Department of Orthodontics, Saveetha Dental College and Hospital, Chennai, India.
Corresponding author email: akriti.tiwari5@gmail.com
Article Publishing History
Received: 19/07/2021
Accepted After Revision: 18/09/2021
Facial type of any individual comprises variations in the skeleton structures and is pertinent to genetic and environmental factors. This may influence the palatal bone thickness, for instance, palate can be deep and narrow for vertical growers while wide and shallow for horizontal growers. Therefore, the aim of the present study was to evaluate palatal bone thickness in different growth patterns in the Dravidian population. 30 CBCTs were retrieved and classified into three groups according to the growth patterns- 10 horizontal growth pattern (<30°), 10 average growth pattern (≃32∓2°) and vertical growth pattern (>30°). The growth pattern was determined based on the SN.GoGn angle. The measurements were made at the midline of the palate and 4 mm sequentially posterior from the standardized landmark. The measurements were made in the anterior, middle and posterior region of the palate.
These measurements in the CBCT were made with the help of CS 3D imaging software. For bone height assessment, linear measurements were performed in a sagittal plane using the ruler tool of the software. One-way ANOVA was performed to evaluate the mean palatal thickness of bone in horizontal growth pattern, average growth pattern and vertical growth pattern in IBM SPSS statistics 23. On performing one-way ANOVA, it was observed that there was a statistically significant difference in the mean of the palatal bone thickness in the anterior of vertical growers. Within the limitations of the present study, it can be concluded that the placement of palatal implants in vertical growers should be done with caution.
Growth Patterns, Miniscrews, Palatal Bone Thickness
Tiwari A, Dinesh SP. S. Palatal Bone Thickness in Different Growth Patterns of Dravidian Population Using Cone-Beam Computed Tomography Systems. Biosc.Biotech.Res.Comm. 2021;14(3).
Tiwari A, Dinesh SP. S. Palatal Bone Thickness in Different Growth Patterns of Dravidian Population Using Cone-Beam Computed Tomography Systems. Biosc.Biotech.Res.Comm. 2021;14(3). Available from:<ahref=”https://bit.ly/2U6JaFT“>https://bit.ly/2U6JaFT</a>
Copyright © This is an Open Access Article distributed under the Terms of the Creative Commons Attribution License (CC-BY). https://creativecommons.org/licenses/by/4.0/, which permits unrestricted use distribution and reproduction in any medium, provided the original author and sources are credited.
INTRODUCTION
The development of mini-implants has gained widespread recognition in the orthodontic field due to their temporary absolute skeletal anchorage without impeding the movement of the orthodontic tooth, as well as their small diameter, which allows easy placement in narrow interdental spaces (Mo et al. 2010). Mini-implants are used in numerous regions, such as, interradicular, infrazygomatic crest, buccal shelf, ramus and palate.
Although mini-implants can be placed buccally or palatally, palatal mini-implants are preferred due to their superior stability and have good quality as well as quantity of bone (Baumgaertel 2009; Mohammed et al. 2018; Park and Shin 2020). Mineral content of bone matrix and heterogeneity of mineralization of paramount importance for quality of bone as well as stability of mini-implants. Moreover, the quality of bone is influenced by several factors, such as heredity, race, environment, nutrition and lifestyle (Frost 1990; Sommerfeldt and Rubin 2002; Borgen et al. 2020).
The success of any mini-implant depends on the degree to which it integrates mechanically and biologically with the host bone. They are commonly inserted in the anterior region of palate, mid-palatal area, and posterior region of palate (Arcuri et al. 2007; Yadav et al. 2018). The advantage of placing miniscrew in these areas, have no significant anatomical structures, such as nerves, blood vessels, or roots, that interfere with the placement.
Additionally, the palatal region is keratinized thereby causing less irritation to the tissue (Ryu et al. 2012; Burhan 2013; Kinzinger, Hourfar and Lisson 2021). Karagkiolidou et al. (2013) reported that success rate of 98% is observed in the anterior region of the palate. Even so, Manni et al. (2011) revealed that failure rate was higher in females as compared to males (Deguchi et al. 2006; Gracco et al. 2008; Manni et al. 2011; Karagkiolidou et al. 2013; Uribe et al. 2015; Kinzinger, Hourfar, and Lisson 2021).
These mini-implants are widely used for molar intrusion, molar protraction, anterior segment protraction and retraction, and en-masse retraction (Deguchi et al. 2006; Gracco et al. 2008; Uribe et al. 2015). Facial type of an individual any individual comprises variations in the skeleton structures and it is pertinent to genetic and environmental factors. They have direct association with craniofacial growth and are divided into three groups-brachyfacial, mesofacial and dolichofacial. In brachyfacial, there is a tendency of horizontal growth pattern. Mesofacial has balanced growth of all facial thirds and dolichofacial has predisposition to vertical growth patterns (McNamara 1981; Cassidy et al. 1998; Kageyama et al. 2006).
This may influence the palatal bone thickness, for instance, palate can be deep and narrow for vertical growers while wide and shallow for horizontal growers (Linder-Aronson 1983; Chen 2021). The amount of available bone for insertion of miniscrews is a limiting factor for orthodontic treatment requiring skeletal anchorage. Taking these factors into account, the aim of the present study was to evaluate palatal bone thickness in different growth patterns in the Dravidian population.
MATERIAL AND METHODS
This retrospective study retrieved CBCTs of subjects who were referred for orthodontic treatment. The CBCTs was obtained using orthophos SL 3D dentsply sirona. Inclusion criteria was as follows: no previous orthodontic treatment, angle’s class I malocclusion; permanent dentition; mild to moderate crowding. Patients having carious, decayed tooth, deciduous dentition periodontal disease with alveolar bone loss, traumatic dental injury, impacted teeth and systemic diseases was excluded from the study.
After applying the inclusion and exclusion criteria, 30 CBCTs were retrieved and classified into three groups according to the growth patterns- 10 horizontal growth pattern (<30°), 10 average growth pattern (≃32∓2°) and vertical growth pattern (>30°). The growth pattern was determined based on the SN.GoGn angle. The region of interest was determined using the orientation lines of the plane. In the axial view, the midsagittal plane and the maxillary first premolar region was defined, superimposing the sagittal and coronal lines, respectively (Fig 1). Followed by, line joining the middle of the distal bony margin of the incisive foramen and the posterior nasal spine (PNS), midsagittal view (Fig 2).
This was taken as the standardized landmark to locate the centre of palate. Subsequently, the measurements were made at the midline of the palate and 4 mm sequentially posterior from the standardized landmark (Fig 3). The measurements were made in the anterior, middle and posterior region of the palate.
Figure 1: Represents the axial view wherein the midsagittal plane and the maxillary first premolar region was defined, superimposing the sagittal and coronal lines, respectively. (Image obtained from CS-3D imaging software)
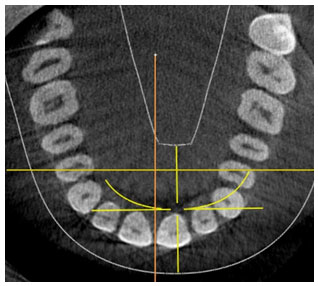
Figure 2: Represents the sagittal view wherein the line joining the middle of the distal bony margin of the incisive foramen and the posterior nasal spine (PNS) was taken as the standardized landmark to locate the centre of palate. (Image obtained from CS-3D imaging software)
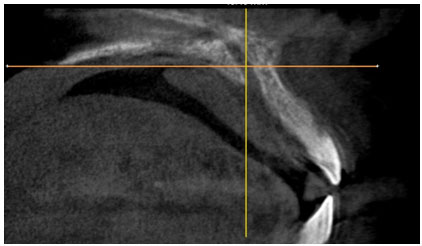
Figure 3: Represents the measurements made at the midline of the palate and 4 mm sequentially posterior from the standardized landmark. (Image obtained from CS-3D imaging software)
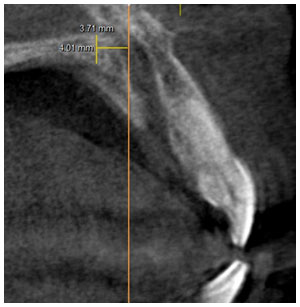
These measurements in the CBCT were made with the help of CS 3D imaging software. For bone height assessment, linear measurements were performed in a sagittal plane using the ruler tool of the software. For statistical analysis, one-way ANOVA was performed to evaluate the mean palatal thickness of bone in horizontal growth pattern, average growth pattern and vertical growth pattern in IBM SPSS statistics 23.
RESULTS AND DISCUSSION
On performing one-way ANOVA, it was observed that there was a statistically significant difference in the mean of the palatal bone thickness in the anterior of vertical growers (Table 1).
Table 1. Represents the mean difference of the palatal bone thickness in different growth patterns in anterior, middle and posterior region.
| Region Growth pattern | Sum of squares | df | Sig |
| Anterior Vertical
Average Horizontal |
2.47 | 2 | 0.03 |
| Middle Vertical
Average Horizontal |
0.15 | 2 | 0.28 |
| Posterior Vertical
Average Horizontal |
2.31 | 2 | 0.08 |
Introduction of skeletal anchorage in orthodontics has enabled orthodontists to facilitate tooth movement in all the three planes efficiently. Above all, palate is the desirable region for mini-implants placement for skeletal anchorage. Several previous studies have attempted to examine the thickness of the palatal bone using various direct and radiological measurements ( Henriksen et al. 2003; Jung et al. 2011; Kim 2014).
In our study, the thickness of the palatal bone was assessed using CBCT. This information is helpful during orthodontic treatment to determine the appropriate length of the mini screw implant and to identify sites for mini screw implant placement with sufficient bone available, especially in the palatal areas of patients.
Information pertaining to palatal bone thickness supports the selection of the ideal miniscrew implant placement sites and miniscrew implant length to ensure adequate retention and to avoid damaging vital structures. Information on the thickness of the palatal bone will help in choosing the ideal locations for mini screw placement and the length of the implant to ensure adequate retention and avoid damage to vital structures (Awadhi et al. 2018; Fallahi et al. 2021).
The growth trend of the one-third face determines the patient’s face type and the direction of its development, which can be more horizontal, more balanced, or vertical. In this sense, the shape of palate is one of the individual characteristics of the face typology and can have different morphologies (Fallahi et al. 2021). In the present study, there was a statistically significant difference observed in the mean palatal bone thickness in the anterior region of the vertical growers.
This finding is in partial agreement with the study conducted by Esteves and Bommarito (2007), wherein it was observed that patients with vertical growth patterns have narrow and deep palate but they did not mention about the palatal thickness as well as the region (Esteves and Bommarito 2007). Similar finding was reported by Poon et al. (2005) wherein it was observed that hyperdivergent patients had bone availability is lower in the anterior and middle region (Poon et al. 2015; Fallahi et al. 2021). Limitations of the present study was limited sample size.
CONCLUSION
The findings of the present study conclude that the placement of palatal implants in vertical growers should be done with caution. These results could be helpful for clinicians to improve the successful use of temporary palatal anchors.
Acknowledgements: The study was supported by the constant guidance of Dr Aravind Kumar, Professor, Head of Department, Department of orthodontics and dentofacial orthopaedics.
Conflict of Interests: Authors declare no conflicts of interest to disclose.
Ethical Clearance Statement: The Current Research Work Was Ethically Approved by the Institutional Review Board (IRB) of Saveetha Dental College and Hospital, Chennai, India.
REFERENCES
Arcuri, C., Muzzi, F., Santini, F., et al. (2007). Five years of experience using palatal mini-implants for orthodontic anchorage. Journal of oral and maxillofacial surgery 65(12) 2492-2497.
Alkadhimi, A. and Al-Awadhi, E.A. (2018) Miniscrews for orthodontic anchorage: a review of available systems. Journal of orthodontics 45(2) 102-114.
Baumgaertel, S., (2009) Quantitative investigation of palatal bone depth and cortical bone thickness for mini-implant placement in adults. American Journal of Orthodontics and Dentofacial Orthopedics 136(1) 104-108.
Burhan, A.S., (2013) Combined treatment with headgear and the Frog appliance for maxillary molar distalization: a randomized controlled trial. The Korean Journal of Orthodontics 43(2) 101-109.
Borgen, T.T., (2020) Trabecular bone score and vertebral fracture assessment in patients with fragility fractures.
Deguchi, T., Nasu, M., Murakami, K., et al. (2006). Quantitative evaluation of cortical bone thickness with computed tomographic scanning for orthodontic implants. American Journal of Orthodontics and Dentofacial Orthopedics, 129(6), 721-e7.
Esteves, A. and Bommarito, S., (2007) Avaliação da profundidade do palato e das dimensões do arco dentário superior em indivíduos com má oclusão e diferentes tipos faciais. Revista Dental Press de Ortodontia e Ortopedia Facial 12 84-98.
Frost, H.M., (1990) Skeletal structural adaptations to mechanical usage (SATMU): 2. Redefining Wolff’s law: the remodeling problem. The anatomical record 226(4) 414-422.
Fallahi, H.R., Zandian et al. (2021) Facial Analysis and Clinical Evaluation Charts. In Integrated Procedures in Facial Cosmetic Surgery. Springer Cham 35-58.
Gracco, A., Lombardo, L., Cozzani, M. et al. (2008). Quantitative cone-beam computed tomography evaluation of palatal bone thickness for orthodontic miniscrew placement. American Journal of Orthodontics and Dentofacial Orthopedics, 134(3), 361-369.
Henriksen, B., Bavitz, B., Kelly, B. et al. (2003). Evaluation of bone thickness in the anterior hard palate relative to midsagittal orthodontic implants. International Journal of Oral & Maxillofacial Implants, 18(4).
Jung, B.A., Wehrbein, H., Heuser, L. et al. (2011). Vertical palatal bone dimensions on lateral cephalometry and cone‐beam computed tomography: implications for palatal implant placement. Clinical oral implants research, 22(6), 664-668.
Kageyama, T., Domínguez-Rodríguez, G.C., Vigorito, J.W. et al. (2006). A morphological study of the relationship between arch dimensions and craniofacial structures in adolescents with Class II Division 1 malocclusions and various facial types. American journal of orthodontics and dentofacial orthopedics, 129(3), 368-375.
Karagkiolidou, A., Ludwig, B., Pazera, P., et al. (2013). Survival of palatal miniscrews used for orthodontic appliance anchorage: a retrospective cohort study. American Journal of Orthodontics and Dentofacial Orthopedics, 143(6), 767-772.
Kinzinger, G.S.M., Hourfar, J. and Lisson, J.A., (2021) Efficiency of the skeletonized Pendulum K appliance for non-compliance maxillary molar distalization. Journal of Orofacial Orthopedics/Fortschritte der Kieferorthopädie 1-12.
Manni, M. Cozzani, F. Tamborrino et al. (2011) Factors influencing the stability of miniscrews. A retrospective study on 300 miniscrews. The European Journal of Orthodontics 33(4) 388-395.
Mohammed, H., Wafaie, K., Rizk, M.Z., et al. (2018). Role of anatomical sites and correlated risk factors on the survival of orthodontic miniscrew implants: a systematic review and meta-analysis. Progress in orthodontics 19(1) 1-18.
Park, J.H. and Shin, K., (2020). An Overview of Clinical Applications for Temporary Anchorage Devices (TADs). Temporary Anchorage Devices in Clinical Orthodontics, 1-15.
Poon, Y.C., Chang, H.P., Tseng, Y.C., et al. (2015). Palatal bone thickness and associated factors in adult miniscrew placements: A cone-beam computed tomography study. The Kaohsiung journal of medical sciences, 31(5), 265-270.
Ryu, J.H., Park, J.H., Thu, T.V.T., et al. (2012). Palatal bone thickness compared with cone-beam computed tomography in adolescents and adults for mini-implant placement. American journal of orthodontics and dentofacial orthopedics, 142(2): 207-212.
Sommerfeldt, D. and Rubin, C., (2001) Biology of bone and how it orchestrates the form and function of the skeleton. European Spine Journal 10(2): S86-S95.
Uribe, F., Mehr, R., Mathur, A., et al. (2015). Failure rates of mini-implants placed in the infrazygomatic region. Progress in orthodontics, 16(1): 1-6.
Yadav, S., Sachs, E., Vishwanath, M., et al. (2018). Gender and growth variation in palatal bone thickness and density for mini-implant placement. Progress in orthodontics, 19(1):1-10.


