1BDS, M.Sc, Department of Physiology, AIIMS, New Delhi, India
2M.Sc., Department of Physiology, AIIMS, New Delhi, India
2PhD, Department of Life Sciences , IGNOU, New Delhi,India
3MDS, Department of Orthodontics and dentofacial deformities, CDER, AIIMS, New Delhi, India
4MD, Department of Physiology, AIIMS, New Delhi, India
Corresponding author email: renuaiims28@gmail.com
Article Publishing History
Received: 05/11/2019
Accepted After Revision: 25/12/2019
Pain is a complex sensory experience and often accompanies orthodontic conditions and interferes with its management. Orthodontic pain induced by application of orthodontic appliances and traction forces on mal-occluded teeth, is typically transient (peaks in 24 hours and subsides within a week), alters sensory perception and normal motor activities such as chewing and talking. The present study was aimed to record thermal sensitivity and motor activity of masseter muscle in patients undergoing fixed orthodontic therapy at 3 time points i.e. before start of treatment (Day 0), at 24 hours (Day 2) and a after a week (Day 7). Pain rating by visual analog scale, Quantitative sensory testing (thermal detection, pain threshold and pain tolerance for both cold and hot stimuli) and surface electromyography (amplitude and time to fatigue) were recorded for masseter muscle. D’Agostino-Pearson and Friedman’s test were applied for determining normality and for comparisons respectively. Twenty eight patients (17 males, 11 females) mean age(17.88 ± 3.92 years) were recruited from Orthodontics and maxillofacial deformity department. We found significant changes in cold pain perception and cold pain tolerance at Day 2, when compared to Day 0 and Day 7. At Day 2 amplitude of maximum voluntary contraction and time to fatigue were significantly lower than Day 0. All other parameters such as thermal thresholds were comparable at all the time points.The findings suggest that orthodontic procedures causes transient sensitization of the trigeminal nociceptive system. Quantitative assessment of somatosensory and motor function may help in better understanding of time kinetics and mechanism of orthodontic pain in order to plan and modify orthodontic treatment based on patients thresholds and responses.
Electromyography, Orthodontic pain, Peripheral sensitization, Quantitative sensory testing.
Arya S, Nanda S, Jha A, Duggal R, Bhatia R. Orthodontic Pain Induced Sensitization of Trigeminonociceptive System of Patients Undergoing Fixed Orthodontic Treatment. Biosc.Biotech.Res.Comm. 2019;12(4).
Arya S, Nanda S, Jha A, Duggal R, Bhatia R. Orthodontic Pain Induced Sensitization of Trigeminonociceptive System of Patients Undergoing Fixed Orthodontic Treatment. Biosc.Biotech.Res.Comm. 2019;12(4). Available from: https://bit.ly/33zYd9M
Copyright © Arya et al., This is an open access article distributed under the terms of the Creative Commons Attribution License (CC-BY) https://creativecommns.org/licenses/by/4.0/, which permits unrestricted use distribution and reproduction in any medium, provide the original author and source are credited.
INTRODUCTION
Pain is an unpleasant somatic and emotional experience associated with actual or potential tissue damage. Pain can also be acute or chronic in nature, it includes sensations evoked by, and reactions to noxious stimuli. Pain is a complex experience and often accompanies orthodontic procedures. Orthodontic pain is the most common complaint resulting from application of orthodontic forces for correction of malocclusion and is a major cause of reduced patient compliance. Orthodontic forces cause movement of mal-aligned teeth that results in an inflammatory process in the periodontal ligament (PDL). It has been correlated with the release and presence of various substances, such as substance P histamine, enkephalin, dopamine, serotonin, glycine, glutamate gamma-amino butyric acid, PGEs, leukotriens, and cytokines. Malocclusion is not only esthetically but also functionally compromising. Orthodontic grip forces induce orthodontic pain which not only alters sensory perception (feelings of pressure, tension and soreness of the teeth) but also makes normal muscular activities difficult for the patients, (Hosseinzadeh et al., 2016, Topolski et al., 2018).
In a previous study to check sensitization of teeth, the various discomforts experienced by patients after appliance placement are described by them as feelings of pressure, tension, soreness of the teeth, and pain (Ngan et al. , 1989). In another study pain escalated 2-4 hours post application of appliances and traction forces, reached peak levels in 24 hours and subsides within a week (Bergius et al., 2000). Despite some studies there is a paucity of research that has systematically explored the changes in the nociception, somatosensory and muscular activity at extra-oral sites during fixed orthodontic treatment. The presence of widespread sensitization is still unclear in the surrounding muscles. More over some studies suggest changes in motor activity which is inferred as a protective reflex following traction. (Scheurer et al. 1996, Michelotti et al. 1999, Bondemark et al., 2004). The study of both somatosensory and motor function helps in understanding the underlying pathophysiological mechanisms of orthodontic pain.
Quantitative sensory testing (QST) is a non-invasive psychophysical testing method in which different modalities (thermal, mechanical, electrical, and chemical) are applied to different tissues (skin, mucosa, muscles and joints) and perception threshold are noted. Electromyography (EMG) is a common electrodiagnostic technique used by orthodontists for evaluating and recording the electrical activity of the muscles. An electromyographic EMG study performed to evaluate the motor and sensory changes associated with separator placement, showed a decrease in motor output as well as pressure pain threshold in muscles of mastication. (Michelotti et al.,1999)In the present study we explored sensory and motor aspects of masseter function in patients undergoing fixed orthodontic therapy.
MATERIAL AND METHODS
Patient characteristics: Twenty patients (11 males and 9 females) of different classes of dental malocclusion (Angle’s Class I, II and III) were recruited from the Orthodontics and dentofacial deformities department of Centre for Dental Education and Research, All India Institute of Medical Sciences (AIIMS). The mean age of subjects was 17.88 ± 3.92 years. All tests were performed at Pain Research and TMS Laboratory, in Department of Physiology at AIIMS, New Delhi. Consent form for procedures, which were further approved by the Institute’s ethical committee (IECPG-248/30.03.2016, RT-17/27.04.2016) was taken from the subjects and thereafter the tests were performed. Non-surgical cases with dental malocclusion aged 13-25 years (for <18 years of patients, guardian was there) with normal growth pattern (FMA-25º-27º) and normal masseter muscle activity were recruited. Patients with current orofacial inflammatory conditions, history of dental or orthodontic treatment 3 months prior to the study, taking medications and any neurological or metabolic disorders were excluded from the study. Quantitative Sensory Testing and Electromyography tests were done on the area overlying masseter muscle at 3 time points once before the start of fixed orthodontic therapy (Baseline, Day 0), then 24 hours after application of appliances and traction forces (Day 2) and finally; after a week (Day 7). At first visit history was taken (both dental and medical), thermal thresholds and motor activity of masseter were recorded. At second visit, (Day 2) patient was asked to report pain experience and the sensory and motor tests were repeated. At third visit, (Day 7) re-evaluation of pain, sensory and motor activity was done.
The study was conducted in a silent, isolated room with an ambient temperature between 21 and 25°C. During the QST, participants were instructed to close their eyes and the tests were performed according to the standard protocol. The QST included the following variables: Thermal detection thresholds (Cold detection threshold-CDT, Warm detection threshold-WDT), pain and pain tolerance thresholds (Cold Pain threshold-CPT, Cold pain tolerance threshold-CPTT; Hot Pain threshold-, HPT, Hot Pain Tolerance threshold-HPTT). The thermal thresholds were recorded using a thermode (30 mm X 30 mm) probe over left masseter muscle and first web space of left hand (as a reference site). (Fig 1)The CDT and the WDT were always measured first, followed by the CPT, HPT, CPTT and HPTT. The baseline temperature was set at 32°C, the temperature increased or decreased, at a rate of 1°C/s, to the lower limit of 0°C or to the upper limit of 50°C, respectively. Subjects were instructed to press a button as soon as they perceived the respective thermal sensation of cold, heat, cold pain, and heat pain and when they could no longer tolerate the cold or hot stimulus.
BioPac, Student laboratory system, BSL Pro (V 3.6.7 model), with pre-gelled
disposable Ag-AgCI cup electrodes (Biopac, UK) were utilized to record surface
EMG signal from masseter muscle, connected to the MP30 unit through smart
sensors. Recordings were done at rest and at maximum voluntary contraction
(MVC) and the results were expressed as amplitude and time to fatigue.
Data Extraction
Data acquisition was done in BioPac, student laboratory system, BSL Pro and Neurosensory analyser TSA-II and extraction was done in MS Office Microsoft
Excel 2013.
Statistical analysis
Descriptive statistics were used to summarize all measurements. The mean and standard deviation values of pain rating (VAS), motor activity (amplitude and time to fatigue at maximum voluntary contraction) were calculated and compared using one way ANOVA. Data was found to be non-parametric for QST data (thermal thresholds- CDT, WDT, CPT, HPT, CPTT, HPTT) at masseter and at hand but parametric for EMG data. Friedman’s test with repeated measures was used to assess the time effects and represented as median with range.
RESULTS AND DISCUSSION
The results of 20 patients are represented. Pain, sensory and motor evaluations were done at all the 3 time points (Day0, Day 2 and Day 7 respectively)
VAS rating for Pain
At baseline the patients were pain free (VAS=0), the pain intensity reached a peak at 24 h (VAS = 5.3, range: 1.9–8.9) and thereafter there was a gradual reduction in the pain intensity by Day 7 (VAS = 1.5; range: 0.5–2.6).
QST findings
We found significant changes in cold detection thresholds (CDT), cold pain thresholds (CPT) and cold pain tolerance thresholds (CPTT) at day 2 at masseter but at day 7 they were comparable to their respective baseline (day 0) values. We found cold detection (p= 0.004) and cold pain tolerance thresholds (p= 0.0001) to be significantly higher when patient had maximum pain i.e at day 2 compared to baseline when patient was pain free. Cold pain threshold decreased significantly at day 2 (p=0.003). Thermal detection, pain and pain tolerance thresholds for the hot stimuli were all comparable at the 3 time points.
EMG findings
The motor activity changes of masseter at maximum voluntary contraction when recorded at 3 time points. Amplitude (at rest) at baseline was 1.22 ± 0.76 mV and on Day 2 it was significantly reduced to 0.53 ± 0.39 mV, on Day 7 the EMG activity at rest and also at MVC were comparable to baseline values.
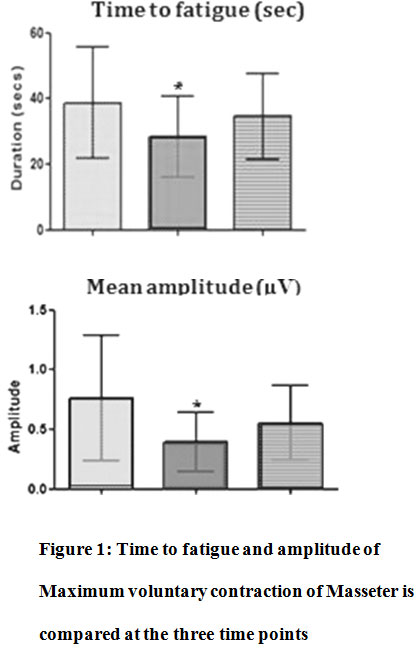 |
Figure 1: Time to fatigue and amplitude of Maximum voluntary contraction of Masseter is compared at the three time points |
Sensory motor correlations: The associations were found between thermal sensory parameters and the motor activity of Masseter muscle at the 3 time points i.e. Day 0, 2 and 7. We are presenting correlations and r values. The significant differences were found between the males and females of their motor activities of Masseter muscle and no significant differences were found in the duration of Masseter muscles activity at MVC at all the three time points .The amplitudes of MVC at Day 2 and 7 were significant (p = 0.051). Thermal sensory parameters showed variable results of CDT values for both at baseline and they were comparable but at day 2 and at day 7 significant differences were found (p =0.029, and p =0.018 respectively). WDT values showed significant differences at baseline at day 7 (p =0.042 and p =0.048 respectively). CPT values were significantly different only on day 2 (p =0.046). HPT values were comparable for both subjects. Females had lower thresholds and lowered pain tolerances at all the times they differed significantly from their male counterparts.
Orthodontic tooth movement is known to cause inflammatory reactions in the periodontium and dental pulp, which release various biochemical mediators such as substance P, histamine, enkephalin, dopamine and serotonin which elicit hyperalgaesia (Yamasaki et al., 1984; Walker et al. , 1987; Davidovitch et al. , 1988; Nicolay et al. , 1990; Davidovitch, 1991; Saito et al. , 1991b; Grieve et al. , 1994; Alhashimi et al. , 2001, Gupta et al., 2014, Al Sayed et al., 2017).
Processing of complex information arising from mechanical force application induces recruitment of neurons, which act by the way of chemical mediators as modulators of the effector response to the stimulus (Vandevska-Radunovic, 1999). Apart from the classic constituents mentioned above, peripheral nerve fibres also participate in the inflammatory process associated with tooth movement (neurogenic inflammation). This involves release of neuropeptides after antidromic stimulation of afferent nerve endings and initiation of an inflammatory reaction. These neuropeptides released are known to elicit a painful response (Vandevska-Radunovic, 1999). Kato et al. (1996) examined the distribution of nerve fibres containing neurofilament protein (NFP), calcitonin gene-related peptide (CGRP), vasoactive intestinal polypeptide (VIP), and neuropeptides Y (NPY) in the PDL of the rat first molar after mechanical force application.Our study is also supported by Jones 1984 that pain is experienced by the majority of patients 4 hours after archwire placement, which further peaks at 24 hour and then It gradually declines.The mechanism of pain which is caused by orthodontic forces are not fully understood till know.
Kamogashira et al., (1988 ) and Marklund et al., (1994) reported that pain perceived has been related to levels of prostaglandin and substance P in the periodontal ligament and which may be probably related to inflammatory response. It may also injure periodontal nerve terminals which was reported by Loescher et al.,( 1993). Our study is in accordance with previous findings of Ngan et al ( 1989). The study suggested that the application of orthodontic separators over 24 hour period induces pain in the teeth and surrounding musculature.
We studied thermal sensitivity through quantitative sensory testing because for the evaluation of somatosensory function the QST parameters are known for providing the small fiber function and therefore offer a diagnostic sensitivity of 67% -70% for small fiber neuropathy (Tobin 1999, Hansson 2007). CDT is considered to represent the response mediated by small myelinated Aδ nerve-fiber conduction, as in relative terms, A delta fibres carry messages at the speed of a messenger on a bicycle. Warm Detection Threshold represent unmyelinated C nerve-fiber conduction, and the responses for noxious Cold and Hot pain may be conducted by both Aδ and C nerve fibers (Yarnitsky, 1991, Ziegler 1999). The patients had decreased sensitivity to cold stimuli and increased tolerance to cold pain suggesting sensitization at the level of Aδ fibres mainly. Since no significant differences were found in the thermal thresholds for warm stimuli, this may be attributed to the fact that the unlike the cold receptors, warm receptors act more like simple thermometers; their firing rates rise monotonically with increasing skin temperature up to the threshold of pain and then saturate at higher temperatures. Thus they cannot play a role in signaling heat pain. They are much less sensitive to rapid changes in skin temperature than are cold receptors. C fibres that carry hot pain sensations are activated at higher temperatures applied for longer duration.
The EMG study showed significant decrease in massetric muscle activity during maximal clenching and chewing. Our reports are in agreement with Goldreich et al, 1994 who also reported that there is reduction in activity of masseter after orthodontic archwire adjustment. In our study there is decrease in motor activity of masseter because of orthodontic pain and masseter muscle was tender and they had difficulty in speaking, chewing and swallowing. The basal tone of masseter was not affected by the pain. Trigeminal nerve provides tactile, proprioceptive, and nociceptive afferents to the face and mouth, and motor function activates the muscles of mastication (Masseter, Medial and Lateral Pterygoid, Temporalis). Such innervation is responsible for the elaborate peripheral feedback and feed-forward information that is essential for the coordination of masticatory muscles in a predictive manner based on learned relationships between patterns of receptor signals and appropriate efferent signals (Trulsson, 2007). Any alteration in the orofacial environment, either from changes in the consistency of the diet or dental manipulations may affect the exteroceptive, proprioceptive and perhaps also the nociceptive inputs into the CNS and thereby may alter the patterns of jaw and tongue movements during mastication (Murray et al, 2004; Sessle, 2006). Lund et al 1994, explained changes that motor programs control the premotor nociceptive interneuron to agonist and antagonist motor neurons in a reciprocal way. To account for the lowering of agonist output in the presence of pain, the motor command includes excitation (or facilitation) of the inhibitory group and the inhibition (or disfacilitation) of the excitatory group supplying agonist motor neurons. In the presence of pain, the agonist muscles’ activity is lowered because of the inhibitory pathway being stimulated and the excitatory pathway being inhibited. In case of orthodontic therapy, application and activation of arch wires would induce the constant forces on the fibers of the periodontal ligament during the course and hence the agonist muscle activity would tend to decrease. At baseline we found absolutely no pain and hypo/hyper activity in masseter (inclusion criteria), we recorded the muscle activity at rest and at maximum voluntary contraction. The above results suggests that pain arising due to application of constant forces on the fibers of the periodontal ligament during orthodontic treatment, agonist muscle i.e. masseter activity decreases because the inter neurons receive convergent excitatory inputs from different tissues. Similar results were reported by Michelloti et al, 1999, who found significant differences in activity of motor activity before and after the start of orthodontic therapy.
Since orthodontic pain is subjective in nature and gender differences are found. Ngan et al., 1989; Erdinç et al., 2004 in their respective studies found adolescent females undergoing orthodontic treatment had lower pain thresholds and pain tolerances compared to age matched Thermal detection, pain and pain tolerance thresholds for the hot stimuli were all comparable at the 3 time points.
CONCLUSION
There is marked peripheral sensitization at the level of nociceptors at a distant site other than oral cavity i.e. at masseter from the orthodontic therapy, also not only thermal hyposensitivity to cold stimuli was seen, also patient’s tolerance to cold pain stimuli increased and motor activity was adversely affected. The study of basal thermal sensitivity and motor activity of masseter muscle before the start of orthodontic treatment will benefit orthodontists in planning and modifying the treatment for patients. Thus QST and EMG may become useful tools during orthodontic therapy for better patient compliance.
ACKNOWLEDGMENTS
We would like to thank the young patients who willingly participated in this study and their parents too. Authors also acknowledge lab technician (Ms Suman) and lab attendant (Mr Surender) of Pain Research and TMS Laboratory for their support. Authors also thank Department of Physiology and Department of Biostatistics, AIIMS, New Delhi for providing the research and data analysis facility.
CONFLICT of INTEREST
There is no conflict of interest
References
Alhashimi N, Frithiof L, Brudvik P, Bakhiet M (2001) Orthodontic movement and de novo synthesis of proinflammatory cytokines. American Journal of Orthodontics and Dentofacial Orthopedics 119:307 – 312.
Al Sayed H, Sultan K, Hamadah O ( 2017) Evaluating low-level laser therapy effect on reducing orthodontic pain using two laser energy values: a split-mouth randomized placebo-controlled trial. Eur J Orthod.; Epub.
Bergius M, Kiliardis S, Berggren U (2000) Pain in orthodontics: a review and discussion of the literature . Journal of Orofacial Orthopedics 61: 125 – 137
Bondemark L Fredriksson K, Ilros S (2004) Separation effect and perception of pain and discomfort from two types of orthodontic separators . World Journal of Orthodontics 5: 172 – 176
Davidovitch Z (1991) Tooth movement. Critical Reviews in Oral Biology and Medicine 2: 411 – 450
Davidovitch Z, Nicolay O F, Ngan P W, Shanfeld J L (1988) Neurotransmitters, cytokines and the control of alveolar bone remodeling in orthodontics. Dental Clinics of North America 32: 411 – 435
Erdinç A M E, Dinçer B (2004) Perception of pain during orthodontic treatment with fixed appliances. European Journal of Orthodontics 26:79 – 85
Goldreich H, Gazit E, Lieberman M A, Rugh J D (1994) The effect of pain from orthodontic arch wire adjustment on masseter muscle electromyographic activity . American Journal of Orthodontics and Dentofacial Orthopedics 106: 365 – 370
Grieve III W G, Johnson G K, Moore R N, Reinhardt R A, DuBois L M (1994) Prostaglandin E (PGE) and interleukin-1 beta (IL-1 β) levels in gingival crevicular fluid during human orthodontic tooth movement. American Journal of Orthodontics and Dentofacial Orthopedics 105:369 – 374
Gupta M, Kandula S, Laxmikanth SM, Vyavahare SS, Reddy SB, Ramachandra CS. (2015) Controlling pain during orthodontic fixed appliance therapy with non-steroidal anti-inflammatory drugs (NSAID): a randomized, double-blinded, placebo-controlled study. J Orofac Orthop. 15(6):471–476.
Hosseinzadeh Nik T, Shahsavari N, Ghadirian H, Ostad SN (2016) Acetaminophen versus liquefied ibuprofen for control of pain during separation in orthodontic patients: a randomized triple blinded clinical trial. Acta Med Iran. 54(7):418–421.
Jones M L (1984) An investigation into the initial discomfort caused by placement of an archwire . European Journal of Orthodontics 6:48 – 54
Kamogashira K, Yanabu M, Ichikawa K, Itoh T, Matsumoto M, Ishibashi K, Abe K (1988) The effects of upper incisor separation on the submandibular and sublingual glands of rats. Journal of dental research 67(3):602-10.
Kato J, Wakisaka S, Kurisu K (1996) Immunohistochemical changes in the distribution of nerve fibers in the periodontal ligament during an experimental tooth movement in rat molar . Acta Anatomica157:53 – 62
Marklund M, Lerner U H, Persson M, Ransjö M (1994) Bradykinin and thrombin stimulate release of arachidonic acid and formation of prostanoids in human periodontal ligament cells. European Journal of Orthodontics 16: 213–22
Michelotti A, Farella M , Martina R (1999) Sensory and motor changes of the human jaw muscles during induced orthodontic pain . European Journal of Orthodontics 21 : 397 – 404
Murray GM, Phanachet I, Uchida S, Whittle T (2004). The human lateral pterygoid muscle: a review of some experimental aspects and possible clinical relevance. Australian dental journal 49(1):2-8.
Ngan P, Kess B , Wilson S (1989) Perception of discomfort by patients undergoing orthodontic treatment . American Journal of Orthodontics and Dentofacial Orthopedics 96: 47 – 53
Nicolay O F, Davidovitch Z, Shanfeld J L, Alley K (1990) Substance P immunoreactivity in periodontal tissues during orthodontic tooth movement . Bone and Mineral 11: 19 – 29
Saito M, Saito S, Ngan P W, Shanfeld J L, Davidovitch Z (1991) Interleukin-1 beta and prostaglandin E are involved in the response of periodontal cells to mechanical stress in vivo and in vitro. American Journal of Orthodontics and Dentofacial Orthopedics 99: 226 – 240
Principles of neural science” Kandel, 5th edition E. R., Schwartz, J. H., & Jessell, T. M. (2000).
Scheurer A P, Firestone R A, Bürgin B W (1996) Perception of pain as a result of orthodontic treatment with fixed appliances. European Journal of Orthodontics 18: 349–357
Sessle BJ (2006) Mechanisms of oral somatosensory and motor functions and their clinical correlates. Journal of oral rehabilitation 33(4):243-61.
Topolski F, Moro A, Correr GM et al., Optimal management of orthodontic pain, J Pain Res 2018; 16;11:589-598.
Trulsson M (2007) Force encoding by human periodontal mechanoreceptors during mastication. Archives of oral biology 1;52(4):357-60.
Vandevska-Radunovic V (1999) Neural modulation of inflammatory reactions in dental tissues incident to orthodontic tooth movement —a review of the literature . European Journal of Orthodontics 21:231 – 247
Walker J A, Tanzer F S, Harris E F, Wakelyn C, Desiderio D M (1987) The enkephalin response in human tooth pulp to orthodontic force . American Journal of Orthodontics and Dentofacial Orthopedics 92: 9 – 16
Yamasaki K, Shibata Y, Imai S, Tani Y, Shibasaki Y, Fukuhara T (1984) Clinical application of prostaglandin E 1 (PGE 1 ) upon orthodontic tooth movement. American Journal of Orthodontics 85: 508 – 518


