Radiation Oncology Unit, King Abdulaziz University Hospital Jeddah, Saudi Arabia
Article Publishing History
Received: 15/07/2020
Accepted After Revision: 25/09/2020
The purpose of this study was to identify factors that increase efficiency, reduce performance rates, decrease overall patient waiting time, and maximize the degree of patient access associated with repeated computed tomography at the Radiation Oncology Unit of King Abdulaziz University Hospital. We retrospectively reviewed the records of all patients who underwent repeated computed tomography at the Radiation Therapy Unit of King Abdulaziz University Hospital from January 2014 to December 2018. Re-scanning was required for communication-related, clinical, patient-related, and technical issues. The characteristics of the study variables were defined using simple descriptive statistics. A chi-squared test was used to establish relationships between categorical variables. A p-value < 0.05 was considered statistically significant.During the study period, 241 cases were referred for re-scanning. The rate of re-scanning almost doubled from 2014 (3.2%) to 2018 (5.7%). Clinical issues were the most common reasons for re-scanning (102 cases), followed by patient-related (89 cases), communication-related (45 cases), and technical issues (3 cases).
The chi-squared test revealed significant associations among the variables (p-value=0.002, <0.001, and <0.001 for communication, clinical, and patient-related issues, respectively). We observed an increasing trend in the overall frequency of re-scanning. The number of re-scanning procedures due to clinical and communication-related issues decreased significantly in 2018, while those owing to patient-related issues increased significantly. Frequent planned evaluation of the workflow and identification of potential reversible and recurring issues responsible for decreased scanning efficiency will be beneficial in radiation oncology. Resolving such issues can improve the safety and quality of patient care.
Re-CT Scan, Workflow, Radiation Therapy, Optimization
Al-Wassia R, Arputharaj V. J, Ujemi R, Bahadur Y, Hijazi H, Khasim A. H. M, Jastaniah Z, Iskandarani O, Attar M. Optimization of Repeat Computed Tomography Simulation for a More Efficient Workflow in the Radiation Therapy Unit: A Single-Institution Experience. Biosc.Biotech.Res.Comm. 2020;13(3).
Al-Wassia R, Arputharaj V. J, Ujemi R, Bahadur Y, Hijazi H, Khasim A. H. M, Jastaniah Z, Iskandarani O, Attar M. Optimization of Repeat Computed Tomography Simulation for a More Efficient Workflow in the Radiation Therapy Unit: A Single-Institution Experience. Biosc.Biotech.Res.Comm. 2020;13(3). Available from: https://bit.ly/2PM0vxR
Copyright © Al-Wassia et al., This is an open access article distributed under the terms of the Creative Commons Attribution License (CC-BY) https://creativecommons.org/licenses/by/4.0/, which permits unrestricted use distribution and reproduction in any medium, provide the original author and source are credited.
INTRODUCTION
The prolonged waiting time for the diagnosis and treatment of cancer is one of the most frequent concerns among attending clinicians and patients. This results to the disease being identified at a more advanced stage with worse prognoses . Longer wait times is not an empty issue, as this results to patient dissatisfaction which consequently has a critical effect on the healthcare outcomes for the patient (Elsaid et al., 2020). A recent study outlined the most common factors of longer wait times in an oncology department, which include waiting for lab results, team/clinic communication, patient factors, chemotherapy preparation, and chemotherapy consultation (Plourde et al., 2020). Their results pointed to laboratory turnaround times as the major cause of delay in oncology clinics.
Computed tomography (CT) scans are commonly used to visualize parts of the human body, in a more powerful way than regular x-ray procedures do. On a doctor’s recommendation, a CT scan can be used to diagnose structural disorders, monitor treatments, visualize internal injuries, and more. In oncology departments, this procedure is used to detect, pinpoint and monitor tumors and infections to diagnose cancer and other diseases. A study conducted from 2015 to 2018 revealed that rapid access to CT scan procedures greatly reduced the waiting time during the diagnostic process (Franco Serrano et al., 2019). Even though repeat CT scans also cause longer waiting times for cancer patients, this procedure provides diagnostic clarity for health care specialists (Lovoli et al., 2019). Further studies must be conducted to evaluate the current state of Saudi healthcare system and its policies addressing the issue of inefficient workflow in hospitals.
In this study, the process required to ensure patient safety in accordance to the international and national accreditation parameters was evaluated, with the goal of improving the overall quality of service to cancer patients at the Radiation Therapy Unit in the institution. Additionally, this study aimed to identify potential opportunities that could increase efficiency, reduce performance rate, decrease the overall patient waiting times, and maximize the patient accessibility associated with re-CT.
MATERIAL AND METHODS
In this study, we retrospectively reviewed the records of all re-CT cases at the Radiation Therapy Unit of our institution from January 2014 to December 2018. The reasons for re-CT were categorized into the following four groups: communication-related, clinical, patient-related, and technical issues. The Radiation Therapy Unit at our institution comprises more than 35 staff members, organized into the following four core disciplines: radiation oncology (RO), physiotherapy, nursing, and radiation therapy. It is the largest single-institution radiation facility in the country’s western region and attends to 1100 new patients yearly, delivering more than 1200 courses of radiation treatment annually. Treatment planning for patients undergoing radiation treatment at this unit includes computed tomography simulation (CT-Sim). CT-Sim influences the initiation of radiation treatment for patients with cancer within an acceptable time duration, according to National Comprehensive Cancer Network guidelines.
The repeat CT (re-CT) procedures performed in the unit required auditing, to optimize the procedures used for tumors at different sites of the body, miscommunication issues, and clinical decisions, all of which eventually led to a re-CT appointment. Accordingly, a multidisciplinary team led by CT-Sim radiation therapists and physicians recently conducted a multifaceted audit of the current procedures and practices concerned with patient appointment for CT-Sim. Re-CT, which was performed because of an inefficient CT procedure, was found to be associated with increased cost.
Statistical analysis was conducted using IBM SPSS version 23. Simple descriptive statistics such as counts and percentages were used to express the characteristics of the categorical and nominal variables, while continuous variables were presented as the mean and standard deviation. The chi-squared test was used to establish the relationship between the categorical variables. These tests were performed under the assumption of normal distribution. A conventional p-value of <0.05 was the criterion for rejecting the null hypothesis. The Hospital’s research committee approved the study.
RESULTS AND DISCUSSION
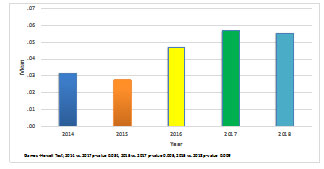
A total of 241 cases were referred for re-CT between January 2014 and December 2018. Table 1 shows the percentage of re-CT cases per year. The number of re-CT cases noted were 28 (3.2%) in 2014, 27 (2.7%) in 2015, 52 (4.7%) in 2016, 69 (5.7%) in 2017, and 65 (5.6%) cases in 2018. The re-CT rate almost doubled from 3.1% in 2014 to 5.6% in 2018, showing a significantly increasing trend (p = 0.001) (Figure 1). Table 2 presents multiple comparisons of the number of re-CT scan cases per year. The result revealed significant differences in the number of such cases between 2014 and 2017, as well as between 2015 and 2017 and between 2015 and 2018.
Figure 1: Graphical representations of the number of re-CT cases from 2014 to 2018 Significance was set at p-value < 0.05. re-CT, repeat computed tomography
Table 1. Number of re-CT scan cases from January 2014 to December 2018
| Variables | Year | p-value | ||||
| 2014 | 2015 | 2016 | 2017 | 2018 | ||
| Total CT | 885 | 975 | 1101 | 1206 | 1163 | – |
| Re-CT | 0.03 ± 0.2 | 0.03 ± 0.2 | 0.05 ± 0.2 | 0.06 ± 0.2 | 0.06 ± 0.2 | 0.001a |
| 28 (3.2%) | 27 (2.8%) | 52 (4.7%) | 69 (5.7%) | 65 (5.6%) | ||
aSignificance level set at 0.05 level using one-way analysis of variance. CT, computed tomography; re-CT, repeat CT
Table 2. Multiple comparison of the number of re-CT cases across 5 years
| (I) Year | (J) Year | Mean Difference (I-J) | 95% Confidence Interval | p-value | |
| Lower Bound | Upper Bound | ||||
| 2014 | 2015 | 0.004 | −0.018 | 0.025 | 0.987 |
| 2016 | −0.016 | −0.039 | 0.008 | 0.378 | |
| 2017 | −0.026* | −0.050 | −0.001 | 0.034 | |
| 2018 | −0.024 | −0.049 | 0.000 | 0.053 | |
| 2015 | 2016 | −0.020 | −0.042 | 0.003 | 0.127 |
| 2017 | −0.030* | −0.053 | −0.006 | 0.005 | |
| 2018 | −0.028* | −0.052 | −0.005 | 0.009 | |
| 2016 | 2017 | −0.010 | −0.035 | 0.015 | 0.818 |
| 2018 | −0.009 | −0.034 | 0.017 | 0.884 | |
| 2017 | 2018 | 0.001 | −0.025 | 0.027 | 1.000 |
*The mean difference is significant at a level of 0.05. re-CT, repeat computed tomography
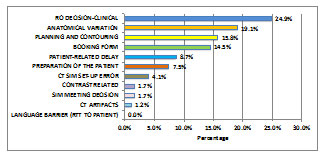
The collected data from patient charts survey revealed 4 major reasons for re-CT, which were divided into the following groups, Table 3: communication-related, clinical, patient-related, and technical issues. Four specific reasons were identified in the communication-related issues group. Thirty-five cases (14.5%) reported issues with the booking form, while a language barrier was not an issue in any case (0.0%). Ten cases (4.1%) experienced a mishap in the CT-Sim set-up. Clinical issues were also raised during the survey. Sixty patients (24.9%) reported that re-CT was performed because of the RO’s decision (clinical): 54 (90%) of 60 patients underwent re-CT, because improvements in planning dictated that all patients with breast cancer had to undergo CT under an altered set-up to ensure better dosimetry quality, while the remaining 10% underwent re-CT owing to malfunctioning equipment. Four patients (2.3%) required re-CT, after a CT-Sim meeting decision (Sim meeting) (where all consultants met and discussed the patients’ treatment plans), while 38 (15.8%) underwent re-CT for reasons related to planning and contouring, predominantly owing to difficulties in achieving dose constraints with three-dimensional (3D) planning and the need for a different set-up for volumetric intensity modulated radiotherapy (VMAT).
Table 3. Issues associated with re-CT
| Variables | Count | % | |
| Communication issues | Booking form | 35 | 14.5 |
| Language barrier: RTT to patient | 0 | 0.0 | |
| CT Sim set-up error | 10 | 4.1 | |
| Clinical issues | RO decision-Clinical | 60 | 24.9 |
| Sim meeting decision | 4 | 1.7 | |
| Planning and contour | 38 | 15.8 | |
| Patient-related issues | Preparation of the patient | 18 | 7.5 |
| Patient-related delay | 21 | 8.7 | |
| Contrast related | 4 | 1.7 | |
| Anatomical variations | 46 | 19.1 | |
| Technical issues | CT artifacts | 3 | 1.2 |
RTT, radiation therapist; CT, computed tomography; re-CT, repeat CT; RO, radiation oncologist; Sim, simulation
Among the patient-related issues, 18 (7.5%) were related to the patients’ self-preparation which means that the patient did not prepare well for the simulation Ct scan by emptying rectum or bladder or sometimes by filling bladder as indicated to them in the preparatory protocol; 21 (8.7%) were associated with patient-related delays, 4 (1.7%) were associated with contrast-related issues, and 46 (19.1%) were associated with anatomical variations. Eighty percent of these patients had tumors of the head and neck and required re-planning because of weight loss and ill-fitting masks. The only technical issues were associated with CT artifacts in 3 cases (1.2%).
Based on the specific reasons described in this review, the RO’s decision (clinical) was the most commonly cited reason (24%, n = 60) for re-CT, as shown in Figure 2. This was followed by cases with anatomical variations, and those with planning and contouring-related issues. The fourth most commonly noted reason was booking form-related problems, followed by patient-related delays, issues pertaining to patients’ self-preparation, and those caused by CT-Sim set-up errors. As shown in Figure 1, language barrier (radiation therapist to patient) was the least commonly observed reason for re-scanning. CT artifacts and contrast-related and SIM meeting decisions were other infrequently cited reasons (1.7% each) (n = 4).
Figure 2: Issues associated with re-CT performance RO, radiation oncologist; SIM, simulation; CT, computed tomography; re-CT, repeat CT; RTT, radiation therapist
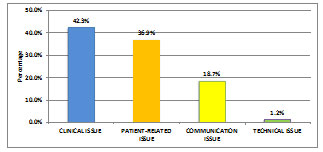
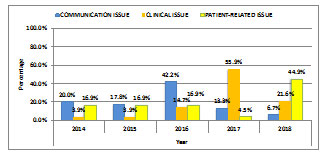
As shown in Table 4 and Figure 3, clinical issues were the most commonly observed causes of re-scanning, followed by patient-related issues, communication-related issues, and finally, technical issues. Table 5 demonstrates the distributions of the three major causes of re-scanning from 2014 to 2018. Re-scanning owing to communication-related problems was observed in 9 (20.0%) cases in 2014, 8 (17.8%) in 2015, 19 (42.2%) in 2016, 6 (13.3%) in 2017, and 3 (6.7%) in 2018. Clinical-related reasons were reported in 4 (3.9%) cases in 2014, 4 (3.9%) in 2015, 15 (14.7%) in 2016, 57 (55.9%) in 2017, and 22 (21.6%) in 2018.
Figure 3: Major causes of or issues related to re-CT scanning of patients re-CT, repeat computed tomography
Table 4. Major causes or issues associated with re-CT performance
| Variables | Count | % |
| Communication issues | 45 | 18.7 |
| Clinical issues | 102 | 42.3 |
| Patient-related issues | 89 | 36.9 |
| Technical issues | 3 | 1.2 |
re-CT, repeat computed tomography
Table 5. Distribution of major issues associated with re-CT per year
| Variables | Total | Year | p-value | ||||
| 2014 | 2015 | 2016 | 2017 | 2018 | |||
| Total | 241 | 28 (11.6%) | 27 (11.2%) | 52 (21.6%) | 69 (28.6%) | 65 (27.0%) | – |
| Communication issues | 45 | 9 (20.0%) | 8 (17.8%) | 19 (42.2%) | 6 (13.3%) | 3 (6.7%) | <0.001a |
| Clinical issues | 102 | 4 (3.9%) | 4 (3.9%) | 15 (14.7%) | 57 (55.9%) | 22 (21.6%) | <0.001a |
| Patient-related issues | 89 | 15 (16.9%) | 15 (16.9%) | 15 (16.9%) | 4 (4.5%) | 40 (44.9%) | <0.001a |
| Technical issues | 3 | 0 (0.0%) | 0 (0.0%) | 3 (100.0%) | 0 (0.0%) | 0 (0.0%) | 0.026a |
asignificance level set at < 0.05 using a chi-square test. re-CT, repeat computed tomography
Finally, patient-related issues were revealed to be responsible for re-CT in 15 cases (16.9%) each in 2014, 2015, and 2016, only 4 cases (4.5%) in 2017, and 40 (44.9%) in 2018. The association between these variables was evaluated using chi-squared tests, which revealed that the variables were significantly related to each other, with p-values =0.002, <0.001, and <0.001 for communication-related, clinical, and patient-related issues, respectively.
Re-scanning owing to clinical causes demonstrated an increasing trend between 2014 and 2017, accounting for 3.9% of all re-CT cases in 2014 and 2015, 14.7% in 2016, and 55.9% in 2017 (Figure 4). Nevertheless, a significant decrease was observed in 2018 (21.6%). The incidence rate of patient-related issues was almost consistent, accounting for 16.9% of all cases every year from 2014 to 2016, which subsequently decreased to 4.5% in 2017, before significantly rising in 2018 (44.9%). Among the 3 identified major causes of re-scanning, patient-related issues were the most commonly cited reasons from 2014 to 2015 and 2018, while communication-related issues were most common in 2016. The rate of re-CT owing to clinical issues was the highest in 2017.
Figure 4: Distribution of major issues of re-CT per year re-CT, repeat computed tomography
DISCUSSION
In this study, an increasing trend in clinical, patient-related, and communication-related issues, which were major factors responsible for re-CT, were observed. The number of re-scanning procedures performed because of clinical and communication-related issues decreased significantly in 2018, while those performed because of patient-related issues increased significantly. Numerous demands are placed on patients with cancer and their families, which include coping with treatment schedules, the resulting side-effects, and adapting to lifestyle limitations and role changes (Merluzzi and Martinez Sanchez 1997). Cancer is associated with a substantial financial burden not just for the patient level, but also at a healthcare service and societal level (Barr et al., 2014). This is relevant to the current need to rationalize the expenditure of resources in a specialty with rising treatment costs, and the decisions made can have a significant impact on the patient’s quality of life (Pearce et al., 2001).
There is a relevant study conducted by Soo et al. (2019) which analyzed patient experiences and perspectives before, during and after imaging-guided breast biopsies. They also proposed policies and strategies to overcome hurdles in optimizing the patient experience. Results showed that exhibiting compassion in delivering cancer diagnoses, along with optimizing the physician-patient communication and developing a patient-centered approach all contribute to overall general satisfaction of the patient population. Additionally, they stated that long wait times in the context of definitive diagnoses are often “intense and agonizing” experiences and contributes to the stress and anxiety experienced by the patient.
On a similar study, where oncology patients’ experiences of a surveillance CT were reviewed (Raaschou et al., 2019). Results showed that radiographers’ focus on the technological aspect of clinical management instead of establishing relations and showing sincere interest and empathy, contribute to the “undesirable” experiences most subject patients share. The study highlighted that establishing communication and relationship with the patient is as important as providing quality radiological interpretation and diagnoses.A literature review conducted by Pearce et al. (2001) in the United Kingdom revealed that the costs associated with cancer treatment and care were complex.
These costs included those related to cancer treatment and service delivery, indirect costs to patients and their caregivers, and the human cost of cancer and its treatment, such as deterioration in the quality of life, lifestyle and role changes, symptom-related distress, and wastage of time. They identified a lack of research on the development of cost-effective healthcare services. With the escalating cost of healthcare and the economic recession, healthcare institutions in Saudi Arabia have identified the need to re-evaluate and reduce expenditures without compromising on the quality of patient care. For instance, CT is a commonly used, less expensive imaging modality, which is instrumental in facilitating the diagnosis of a wide range of medical conditions, especially cancer (Jabali et al., 2015).
Ultimately, this study aimed to identify opportunities to increase the efficiency of CT, to reduce the rate of re-CT and patient waiting time, and maximize patient access to this essential diagnostic modality, as a part of treatment. We discovered that clinical problems such as the RO’s decision to repeat the scan, because of mismatch between set-up and planning requirements; planning and contouring-related issues; anatomical variations (patient-related); and booking form-related issues (communication-related issue) were the most common causes of re-CT from 2014 to 2018. These findings are vital, as they indicate the need for providing continuous education to clinical teams on the services they are expected to provide, as the burden of cancer is already enormous on patients and their families.
During the study duration (2014–2018), the rate of re-CT almost doubled from 3.1% in 2014 to 5.7% in 2018, thus, showing a prominent increasing trend. According to the findings, the RO’s decision (clinical) was the most commonly cited cause of re-CT, which accounted for 60 of 241 cases from 2014–2018. Overall, 90% of the 60 cases underwent re-scanning because of changes in the breast cancer set-up for the achievement of proper constraints; 10% (6 cases) of the cases underwent re-CT because of malfunctioning equipment.The deep inspiration breath-hold technique (DIBH) was not utilized at our center, and switching to VMAT planning was the only way to improve coverage whilst respecting normal tissue constraints for patients with breast cancer. Moreover, differences in the CT protocol around the world must be taken into account, especially those pertaining to the inclusion of the internal mammary lymph (IM) nodes (Duane et al., 2019), which may be more challenging with 3D planning (explaining the more frequent need to switch to VMAT).
The observed surge in the re-CT rate could be related, at least partially, to the appointment of a few new ROs with different practice backgrounds with respect to IM radiotherapy, and the use of intensity-modulated radiotherapy (IMRT) for different sites in general. For technical reasons related to differences in the machines used at our institution, the switch from 3D to VMAT for breast cancer-related radiotherapy requires a different set-up, resulting in re-CT. Differences in the set-up for 3D and VMAT are also applicable to other sites, e.g., bladder emptiness and fullness for pelvic IMRT.
Some measures can be taken to attempt to reduce the re-CT rate, improve CT efficiency, and decrease the degree of patient anxiety related to unplanned treatment delays in the above-mentioned situations. First, certain screening criteria must be implemented to aid in the identification of patients who are likely to benefit from DIBH or VMAT, followed by re-scanning with a different set-up but at the same appointment (Czeremszyńska et al., 2017; Rice et al., 2017). Second, institutional practice guidelines should be developed, to decrease the frequency of variations in practice, to limit the need for re-CT associated with unpredictable anatomical factors that complicate planning and dictate technique changes.
Third, while the timely identification of such patient-related factors may not change the need for re-CT, it can shorten delays in treatment initiation and their subsequent effects on treatment outcomes (Khorana et al., 2019), thereby alleviating the degree of anxiety and distress. Finally, reducing the inevitably high demand-related machine malfunction rate through rigorous quality assurance and proper maintenance programs can lower the magnitude of the problem and the associated mistrust from the patient’s side and reduce the worsened disease outcomes related to the tumor repopulation effect (Bohmer and Edmondson 2001; Fiol and Lyles 1985).
In 2019, a study by Beaumont et al. compared the standard radiological workflow and a novel “hybrid” workflow they proposed. Their study pointed to trial nonconformities like blank reports, unsigned reports, missing/wrong patients’ appointment dates as unnecessary errors that consume valuable time. Their proposed hybrid workflow saved around 87% of radiologists time and could offer a plausible opportunity for reducing costs with improved imaging quality. Overall, they pointed out that time efficiency in radiological clinical trials can be improved; electronic case report forms reduces nonformities; and that radiologists can delegate non-essential tasks. Al Hroub et al. (2019) also conducted a similar study where they made use of lean thinking concepts and tools to improve the workflow efficiency in their outpatient oncology center.
After implementation, the mean clinic waiting time decreased from 72.5 minutes to 19.5 minutes and 21 minutes at two different quarters (period of implementation). They attributed this to the redesigned electronic appointment system which reduced patient waiting time, improved patient satisfaction and resource utilization. Additionally, their updated workflow reallocates health-care providers’ time and promotes a new perspective towards a direct and individualized patient care.
Anatomical variation was the second most commonly cited reason for re-CT, including weight loss or gain during radiotherapy. Forty-six cases of anatomical variation (patient-related) were identified; the majority was observed in patients with head and neck cancer. Other researchers have also identified that these sites are among the most common sites requiring re-scanning (Carroll and Edmondson 2002). The optimization of nutritional support and availability of an onsite dietitian, an aspect that is being investigated, would theoretically decrease the magnitude of weight loss and need for re-scanning (Colasanto et al., 2005). Interestingly, there is a lack of evidence supporting the efficiency of prophylactic feeding for weight loss prevention and subsequent re-planning (Brown and Yabroff 2006). However, adaptive radiotherapy for head and neck cancers improves the coverage of shrinking tumors and reduces the degree of overdose to the organs at risk (Surucu et al., 2017).
Our findings revealed a statistically significant association between the year and cause of re-scanning. A notable increasing trend was observed from 2014 to 2017 in the re-scanning rates associated with clinical issues that coincided with the enrollment of new ROs. Moreover, re-CT rates caused by patient-related issues have increased significantly from 2017 (4 cases) to 2018 (40 cases); consequently, attention to patients’ preparation strategies, including proper education to ensure satisfactory planning and treatment delivery, is of paramount importance. The use of written and audiovisual material may improve patient satisfaction and more importantly, education outcomes (Saeed 2018; Savage et al., 2017).
Communication-related issues, especially booking form-related issues, were identified to be among the most commonly cited causes of re-CT. Two very important measures that can minimize the degree of these issues are already under implementation. First, the development and frequent updating of departmental policies and procedures are crucial for the maintenance of the program’s quality and will decrease the amount of information to be filled in the booking form, thereby reducing error rates, and ultimately, re-CT rates. Second, shifting to paperless forms from paper-based booking ones and the development of standard site and disease-specific care plans may also improve the quality and efficiency of booking forms, and subsequently, reduce the rate of re-CT.
A study conducted by Woolen et al. (2018) attempted to utilize and asses the efficacy of online patient portals, specifically in relation to the time of release of CT scan results. Their research revealed that the outpatient population prefer to receive imaging results regarding a probable cancer diagnosis as soon as possible with direct communication with their physician over the telephone, as compared to receiving the result in their physician’s office or over other media such as electronic mail. However, they surveyed only their local outpatient population, and may not apply to other departments or their inpatient population. Further studies may be conducted if this approach overcomes other bureaucratical or clinical hindrances to improve workflow efficiency.
Healthcare institutions play a major role in the diagnosis, treatment, and monitoring of patients with cancer. Therefore, it is important that they initiate the development of processes that involve procuring new knowledge and the application of this knowledge (Fiol and Lyles 1985). Healthcare delivery researchers state that learning is a cyclical and multi-level process (Bohmer and Edmondson 2001; Carroll and Edmondson 2002; Hamel et al., 2014). System errors and inadequacies are frequently organizational, including multiple individuals and/or systems within the hospital, and necessitate a more holistic view of the organizational and clinical characteristics of care (Goodman et al., 2011; Hamel et al. 2014; Ramanujam and Rousseau 2006).
The present study is the first to identify opportunities that increase efficiency, reduced performance rate and overall patient wait times, and maximized patients’ access to re-CT, as part of radiation therapy in Saudi Arabia. It is limited to the local population of the Radiology Oncology Unit of King Abdulaziz University Hospital. Lastly, this study may be used as a guide to reform and redesign policies accordingly to improve overall patient satisfaction and produce an efficient workflow beneficial to both healthcare workers and patients.
CONCLUSION
While the need for re-CT is inevitable in any radiation therapy unit, frequent planned evaluation of the workflow and the potential reversibility and recurrence of issues responsible for decreased CT efficiency in any department is essential, particularly at times when the degree of the changes in manpower is significant. The resolution of these recurring issues may aid in reducing the rate of re-CT, and inevitably improve the safety and quality of patient care.
REFERENCES
Al Hroub A, Obaid A, Yaseen R, El-Aqoul A, Zghool N, Abu-Khudair H, Al Kakani D, Alloubani A. (2019) Improving the Workflow Efficiency of An Outpatient Pain Clinic at A Specialized Oncology Center by Implementing Lean Principles. Asia Pac J Oncol Nurs 6(4): 381-388.
Barr B, Bambra C, Whitehead M. (2014) The impact of NHS resource allocation policy on health inequalities in England 2001-11: longitudinal ecological study. BMJ 348: g3231.
Beaumont H, Bertrand AS, Klifa C, Patriti S, Cippolini S, Lovera C, Iannessi A. (2019) Radiology workflow for RECIST assessment in clinical trials: Can we reconcile time-efficiency and quality? Eur J Radiol 118: 257-263.
Bohmer RM, Edmondson AC. (2001) Organizational learning in health care. Health Forum J 44(2): 32-35.
Brown ML, Yabroff KR (2006). Economic impact of cancer in the United States. Cancer Epidemiology and Prevention. D. Schottenfeld and J. F. Fraumeni. Oxford, England, Oxford University Press: 202-213.
Carroll JS, Edmondson AC. (2002) Leading organisational learning in health care. Qual Saf Health Care 11(1): 51-56.
Colasanto JM, Prasad P, Nash MA, Decker RH, Wilson LD. (2005) Nutritional support of patients undergoing radiation therapy for head and neck cancer. Oncology (Williston Park, N.Y.) 19(3): 371-387.
Czeremszyńska B, Drozda S, Górzyński M, Kępka L. (2017) Selection of patients with left breast cancer for deep-inspiration breath-hold radiotherapy technique: Results of a prospective study. Reports of practical oncology and radiotherapy : journal of Greatpoland Cancer Center in Poznan and Polish Society of Radiation Oncology 22(5): 341-348.
Duane FK, McGale P, Teoh S, Mortimer C, Broggio J, Darby SC, Dodwell D, Lavery B, Oliveros S, Vallis KA, Taylor CW. (2019) International Variation in Criteria for Internal Mammary Chain Radiotherapy. Clinical oncology (Royal College of Radiologists (Great Britain)) 31(7): 453-461.
Elsaid M, Morgan J, Colorado N, Woolsey J, Canterberry N, Rice P, Russo C. (2020) Chemotherapy Wait Times in a Network of Pediatric Oncology Clinics. J Pediatr Hematol Oncol 42(6): e475-e478.
Fiol CM, Lyles MA. (1985) Organizational learning. Acad Manage Rev 10: 803-813.
Franco Serrano J, Ordóñez Gómez PL, Lahosa Córdoba C, Mollá Landete MÁ, Tarrasó Castillo J. (2019) Effect of a fast track CT pathway on diagnostic and treatment waiting times in lung cancer patients. Eur Respir J 54(suppl 63): PA3080.
Goodman PS, Ramanujam R, Carrol JS, Edmondson AC, Hofmann DA, Sutcliffe KM. (2011) Organizational errors: Directions for future research. Res Organ Behav 31: 151-176.
Hamel LM, Chapman R, Eggly S, Penner LA, Tkatch R, Vichich J, Albrecht TL. (2014) Measuring the use of examination room time in oncology clinics: a novel approach to assessing clinic efficiency and patient flow. J Oncol Pract 10(6): e385-389.
Iovoli AJ, Platek A, DeGraaff LH, Yau E, Wooten KE, Arshad H, Gupta V, Kuriakose M, Hicks WL, Singh AK. (2019) Do Repeat PET/CT Scans Have Value in Head and Neck Cancer When Initial Post-Treatment Scans Are Equivocal? Int J Radiat Oncol Biol Phys 105(1)
Jabali AK, Farid KY, Matani A, Al Mulhim F. (2015) Key factors influencing the usage of MRI in Saudi Arabia. Procedia Comput Sci 65: 562-571.
Khorana AA, Tullio K, Elson P, Pennell NA, Grobmyer SR, Kalady MF, Raymond D, Abraham J, Klein EA, Walsh RM, Monteleone EE, Wei W, Hobbs B, Bolwell BJ. (2019) Time to initial cancer treatment in the United States and association with survival over time: An observational study. PloS one 14(3): e0213209-e0213209.
Merluzzi TV, Martinez Sanchez MA. (1997) Perceptions of coping behaviors by persons with cancer and health care providers. Psychooncology 6(3): 197-203.
Pearce S, Kelly D, Stevens W. (2001) ‘More than just money’-widening the understanding of the costs involved in cancer care. J Adv Nurs 33(3): 371-379.
Plourde CL, Varnado WT, Gleaton BJ, Das DG. (2020) Reducing Infusion Clinic Wait Times Using Quality Improvement. JCO Oncol Pract: JOP1900643.
Raaschou H, Pilegaard M, KLausen L, Danielsen AK. (2019) Oncology patients’ experience of a routine surveillance CT examination: Relationships and communication. Radiography 25(4): 308-313.
Ramanujam R, Rousseau DM. (2006) The challenges are organizational not just clinical. J Organ Behav 27(7): 811-827.
Rice L, Goldsmith C, Green MM, Cleator S, Price PM. (2017) An effective deep-inspiration breath-hold radiotherapy technique for left-breast cancer: impact of post-mastectomy treatment, nodal coverage, and dose schedule on organs at risk. Breast cancer (Dove Medical Press) 9: 437-446.
Saeed N. (2018) Patient education in radiation oncology: Evolution and innovation. Appl Rad Oncol 7(1): 43-49.
Savage K, Arif S, Smoke M, Farrell T. (2017) Preferences in Learning Styles and Modes of Information Delivery in Patients Receiving First-Day Education for Radiation Therapy. Journal of medical imaging and radiation sciences 48(2): 193-198.
Soo MS, Shelby RA, Johnson KS. (2019) Optimizing the Patient Experience during Breast Biopsy. Journal of Breast Imaging 1(2): 131-138.
Surucu M, Shah KK, Roeske JC, Choi M, Small W, Jr., Emami B. (2017) Adaptive Radiotherapy for Head and Neck Cancer. Technology in cancer research & treatment 16(2): 218-223.
Woolen SA, Kazerooni EA, Steenburg SD, Nan B, Ma T, Wall A, Linna NB, Gayed MJ, Kushdilian MV, Parent K, Cahalan S, Alameddine M, Ladd LM, Davenport MS. (2018) Optimizing Electronic Release of Imaging Results through an Online Patient Portal. Radiology 290(1): 136-143.