1Department of Physical Therapy and Health Rehabilitation, College of Applied
Medical Sciences, Majmaah University, Al Majmaah 11952, Saudi Arabia
2Department of Applied Health Sciences, AIHMS, New Delhi, India
3Department of Physiotherapy, Santosh University, Ghaziabad, India
4College of Applied Medical Sciences, Al Mareefa University, Riyadh 13713, Saudi Arabia
Corresponding author email: m.molla@mu.edu.sa
Article Publishing History
Received: 15/01/2022
Accepted After Revision: 29/03/2022
Text neck syndrome is a stress/overuse injury in the neck caused by leaning forward for extended periods of time, such as when reading and texting on a cellphone, and has been linked to stress injuries. The primary cause of the disorder is the weight of the head which while bending it forward or looking down at a 45 to 60 degree angle during texting produces around 50 to 60 pounds of stress on the neck, increasing pressure over time and causing damage. While the majority of treatment is mostly based on. The aim of the present study was to evaluate the effectiveness of treatment between osteopathic intervention and modified cervical exercise therapy program among text neck syndrome patients. In total, seventy two patients were selected based on inclusion/exclusion criteria out of which 6 dropped out. In the end, 66 patients were randomly were allocated into two groups namely, the osteopathic treatment group(n=33) and modified cervical exercise group(n=33). The treatment program was followed for 3 weeks and the patients were evaluated for Numeric Pain Rating Scale(NPRS), Neck disability index(NDI) , Cervical range of motion as well as cranio-vertebral angle to measure the treatment effectiveness. Paired t-test showed significant differences in both groups between variables mean scores from the baseline readings after three weeks of intervention. Statistical significant differences were observed in the mean scores for all the outcome measures including NPRS, Cervical ROM, Craniovertebral angle and NDI. The result of the study suggests that Osteopathic treatment technique along with modified cervical exercise therapy is more effective than modified cervical exercise alone in treating text neck syndrome patients(p<0.05).
Osteopathy, Modified Cervical Exercise, Smartphone, Text Neck Syndrome.
Miraj M, Zhrani M. A, Alanazi A, AlQahtani M, Ahmad F, Kashoo F, Raheem S. A, Kumar D, Chauhan P, Unnikrishnan R. K, Muthuswamy H. Effectiveness of Osteopathic Treatment Versus Modified Cervical Exercise Therapy in Patients with Text Neck Syndrome. Biosc.Biotech.Res.Comm. 2022;15(1).
Miraj M, Zhrani M. A, Alanazi A, AlQahtani M, Ahmad F, Kashoo F, Raheem S. A, Kumar D, Chauhan P, Unnikrishnan R. K, Muthuswamy H. Effectiveness of Osteopathic Treatment Versus Modified Cervical Exercise Therapy in Patients with Text Neck Syndrome. Biosc.Biotech.Res.Comm. 2022;15(1). Available from: <a href=”https://bit.ly/3Gt6lxW“>https://bit.ly/3Gt6lxW</a>
INTRODUCTION
The term, “Text neck” first coined by Dr. Dean L. Fishman is used to describe neck pain and injury due to the repetitive stress that results from extreme watching or texting on handheld devices such as cell phone or tablet used too frequently and for longer duration of time (David et al.,2021). Literature review states that the prevalence of text neck syndrome ranges from 30%-68% among different population and cohorts across different parts of the world (Kazeminasab et al.,2021; Safri et al.,2017 and Cohen,2015). In one of the published research, it was also observed that 79% of the population between the age group of 18-44 years, have their cell phones with them almost all the time of the day except for only 2 hours of their working day spend without cell in hand (David et al.,2021).
Increasingly, large number of people are spending greater amount of time on handheld devices Smartphone, computer, tablets and e-readers (Cohen,2014; Lee and Song, 2014).The end result is prolonged flexion of the neck, bent over these electronic devices resulting in the “text neck”. It is a growing health concern and has the potential to affect millions of people all over the world. Bad posture such as stooping posture with prolonged sitting texting on mobile, sedentary lifestyle, weak physique especially upper torso are potential risk factors for the development of text neck syndrome (Genebra et al.,2017; Ariens et al.,2001).
Various treatment are suggested to manage text neck syndrome(Pangarkar and Lee,2011). Cervical Neck exercises including Neck isometrics, Neck Strengthening exercises, stretching of platysma and other neck muscles such as trapezius are some of the mainstay of treatments to manage the condition(Pangarkar and Lee,2011; Skelly et al., 2020).Similarly, electrotherapeutic modalities like Ultrasound, TENS etc. as well as other forms of physical therapy such as aqua therapy are been used to treat the condition for managing pain but have been found with limited success(Corvillo et al.,2020).
Osteopathy, is yet another system of therapy founded in early 19th century, used effectively in treating musculoskeletal conditions. It is based upon the theory that manipulation of muscles and bones to promote structural integrity could restore or preserve health. This alternative medicine technique emphasizes upon manual readjustment, myofascial release and other physical manipulation of muscle tissue and bones (Mandara et al.,2010; Groisman et al.,2020). Recent studies stated that Osteopathic treatment of the cervical spine have helped assist healing of injury or dysfunction of the cervical region, although there is limited research regarding the effectiveness of osteopathic treatment for chronic neck pain and neck disability(Cohen, 2015).
Similarly, modified cervical exercises combining Mackenzie’s exercise program and Kendall’s exercise program are known to effectively decrease neck pain and increase ROM, thereby contribute to the recovery and improvement of forward head posture(Pangarkar and Lee,2011).The McKenzie’s exercise program involves repeated self-treatment exercises performed by patients, with a focus on extension exercises. The exercise program includes joint motion exercises, manual therapy, and patient education. Likewise, Kendall’s exercise program focuses on the notion that unstable forward head posture can be corrected via alignment exercises, although this not only involves strengthening the deep neck flexors and shoulder retractors, but also stretching the chest muscles(Skelly et al.,2020). Combining the two exercise techniques, a modified cervical exercises program is developed which were simple and easy-to-follow techniques.
The two techniques even though been extremely good, advantageous and easy to perform are never been evaluated for their efficacy in managing the symptoms of text neck syndrome. Therefore the aim of the present study is to measure the effectiveness of the two manual therapy methods in treating text neck syndrome symptoms .
MATERIAL AND METHODS
Subjects: The design of the study was a randomized controlled trial(pretest-posttest experimental control group design). All participants provided their written informed consent prior to participation in the study. This study was conducted in department of physiotherapy at AIHMS and Santosh Physiotherapy Centre. The inclusion criteria for this study were the following: age 18 to 30 years, both genders ,more than one year using a smartphone, having symptoms of text neck syndrome, using smart phones for more than 4 hours/day, VAS at least 3/ 10, a CVA of less than 54°, no disabilities affecting dizziness or balance, no nervous system or musculoskeletal disease, and no respiratory problems(Robert and Dhasaradharaman,2020). The following exclusion criteria were applied: vestibular system problems, and being unable to perform the exercises (Kong, Kim and Shim, 2017).
Necessary ethical approval was taken from the Department Ethical Committee, AIHMS, New Delhi(AIHMS/21/421). Those participants who were willing to be a part of the study were included in the study
A minimum sample size of 60 patients was required using statistical power of 80%,the effect size of 0.20 and 0.05 significance level to measure effectiveness of technique used in the study. A total of 72 patients were recruited who fulfilled the inclusion criteria. However due to personal reasons or failure to continue treatment, only 66 patients could participate in the study, equally divided into two groups(Experimental group A i.e Osteopathy + Modified Cervical, and Control group B i.e Modified Cervical exercises alone), each having 33 participants.
Procedure: The 66 selected subjects were randomly allocated on the basis of inclusion and exclusion criteria into two groups i.e. group A and group B after taking informed consent from them. The selected participants were assessed based on outcome measures (NPRS, NDI, ROM, CVA) initially and after 3 week of intervention. After the baseline assessment , Group A were receive osteopathy treatment (Sacral release, Diaphragm release, Scalene release, Sternocleido mastoid release, Bypass release, Circular release, Opposite release, Clavical ligament release). The treatment was given for 25 minutes, 2 days in a week for 3 weeks (Kong, Kim and Shim, 2017). The group was asked to perform modified cervical exercise program, once at home for 5 times in a week for 3 weeks.
Group B performed modified cervical exercises in the following manner: (1) slowly pull the subject’s neck to the head, thereby attaching the chin to the neck; (2) the subject’s eyes should be looking directly forward; (3) hold both hands on the back of the subject’s head; (4) ask the subject to push his/her head backwards against the hands; and (5) ask for the hands to be spread as wide as possible in order to stretch the pectoralis major. Each group performed three sets of exercises, with one set being defined as five circuits, which is, performing 7 sec of exercises followed by 10 sec of rest. To reduce the potential for errors, physical therapists supervised the performance of the exercises. The exercise took only 8 minutes and was performed 5 times in a week for 3 weeks.
Various outcome measures were evaluated to measure the effectiveness of the treatment methods. Numeric Pain Rating Score to measure pain, Range of motion (ROM) in terms of Cervical flexion and extension and cranio vertebral angle (CVA) and functional index in form of Neck disability Index was measured to evaluate the treatment efficacy on Day O and Day 21(i.e after 3 weeks of Treatment).
The craniovertebral angle is defined as the angle between a horizontal line passing through the C7 vertebra and a line extending from the tragus of the ear to the C7 vertebra. Measurement of craniovertebral angle is one of the common method in assessing forward head posture14. A picture of lateral view of each subject was taken to assess the FHP. A camera was placed at a distance of 150 m . The height of camera was adjusted on shoulder level. A self-balanced position was chosen to standardize the head and neck posture of subjects. To achieve this position, subjects moved their head and neck into flexion and extension in the full range and gradually reduced its range until the subject eventually stopped moving and maintained the head and neck in a natural position . The necessity of maintaining a natural position before the photography was explained to the subjects . The tragus of the ear was clearly marked and a pointer was taped to the skin overlying the spinous process of the C7. Once the picture was obtained, it was used for measuring the craniovertebral angle.
Statistical Analysis: Statistical analysis was done by using SPSS software, version 17. Paired t- test for within group analysis and T- test for between group analysis was used to find out the comparison between osteopathy treatment along with modified cervical exercises and modified cervical exercises alone in patient’s with text neck syndrome using various outcome measures such as NPRS, NDI, ROM and CVA. A statistically significant difference was defined as p value less than 0.05
RESULTS AND DISCUSSION
The mean age of the patients in both groups A and were 23.71± 4.45 and 22.5 ± 5.51 respectively (p>0.05). The result of study suggests that there was a significant decrease in VAS and NDI and increased range of motion and craniovertebral angle was observed in both the groups as compared to the control group. However, on further analysis between the 2 treatment, the osteopathy treatment was more effective than Modified cervical Exercise in text neck syndrome(p<0.05*).
Figure 1
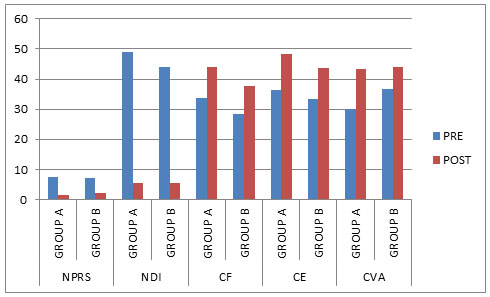
NPRS= Numerical pain rating scale, NDI = Neck Disability Index, CF = Cervical Flexion, CE = Cervical Extension, CVA = Craniovertebral Angle
As evident from Fig. 1, Numeric Pain Rating Scale the pre, middle and post mean and SD of Group A and Group B: pre mean and SD is 7.35±0.745and 7.05±1.146 and post mean and SD is 1.45±1.146 and 2.20±1.281 respectively (p=0.027*). This result shows that there is a significant difference in NPRS over 3 weeks of treatment between the groups.
With reference to measuring the improvement in cervical flexion Range of Motion between Group A and Group B was that pre mean and SD was 33.75±3.782 and 28.45±5.671 and post mean and SD was 44.05±5.960 and 37.85±6.277(p=0.013**) respectively. This result shows that there is a significant difference between week 0 and 3 between the groups suggesting osteopathic treatment along with modified cervical exercises being better than modified cervical exercises alone in treating text neck syndrome symptoms.
Likewise on measuring Cervical Extension Range of Motion (CEROM) the pre mean and SD for group A and B was 36.40±7.358 and 33.30±9.091 respectively. Over treating the two groups for over 3 week, the post mean and SD readings for CEROM was 48.35±7.569 and 43.55±9.456 respectively(p=0.031*) showing better effectiveness in Group A.
Similarly, we measured the Cranio vertebral angle for both the group at week 0 and 3 (called the and post mean and SD of Group A and Group B). The pre mean and SD of CVA was 30.05±5.482 (group A) and 36.80±6.771 (group B). The post mean and SD at week 3 for group A and B was 42.25±5.447and 44.10±6.439 respectively(p=0.027*), found to be statistically significant.
Similarly for measuring NDI (Neck Disability Index) the pre and post mean and SD of Group A and Group B was 49.10±14.037(group A) and 43.95±11.696(group B) and post mean and SD is 5.35±7.436(group A)and 8.10± 4.767(group B), found to be statistically better than group B(p=0.028*).
The purpose of present study was to examine effectiveness between osteopathic treatment and modified cervical exercise in patient with Text neck syndrome. The result of the study suggests that statistically significant decrease in VAS, NDI and increase in ROM and CVA were observed in both the protocols however osteopathic treatment along with modified cervical exercise was more effective than modified cervical exercise alone in treating the patients of text neck syndrome(Fig. 1).
An earlier study conducted by Mandara et al (2010) suggested that Osteopathy manipulative treatment added to standard care was able to significantly reduce neck pain and disability as compared to Sham manipulation and standard care. However the effect of treatment seems to depend upon the number of manipulative sessions. Lately, another recent study done by Groisman et al.(2020) has compared the immediate effects of high-velocity, low-amplitude manipulation treatment with a craniocervical flexion exercise protocol on various outcome measures using pain intensity (VAS), cervical spine range of motion (ROM), pressure-pain thresholds (PPT) and EMG activation of sternocleidomastoid muscle (SCM) during a craniocervical flexion test (CCFT) in patients with non specific chronic neck pain.
The study suggested that while both the manual interventions improved ROM and pain immediately following treatment, Manipulation therapy was more effective than exercise in improving ROM. However, none of the interventions led to changes in EMG. The findings of our study differed from this study in the way that while we measured the effects of the osteopathic treatments for 3 weeks, the study conducted by Groisman et al (2020) was done to study the immediate effects. Moreover, we used text neck syndrome patients to be more specific as compared to the above mentioned study where non-specific chronic neck pain patients were recruited for the study.
With reference to the studies conducted earlier by other authors such as Rathore (2003) and later by Kong, Kim and Shim (2017) on the use of modified cervical exercise in mitigating the effects of text neck syndrome patients, it was found that both McKenzie protocol and Kendal exercise were effective in reducing neck pain and improve ROM. However with reference to the number of repetitions per day it was suggested the modified head exercises proved effective in increasing the range of motion of those with forward head posture when performed three times a day14. In the current study, we used modified cervical exercises, performed for at least 8 minutes, once a day for 5 times in a week for over 3 weeks. Similarly, a report by Rathore (2003) has concluded that McKenzie protocol significantly improved cervical ROM, pain intensity level and neck functional activity level when compared to the control group treated with conventional treatment.
Though there were significant differences between the two studies. While it was conducted on machine operators, the present study was conducted on text neck syndrome patients. In the present study combined benefits of osteopathic treatment along with modified cervical exercises might be responsible for better outcome measure results as compared to modified cervical exercise alone. It was concluded that while osteopathic treatments might have corrected the postural aberrations acutely bringing about biomechanical alignment bringing about marked modifications in the cognitive and sensory perception of pain, the McKenzie exercises particularly by means of directional preference exercises improved self-confidence in patients might be by restoring the manipulation corrections which may have resulted in better results.
This in turn have also might have helped in reducing anxiety created by anticipation of pain and related fear beliefs towards a given physical performance as explained by Roddey et al., (2002) in earlier conducted studies. It was demonstrated that the effect of Kendall’s exercise program in patients with forward head posture cause stretching of neck extensors, pectoralis major and deep neck flexor bringing about significant improvement in postural alignment. In some of the earlier studies conducted it was concluded that Osteopathy manipulative treatment is a reasonable alternative to parenteral nonsteroidal anti-inflammatory medication for patients with acute neck pain in the ED settings, ( Safri et al 2017). Thus, when combined with modified cervical exercises, osteopathic treatment might help not only to correct the neck malalignment but might help to maintain the corrections for time duration due to the modified cervical exercises.
Limitations of the Study: The study had several limitations. The sample size was small, duration of study was limited, moreover procedural and instrumental error could not be controlled during the study. Despite the relationship between treatment and clinical improvement, a definitive causal relationship cannot be concluded due to certain other limitations of the study design. These data (VAS, NDI, ROM, CVA) were collected after their final treatment session after week 3. It would be possibly better to obtain data after each individual session to measure the improvements more accurately. Moreover, for measuring CVA, the photographs are taken in sitting position. As the CVA in sitting position is affected by other parts of spine which may lead to confusion with forward head posture due to which error occurs in calculating the CVA.
CONCLUSION
It is concluded that osteopathic treatment in combination with modified cervical exercises is significantly better in treating text neck syndrome patients than modified cervical exercises alone. Future studies can be done using larger sample size as well as longer follow-up to measure the interventions efficacy. Moreover, different intervention procedures and parameters could be experimented for improving cervical muscle strength and endurance.
Ethical Clearance:Necessary ethical approval was taken from the Department Ethical Committee, AIHMS, New Delhi India (AIHMS/21/421). Those participants who were willing to be a part of the study were included in the study
Conflict of Interest: Authors declare no conflict of interest.
ACKNOWLEDGEMENTS
The authors are grateful to the Deanship of Scientific Research, Al Majmaah University for funding through Vice Deanship of Scientific Research Chairs via Ref. no. RGP-2019-35.
REFERENCES
Ariëns GA, van Mechelen W, Bongers PM, Bouter LM, van der Wal G.(2001) Psychosocial risk factors for neck pain: a systematic review. Am J Ind Med ;39(2):180–93.
Cohen SP.(2015) Epidemiology, diagnosis, and treatment of neck pain. Mayo Clin Proc. ;90(2):284–99.
Corvillo I, Armijo F, Álvarez-Badillo A, Armijo O, Varela E, Maraver F.(2020) Efficacy of aquatic therapy for neck pain: a systematic review. Int J Biometeorol. 2020;64(6):915–25.
David D.; Giannini C.; Chiarelli F.; Mohn A.(2021) Text Neck Syndrome in Children and Adolescents. Int. J. Environ. Res. Public Health 2021, 18, 1565. https://doi.org/10.3390/ijerph18 041565
Genebra CVDS, Maciel NM, Bento TPF, Simeão SFAP, Vitta AD. (2017) Prevalence and factors associated with neck pain: a population-based study. Braz J Phys Ther. 21(4):274–80.
Groisman S, Malysz T, de Souza da Silva L, Rocha Ribeiro Sanches T, Camargo Bragante K, Locatelli F, Pontel Vigolo C, Vaccari S, Homercher Rosa Francisco C, Monteiro Steigleder S, Jotz GP.(2020) Osteopathic manipulative treatment combined with exercise improves pain and disability in individuals with non-specific chronic neck pain: A pragmatic randomized controlled trial. J Bodyw Mov Ther. 24(2):189-195. doi: 10.1016/j.jbmt.2019.11.002. Epub 2019 Nov 13. PMID: 32507144.
Kazeminasab S., Nejadghaderi SA., Amiri P et al. (2022) Neck pain: global epidemiology, trends and risk factors. BMC Musculoskelet Disord 23, 26 : 1-13 https://doi.org/10.1186/s12891-021-04957-4
Kong YS; Kim YM and Shim JM. (2017)The effect of modified cervical exercise on smartphone users with forward head posture. J Phys Ther Sci 29(2) : 328 -331 doi:10.1589/jpts.29.328
Lee JI and Song HS.(2014) The Correlation Analysis between Hours of Smartphone Use And Neck Pain in the Gachon University Students. The acupuncture 31(2) : 99-111 Doi : https://doi.org/10.13045/acupunct.2014028.
Mandara A, CerianiGuzzetti G, GulisanoV, Fusaro A, Bado F.(2010) Osteopathic manipulative treatment for the effect on pain and disability. International Journal of Osteopathic Medicine;13: 105
Pangarkar S. and Lee PC.(2011) Conservative Treatment for Neck Pain: Medications, Physical Therapy, and Exercise. Phys. Med. And Rehab. Clin. Of North America. 22(3) : 503-20.doi : 10.1016/j.pmr.2011.04.001
Rathore S. ( 2003) Use of McKenzie cervical protocol in the treatment of radicular neck pain in a machine operator. J Can Chiropr Assoc. 2003;47(4):291-297.
Robert F, Dhasaradharaman K. (2020) A Comparative Study between Stretching With Postural Modification versus Stretching Alone In Smartphone Users with Neck Disability. International Journal of Health Sciences and Research. 2020;10(2):125-30
Roddey TS, Olson SL, Grant SE: The effect of pectoralis muscle stretching on the resting position of the scapula in persons with varying degrees of forward head/rounded shoulder posture. J Manual ManipTher, 2002, 10: 124–128.
Safri S, Kolahi A-A, Hoy D, Buchbinder R, Mansournia MA, Bettampadi D, et al. (2017) Global, regional, and national burden of neck pain in the general population, 1990–2017: systematic analysis of the Global Burden of Disease Study. BMJ. 2020;368.
Skelly AC, Chou R, Dettori JR, Turner JA, Friedly JL, Rundell SD, et al. (2020) AHRQ Comparative Efectiveness Reviews. In: Noninvasive nonpharmacological treatment for chronic pain: a systematic review update. Rockville: Agency for Healthcare Research and Quality (US); 2020.


