College of Nursing, Jeddah, King Saud bin Abdulaziz University for Health Sciences, KSA
Corresponding author email: najjarH@ksau-hs.edu.sa
Article Publishing History
Received: 10/07/2020
Accepted After Revision: 09/09/2020
Evidence-based practice (EBP) is recognized internationally as a foundational element in health care. When delivered in a context of caring and a supportive organizational culture, the highest quality of care and best patient outcomes can be achieved. The study aimed to describe the evidenced-based practice and research utilization amongst critical care nurses at the National Guard Hospital in Jeddah, Saudi Arabia. This study followed a cross-sectional descriptive quantitative approach. The study was conducted in the critical care units of a military hospital in Saudi Arabia. A convenience sampling method including 96 critical care nurses was used. Data was collected using a tool that has established reliability and validity. Descriptive statistics included (mean, SD, frequencies, and percentages) and Inferential statistics were carried out such as (independent t-test, and Chi-square) using the Statistical Package for the Social Sciences.
The biggest barrier was reported as insufficient time on the job to implement new ideas, M= 3.10, from the construct of setting. The lowest barrier was reported as I feel the benefits of changing practice will be minimal, M= 2.45. More females (79%) reported the construct of setting as the barrier, M= 2.88. There was a significant difference noted in the four constructs and age, P= 0.00 was noted. For EBP and research utilization to become the golden standard of health care, health care organizations and systems should advocate its use. Even though EBP has been highlighted as a core competency for health care professionals, the uptake of EBP into practice remains a challenge.
Evidenced-Based Practice, Research, Critical Care Nurses
Alnajjar H, de-Beer J. Describing Evidenced-Based Practice and Research Utilization Amongst Critical Care Nurses at A Military Hospital in Jeddah, Saudi Arabia. Biosc.Biotech.Res.Comm. 2020;13(3).
Alnajjar H, de-Beer J. Describing Evidenced-Based Practice and Research Utilization Amongst Critical Care Nurses at A Military Hospital in Jeddah, Saudi Arabia. Biosc.Biotech.Res.Comm. 2020;13(3). Available from: https://bit.ly/32Y6W8Q
Copyright © Alnajjar and de-Beer This is an open access article distributed under the terms of the Creative Commons Attribution License (CC-BY) https://creativecommons.org/licenses/by/4.0/, which permits unrestricted use distribution and reproduction in any medium, provide the original author and source are credited.
INTRODUCTION
Evidence-based practice (EBP) is recognized internationally as a foundational element in health care (Lehane et al 2019). EBP has been defined as a problem-solving approach to the delivery of health care that integrates the best evidence from studies and patient care data with clinician expertise and patient preferences and values. When delivered in a context of caring and a supportive organisational culture, the highest quality of care and best patient outcomes can be achieved (Melnyk et al, 2009). The emergence of EBP has been fast spreading within health care and has resulted in changing the way health care is undertaken (All Answer Ltd, 2018).
Determinants of successful implementation of EBP in clinical practice have been described in multiple studies and relate to the individual, the clinical question, the evidence, and the environment or context in which these occur. The successful implementation of EBP is dependent on the individual, the clinical question, the evidence, and the context (Rios & Thabane, 2010; Krupski, et al., 2008;). Several process models that have been developed to guide nurses through EBP. Most are process models that focus on guiding the nurse through the necessary steps however these models have not been consistently and uniformly used (Titler, 2018).
Nurses are the largest health professional groups that can help achieve implementing EBP as they are in direct contact with patients where assessment and care interventions are made daily (Hagdu, Almaz & Tsheay, 2015). Evidence-based nursing practice allows nurses to provide the highest quality care based on the best evidence that can exist, which in turn results in a positive outcome in nursing interventions. To improve current and future patient outcomes it is essential to incorporate an EBP approach in clinical nursing ( Elarab, El Salem, Behalik, et al, 2012). Today clinical decision making is driven by EBP which is a theory- derived promoting optimal patient outcomes by incorporating the best evidence, the nurses’ experience, and patient preferences (Penz,2006).
However, despite nurses being in a pivotal position to achieve optimal patient outcomes, research findings are often conveyed to researchers and not nurses in the clinical setting. As a result of this, the concept of research utilization was introduced into nursing only in the 1970s (Stetler, 2001). In addition to this, Patelarou, Kiriakouis, Stamou, et al (2017) highlighted that health professionals’ adoption of EBP in practice remains limited even though they “are familiar with EBP and believe in its value”.
Further to this, the healthcare professional has a positive attitude towards EBP however their understanding and skills related to EBP are inadequate. Despite the benefits of EBP, there are many personal and organizational barriers impeding EBP implementation. These barriers can be summarized in terms of the attitude of nurses to undertake research (lack of research knowledge; lack of communication; lack of communication from knowledgeable colleagues; weakness of evaluating the research), organizational constraints (time; lack of authority; unsupportive personnel) and research communication (not readily available reports, research jargon, and literature) ( Panagiari, 2008 Shayan et al 2019).
Although there are increased demands for the utilization of research in nursing practice, there are differences in the nurses’ education level regarding research utilization (Elarab et al., 2012). Evidence-based practice requires making professional decisions based on systematically gathered evidence drawn from research and experience based on the patients’ desires and needs in a specific situation (Dalheim et al., 2012). As nurses are engaging more in EBP assistance is needed in providing greater evidence base guidance to deliver effective care defined by the best research. This will also assist in resolving problems in the clinical setting to achieve excellence in delivering patient care (Al Touby , 2017).
Increased awareness that nursing should become an evidence-based profession has recently become more and more important in several countries around the world (Biesta, 2007). EBP may be more successfully implemented if the interventions overcome identified barriers (Dalheim et al., 2012; Hadid & Barnawi, 2012). As nurses gain EBP knowledge and skills, they realize it’s not only practical within the context of their practice setting, but they also develop a passion for their roles as EBP practitioners resulting in them delivering a higher quality of care with improved patient outcomes (Fineout-Overholt, Melnyk, Stillwell and Williamson, 2010).
The Critical Care Unit (CCU) is a high tech, fast-paced environment. Admission to a CCU is mostly unplanned and the patients are in a critical condition (Hashim and Hussin, 2012). Admissions are due to illnesses which are often life-threatening resulting from trauma, surgery, sepsis or shock where patients are susceptible to dysfunction of multiple organ systems including respiratory, cardiovascular and digestive system (Wright-Myrie, Kahwa, and Dover-Roberts, 2013). The intensive care environment imposes physical, emotional, and cognitive stresses on Critical Care Nurses (CCNs) and they must be adequately trained to deal with rapidly changing technology, which can be both a support and a burden to staff members (Almerud, Alapack, Fridlund and Ekebergh, 2008).
CCNs must assess and monitor the patients’ physiological responses to treatment, paying close attention to conditions requiring immediate interventions. Patients admitted to CCUs tend to be physiologically unstable, requiring constant cardiac and respiratory monitoring and continuous adjustments of treatment. These challenges require CCNs to be skilled at interpreting, integrating, and responding to a variety of information (Losa Iglesias, Vallejo, and Fuentes, 2010).
There are many reasons put forward to why it is so difficult to provide evidence-based care. “One of the most obvious is the fact that new evidence is being generated at an ever-increasing rate. It is estimated that nearly one million new articles are posted on PubMed annually” (Loannidis et al, 2018, p: 795). Therefore, health care professionals are faced with the challenge of finding, appraising, and integrating new evidence into the routine practice (Shayan et al, 2019). Further to this, most healthcare professionals are unaware of the poor quality of evidence that results in improper care and wastage of health resources, Therefore, efforts should focus on training healthcare professionals to be more sensitive to the limitations of the evidence, doing critical appraisals and improving communication skills. This will equip health care professionals to effectively summarize and discuss medical evidence with patients to improve decision-making. (Loannidi et al, 2018).
EBP remains limited, although most health care professionals are familiar with EBP and believe in its value (Patelarou et al, 2017). Evidence-based practice and research utilization is a phenomenon that is relatively under-researched within the context of Saudi Arabia (Alqahtani et al, 2018; Alshehri et al, 2017; Gulman et al, 2017; Bahammam & Linkawi 2014). and more specifically within the context of nursing and critical care nursing. Critical care is an area of specialization where patients are physiologically compromised within a highly technical environment. Hence critical care nurses should have a strong knowledge base on EBP guidelines to provide the best possible care. This study was conducted within critical care nursing in the context of Saudi Arabia and has contributed to research within EBP within these contexts.
MATERIAL AND METHODS
The study was conducted in the National Guard hospital in critical care units, Jeddah, Saudi Arabia. This is a tertiary hospital that has 596 beds. Two hundred and one beds are allocated to the critical care units within 10 critical care units. This study followed a cross-sectional descriptive design. The ethical approval of the study (approval NO. RJ15/013/J) was received from the Research Office at King Abdullah International Medical Research Centre. Before the data collection, the informed consent form was signed by each participant of the study. Sampling was completed using a convenience sampling method. The total population of CCNs was 277, however only 96 critical care nurses working in 10 adult critical care units. Only critical care nurses with a minimum of six months of experience were included in the study. Data collection was done using a questionnaire that consisted of four sections. Section A represented the demographic section of respondents, section B represents the meaning of EBP, Section C represented barriers to EBP, and research utilization, Section D, represented the participation in research activities.
Section C of the tool was adopted by Funk, Champagne, Tornquist, and Wiese (1991). The original questionnaire consists of 28 items into four subscales namely adopter, organization, research, and communication. The responses were provided on a Likert scale, that was rated from not at all familiar to very familiar (1, not all familiar; 2, to little extent familiar; 3, to moderate extent familiar; 4, to a greater extend familiar; 5, completely familiar). The 28 items on the tool were adopted from the original tool and amended for the Saudi context. This section of the tool was divided into four constructs namely the setting (11 items), research (4 items), nurse (8 items), and presentation (5 items).
Section B, and D were developed by the researchers after a literature review. A pilot test was completed using the entire tool and revealed a Cronbach alpha of 0.90. Those involved in the pilot test were excluded from the final data collection of the study. The pilot test included five critical care lecturers. Section D of the tool has existing reliability of Cronbach alpha of 0.65-0.80 and 0.61-0.71 (Funk, Champagne, Wiese & Tornquist, 1991) and 0.74-0.87 (Kang, 2015). However, the tool was piloted and showed a Cronbach alpha of 0.937. SPSS version 20 was used for data analysis.
RESULTS AND DISCUSSION
A total of 96 CCNs participated in the study. 82, 3% of respondents were female. The majority (33.3%) of respondents were between 35-45 years of age. The most common educational qualification among respondents was a bachelor’s degree in nursing (69.8%). Most respondents 30.2% had nursing experience within 1-5 years with only 10.4% of respondents having more than 20 years of experience in critical care.
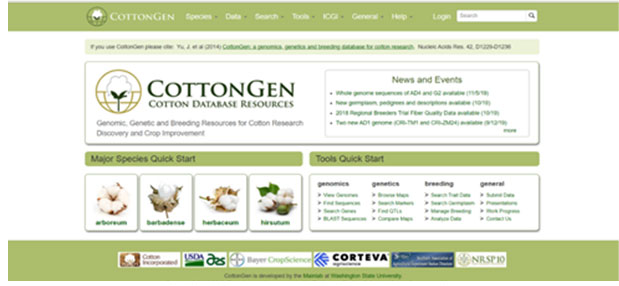
Figure 1: Meaning of EBP
Participants were asked about the meaning of EBP and the majority of participants (53%) indicated that EBP includes best clinical expertise, best available evidence, and patient preferences, which is the correct response as EBP includes patient preferences, clinical expertise, and best available evidence.
Table 1. Barriers to research utilization and EBP in terms of constructs
| Construct | N | Minimum | Maximum | Mean | Std. Deviation |
| Setting | 96 | 12.00 | 60.00 | 34.38 | 9.07 |
| Presentation | 96 | 6.00 | 30.00 | 16.57 | 4.44 |
| Nurse | 96 | 6.00 | 30.00 | 16.31 | 4.27 |
| Research | 96 | 4.00 | 20.00 | 10.84 | 3.15 |
The above table highlights that barriers relating to the construct of the setting were the biggest barrier, M=34.38 with the construct of research being the lowest barrier, M= 10.84.
Table 2. Barriers related to research utilization and EBP
| Construct | Mean | Std. Deviation | ||
| 1. I feel the benefits of changing practice will be minimal | Nurse | 2.45 | 1.239 | |
| 2. I am unwilling to change/try new ideas | Nurse | 2.53 | 1.151 | |
| 3. The research has methodological inadequacies | Research | 2.55 | .961 | |
| 4. I do not see the value of research for practice | Nurse | 2.60 | 1.235 | |
| 5. I am isolated from knowledgeable colleagues with whom to discuss the research | Nurse | 2.68 | 1.110 | |
| 6. The administration does not support EBP implementation | Setting | 2.68 | 1.138 | |
| 7. I am unaware of the research- | Nurse | 2.70 | 1.087 | |
| 8. Research reports/articles are not readily available | Presentation | 2.72 | .948 | |
| 9. I see little benefit for myself | Nurse | 2.73 | 1.128 | |
| 10. Access to research evidence is poor (slow or no computers, or databases) | Setting | 2.74 | 1.126 | |
| 11. Statistical analyses are not understandable | Presentation | 2.75 | 1.016 | |
| 12. The research is not relevant to practice | Presentation | 2.76 | 1.054 | |
| 13. The research has not been replicated | Research | 2.76 | 1.074 | |
| 14. The amount of research information is overwhelming | Research | 2.76 | 1.023 | |
| 15. I am uncertain whether to believe the results of the research | Research | 2.77 | .968 | |
| 16. Implications for practice are not made clear | Presentation | 2.80 | .902 | |
| 17. The facilities are inadequate for implementation | Setting | 2.81 | .921 | |
| 18. The relevant literature is not compiled in one place | Presentation | 2.82 | 1.086 | |
| 19. I do not feel capable of evaluating the quality of the research | Nurse | 2.83 | 1.063 | |
| 20. There is resistance to make changes in the work setting | Setting | 2.83 | 1.185 | |
| 21. I feel the benefits of changing practice will be minimal | Nurse | 2.84 | .944 | |
| 22. Other staff are not supportive of the implementation | Setting | 2.84 | 1.079 | |
| 23. The administration will not allow implementation | Setting | 2.85 | 1.161 | |
| 24. There is not support or incentives for clinical practice development | Setting | 2.91 | 1.152 | |
| 25. I do not have time to read the research | Setting | 2.99 | .968 | |
| 26. I do not feel I have enough authority to change patient care procedures | Setting | 3.08 | 1.262 | |
| 27. I feel results are not generalizable to own setting | Setting | 3.09 | 1.077 | |
| 28. There is insufficient time on the job to implement new ideas | Setting | 3.10 | 1.147 | |
Table 2 above indicates that the biggest barrier to research utilization and EBP related to the construct of the setting. From this construct, the biggest barrier was of insufficient time on the job to implement new ideas which had a mean score of M= 3.10. The average mean score of the top five barriers to research and EBP was M= 3.03.
Table 3. Gender differences in terms of the different constructs
| Construct | Gender | N | Mean | Std. Deviation | Std. Error Mean |
| Presentation | Female | 79 | 2.7679 | .77782 | .08751 |
| Male | 17 | 2.7353 | .55920 | .13563 | |
| Research | Female | 79 | 2.7089 | .82278 | .09257 |
| Male | 17 | 2.7206 | .63049 | .15292 | |
| Nurse | Female | 79 | 2.7236 | .74530 | .08385 |
| Male | 17 | 2.6961 | .55664 | .13500 | |
| Setting | Female | 79 | 2.8808 | .79726 | .08970 |
| Male | 17 | 2.7941 | .53774 | .13042 |
Table 3 highlights that even though there is no statistical difference between gender and the barriers to research utilization and EBP, from the construct of setting, females perceived the setting to more of barrier M= 2.88 than males, M= 2.79.
Table 4. Barriers related to age
| Paired Samples Test | |||||
| Paired Differences | t | df | Sig. (2-tailed) | ||
| 95% Confidence Interval of the Difference | |||||
| Upper | |||||
| Pair 1 | Age – presentation | 34.92194 | 39.182 | 95 | .000 |
| Pair 2 | Age – research | 34.98890 | 38.879 | 95 | .000 |
| Pair 3 | Age – nurse | 34.97111 | 39.099 | 95 | .000 |
| Pair 4 | Age – setting | 34.82539 | 38.904 | 95 | .000 |
Table 4, highlights that there are significant differences in terms of age between the barriers related to the various constructs. Younger nurses within the age group of fewer than 25 years (4.2%) found the construct of presentation of t research to be the biggest barrier, M= 34.92, with the majority of nurses between 25-35 years (49%), found that barriers related to the construct of research were the biggest barrier, M=34.98. Nurses between the ages of 35-45 years (33.3%), reported that barriers related to the construct of the nurse were the biggest barrier, M=34.97. Finally, the older nurses, between the age group of 45- 60 years (13.7%) reported that the construct of the setting was the biggest barrier, M= 34.82. Hence, within this study, it can be assumed that the younger nurses reported barriers related to research-related issues, whilst the older nurses reported barriers to shortcomings in themselves as nurses and the organization.
Table 5. Participation in research during your employment at the current hospital
| Frequency | Percent | |
| Not at all | 50 | 52.1 |
| Once | 33 | 34.4 |
| 2-3 times | 10 | 10.4 |
| More than 3 times | 3 | 3.1 |
| Total | 96 | 100.0 |
Table 5 above highlights that only half (50%) of the respondents’ participation in research during their time of employment at the present hospital. Only N=33 (34.4%) of respondents participated in research once; while N=10(10.4%) participated in research 2-3 times and N= 3(3.1%) participated in research more than 3 times.
Further to this, it was noted that respondents N= 24 (51.1%) between the age groups of 25-35 years were more active in research participation that all other groups. In addition it was found that more females n= 35 (36.4 %) participated in research than males N= 11 (10.4%). Most respondents N=23(69.7%) who participate in the research were mostly from the adult general CCU whilst only N= 10 (30.3%) respondents from the pediatric CCU participated. In addition, N= 18 (18.7%) searched for information, research or evidence to support their nursing practice several times a week, whilst N= 28 (29.2) searched weekly, N= 33(34.4%) 1-2 times per month, N=13 (13.5%) less than once a month, whilst, N= 4 (4.2%) never searched for any information. Also, only N= 19 (19.8%) of respondents had a subscription to a health journal.
This study highlighted that only 50 % of nurses were involved in the research. In addition, even though 50% were not involved in research, 53% of respondents had the correct conceptualization of what EBP was. The correct meaning of EBP included the best clinical expertise, best available evidence, and patient preferences. Sackett et al, (1996) suggest the best available evidence is, therefore, integration of three factors; clinical expertise, results of high-level systematic, clinical research, and patient preference. However, Hoffmann et al (2013) expanded the definition to include available resources. Further to this, the current study did not highlight any significant correlation between the lack of EBP and research utilization with a lack of understanding of what EBP meant.
However, Al-Baghlie and Al-Almaie (2004), found that physicians who had no understanding of what evidence-based medicine was, were the ones who had a negative attitude towards evidence-based medicine. It is interesting to note that Al- Baghlie and Al-Almaie (2004) reported that”…the poor understanding of evidenced-based medicine could lead to misunderstandings where physicians who misunderstood evidenced-based medicine would be protective of their current way of practicing medicine. Contrary to the findings Mallion and Brooke (2016), reported that even though almost one-third of respondents never heard about EBP which was higher in from previous studies, the median total score for EBP beliefs was positive.
The least reported barrier to research utilization and EBP was ” I feel the benefits for changing practice will be minimal” There is a possibility that nurses within this study found that EBP is beneficial. This can be further attributed to the fact that changing practice can be related to the benefits of changing behavior which can be related to the best possible care for patients. as Greenhalgh et al., (2014) implore, EBP should always have “the care of individual patients as its top priority.
Further to this, one of the major findings of this study highlighted that the top barrier of research utilization was insufficient time: to implement new ideas and the time to read research More recently, Mallion & Brooke (2016), and Gomes Perieria, da Silva Peixoto de Oliveira Cardoso & Correia dos Santos Cardosa Martins (2012) also reported that the most significant barrier to the implementation of EBP was a lack of time. This is reiterated by Shayan et al (2019) who also highlighted that time is a barrier to the implantation of EBP. The lack of time to conduct research, to read research findings, and to implement new ideas were all barriers of EBP related to time.
Further to this, a lack of time has been related to increased workload. Health care institutions tend to have a culture of busyness that is rewarded and valued, however, it does not encourage nurses to spend time sitting and reading (Dalheim, Harthug, Nilsen, et al 2012; Jordan, Bowers & Morton, 2016). The lack of time to read and document research is well cited in the literature (Brown, Kim, Stichler & Fields, 2010; Breimaier, Halfens, & Lohrmann, 2011). According to Barends et al (2017), time is important for EBP to be realized as generating research evidenced and the use of evidence is time-consuming. Besides, numerous studies highlight that an increased workload reduces time on the job for EBP related articles (, Khammarnia et al, 2015; Adib‐Hajbaghery, 2007 Ebrahimi et al, 2017).
The findings of this study highlight the top five barriers, as well as other barriers to research utilization and EBP, was related to the construct of the setting. Most respondents reported that setting or the organization related factors were the biggest challenges. These barriers included “other staff members not being supportive of implementation”, “administration will not allow implementation” and “there is no support or incentives for clinical practice”. Kaplan et al., (2014) reported that support from administrators and leaders is important to promote the use of research among clinical nurses. According to organizational support is vital to EBP sustainability. When there is no organizational will to perform and support EBP, EBP will not be achieved. Further to this if managers within an institution do not support staff to acknowledge and embrace EBP then EBP cannot be achieved (Shayan et al 2019; Florczak,2016).
One of the major barriers of EBP in this study was that “administration does not support EBP implementation”. This finding is reiterated by Renolen et al., (2018), who found that clinical nurses experience a lack of recognition and support from leaders. Hence, they proposed that it is important for leaders to continuously support nurses in their efforts of EBP. Aasekjær et al., (2016) also reported that for an organization’s program of EBP to survive long term, leaders should sustain commitment and engagement towards this program. In addition, this study highlighted the top third barrier to research utilization and EBP was nurses not having enough authority to make changes related to patient care. This similar to the findings of Jordan et al., (2016); Baird &Miller (2015); Gerrish & Cooke (2013). However, according to Dunbar et al., (2007) the lack of authority of nurses can be addressed through the development of shared governance systems. Hence nurses and leaders can work together to have one voice in decision making and policy changes that affect patient care and work environments.
A statistically significant difference was noted with age and barriers to research utilization and EBP. Hence, within this study, it can be assumed that the younger nurses reported barriers related to research-related issues, whilst the older nurses reported barriers to shortcomings in themselves as nurses and the organization. This is similar to the findings of Khammamia et al., (2015), who reported that the older respondents in their study reported more organizational barriers than the younger respondents. This finding was attributed to the fact that older individuals might be more aware of the current trends or know that EBP is something that they should be doing. Also, older individuals may be more familiar with hospital systems and factors associated with the use of EBP.
Another significant finding within this study shows that the majority of nurses only searched for information, research, or evidence at least 1-2 times a month. This could be attributed to a lack of time and a lack of skills to search (Bahadori, Raadabadi & Ravangard et al, 2016; Renolen, Høye, Hjälmhult, et al, 2018). According to Majid et al (2011), EBP is a multistep process where nurses need sufficient time for EBP. In addition, Young and Ward (2001) also found that a lack of information skills is a barrier. Further to this, the low use of electronic information sources could be due to a lack of knowledge about the existence of such sources and limited literature searching skills of the nurses (Jones, Schilling and Pesut 2011; Hider et al. 2009).
The findings of this study highlight that the barriers to EBP and research utilization within critical care within Saudi Arabia is similar to barriers faced by health care professionals in developed countries. It is therefore important to support health care professionals who are challenged with limit EBP capabilities. The findings of this study recommend that the phenomenon of barriers to EBP and research utilization be explored from a qualitative lens within a Saudi context to getting a richer understanding of this phenomenon. Also, the study can be repeated with a larger sample size in more than one setting.The study limitation included one setting inclusive of just CCNs. In addition, within this study, although the total population was 277 nurses only 96 CCNs participated. This is a response rate of 35% and highlights that nurses are reluctant to partake in research.
CONCLUSION
For EBP and research utilization to become the golden standard of health care, health care organizations and systems should advocate its use. Even though EBP has been highlighted as a core competency for health care professionals, the uptake of EBP into practice remains a challenge.
REFERENCES
Aasekjær, K., Waehle, H. V., Ciliska, D., Nordtvedt, M. W., & Hjälmhult, E. (2016). Management involvement—a decisive condition when implementing evidence‐based practice. Worldviews on Evidence‐Based Nursing, 13(1), 32-41.
Adib‐Hajbaghery, M. (2007). Factors facilitating and inhibiting evidence‐based nursing in Iran. Journal of advanced nursing, 58(6), 566-575.
Al- Baghlie, N., & AL-ALmaie, SM. (2004). Physician attitudes towards evidence-based medicine in eastern Saudi Arabia. Ann Saudi Med, 24(6), 425-428.
All Answers Ltd. (November 2018). Benefits of Evidence-Based Practice (EBP). Retrieved from
https://nursinganswers.net/essays/benefits-evidence-based-practice-ebp-1216.php#citethis Accessed on 18 July 2020.
Almerud, S., Alapack, R.J., Fridlund, B. & Ekebergh, M. (2008). Beleaguered by technology: care in technologically intense environments. Nursing Philosophy, 9(1), 55-61.
Alqahtani, M. M., Kashoo, F. Z., & Ahmad, F. (2018). Current scenario of evidence-based practice and rationale of preferred approach in stroke rehabilitation among physiotherapists in Saudi Arabia: A cross-sectional survey. Saudi Journal for Health Sciences, 7(1), 53.
Alshehri, M. A., Alalawi, A., Alhasan, H., & Stokes, E. (2017). Physiotherapists’ behavior, attitudes, awareness, knowledge, and barriers in relation to evidence-based practice implementation in Saudi Arabia: a cross-sectional study. International journal of evidence-based healthcare, 15(3), 127.
Al Touby, Salem & Larson, Elaine & Noureddine, Samar & Altaweli, Roa & Nagshabandi, Elham & Abdel Aziz El Seesy, Nagla & Hanafy, Nesreen & Abubakar, Fadma & Ibrahim, Radhwan. (2017). Building Evidence-Based Practice in Resource-Limited Settings: Exemplars of success. Global Journal for Research Analysis. 6(4). 715.
Bahadori, M., Raadabadi, M., Ravangard, R., & Mahaki, B. (2016). The barriers to the application of the research findings from the nurses’ perspective: A case study in a teaching hospital. Journal of education and health promotion, 5(14).
Bahammam, M. A., & Linjawi, A. I. (2014). Knowledge, attitude, and barriers towards the use of evidence-based practice among senior dental and medical students in western Saudi Arabia. Saudi medical journal, 35(10), 1250
Barends, E., Villanueva, J., Rousseau, D. M., Briner, R. B., Jepsen, D. M., Houghton, E., & Ten Have, S. (2017). Managerial attitudes and perceived barriers regarding evidence-based practice: An international survey. PloS one, 12(10), e0184594.
Baird, L. M. G., & Miller, T. (2015). Factors influencing evidence-based practice for community nurses. British journal of community nursing, 20(5), 233-242
Biancofiore, G., Barsotti, E., Catalani, V., Landi, A., Bindi, L., Urbani, L., Desimone, P., Stefanini, A., Sansevero, A. & Filipponi, F. (2007). Nurses’ knowledge and application of evidence-based guidelines for preventing ventilator-associated pneumonia. Minerva anestesiologica, 73(3), 129-134.
Breimaier, H. E., Halfens, R. J., & Lohrmann, C. (2011). Nurses’ wishes, knowledge, attitudes, and perceived barriers on implementing research findings into practice among graduate nurses in Austria. Journal of clinical nursing, 20(11‐12), 1744-1756.
Brown, C. E., Kim, S. C., Stichler, J. F., & Fields, W. (2010). Predictors of knowledge, attitudes, use, and future use of evidence-based practice among baccalaureate nursing students at two universities. Nurse Education Today, 30(6), 521-527.
Dalheim, A., Harthug, S., Nilsen, RM., Nortveldt, MW. (2012). Factors influencing the development of evidence-based practice among nurses: a self-report survey. BMC Health Serv Res, (12): 367.
Dunbar, B., Park, B., Berger-Wesley, M., Cameron, T., Lorenz, B. T., Mayes, D., & Ashby, R. (2007). Shared governance: making the transition in practice and perception. Journal of Nursing Administration, 37(4), 177-183.
Ebrahimi, H., Seyedrasooli, A., Khodadadi, E., & Yousefi, F. (2017). Barriers and facilitators of evidence-based practice from the perspective of nurses who work in northwestern psychiatric centers of Iran. Journal of Research in Medical and Dental Science, 5(3), 29-36.
Elarab, H. S. E., El Salam, S. A., Behalik, S. G., & Eltayeb, H. E. (2012). Nurses, Practice, Knowledge, and Attitude towards Evidence-Based Practice at Yanbu general hospital-kingdom of Saudi Arabia.life science Journal-ACTA Zhengzhou University Overseas Edition, 9(3), 1062-1071.
Ghulman, F. A., Salem, O. A., Baddar, F. M., & Mubaraki, B. M. (2017). Barriers of evidence-based practice in Saudi Arabia. IOSR J Nurs Health Sci, 6, 10-14
Kang, H. (2015). Geriatric hospital nurses’ perceived barriers to research utilization and empowerment. Asian Nursing Research, 9(1): 65-72.
Florczak, K. L. (2016). Evidence-based practice: What’s new is old. Nursing Science Quarterly, 29(2), 108-112.
Fineout-Overholt, E., Melnyk, B.M., Stillwell, S.B. & Williamson, K.M. (2010). Evidence-Based Practice, Step by Step: Critical Appraisal of the Evidence: Part II: Digging deeper—examining the” keeper” studies. AJN The American Journal of Nursing, 110(9), 41-48.
Funk, S.G., Champagne, M.T., Wiese, R.A. & Tornquist, E.M. (1991). BARRIERS: the barriers to research utilization scale. Applied Nursing Research, 4(1), 39-45.
Gerrish, K., & Cooke, J. (2013). Factors influencing evidence-based practice among community nurses. Journal of Community Nursing, 27(4), 98-101.
Gommes Pereira, RP., da Silva Peixoto de Oliveira Cardosa, MJ., & Correia dos Santos Martins, (2012). Attitudes and barriers to evidence-based nursing practice in a community context.
Referencia: Revista Cientifican da Unidade de Investigacao em Ciencias da Saude: Dominio de Enfermagem, 3: 55- 62.
Greenhalgh, T., Howick, J., & Maskrey, N. (2014). Evidence-based medicine: a movement in crisis? BMJ, 348 (g3725).
Hadid, L.a.R.A. & Barmawi, M.a.A. (2012). Factors influencing the adoption of evidence-based principles in nursing education: A Jordanian perspective. Journal of Nursing Education & Practice, 2(2),71-79.
Hadgu, G., Almaz, S., & Tsehay, S. (2015). Assessment of nurses’ perceptions and barriers on evidence-based Practice in Tikur Anbessa Specialized Hospital Addis Ababa Ethiopia. Am J Nurs Sci, 4(3), 73-83.
Hashim, F., & Hussin, R. (2012). Family needs of patients admitted to the intensive care unit in a public hospital. Procedia-Social and Behavioral Sciences, 36, 103-111.
Hider, P. N., Griffin, G., Walker, M., & Coughlan, E. (2009). The information-seeking behavior of clinical staff in a large health care organization. Journal of the Medical Library Association: JMLA, 97(1), 47.
Hoffmann, T., Bennett, S., & Del Mar, C. (2013). Evidence-based practice across the health professions (2nd ed.). Sydney: Churchill Livingstone Elsevier.
Jensen, L.S. (2012) Perception of Barriers to Evidence-Based Practice Among Critical Care Nurses.
Jones, J., Schilling, K., & Pesut, D. (2011). Barriers and benefits associated with nurses’ information seeking related to patient education needs on clinical nursing units. The open nursing journal, 5, 24-30.
Jordan, P., Bowers, C., Morton, D. (2016). Barriers to implementing evidence-based practice in a private intensive care unit in the Eastern Cape. SAJCC, 32(2): 50-54.
Khammarnia, M., Haj Mohammadi, M., Amani, Z., Rezaeian, S., & Setoodehzadeh, F. (2015). Barriers to implementation of evidence-based practice in Zahedan teaching hospitals, Iran, 2014. Nursing research and practice, 2015.
Kaplan, L., Zeller, E., Damitio, D., Culbert, S., Bayley, K.B.,2014. Improving the culture of evidence-based practice at a Magnet(R) hospital. J. Nurses Prof. Dev. 30 (6), 274–280.
Krupski, T. L., Dahm, P., Fesperman, S. F., & Schardt, C. M. (2008). How to perform a literature search. The Journal of Urology, 179(4), 1264-1270.
Lehane, E., Leahy-Warren, P., O’Riordan, C., Savage, E., Drennan, J., O’Tuathaigh, C., … & Lynch, H. (2019). Evidence-based practice education for healthcare professions: an expert view. BMJ evidence-based medicine, 24(3), 103-108.
Loannidis, J. P., Stuart, M. E., Brownlee, S., & Strite, S. A. (2017). How to survive the medical misinformation mess. European journal of clinical investigation, 47(11), 795-802.
Losa Iglesias, M.E., Vallejo, R.B.D.B. & Fuentes, P.S. (2010). The relationship between experiential avoidance and burnout syndrome in critical care nurses: A cross-sectional questionnaire survey. International journal of nursing studies, 47(1), 30-37.
Mallion, J., & Brooke, J. (2016). Community – and hospital-based nurses’ implementation of evidence-based practice: Are there any differences? British Journal of Community Nursing, 21(3): 148-154.
Majid, S., Foo, S., Luyt, B., Zhang, X., Theng, Y. L., Chang, Y. K., & Mokhtar, I. A. (2011). Adopting evidence-based practice in clinical decision making: nurses’ perceptions, knowledge, and barriers. Journal of the Medical Library Association: JMLA, 99(3), 229.
Melnyk, B. M., Fineout-Overholt, E., Stillwell, S. B., & Williamson, K. M. (2009). Evidence-based practice: step by step: igniting a spirit of inquiry. AJN The American Journal of Nursing, 109(11), 49-52.
Panagiari, D. (2008). Barriers and Facilitators for implementing evidence-based practice among German nurses working in a general hospital (Master’s thesis, University of Twente).
Patelarou, A. E., Kyriakoulis, K. G., Stamou, A. A., Laliotis, A., Sifaki-Pistolla, D., Matalliotakis, M., … & Patelarou, E. (2017). Approaches to teach evidence-based practice among health professionals: an overview of the existing evidence. Advances in Medical Education and Practice, 8, 455.
Penz, K. L., & Bassendowski, S. L. (2006). Evidence-based nursing in clinical practice: implications for nurse educators. The Journal of Continuing Education in Nursing, 37(6), 250-254.
Renolen, Å., Høye, S., Hjälmhult, E., Danbolt, L. J., & Kirkevold, M. (2018). Keeping on track Hospital nurses’ struggles with maintaining workflow while seeking to integrate evidence-based practice into their daily work: A grounded theory study. International journal of nursing studies, 77, 179-188.
Rios, L. P., Ye, C., & Thabane, L. (2010). Association between framing of the research question using the PICOT format and reporting quality of randomized controlled trials. BMC Medical Research Methodology, 10(1), 11.
Shayan, S. J., Kiwanuka, F., & Nakaye, Z. (2019). Barriers associated with evidence‐based practice among nurses in low‐and middle‐income countries: A systematic review. Worldviews on Evidence‐Based Nursing, 16(1), 12-20.
Sackett, D., Rosenberg, W., Gray, J., Haynes, R., & Richardson, W. (1996). Evidence-based medicine: what it is and what it isn’t. BMJ: British Medical Journal, 312(7023), 71-72.
Stetler, C. B. (2001). Updating the Stetler Model of research utilization to facilitate evidence-based practice. Nursing Outlook, 49(6), 272-279.
Titler, M. G. (2018). Translation research in practice: An introduction. OJIN: The Online Journal of Issues in Nursing, 23(2).
Wright-Myrie. D., Kahwa, E., Dover-Roberts, D.(2013) Nutrition in critical illness: Critical care nurses’ knowledge and skills in the nutritional management of adults requiring intensive care – A review of the literature. Caribbean Journal of Nursing.1(1):49-55.
Young, JM., & Ward, JE. (2001). Evidence-based medicine in general practice: beliefs and barriers among Australian GPs. J Eval Clin Pract, 7(2): 201-210.