeruption and Occlusal Interferences in Unopposed Posterior Teeth. J Contemp Dent Pract; 23(6):165-72. 10.5005/jp-journals-10024-3143
Newman M, Takei H, Klokkevold P, et al. (2018). Newman and Carranza’s clinical periodontology. Saunders; Pp 231.
Noman NA, Aladimi AA, Alkadasi BA et al. (2019). Social Habits and Other Risk Factors that Cause Tooth Loss: An Associative Study Conducted in Taiz Governorate, Yemen. J Contemporary Dental Practice; 20 (4): 429-40.
Obrez A and Gallo LM (2006). Functional and biomechanical analysis of the TMJ.In: Laskin,DM,eds. Temporomandibular disorders, an evidence based approach to diagnosis and treatment. IL: Quintessence:29-30.
Patil SA, Kulkarni S, Thakur S, et al. (2016). Crown lengthening procedure following intentional endodontic therapy for correction of supraerupted posterior teeth: case series with long-term follow-up. J Indian Soc Periodontol; 20(1):103. DOI: 10.4103/0972-124X.175176.
Salazar G, Serrano AF and Mazzey GO (2018). Intrusion of an overerupted maxillary molar with orthodontic mini-implants for implant restorative purposes. J Int Oral Health; 10(1):44. DOI: 10.4103/ jioh.jioh_236_17.
Shillingburg HT, Hobo S, Whitsett LD, et al. (2012). Fundamentals of Fixed Prosthodontics, Quintessence Publishing Co, 4(7) pp 87.
Tiago CM, Previdente L and Nouer PRA (2016). Molar intrusion with orthodontic mini-implants. RGO—Rev Gaúch Odontol; 64(3):327–332. DOI: 10.1590/1981-8637201600030000133274.
Wang MQ, Cao HT, Liu FR, et al. (2007). Association of tightly locked occlusion with temporomandibular disorders. J Oral Rehabil; 34: 169-73. http://dx.doi.org/10.1111/j.1365-2842.2006.01657.x.


