Department of Medicine, Alimam Muhammad Ibn Saud Islamic University, Riyadh, Saudi Arabia.
Corresponding author email: hussaingad5@gmail.com
Article Publishing History
Received: 11/12/2020
Accepted After Revision: 24/03/2021
COVID-19 outbreak affects patients with chronic diseases in several ways including psychological and pathological effects. Accordingly, the present study aimed to evaluate the pathopsychological impact of the COVID-19 outbreak in patients with comorbidities in Saudi Arabia. In this online questionnaire-based cross-sectional study, 161 Saudi patients with chronic diseases were conscripted during the country’s complete lockdown due to the COVID-19 outbreak (May–June,2020). A purposeful electronic questionnaire was premeditated and circulated over different social media clusters irrespective of age or gender.On asking the patients “Does COVID-19 outbreak disturb your treatment”, 70/161(43.5%) answered “Yes”. Out of the 70 patients 31/88(35.2%) were males and 39/73(53.4%) were females, the risk with female gender RR (95%CI) = 1.5166 (1.0632 to 2.1633), P = 0.0216, z statistic = 2.298. On asking the patients “Does COVID-19 outbreak increased your illness”, 81/161(50.5%) answered “Yes”. On asking the patients “Did you get new pathologic symptoms due to irregularity of treatment”, 73/161(45.3%) answered “Yes”. Patients with chronic diseases were extremely influenced (pathologically and psychologically) by the COVID-19 outbreak procedures. The psychological influence was more common among women compared to men.
COVID-19, Psychological, Pathological, Saudi Arabia, Comorbidities, Chronic Diseases
Alharbi S. H. Patho-Psychological Impact of COVID-19 Outbreak in Patients with Comorbidities in Saudi Arabia. Biosc.Biotech.Res.Comm. 2021;14(1).
Alharbi S. H. Patho-Psychological Impact of COVID-19 Outbreak in Patients with Comorbidities in Saudi Arabia. Biosc.Biotech.Res.Comm. 2021;14(1). Available from: <a href=”https://bit.ly/3oJ4Qky”>https://bit.ly/3oJ4Qky</a>
Copyright © This is an Open Access Article distributed under the Terms of the Creative Commons Attribution License (CC-BY). https://creativecommons.org/licenses/by/4.0/, which permits unrestricted use distribution and reproduction in any medium, provided the original author and sources are credited.
INTRODUCTION
Coronavirus diseases 19 (COVID-19) provided a massive challenge to the whole health care system and test their available facilities exclusively for the management of patients with chronic diseases. Intensive care unit (ICU) is required for almost 20% of COVID-19 patients with multiple comorbidities and hospitalization was concomitant with a case fatality rate (CFR) of >13%. As the virus is globally spreading, nations necessitate urgent preparation of all national resources in terms of infrastructure, personnel, and other facilities to reduce the disease fatality particularly among severe cases (Gutiérrez-Ocampo et al. 2020). Epidemiological and the clinical presentations of COVID-19 infected individuals have been described but risk factors for mortality and a full clinical course of illness, comprising viral shedding, have not been well designated (Du et al. 2020 ).
This novel COVID-19 has specifically high morbidity in the elderly and comorbid populations. Uremic patients on dialysis combine an intrinsic fragility and a very frequent burden of comorbidities with a specific setting in which many patients are repeatedly treated in the same area (hemodialysis centers) (Pizzarelli et al. 2020). Since the COVID-19 has broad clinical range starting from mild sickness to acute respiratory distress syndrome (ARDS) with a high fatality, there is a necessity for further exploration to recognize primary indicators of disease severity. New recommendations stressed the fact that older patients, patients with chronic illnesses, or dyspnea must be monitored particularly in the 1st to 2nd week after the appearance of the initial symptoms (Cheong et al., 2020). Furthermore, comorbidities can significantly influence the prognosis mode of COVID-19 fate, especially among patients with CVD metabolic diseases. In such patients, the infection may lead to heart damage (Zhao et al. 2020) . However, the present study aimed to assess the pathopsychological impact of the COVID-19 outbreak in patients with comorbidities in Saudi Arabia.
MATERIAL AND METHODS
In this online questionnaire-based cross-sectional study, 161 Saudi patients with chronic diseases were conscripted during the country’s complete lockdown due to the COVID-19 outbreak (May – June 2020). The study was premeditated to assess the pathopsychological effects of the COVID-19 outbreak and its association with a lockdown on patients with chronic illnesses. A purposeful electronic questionnaire was premeditated and circulated over different social media clusters irrespective of age or gender. The pathopsychological influence of the COVID-19 outbreak on patients with chronic diseases was thereafter recognized with several pathopsychiatric measures.
Besides the demographical characteristics of the patients, the questionnaire involved the following cognitive measures; Types of chronic disease, Does COVID-19 outbreak prevent you from seeing your doctor, Does COVID-19 outbreak disturb your treatment, Does COVID-19 outbreak increased your illness, Did you get new pathologic symptoms due to irregularity of treatment, Feeling highly anxious after registering of the first case in my city, I have psychological effects from home lockdown, such as nervousness, depression, etc., During the lockdown, frequencies of being upset, because of the Corona’s, During the lockdown, frequencies of being unable to control important things in your life?, During the lockdown, frequencies of felt tense and anxious about the new epidemic around you?, During the lockdown, frequencies of felt angry about things that happened outside your control?, Social isolation led to increased depression and anxiety.
Statistical Analysis: Following the initial representation of the data in Microsoft Excel, the obtained data were then sent to the SPSS program and analyzed obtained. Statistical significant values, such as relative risk were produced applying a 95% confidence interval. A Chi-square test was done (P-value <0.05 was considered statistically significant).
Ethical Consent: The proposal for the present study was approved by the Ethical Committee at the College of Medicine, University Ha’il, Saudi Arabia. HREC 00123a/CM-UOH.04/20.
RESULTS AND DISCUSSION
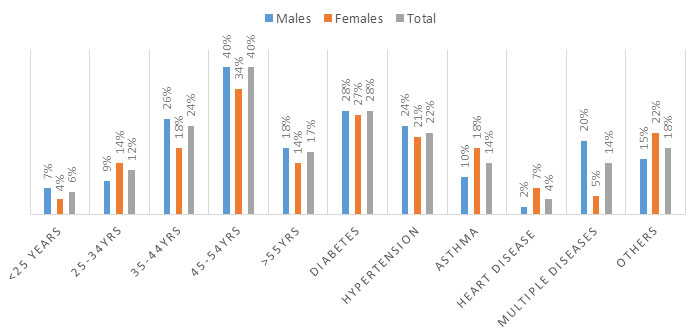
About 161 patients with different chronic diseases were assessed their ages ranging from 19 to 70 years with a mean age of 45 years. Out of the 161 patients, 88/161(55%) were males and 73/161(45%) were females. The majority of patients were at the age range 45-54 years followed 35-44 years constituting 65/161(40.4%) and 39/161(24.2%), respectively (see Table 1, Fig 1.The most frequent chronic illness was diabetes 45/161(28%) followed by hypertension 36/161(22.4%) (See Table 1, Fig 1).
Table 1. Distribution of patients by age, chronic diseases, and sex
| Variable | Males | Females | Total |
| Age | |||
| <25 years | 6 | 3 | 9 |
| 25-34 | 8 | 12 | 20 |
| 35-44 | 23 | 16 | 39 |
| 45-54 | 35 | 30 | 65 |
| >55 | 16 | 12 | 28 |
| Total | 88 | 73 | 161 |
| Types of chronic disease | |||
| Diabetes | 25 | 20 | 45 |
| Hypertension | 21 | 15 | 36 |
| Asthma | 9 | 13 | 22 |
| Heart disease | 2 | 5 | 7 |
| Multiple diseases | 18 | 4 | 22 |
| Others | 13 | 16 | 29 |
| Total | 88 | 73 | 161 |
Figure 1: Patients by age, chronic diseases, and sex
On asking the patients “Does COVID-19 outbreak prevent you from seeing your doctor“, 99/161(61.5%) answered “Yes”. Out of the 99 patients, 46/88(52.3%) were males and 53/73(72.6%) were females. The relative risk (RR) associated with females and the 95% confidence interval (95%CI) was 1.3889(1.0878 to 1.7734), P = 0.0084, z statistic = 2.635.
On asking the patients “Does COVID-19 outbreak disturb your treatment”, 70/161(43.5%) answered “Yes”. Out of the 70 patients 31/88(35.2%) were males and 39/73(53.4%) were females, the risk with female gender RR (95%CI) = 1.5166 (1.0632 to 2.1633), P = 0.0216, z statistic = 2.298. On asking the patients “Does COVID-19 outbreak increased your illness”, 81/161(50.5%) answered “Yes”. Out of the 81 patients 43/88(49%) were males and 38/73(52%) were females, the risk with female gender RR (95%CI) = 1.0653 (0.7838 to 1.4479), P = 0.6861, z statistic = 0.404. On asking the patients “Did you get new pathologic symptoms due to irregularity of treatment”, 73/161(45.3%) answered “Yes”. Out of the 73 patients 43/88(49%) were males and 30/73(41%) were females, the risk with male gender RR (95%CI) = 1.1890 (0.8396 to 1.6839), P = 0.3295, z statistic = 0.975.
Table 2. COVID-19 outbreak effects on regular treatment of patients by sex
| Variable | Males (n=88) | Females (n=73) | Total (n=161) |
| Does COVID-19 outbreak prevent you from seeing your doctor | |||
| Yes | 46 | 53 | 99 |
| No | 42 | 20 | 62 |
| Does COVID-19 outbreak disturb your treatment | |||
| Yes | 31 | 39 | 70 |
| No | 57 | 34 | 91 |
| Does COVID-19 outbreak increased your illness | |||
| Yes | 43 | 38 | 81 |
| No | 45 | 35 | 80 |
| Did you get new pathologic symptoms due to irregularity of treatment | |||
| Yes | 43 | 30 | 73 |
| No | 45 | 43 | 88 |
Table 3, summarized the distribution of the COVID-19 outbreak effects on the regular treatment of patients by age. On asking the patients “Does COVID-19 outbreak prevent you from seeing your doctor”, out of the 99 patients answered “Yes”, 33/99(33.3%), 24/99(24.2%), and 21/99(21.2%) were aged 45-54 years, >55 years, and 35-44 years, correspondingly.
On asking the patients “Does COVID-19 outbreak disturb your treatment”, out of the 70 patients answered “Yes”, 27/70(38.6%), 15/70(21.4%), and 14/70(20%) were aged 45-54 years, >55 years, and 35-44 years, one-to-one. On asking the patients “Does COVID-19 outbreak increased your illness”, out of the 81 patients answered “Yes”, 33/81(40.7%), and 20/81(24.7%),) were aged 45-54 years, and 35-44 years, respectively. On asking the patients “Did you get new pathologic symptoms due to irregularity of treatment”, out of the 73 patients answered “Yes”, 28/73(38.4%), and 17/73(23.3%),) were aged 45-54 years, and 35-44 years, respectively.
Table 3. COVID-19 outbreak effects on regular treatment of patients by age
| Variable | <25years | 26-34 | 35-44 | 45-54 | >55 | Total |
| Does COVID-19 outbreak prevent you from seeing your doctor | ||||||
| Yes | 5 | 16 | 21 | 33 | 24 | 99 |
| No | 4 | 4 | 18 | 32 | 4 | 62 |
| Does COVID-19 outbreak disturb your treatment | ||||||
| Yes | 4 | 10 | 14 | 27 | 15 | 70 |
| No | 5 | 10 | 25 | 38 | 13 | 91 |
| Does COVID-19 outbreak increased your illness | ||||||
| Yes | 6 | 10 | 20 | 33 | 12 | 81 |
| No | 3 | 10 | 19 | 32 | 16 | 80 |
| Did you get new pathologic symptoms due to irregularity of treatment | ||||||
| Yes | 7 | 9 | 17 | 28 | 12 | 73 |
| No | 2 | 11 | 22 | 37 | 16 | 88 |
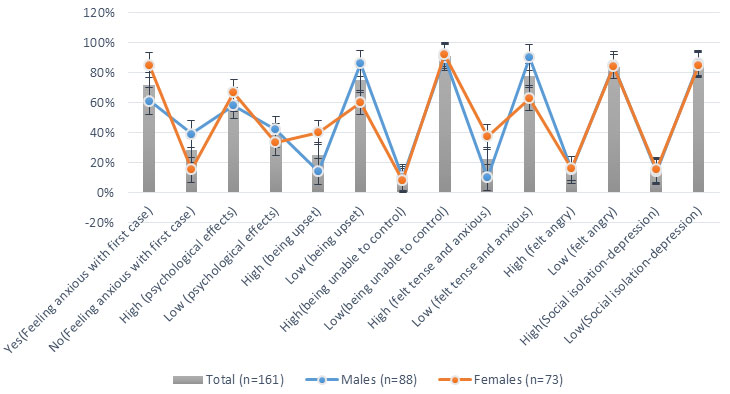
Table 4, Fig 2, summarized the distribution of COVID-19 outbreak by gender and psychological effects. On asking the patients “Feeling highly anxious after registering of the first case in my city”, 116/161(72%) answered “Yes” of whom 54/88(61.4%) were males and 62/73(85%) were females. The risk associated with female gender was; RR (95%CI) = 1.3841(1.1424 to 1.6769), P = 0.0009, z statistics = 3.320.
On asking the patients “I have psychological effects from home lockdown, such as nervousness, depression, etc.”, 100/161(62%) responded “high” of whom 51/88(58%) were males and 49/73(67%) were females. The risk associated with female gender was; RR (95%CI) = 1.1582 (0.9114 to 1.4719), P = 0.2297, z statistics = 1.201.On asking the patients “During the lockdown, frequencies of being upset, because of the Corona’s”, 41/161(25.5%) responded “high” of whom 12/88(13.6%) were males and 29/73(40%) were females. The risk associated with female gender was; RR (95%CI) = 2.9132 (1.6037 to 5.2920), P = 0.0004, z statistics = 3.511.On asking the patients “During the lockdown, frequencies of being unable to control important things in your life?”, 15/161(9.3%) responded “high” of whom 9/88(10.2%) were males and 6/73(8.2%) were females.
On asking the patients “During the lockdown, frequencies of felt tense and anxious about the new epidemic around you?”, 36/161(22.4%) responded “high” of whom 9/88(10.2%) were males and 27/73(37%) were females. The risk associated with female gender was; RR (95%CI) = 3.6164 (1.8182 to 7.1931), P = 0.0002, z statistics = 3.664.On asking the patients “During the lockdown, frequencies of felt angry about things that happened outside your control?”, 25/161(15.5%) responded “high” of whom 13/88(14.8%) were males and 12/73(16.4%) were females. On asking the patients “Social isolation led to increased depression and anxiety”, 23/161(14.3%) responded “high” of whom 12/88(13.6%) were males and 11/73(15%) were females.
Table 4. COVID-19 outbreak by gender and psychological effects
| Variable | Males (n=88) | Females (n=73) | Total (n=161) |
| Feeling highly anxious after registering of the first case in my city | |||
| Yes | 54 | 62 | 116 |
| No | 34 | 11 | 45 |
| I have psychological effects from home lockdown, such as nervousness, depression, etc. | |||
| High | 51 | 49 | 100 |
| Low | 37 | 24 | 61 |
| During the lockdown, frequencies of being upset, because of the Corona’s | |||
| High | 12 | 29 | 41 |
| Low | 76 | 44 | 120 |
| During the lockdown, frequencies of being unable to control important things in your life? | |||
| High | 9 | 6 | 15 |
| Low | 79 | 67 | 146 |
| During the lockdown, frequencies of felt tense and anxious about the new epidemic around you? | |||
| High | 9 | 27 | 36 |
| Low | 79 | 46 | 125 |
| During the lockdown, frequencies of felt angry about things that happened outside your control? | |||
| High | 13 | 12 | 25 |
| Low | 75 | 61 | 136 |
| Social isolation led to increased depression and anxiety | |||
| High | 12 | 11 | 23 |
| Low | 76 | 62 | 138 |
Figure 2: COVID-19 outbreak by gender and psychological effects
The highest COVD-19 related fatality was commonly occurring among individuals with comorbidities. COVID-19 outbreak affects patients with chronic diseases in several ways including psychological effects, chronic disease evolution due to interruption of follow up or loss of treatment optimization, loss of physical activity, increased consumption of avoidable nutrients which may be harmful with a particular illness, etc. Consequently, the present study aimed to evaluate the pathopsychological impact of the COVID-19 outbreak in patients with comorbidities in Saudi Arabia.
In the current study, about 61.5% of the patients claimed that COVID-19 associated procedures prevented them from seen their doctors, and women were significantly affected (P = 0.0084) compared to men. Although there limited data on follow up patients with chronic diseases during the COVID-19 outbreak, unfavorable outcomes involving disease progression and increased fatality risk were witnessed (Sala et al., 2020). About 43.5% of the patients indicated that the lockdown procedures disturb their treatment in one way or another. Females were also significantly (P = 0.0216) affected than males. Moreover, about 50.5% of the patients experienced increased illness liability during the lockdown. A recent investigation in this context has shown that COVID-19 is an independent risk factor for chronic comorbidity fatality upsurge (Green et al. 2020).
A recent data analysis in this context showed that considerable morbidity and mortality associated with chronic comorbidity among COVID-19 patients, particularly among those with cardiovascular (hypertension), metabolic (diabetes) diseases even greater than chronic pulmonary diseases, and the fatality increases with the severity of the preexistent chronic illness (Lu et al., 2020). Moreover, approximately 45.3% of the patients in this series of patients reported: “new pathologic symptoms due to the irregularity of treatment”. Limited access to diagnostic services and optimum treatment constituents represent the most important issues for patients with chronic diseases during the lockdown during the COVID-19 pandemic. Inadequate aptitude to control together disease severity and the existence of medication adversative special effects, and significantly affect the patient (Gutiérrez-Ocampo et al. 2020).
The findings of the present study have shown that females and elderly people were more likely to be affected path psychologically by COVID-19 associated events. This necessitates future plans for this section of the population. Stress, and anxiety, and depression features were commonly observed indicators among patients with chronic diseases in the current series. Similar findings were recently reported from Spain in a study assessed levels of stress anxiety and depression during the COVID-19 pandemic. Higher symptoms were more frequent among younger persons with chronic illnesses compared to the general population. The symptoms of stress, anxiety, and depression increased with the elevation of lockdown levels (Idoiaga-Mondragon et al., 2020).
However, the findings in the present study seemed to be similar to those reported globally (Ventriglio et al., 2020). This necessitates future strategies for patients with comorbidities including psychological intervention and planned follow-up. Although the present study has some limitations including its cross-sectional setting, it provided valuable information, which may assist for future management of patients with chronic comorbidities in situations of pandemic diseases.
CONCLUSION
Patients with chronic diseases were extremely influenced (pathologically and psychologically) by the COVID-19 outbreak procedures. The psychological influence was more common among women compared to men. Future strategies for patients with comorbidities including psychological intervention and planned follow-up are deemed important.
Conflict of Interest: Author declares no conflicts of interests to disclose.
REFERENCES
Basile C, Combe C, Pizzarelli et al. (2020). Recommendations for the prevention, mitigation and containment of the emerging SARS-CoV-2 (COVID-19) pandemic in hemodialysis centers. Nephrol Dial Transplant. GFAA 069.
Docherty AB, Harrison EM, Green CA, et al. (2020). Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterization Protocol: prospective observational cohort study. BMJ. 369:m1985. doi:10.1136/bmj.m1985
Goh KJ, Choong MC, Cheong EH, et al. (2020). Rapid Progression to Acute Respiratory Distress Syndrome: Review of Current Understanding of Critical Illness from COVID-19 Infection. Ann Acad Med Singapore. 49(1):1–9.
Li B, Yang J, Zhao F, et al. (2020). Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin Res Cardiol. 10.1007/s00392-020-01626-9. doi:10.1007/s00392-020-01626-9.
Liu H, Chen S, Liu M, Nie H, Lu H. (2020). Comorbid Chronic Diseases are Strongly Correlated with Disease Severity among COVID-19 Patients: A Systematic Review and Meta-Analysis. Aging Dis. 11(3):668-678. doi:10.14336/AD.2020.0502.
Ozamiz-Etxebarria N, Dosil-Santamaria M, Picaza-Gorrochategui M, Idoiaga-Mondragon N. (2020). Stress, anxiety, and depression levels in the initial stage of the COVID-19 outbreak in a population sample in the northern Spain. Niveles de estrés, ansiedad y depresión en la primera fase del brote del COVID-19 en una muestra recogida en el norte de España. Cad Saude Publica. 36(4):e00054020. doi:10.1590/0102-311X00054020.
Rodriguez-Morales AJ, Cardona-Ospina JA, Gutiérrez-Ocampo E, et al. (2020) Clinical, laboratory and imaging features of COVID-19: A systematic review and meta-analysis. Travel Med Infect Dis. 10162.
Tadic M, Cuspidi C, Sala C. (2020). COVID-19 and diabetes: Is there enough evidence?. J Clin Hypertens (Greenwich). 22(6):943-948. doi:10.1111/jch.13912.
Torales J, O’Higgins M, Castaldelli-Maia JM, Ventriglio A. (2020). The outbreak of COVID-19 coronavirus and its impact on global mental health. Int J Soc Psychiatry. 66(4):317-320. doi:10.1177/0020764020915212
Wong AW, Fidler L, Marcoux V, et al. (2020) Practical Considerations for the Diagnosis and Treatment of Fibrotic Interstitial Lung Disease During the COVID-19 Pandemic. Chest. S0012-3692(20)30756-X. doi:10.1016/j.chest.2020.04.019.
Zhou F, Yu T, Du R, et al. (2020 Mar). Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study Lancet. 28;395(10229):1038.