Conservative Dental Science Department, College of Dentistry, Prince Sattam Bin Abdulaziz University, Al-Kharj, Saudi Arabia.
Corresponding author email: zaidaljeadi@gmail.com
Article Publishing History
Received: 04/02/2020
Accepted After Revision: 20/03/2020
To assess and compare different conditioning regimes (laser and conventional) on shear bond strength (SBS) of resin modified glass ionomer cement (RMGIC) bonded to dentinal tissue. Sixty permanent intact human third molars were prepared and allocated into six groups (n=10 each). Group 1, dentin was conditioned with Nd-Yag laser (NYL), Group 2: Er, Cr:YSGG laser (ECL), group 3: total etch adhesive, group 4: self-etch adhesive resin, group 5: 25% polyacrylic acid (PAA) and group 6: no treatment group. After surface conditioning of all fifty samples resin modified glass ionomer cement (RMGIC) was mixed and build up was performed. For SBS testing, specimens (n=10) in each group were placed in a custom jig of a Universal testing machine. For the de-bonded surface fracture analysis was completed using stereomicroscope at 40x magnification. Descriptive statistics i.e., means and standard for SBS were compared using analysis of variance (ANOVA) and Tukey’s post hoc test at a significance level of (p0.05. In laser, irradiated groups admixed failure was common. Dentin conditioned with PAA exhibited cohesive failure. The use of ECL and not NYL has a protentional to be used as conditioning regime in clinical setting prior to application of RMGIC.
RMGIC, Dentin Conditioning, Er,Cr:YSGG, Nd-Yag laser, Shear Bond strength.
Al Jeaidi Z. A. Influence of Nd-YAG And Er-Cr-YSGG Laser Conditioning on the Adhesive Bond Strength of Resin Modified Glass Ionomer Cement with Dentin. Biosc.Biotech.Res.Comm. 2020;13(1).
Al Jeaidi Z. A. Influence of Nd-YAG And Er-Cr-YSGG Laser Conditioning on the Adhesive Bond Strength of Resin Modified Glass Ionomer Cement with Dentin. Biosc.Biotech.Res.Comm. 2020;13(1). Available from: https://bit.ly/2RgDyVn
Copyright © Al Jeaidi, This is an open access article distributed under the terms of the Creative Commons Attribution License (CC-BY) https://creativecommons.org/licenses/by/4.0/, which permits unrestricted use distribution and reproduction in any medium, provide the original author and source are credited.
INTRODUCTION
In clinical practice premature restorative failure is a major concern. Most of the failures results at the interface between tooth structure and dental tissue due to poor bond strength resulting in secondary caries, microleakage, discoloration and fracture (Mjör and Gordan, 2002). Available evidence suggests glass ionomer cements (GIC) unveils improved bond integrity due to physio-chemical bonding with hydroxy appetite crystals in dentin, compared to adhesive resins (De Munck et al., 2005; Yoshida et al., 2000)
In recent years resin modified glass ionomer cement (RMGIC) has become popular due to fluoride release and biocompatibility (Swartz et al., 1984). But, debate still exits on tooth conditioning prior to RMGIC application. Recent reports have shown RMGIC to improve bond integrity on application of various conditioning regimes(Cardoso et al., 2010; Hotz et al., 1977; Powis et al., 1982). Whereas, other studies have stated no improvement in bond strength after surface treatment (Hamama et al., 2014; Imbery et al., 2013). The prime purpose for conditioning dentin is to remove the smear layer formed during cavity preparation which acts as a barrier, in forming a durable bond. Currently, there are numerous conditioners available in the market, but their efficacy and effectiveness are still dubious, (Alkhudhairy, et al., 2019a).
Alternative methods in the form of lasers Er,Cr:YSGG (ECL) and Nd-Yag (NYL) to condition tooth surface has displayed convincing results, (Alkhudhairy, AlKheraif, et al., 2018; Alkhudhairy, Naseem, et al., 2018; Vohra et al., 2018, Alkhudhairy, Naseem, Ahmad, et al., 2019; Alkhudhairy, Vohra and Naseem, 2019a; Alkhudhairy, Vohra, Naseem, et al., 2019). Interestingly, existing data suggests that lased dentinal surface exhibit open tubules, increase roughness and caters resembling to acid etched surface, ( Ekworapoj et al., 2007, Alkhudhairy, Vohra and Naseem, 2019a). Moreover, it provides a clean surface free of smear layer and enhances tooth adhesion (Kobayashi et al., 2003).
To our knowledge from indexed literature limited evidence on the use of lasers (ECL, NYL) as dentin conditioner prior to GIC application exists. Moreover, efficacy of different conditioning regimes and their comparison with laser conditioning is scarce and limited. It is hypothesized that dentin conditioned with ECL and NYL will exhibit bond strength similar to dentin treated with other surface regimens. Therefore, the aim of the present study was to assess and compare different conditioning regimes (lased and conventional) on shear bond strength (SBS) of RMGIC bonded to dentinal tissue.
MATERIAL AND METHODS
Sixty permanent intact human third molars free of caries, cracks were used as a bonding substrate. Teeth were isolated and stored in 0.5% chloramine T solution at 4 °C for duration of one month to disinfect, following storage in distilled water until use. With a low speed diamond saw (Isomet, Buehler, USA) the enamel surface was removed, and dentin surface was made flat. To attain a homogenize surface roughness, dentin polishing using silicon carbide grinding discs 800 and 1200 grits (Buehler, Great Britain UK) under water irrigation on a polishing machine (Stone Liu Shanghai Smedent Medical Instrument Co., Ltd) was used. Teeth were mounted vertically in acrylic resin within the sections of polyvinyl pipes (6mm diameter) up to cement-o-enamel junction (CEJ). Now based on the conditioning protocol the samples were allocated into six groups (n=10 each)
Group 1: Dentin surface was conditioned with Nd-Yag laser (NYL) (Hoya ConBio Delight, Sweden & Martina, Padova, Italy) at 150 mJ, 10 Hz and 1W for a duration of 60 sec in a non-contact circular motion using a quartz optical fibre having diameter of 320-μm.
Group 2: The surface of bonded dentin samples were treated with Er,Cr:YSGG laser (ECL) (Biolase- Waterlase I-Plus) at 0.5W and power 30Hz in a circular, non-contact position using tip MZ6 from a distance of 1mm for duration of 60 sec.
Group 3: 37% phosphoric acid was applied on dentin for 5 sec and washed with water spray thoroughly for 10sec. Bonding agent was applied and air dried for 10sec without the surface being desiccated. The bonding agent was reapplied and photo cured (Bluephase G2, Ivoclar,Vivadent) for 10 sec.
Group 4: On bonded dentinal surface self-etching primer was implemented and left undisturbed for 20 sec, gently air dried. Bonding agent was applied, spread uniformly with a light air stream, and light cured (Bluephase G2, Ivoclar,Vivadent) for 10 s.
Group 5: Polyacrylic acid (PAA) was applied on bonded dentinal surface and was left undisturbed for 10 sec. The surface was rinsed for 10 sec and air dried 5 sec without desiccation.
Group 6: Dentinal surface of this group did not receive any surface treatment.
After surface conditioning regimes of all fifty samples resin modified glass ionomer cement (RMGIC) Fuji II LC GC, Tokyo, Japan was mixed according to manufacturer instructions and build up was done incrementally using a tofelmire matrix holder at a height of 5mm and cured 20sec (Bluephase G2, Ivoclar,Vivadent).The specimens were covered with GC varnish (GC, America, Inc) and stored in distilled water at 24C until use.
Shear bond Strength (SBS) :For SBS testing specimen (n=10) each group were placed in a custom jig of a Universal testing machine (Lloyds, LF, plus, Ametek Inc, Great Britain, UK) under a cross head speed of 1mm/ min until failure occurred. The force was applied parallel to bonded samples. The maximum force required to generate fracture was recorded in MPa.
Failure mode Analysis: Fracture analysis was completed by two examiners using stereomicroscope at 40x magnification (Preconfigured Olympus Stereo Microscope Systems, SZX7, Edmund Optics UK). Type of failure was categorized into adhesive cohesive and admixed.
Statistical Analysis: SBS data was tabulated using statistical program for social science (SPSS version 19, Inc., Chicago, US). Normality of data obtained was assessed using Kolmogorov-Smirnov test. Descriptive statistics i.e., means and standard for SBS were compared using analysis of variance (ANOVA) and Tukey’s post hoc test at a significance level of (p < 0.05)
RESULTS AND DISCUSSION
The data observed in the existing study was normally distributed. Table 1 displays SBS of RMGIC bonded to different conditioning regimes to dentin. The maximum SBS values were observed in PAA (20.44±3.92) and the minimum values were noted (12.54±2.25). RMGIC conditioned with NYL (13.45±2.44) and control group (12.45±2.25) were comparable p>0.05. Furthermore, conditioning of RMGIC with ECL (18.54±3.24), TE (19.44±3.74), SE (18.22±3.55) and PAA (20.44±3.92) were comparable p>0.05.
Table 1: Comparison of means and SD for bond strength values among study groups using ANOVA and Tukey multiple comparisons test
| Type of RMGIC | Group 1: Nd-Yag laser (NYL) irradiation | Group 2: Er,Cr:YSGG laser (ECL) irradiation | Group 3: Total etch (Optibond solo Plus) | Group 4: Self-Etch (Clearfill SE) | Group 5: Dentin Conditioner
10% Polyacrylic acid) PAA |
Group 6: Control
No Treatment |
P-value! |
| Fiji II LC | 13.45±2.44a | 18.54±3.24b | 19.44±3.74b | 18.22±3.55b | 20.44±3.92b | 12.45±2.25a | ˂0.05 |
Different upper script letters indicate statistical differences (p < 0.05).
! Showing significant difference among study group (ANOVA
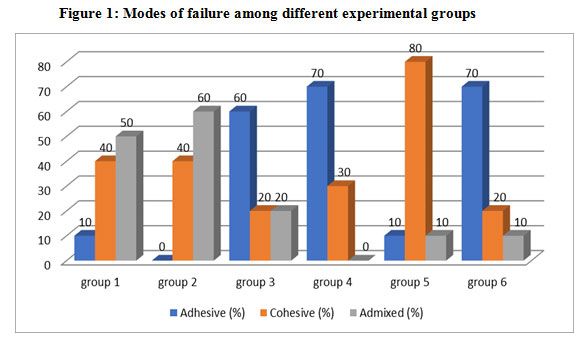
Mode of failure amongst all experimental groups, adhesive failure type was pertinent (Figure 1). In laser, irradiated groups admixed failure was common. Moreover, In TE and SE groups adhesive failure was found in majority. Dentin conditioned with PAA exhibited cohesive failure.
Figure 1: Modes of failure among different experimental groups
The existing study was based on the hypothesis that dentin conditioned with ECL and NYL and bonded to RMGIC will exhibit comparable bond integrity to different conditioning regimes. The present in-vitro experiment revealed that bond strength of dentin conditioned with ECL was comparable to PAA, SE and TE. Whereas, dentin conditioned with NYL displayed low bond strength scores compared to different conditioning regimes but was comparable to non-treatment group. Therefore, the hypothesis was partially accepted. The durability of a restoration is contingent on the adhesive capability, which can be assessed by SBS testing. In the present study SBS of the restoration was determined using universal testing machine. The method is simple to use, widely acceptable, provides comparative analysis and samples does not require further processing after bonding procedures (Sirisha, Rambabu, Ravishankar, et al., 2014; Sirisha, Rambabu, Shankar, et al., 2014).
Conditioners are used to promote adhesion, remove smear layer, improve surface energy and promote surface wettability (Tanumiharja et al., 2000). In the present study ECL at 0.5 W and 30 Hz was used to condition dentin prior to RMGIC. ECL works at a wavelength of 2780 micrometres displays strong affinity to hydroxyapatite crystals in dentin and water. In the existing study ECL at low level exhibited SBS (18.54±3.24) similar to dentin conditioned with PAA (20.44±3.92). This finding was in line with a study by (Alkhudhairy, Al-Johany, Naseem, et al., 2019; Ekworapoj et al., 2007; Garbui et al., 2013). A probable explanation to these conclusions is ECL at low level causes loss of water and collapse of the dentinal collagen resulting in reduction of hydrophilicity of dentin, which indirectly improves the suitability of hydrophobic polymeric materials like RMGIC to adhere well with the dentin structure (Alkhudhairy, Al-Johany, Naseem, et al., 2019). Furthermore, lased dentin results in smear free layer following easy penetration of RMGIC exhibiting strong bond affinity (Ekworapoj et al., 2007). Moreover, due to improved surface energy of lased dentin ionic exchange between the intermediary layer of RMGIC and dentin structure might influence better bod integrity (Alkhudhairy, Vohra and Naseem, 2019b).
The other laser used in the present study NYL (13.45±2.44) exhibited statistically significant difference compared to PAA (20.44±3.92) TE (19.44±3.74) and SE (18.22±3.55) experimental groups. These findings were not in harmony with the outcome of work carried out by Kobayashi et al., (2003) and Aljdaimi et al., (2018). In authors opinion diversity in results can be attributed to power and frequency of laser, duration of laser, type of dentin (human or bovine) and kind of RMGIC and conditioning regimes. Moreover, since the power of NYL used in the current study was 1W it is conceivable that NYL at low level did not significantly removed the smear layer, altered the hybrid layer and produced morphological changes in dentin compromising bond integrity (Kobayashi et al., 2003).
Dentin conditioned with TE (19.44±3.74), SE (18.22±3.55) and PAA (20.44±3.92) displayed comparable bond strength. In the current study, 37% phosphoric acid was used for 5 sec to condition dentin. Reducing the conditioning time to 5 sec enhances micro-mechanical retention by forming resin tags, enhances resin infiltration of RMGIC and results in less loss of calcium ions improving ionic bonding of RMGIC with dentin (Tay et al., 2001).Moreover, SE adhesives (18.22±3.55) displayed SBS values similar to dentin conditioned with PAA (20.44±3.92) and TE (19.44±3.74). Our findings, of the present study were in concurrent with the results of (Besnault et al., 2004; Coutinho et al., 2006). Multiple explanations can be given for such outcomes. Primary, reason is SE adhesives and RMGIC both have carbon-carbon bonds which on polymerization changes to covalent bonds improving adhesion. Secondly, presence of water in both RMGIC and SE adhesives improves their wettability on dentinal surface which indirectly improve RMGIC spread over dentin conditioned surfaces with SE adhesives. Thirdly, low modulus of elasticity of RMGIC renders low polymerization shrinkage compared to resin composites (Besnault et al., 2004; Coutinho et al., 2006). Based on the result of our finding the author recommends use of SE adhesives to condition dentin as the conditioning method is less technique sensitive and more user friendly and provide desirable results similar to TE.
The highest bond strength scores were observed in group conditioned with PAA (20.44±3.92). Possible explanation reported for this outcome is that dentinal surface conditioned with acid creates irregularities and pores on the substrate surface boosting adhesion (Hamama et al., 2014). This finding was in synchronization with work of Tanumiharja et al., (2000). Moreover, in the same study by Tanumiharja et al.,(2000) reported that wettability of surface enhances infiltration of HEMA into collagen network of dentin increasing bond scores. Recently, work by Sauro et al., (2018) reported dentin conditioned with PAA increases the risk of collagen collapse and degradation at dentin/ material interface under prolong stress, mechanical cycling and saliva immersion ultimately leading to bond failure. Therefore, though the SBS values of PAA conditioned group is the highest in the existing study, PAA as conditioner should be used with caution.
Based on fracture analysis, admixed and cohesive failure was found to be pertinent in lased dentin and surface conditioned with PAA. Such failure type can be attributed to porosity within the material which act as a centre of stress resulting in breakage within the material, implying better bond integrity (Saraç et al., 2009).
The biggest limitation of the study was not carrying out the micro morphological analysis of the bonded surface. Conditioning of dentin surface using laser is a unique concept and needs further clinical and non-clinical assessment in the form of durability testing of conditioned surface, surface energy measurements, surface profiling and scanning electron microscopic evaluation. Promising invitro results not always can assure clinical success. These laboratory-based studies act as a screening tool for selection of materials used in in-vivo study design. Therefore, more studies to extrapolate the findings and recommendations of present study should be performed.
CONCLUSION
The use of ECL and not NYL has a protentional to be used as conditioning regime in clinical setting prior to application of RMGIC.
REFERENCES
Aljdaimi, A., Devlin, H. and Dickinson, M. (2018), Effect of the Er: YAG laser on the shear bond strength of conventional glass ionomer and BiodentineTM to dentine European Journal of Dentistry, Wolters Kluwer Medknow Publications, Vol. 12 No. 3, pp. 380–385.
Alkhudhairy, F., Al-Johany, S.S., Naseem, M., Bin-Shuwaish, M. and Vohra, F. (2019), Dentin bond strength of bioactive cement in comparison to conventional resin cement when photosensitized with Er,Cr:YSGG Laser Pakistan Journal of Medical Sciences, Vol. 36 No. 2, available at:https://doi.org/10.12669/pjms.36.2.1284.
Alkhudhairy, F., AlKheraif, A., Bin-Shuwaish, M., Al-Johany, S., Naseem, M. and Fahim Vohra, Mc. (2018), Effect of Er,Cr:YSGG Laser and Ascorbic Acid on the Bond Strength and Microleakage of Bleached Enamel Surface Photomedicine and Laser Surgery, Vol. XX No. Xx, pp. 1–8.
Alkhudhairy, F., Naseem, M., Ahmad, Z.H., Alnooh, A.N. and Vohra, F. (2019), Efficacy of phototherapy with different conventional surface treatments on adhesive quality of lithium disilicate ceramics Photodiagnosis and Photodynamic Therapy, Elsevier B.V., Vol. 25, pp. 292–295.
Alkhudhairy, F., Naseem, M., Bin-Shuwaish, M. and Vohra, F. (2018) Efficacy of Er Cr: YSGG laser therapy at different frequency and power levels on bond integrity of composite to bleached enamel, Photodiagnosis and Photodynamic Therapy, Vol. 22, available at:https://doi.org/10.1016/j.pdpdt.2018.02.019.
Alkhudhairy, F., Vohra, F. and Naseem, M. (2019a), Influence of Er,Cr:YSGG Laser Dentin Conditioning on the Bond Strength of Bioactive and Conventional Bulk-Fill Dental Restorative Material Photobiomodulation, Photomedicine, and Laser Surgery, available at:https://doi.org/10.1089/photob.2019.4661.
Alkhudhairy, F., Vohra, F. and Naseem, M. (2019b) Influence of Er,Cr:YSGG Laser Dentin Conditioning on the Bond Strength of Bioactive and Conventional Bulk-Fill Dental Restorative Material Photobiomodulation, Photomedicine, and Laser Surgery, available at:https://doi.org/10.1089/photob.2019.4661.
Alkhudhairy, F., Vohra, F., Naseem, M. and Ahmad, Z.H. (2019), Adhesive bond integrity of dentin conditioned by photobiomodulation and bonded to bioactive restorative material”, Photodiagnosis and Photodynamic Therapy, Elsevier B.V., Vol. 28, pp. 110–113.
Besnault, C., Attal, J.P., Degrange, M. and Ruse, D. (2004), Self-etching adhesives improve the shear bond strength of a resin-modified glass-ionomer cement to dentin”, Journal of Adhesive Dentistry, Vol. 6 No. 1, pp. 55–59.
Cardoso, M.V., Delmé, K.I.M., Mine, A., Neves, A. de A., Coutinho, E., De Moor, R.J.G. and Van Meerbeek, B. (2010), Towards a better understanding of the adhesion mechanism of resin-modified glass-ionomers by bonding to differently prepared dentin, Journal of Dentistry, Vol. 38 No. 11, pp. 921–929.
Coutinho, E., Van Landuyt, K., De Munck, J., Poitevin, A., Yoshida, Y., Inoue, S., Peumans, M., et al. (2006), Development of a self-etch adhesive for resin-modified glass lonomer Journal of Dental Research, Vol. 85 No. 4, pp. 349–353.
Ekworapoj, P., Sidhu, S.K. and McCabe, J.F. (2007), Effect of surface conditioning on adhesion of glass ionomer cement to Er,Cr:YSGG laser-irradiated human dentin”, Photomedicine and Laser Surgery, Vol. 25 No. 2, pp. 118–123.
Garbui, B.U., De Azevedo, C.S., Zezell, D.M., Aranha, A.C.C. and Matos, A.B. (2013), Er,Cr:YSGG Laser dentine conditioning improves adhesion of a glass ionomer cement”, Photomedicine and Laser Surgery, Vol. 31 No. 9, pp. 453–460.
Hamama, H.H., Burrow, M.F. and Yiu, C. (2014), Effect of dentine conditioning on adhesion of resin-modified glass ionomer adhesives Australian Dental Journal, Vol. 59 No. 2, pp. 193–200.
Hotz, P., McLean, J.W., Sced, I. and Wilson, A.D. (1977), The bonding of glass ionomer cements to metal and tooth substrates, British Dental Journal, Vol. 142 No. 2, pp. 41–47.
Imbery, T.A., Namboodiri, A., Duncan, A., Amos, R., Best, A.M. and Moon, P.C. (2013), “Evaluating dentin surface treatments for resin-modified glass ionomer restorative materials”, Operative Dentistry, Vol. 38 No. 4, pp. 429–438.
Kobayashi, C.A., Osada, T., Fukunaga, H., Kawawa, T., Fujishima, A., Miyazaki, T., Kimura, Y., et al. (2003) Effect of Nd:YAG laser irradiation on shear bond strength of glass-ionomer luting cement to dentin surface, International Journal of Prosthodontics, Vol. 16 No. 5, pp. 493–498.
Mjör, I.A. and Gordan, V. V. (2002), Failure, repair, refurbishing and longevity of restorations Operative Dentistry.
De Munck, J., Van Landuyt, K., Peumans, M., Poitevin, A., Lambrechts, P., Braem, M. and Van Meerbeek, B. (2005), A critical review of the durability of adhesion to tooth tissue: Methods and results Journal of Dental Research, February.
Powis, D.R., Follerås, T., Merson, S.A. and Wilson, A.D. (1982), Improved adhesion of a glass ionomer cement to dentin and enamel. Journal of Dental Research, Vol. 61 No. 12, pp. 1416–1422.
Saraç, D., Külünk, S., Saraç, Y.S. and Karakas, Ö. (2009), Effect of fluoride-containing desensitizing agents on the bond strength of resin-based cements to dentin, Journal of Applied Oral Science, Bauru School of Dentistry, University of Sao Paulo, Vol. 17 No. 5, pp. 495–500.
Sauro, S., Faus-Matoses, V., Makeeva, I., Martí, J.M.N., Martínez, R.G., Bautista, J.A.G. and Faus-Llácer, V. (2018), Effects of polyacrylic acid pre-treatment on bonded-dentine interfaces created with a modern bioactive resin-modified glass ionomer cement and subjected to cycling mechanical stress, Materials, MDPI AG, Vol. 11 No. 10, available at:https://doi.org/10.3390/ma11101884.
Sirisha, K., Rambabu, T., Ravishankar, Y. and Ravikumar, P. (2014), Validity of bond strength tests: A critical review-Part II, Journal of Conservative Dentistry, Medknow Publications, 1 September.
Sirisha, K., Rambabu, T., Shankar, Y.R. and Ravikumar, P. (2014), Validity of bond strength tests: A critical review: Part I, Journal of Conservative Dentistry, Medknow Publications.
Swartz, M.L., Phillips, R.W. and Clark, H.E. (1984), Long-term F Release from Glass Ionomer Cements, Journal of Dental Research, Vol. 63 No. 2, pp. 158–160.
Tanumiharja, M., Burrow, M.F. and Tyas, M.J. (2000), Microtensile bond strengths of glass ionomer (polyalkenoate) cements to dentine using four conditioners Journal of Dentistry, Vol. 28 No. 5, pp. 361–366.
Tay, F.R., Smales, R.J., Ngo, H., Wei, S.H. and Pashley, D.H. (2001), Effect of different conditioning protocols on adhesion of a GIC to dentin. The Journal of Adhesive Dentistry, Vol. 3 No. 2, pp. 153–67.
Vohra, F., Alghamdi, A., Aldakkan, M., Alharthi, S., Alturaigi, O., Alrabiah, M., Al-Aali, K.A., et al. (2018), Influence of Er: Cr: YSGG laser on adhesive strength and microleakage of dentin bonded to resin composite. In-vitro study, Photodiagnosis and Photodynamic Therapy, Vol. 23, available at:https://doi.org/10.1016/j.pdpdt.2018.08.002.
Yoshida, Y., VanMeerbeek, B., Nakayama, Y., Snauwaert, J., Hellemans, L., Lambrechts, P., Vannerle, G., et al. (2000), Evidence of chemical bonding at biomaterial-hard tissue interfaces, Journal of Dental Research, Vol. 79 No. 2, pp. 709–714.