1 Saveetha Dental College, Chennai, India.
2Director of Academics, Department of Prosthodontics, Saveetha Dental College, Chennai, India.
Corresponding author email: drsbk25@gmail.com
Article Publishing History
Received: 13/07/2020
Accepted After Revision: 22/09/2020
Coronavirus disease (COVID-19) is a highly infectious disease which came to limelight in the beginning of the year 2020. With its rapid increase and spread, finally on 11th March, 2020, WHO declared the COVID-19 a pandemic disease . The possible routes of 2019- nCoV transmission are direct contact, droplet and aerosol transmission, fomite spread and feco-oral routes. Many dental procedures like tooth preparation, ultrasonic scaling, caries removal, etc produce aerosols and droplets which are contaminated with bacteria, viruses, and blood. These have the potential to spread infections to dental personnel and other people in the dental office. Not only this but also due to the characteristics of dental settings like closed air-conditioned space, the risk of cross infection may be high between dental practitioners and patients. A better understanding of aerosol transmission and its implication in dentistry can help us identify and rectify negligence in daily dental practice. It is crucial for dentists to refine preventive strategies to avoid the COVID-19 infection by focusing on patient selection, hand hygiene, all personal protective equipment (PPE), and caution in performing aerosol-generating procedures. These special precautions elaborated in this paper would help control the spread of COVID-19.
COVID-19, Corona, Dental Practice
Kachhara S, Nallaswamy D, Maiti S, Tulsani M. Dentistry Amid Corona Viral Disease-19: The Why, What, When and How of it ?. Biosc.Biotech.Res.Comm. 2020;13(3).
Kachhara S, Nallaswamy D, Maiti S, Tulsani M. Dentistry Amid Corona Viral Disease-19: The Why, What, When and How of it ?. Biosc.Biotech.Res.Comm. 2020;13(3). Available from: https://bit.ly/3h4TSTi
Copyright © Kachhara et al., This is an open access article distributed under the terms of the Creative Commons Attribution License (CC-BY) https://creativecommons.org/licenses/by/4.0/, which permits unrestricted use distribution and reproduction in any medium, provide the original author and source are credited.
INTRODUCTION
Coronavirus disease (COVID-19) is a highly infectious disease which came to limelight in the beginning of the year 2020. It spreads due to the newly discovered coronavirus which was first isolated on 7th January 2020 in Wuhan, China and was tentatively named as 2019-nCoV on 17th January 2020 (Mukhtar and Mukhtar, 2020). The International Committee on Taxonomy of Viruses named the virus SARSCoV-2 due to its resemblance to SARS coronavirus (Huffman, 2020). On 30th January 2020, the WHO declared this Chinese outbreak of COVID-19 to be a Public Health Emergency of International Concern (PHEIC) as per the International Health Regulations (IHR, 2005) posing a high risk to countries with vulnerable health systems. On February 11, 2020, the WHO Director-General, Dr. Tedros Adhanom Ghebreyesus, named this disease “COVID-19,” which is the acronym of “coronavirus disease 2019” (Cascella et al., 2020).
There was an unprecedented spread of the disease to 18 countries with four countries reporting human-to-human transmission. On February 28, 2020, WHO raised the threat to the CoV epidemic to “very high” level. Finally on March 11, as the number of COVID-19 cases outside China had increased 13 times and the number of countries involved had tripled with more than 118,000 cases in 114 countries and over 4,000 deaths, WHO declared the COVID-19 a pandemic. In India it started to spread from early March, where only 3 cases were reported till 3rd March. Soon there was a spurt, and by 5th March, 29 cases had been reported; mostly in Delhi, Jaipur and Agra in Italian tourists and their contacts (Singhal, 2020). As of 1st August,2020 in India, there are 17,51,919 confirmed cases out of which 16,96,558 have recovered, while 37,403 are dead. Currently, worldwide 1,80,13,101 cases have been confirmed to be corona positive, out of which 1,13,26,866 have recovered while 6,88,289 are deceased (WHO, 2020).
The possible routes of 2019- nCoV transmission are mainly direct contact and droplet transmission as stated in the 6th Edition of COVID-19 Treatment Regimen (Trial Implementation) published by the National Health Commission of the People’s Republic of China (2020). Aerosol transmission is also possible when there is an exposure to high concentrations of aerosols in a relatively closed environment (Ge et al., 2020). It is also critical to remember that the virus can survive on hands, objects or surfaces that were exposed to infected saliva in the previous nine days (Meng, Hua and Bian, 2020; Spagnuolo et al., 2020).
The evidence shows that many dental procedures like tooth preparation, ultrasonic scaling, caries removal, etc produce aerosols and droplets which are contaminated with bacteria, viruses, and blood. These have the potential to spread infections to dental personnel and other people in the dental office (Harrel and Molinari, 2004);(Ge et al., 2020). Not only this but also due to the characteristics of dental settings like closed air conditioned space, the risk of cross infection may be high between dental practitioners and patients. This leads us to understand the importance of strict and effective infection control protocols for dental practices and hospitals in countries/regions that are (potentially) affected with COVID-19. It is crucial for dentists to refine preventive strategies to avoid the COVID-19 infection by focusing on patient selection, hand hygiene, all personal protective equipment (PPE), and caution in performing aerosol-generating procedures (Meng, Hua and Bian, 2020). This paper aims to review and bring forth the necessary guidelines to be followed by dentists for their practice amid COVID-19.
The Corona Virus
Family: Coronaviruses belong to the family of Coronaviridae and order Nidovirales. Their genome consists of large, single, plus-stranded RNA (Gorbalenya et al., 2006; Fehr and Perlman, 2015). Currently, there are four genera of coronaviruses: αCoV, β-CoV, γ-CoV, and δ-CoV (Peng et al., no date), amongst which only the α-CoV and β-CoV mainly infect the respiratory, gastrointestinal, and central nervous system of humans and mammals (Perlman and Netland, 2009). This is not the first time the corona virus has spread throughout the world. Earlier SARS-CoV and the Middle East respiratory syndrome coronavirus (MERS-CoV) explored in 2002–2003 and in 2012, respectively, causing fatal severe respiratory diseases (Falsey and Walsh, 2003; Holmes, 2003). 2019-nCoV which was explored in Wuhan, like SARS-CoV belongs to the β-CoV genera according to the phylogenetic analysis based on the viral genome and is considered to be more fatal and dangerous than the previous two types (Wu et al., 2020).
Structure:
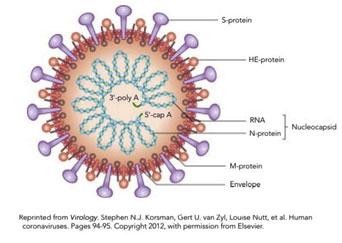
Figure 1: COVID-19 ( after WHO)
A typical corona virus has a round or elliptic and often pleomorphic form, and a diameter of approximately 60–140 nm with ‘spiked’ protein in its membrane envelope (Li, 2016). It expresses other proteins like RNA polymerase, 3-chymotrypsin-like protease, papain-like protease, helicase, glycoprotein, and accessory proteins (Zhou et al., 2020). The S protein from coronavirus can bind to the receptors of the host to facilitate viral entry into target cells like the human angiotensin converting enzyme (ACE2) (Belouzard et al., 2012). 2019-nCoV can effectively use ACE2 as a receptor to invade cells, which may promote human-to-human transmission. Like other CoVs, it is sensitive to ultraviolet rays and heat and can be effectively inactivated by lipid solvents including ether (75%), ethanol, chlorine-containing disinfectant, peroxyacetic acid and chloroform except for chlorhexidine (Cascella et al., 2020).
Manifestation: Patients with COVID-19 usually present with clinical symptoms of dry cough and shortness of breath. In addition symptoms such as fever, chills, muscle pain, headache, sore throat, reduced sense of smell (hyposmia), and abnormal taste sensation (dysgeusia) have also been reported, (Guan et al., 2020). In addition, abnormal chest X-ray and computed tomographic findings such as ground-glass opacities are typically found in the chest. Notably, about 80% of these patients have only mild symptoms that resemble flu like symptoms and seasonal allergies, which might lead to an increased number of undiagnosed cases(Ather et al., 2020) Currently, in the world out of the infected cases, 21,88,010 (98%) cases have shown mild symptoms while 49,074 are in serious condition(2%)(WHO).
The incubation period of this disease can range from 0 to 24 days which allows its transmission to occur even before any symptoms pop up(Guan et al., 2020; Rothe et al., 2020). The higher-risk patient population manifests symptoms typical of pneumonia or acute respiratory distress syndrome. Severe forms of this disease have a predilection for men with a mean age of 56 years with preexisting chronic illnesses such as cardiovascular disease or immunosuppression, (Ather et al., 2020). Some unconfirmed data suggest that Asian males have a large number of ACE2-expressing cells in the lung, which may partially explain the male predominance of COVID-19(del Rio and Malani, 2020).
Modes of transmission: In general, any respiratory virus infection can occur through(Moriyama, Hugentobler and Iwasaki, 2020):Contact (direct or indirect), Droplet spray in short range transmission, Aerosol in long-range transmission (airborne transmission). The common transmission routes of novel coronavirus include direct transmission (cough, sneeze, and droplet inhalation transmission) and contact transmission (contact with oral, nasal, and eye mucous membranes)(Lu, Liu and Jia, 2020). The virus is thought to spread mainly between people who are in close contact with one another (about 6 feet) and through respiratory droplets produced when an infected person coughs or sneezes(centre for disease control).
This had led to recommendations of social distancing. Another important route of transmission is if droplets of CoV-19 land on inanimate objects located nearby an infected individual and are subsequently touched by other individuals(for Disease Control and Others, 2020). In addition, studies have shown the presence of SARS-CoV-2 in both saliva and feces of the affected patients (To et al., 2020; Zhang, Wang and Xue, 2020). Some people without symptoms may also be able to spread the virus (Chan et al., 2020) and transmission may occur before the disease symptoms appear.
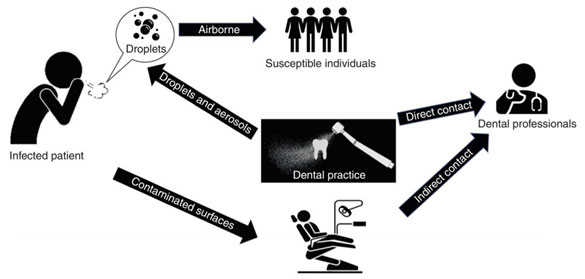
Corona and dentistry: SARS-CoV-2 can bind to human angiotensin converting enzyme 2 (ACE-2) positive cells (Zhou et al., 2020). The ACE2 are highly expressed on the mucosa of the oral cavity, epithelial cells of the tongue and also in the salivary glands. These findings have concluded that the oral cavity is a potentially high risk for 2019-nCoV infectious susceptibility, (Xu et al., 2020) and also a possible explanation for the presence of SARS-CoV-2 in secretory saliva(Hoffmann et al., 2020; Sabino-Silva, Jardim and Siqueira, 2020). Dental care settings involve face-to-face communication with patients, frequent exposure to saliva, blood, and other body fluids, and the handling of sharp instruments. This leads dental professionals to be at high risk for nosocomial infection, become potential carriers of the disease and also expose patients to cross-contamination (Fig 2).
Figure 2: Transmission of infection in dental setting.
Characteristics of dental set up which make it prone to spread of CoV-19
Production of bioaerosols : When performing dental procedures with a high speed handpiece or scaling using the ultra – sonic scaler, aerosols are generated(Organization and Others, 2020). These aerosols when combined with bodily fluids in the oral cavity, such as blood and saliva, create bioaerosols which are commonly contaminated with bacteria, fungi, and viruses and have the potential to float in the air for a considerable amount of time and be inhaled by the dentist or other patients (Grenier, 1995; Jones and Brosseau, 2015) leading to spread of disease. Based on the current epidemiological data, 2019-nCoV has higher transmissibility than SARS-CoV and MERS-CoV(Chen, 2020) making dental clinics very prone to spread of infection.
Small confined place: A dental clinic is a small confined place with an air conditioner whose strong airflow directs and propagates the droplet transmission. Most dental settings neither have airborne infection isolation rooms nor a respiratory protection program. Most of the equipment found in the dental settings do not withstand chemical sterilization and fumigation. Viruses can remain viable in aerosols for up to 3 hours and this makes dental clinic prone to spread of infection (van Doremalen et al., 2020).
Fomite spread:Human coronaviruses such as SARS-CoV, Middle East Respiratory Syndrome coronavirus (MERS-CoV), or endemic human coronaviruses (HCoV) can persist on surfaces like metal, glass, or plastic for up to a couple of days (Otter et al., 2016; Kampf et al., 2020) which make these contaminated surfaces in healthcare settings a potential source of coronavirus transmission. In dental practices, droplets and aerosols from infected patients are likely to contaminate the whole surface in dental offices. At room temperature, CoV-19 remains infectious from 2 h up to 9 days, and persists better at 50% compared with 30% relative humidity. Thus, keeping a clean and dry environment in the dental office would help decrease the persistence of 2019- nCoV (Peng et al., 2020).
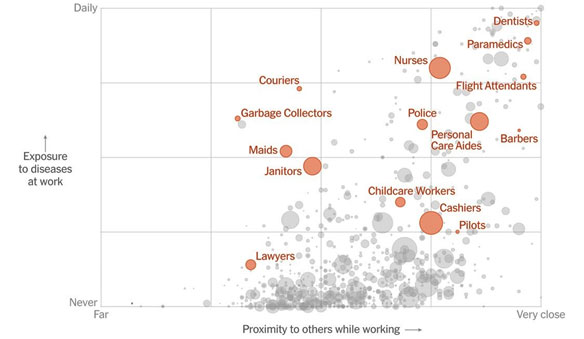
Floor: In a study in China, the floor swab samples tested positive for CoV-19 (ICU 70% , GW 15.4%), perhaps because of gravity and air flow causing most virus droplets to float to the ground(Guo et al., 2020). This brings to light that the floor itself can be contaminated in a dental setting and needs to be disinfected after every patient. In a news article by Lazaro Gamio, The New York Times, 15th March, 2020, the dental profession was shown to be at the highest risk amongst the health care workers (Fig 3). There is a potential for transmission of COVID-19 via aerosol, fomites or fecal-oral route that may contribute to nosocomial spread in the dental office setting (Peng et al., 2020). Therefore, modification of standard precaution and infection control regimen targeted toward 2019- nCoV is essential during this outbreak.
Figure 3: Workers who face greatest coronavirus risk. (A news article in New York Times dated 15th March, 2020)
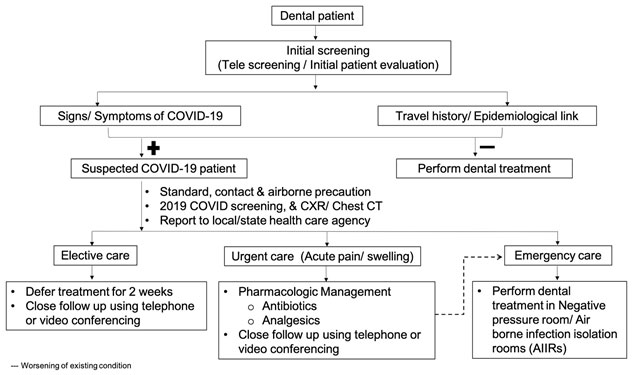
Our role as Dental Professionals (Jamal et al., 2020):a) Believe and follow reliable information.b) Avoid panic and rumors c) Take the recommendations from the local, state and government public health officials. d) Heed the call to temporarily suspend all non-urgent dental treatment until this crisis is over. Based on the experience gained from the previous outbreaks of SARS-CoV, data available on SARS-CoV-2 and its associated disease (COVID-19) and recommendations provided from dental council of india and indian dental association, certain specific measures are discussed here for dental patient management in this epidemic period of COVID-19 (Fig 4). On March 17, 2020, the Dental Council of India recommended that dentists postpone elective procedures for the country lockdown period and instead only provide treatment for dental emergencies.
Figure 4: Patient screening for COVID19 management.
Dental emergencies: American Dental Association says that dental emergencies are potentially life threatening and require immediate treatment to stop ongoing tissue bleeding, alleviate severe pain or infection, and include uncontrolled bleeding, cellulitis or any swelling that potentially compromise the patient’s airway and trauma involving facial bones. Urgent dental care focuses on the management of conditions that require immediate attention to relieve severe pain and/or risk of infection. These should be treated as minimally invasively as possible and are as follows: Severe dental pain from pulpal inflammation pericoronitis or third-molar pain, surgical post-operative osteitis, dry socket dressing changes, abscess, or localized bacterial infection resulting in localized pain and swelling. Tooth fracture resulting in pain or causing soft tissue trauma, Dental trauma with avulsion/luxation, Dental treatment required prior to critical medical procedures, Final crown/bridge cementation if the temporary restoration is lost, broken or causing gingival irritation, Biopsy of abnormal tissue, Amid the covid scenario, treatment should be provided only if it falls in any of these categories.
Dentists who should avoid practice (Jamal et al., 2020):Above the age of 55 years.Having underlying systemic conditions like diabetes mellitus, chronic liver disease, heart and kidney diseases, lung conditions, cancer, pregnancy, foreign travel history in the last 28 days. Anyone suffering from cough/ cold/ fever
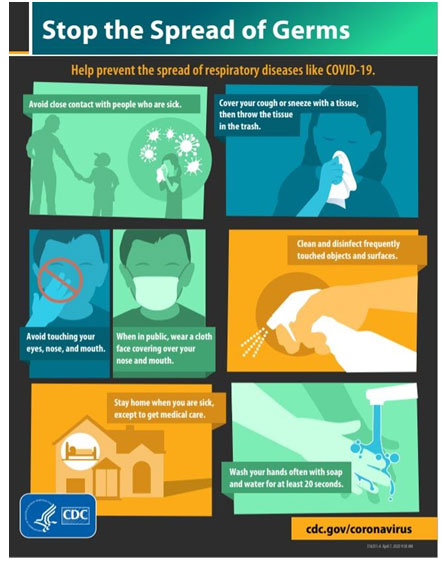
Precautions to be taken while practising dentistry:(A) Changes in Dental office:Waiting area management: Seating to be rearranged for social distancing. A spatial separation of at least 1m should be maintained between patients (Ge et al., 2020). Use of audio-visuals – These are posters or videos on TV screens regarding the behavioural changes like hand hygiene, respiratory hygiene, and cough etiquette to be followed during pandemic times (Fig 5).
Figure 5: Visual alert for sticking in the dental clinic.
Sign at entrance – Instructing patients having symptoms of a respiratory infection (e.g., cough, sore throat, fever, sneezing, or shortness of breath) to please reschedule their dental appointment and call their physician. Hand sanitizer upon entry and exit.Adequate ventilation required – For rooms with natural ventilation, 60 L/s per patient is considered adequate ventilation (World Health Organization, Chartier and Pessoa-Silva, 2009). Sensor devices like automatic hand sanitizer dispenser, auto liquid soaps, automatic door remote chair operating etc. can be introduced.
Patient Instructions: Patients should be informed that emergency work is given priority and elective procedures especially oral prophylaxis not recommended till further notice. Self declaration form to be filled by all the patients. This resolves legal as well as social stigma issues.Patients should visit the clinic only by appointment. Patient plus one attending person maximum that too if required. Face mask to be worn by patients as well as the accompanying person. Hand hygiene and respiratory instructions to be followed on how to use tissues to cover nose and mouth when coughing or sneezing, to dispose off tissues and contaminated items in waste receptacles immediately.Patients should cooperate and not put forth unreasonable demands.
Dental staff instructions: Front desk staff should be separated from the waiting room using transparent glass or barriers. No handshakes with the patients. Proper training to be given regarding the use and disposal of dental waste and PPE. Face mask to worn all the time.
Operatory management:The clinical team should wear gloves, mask, head cap and shoe covers at all times.Patients can remove mask at the time of oral examination and procedure (Attendee to wear mask full time).Multichair clinics without cabins should treat single patient at a time in case of aerosol procedure. Chair as well as the other contact surfaces like arm rest, light handle, tray handle etc should be wrapped in barrier film or disinfected after every patient. The barrier film should be changed after every patient. Air purifiers/ Filters to remove/filter contaminated air in treatment areas. Eg.High efficiency particulate arrestor (HEPA) filter, High volume evacuator(HVE).
HVE filter – It is a suction device which helps to remove air at a rate of up to 2.83 m3 per minute and can effectively reduce contamination caused by the operating site by 90% (Narayana et al., 2016). However, it needs to be held at a proper distance (approximately 6–15 mm) from the active ultrasonic tip and always requires a dental assistant.
HEPA filter: It is an air filtration device that can remove 99.97% of the particles measuring 0.3 μm in diameter but it may become a source of microbes if the retained microorganisms proliferate and enter back into the filtered air(Chuaybamroong et al., 2010). Negative pressure treatment room/Airborne infection isolation rooms (AIIRs): Patients with suspected or confirmed COVID-19 infection should not be treated in a routine dental practice setting. Anticipatory knowledge of health care centers with provision for AIIRs would help dentists to provide emergency dental care if the need arises (Lai et al., 2020). Keep the AC vent facing upwards.
Precautions before treating patients: Patient evaluation and Cohorting : A detailed medical history form, COVID-19 screening questionnaire and assessment of a true emergency questionnaire (Fig 7) to be filled by the patient.Measurement of patient’s body temperature using a non-contact forehead thermometer or with cameras having infrared thermal sensors (Peng et al., 2020).Decide if treatment is required or not. Prescribe medications if not treating.
Figure 6: Assessment of true emergency form
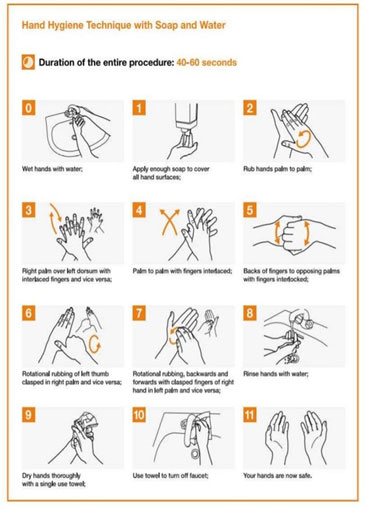
Hand hygiene:Wash hands with soap and water for at least 20 seconds or use an alcohol-based hand sanitizer with at least 60% alcohol (Fig 8) .Wash hands before and after any direct patient contact and between patients , whether or not gloves are worn, immediately after gloves are removed, before handling an invasive device, after touching blood, body fluids, secretions, excretions, non-intact skin, and contaminated items, even if gloves are worn, during patient care, when moving from a contaminated to a clean body site of the patient, after contact with inanimate objects in the immediate vicinity of the patient.
Figure 7: Hand hygiene instructions.
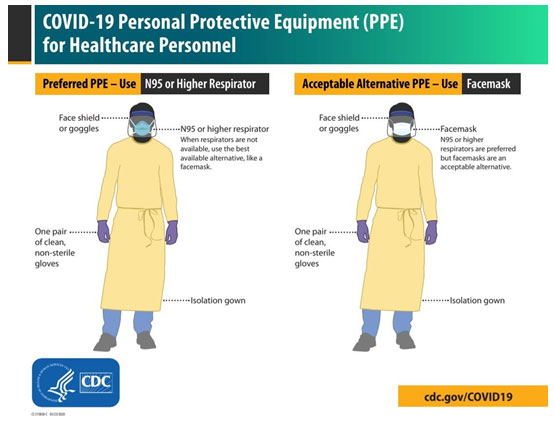
Personal Protective Equipment ( See Fig 9):Hazmat Suit – required for aerosol procedure else surgical gown or surgical apron may suffice.Head caps- surgical head caps or bouffant caps to protect hair. Disposables are preferable.Face Masks – Surgical Masks 3 or 4 ply adequate for regular checkup but N95 compulsory for aerosol procedure.Eye wear -sealed eyewear preferable like swimming goggles . In case of aerosol procedures, face shields are needed.Shoe covers – please avoid being barefoot both for doctor and patient. Shoe covers to be provided for all entering the clinic.Gloves – one pair of gloves at all times to prevent unnecessary touching of face and mouth and eyes etc., second pair during procedure. Preferably nitrile or surgical gloves when doing procedures.Proper sequence to be followed for wearing and removing the PPE.
Figure 8: Personal protective equipment
(C) Precautions while treating patients: Preprocedural mouth rinse : Patient to gargle with 0.2 % povidone iodine or 0.12% CHX for a full minute to reduce microbial load in saliva (Kariwa, Fujii and Takashima, 2006; Peng et al., 2020). Previous studies have shown that SARS and MERS were highly susceptible to povidone mouth rinse (Eggers et al., 2018).
Disposable devices: Use of disposable (single use) devices such as mouth mirror, syringes and blood pressure cuff to prevent cross-contamination.
Radiographs: Extraoral imaging such as panoramic radiograph or CBCT should be used to avoid the gag reflex or cough that may occur with intraoral imaging. When intraoral imaging is mandated, sensors should be double- barrier to prevent perforation and cross-contamination (Hokett et al., 2000).
Preferably no aerosol procedure: If required, then use: Continuous high volume suction to reduce aerosol spread. Rubber dam isolation to minimize splatter generation as it helps to shield the airway out reducing the chances of viral load in aerosols. It has been reported that the use of rubber dam could significantly reduce airborne particles in the 3-foot diameter of the operational field by 70%(Samaranayake, Reid and Evans, 1989).Anti-retraction hand pieces with specially designed anti-retraction valves or other anti-reflux designs are strongly recommended as an extra preventive measure for cross-infection(Samaranayake and Peiris, 2004). They significantly reduce the backflow of oral bacteria and virus into the tubes of the hand piece and dental unit as compared with the hand piece without anti-retraction function(Hu et al., 2007).
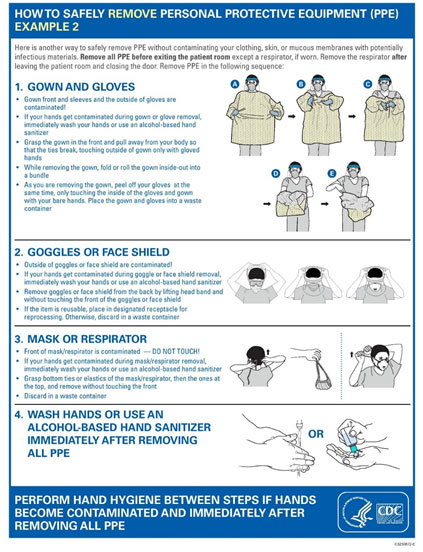
Precautions after treating patients: Disposal of PPE :One should follow the correct removal sequence of PPE (Fig 10).It is recommended to dispose off each set of PPE in individual bags.
Figure 9: Removal sequence of PPE.
Management of medical waste:The reusable instrument and items should be pretreated, cleaned, sterilized, and properly stored.The medical waste should be transported to the temporary storage area.Double-layer yellow color medical waste package bags and “gooseneck” ligation should be used for medical and domestic waste generated by the treatment of patients with suspected or confirmed 2019-nCoV infection as they are regarded as infectious medical waste, (Peng et al., 2020).
Disinfection of clinical settings:Separate shoe covers for everyone entering the operatory to prevent spread through the floor. Surface disinfection with aldehyde free solutions is recommended eg, Bacillol, Surfasept etc.Floor cleaning should be done by wet mopping with surgical floor cleaners or hypochlorite solution, use of broom is not advised. All these precautions should be followed once the dentist decides to start his/her clinical practise.
Special care for Prosthodontists
- Impressions to be washed with water and disinfected with cold sterilisation like cidex or sprays like Dimenol.
- Extreme care to be taken while transfering materials to and from the dental lab.
- Gagging should not occur while suctioning.
- Correct impression trays to be selected and adjusted for avoiding cough reflex. For highly sensitive patients, consider applying oral mucosa anesthesia to the throat before impression taking.
- During tooth preparation try to incorporate rubber dam application. For example, design supra-gingival margin for posterior bridge or use a split-dam technique (Li et al., 2004)
- During removable partial denture or complete denture try-in, avoid touching other objects in the dental office after contacting patients’ saliva.
Reopening guidelines after lockdown (Centre for disease control and prevention)
Develop your plan:Determine what needs to be cleaned (areas unoccupied for 7 or more days require only routine cleaning), how areas will be disinfected (prioritize disinfecting frequently touched surfaces) and consider resources and equipment needed (availability of cleaning products and personal protective equipment (PPE) appropriate for cleaners).
Implement: Clean visibly dirty areas with soap and water, use appropriate disinfectant product (EPA- approved disinfectant against COVID-19) and always follow the safety information and application instructions.
Maintain and Revise: Continue routine cleaning and disinfection (disinfect frequently touched surfaces at least daily), maintain safe practices (frequent hand washing, face masks and staying home if sick, maintaining social distancing)
CONCLUSION
Dentistry being highly prone to spread of infection, we as dental professionals should take utmost care and precautions while practicing it. In India, the dental council of India released a circular explaining all the preventive and precautionary measures to be taken by the dentists amid COVID-19. It also announced that all dentists should be performing only emergency procedures in support of the country’s lockdown initiated by the government of India until further notice. The emergence of COVID-19 has brought new challenges and responsibilities to dental professionals. A better understanding of aerosol transmission and its implication in dentistry can help us identify and rectify negligence in daily dental practice. In addition to the standard precautions, implementation of special precautions like patient evaluation, hand hygiene, personal protective measures, mouth rinse before dental procedures, rubber dam isolation, anti-retraction hand piece, disinfection of the clinic settings, and management of medical waste could prevent disease transmission from asymptomatic carriers. These special precautions would help control the spread of COVID-19.
Conflict of Interest: The authors declare no conflict of interest, financial or otherwise.
REFERENCES
Aslam, M.R.A., Suryawati, C. and Agushybana, F., (2020). The Importance of Prevention and Control of Coronovirus Disease (Covid-19) in Dental and Oral Hospital. Jurnal Ilmu Kesehatan Masyarakat, 11(2), pp.89-100.
Ather, A., Patel, B., Ruparel, N.B. et al,( 2020). Coronavirus disease 19 (COVID-19): implications for clinical dental care. Journal of endodontics.
Belouzard, S., Millet, J.K., Licitra, B.N. et al, (2012). Mechanisms of coronavirus cell entry mediated by the viral spike protein. Viruses, 4(6), pp.1011-1033.
Cascella, M., Rajnik, M., Cuomo, A., et al, (2020). Features, evaluation and treatment coronavirus (COVID-19). In Statpearls [internet]. StatPearls Publishing.
Chan, J.F.W., Yuan, S., Kok, K.H., et al, (2020). A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. The Lancet, 395(10223), pp.514-523.
Chartier, Y. and Pessoa-Silva, C.L., (2009). Natural ventilation for infection control in health-care settings. World Health Organization.
Chen, J., (2020). Pathogenicity and transmissibility of 2019-nCoV—a quick overview and comparison with other emerging viruses. Microbes and infection.
Chuaybamroong, P., Chotigawin, R., Supothina, et al, (2010). Efficacy of photocatalytic HEPA filter on microorganism removal. Indoor Air, 20(3), pp.246-254.
Dar Odeh, N., Babkair, H., Abu-Hammad, S. et al., (2020). COVID-19: Present and Future Challenges for Dental Practice. International Journal of Environmental Research and Public Health, 17(9), p.3151.
Eggers, M., Koburger-Janssen, T., Eickmann, M.et al, (2018). In vitro bactericidal and virucidal efficacy of povidone-iodine gargle/mouthwash against respiratory and oral tract pathogens. Infectious diseases and therapy, 7(2), pp.249-259.
Falsey, A.R. and Walsh, E.E., (2003). Novel coronavirus and severe acute respiratory syndrome. The Lancet, 361(9366), pp.1312-1313.
Fehr, A.R. and Perlman, S., (2015). Coronaviruses: an overview of their replication and pathogenesis. In Coronaviruses (pp. 1-23). Humana Press, New York, NY.
Fini, M.B., (2020). What dentists need to know about COVID-19. Oral Oncology, p.104741.
Ge, S., Yang, C.H., Hsu et al, (2007). A critical period for enhanced synaptic plasticity in newly generated neurons of the adult brain. Neuron, 54(4), pp.559-566.
Gorbalenya, A.E., Enjuanes, L., Ziebuhr, J.et al, (2006). Nidovirales: evolving the largest RNA virus genome. Virus research, 117(1), pp.17-37.
Guan, W.J., Ni, Z.Y. et al, (2020). Clinical characteristics of 2019 novel coronavirus infection in China. MedRxiv.
Guo, Z.D., Wang, Z.Y. and Zhang, S.F., (2020). Aerosol and surface distribution of severe acute respiratory syndrome coronavirus 2 in hospital wards, Wuhan, China, 2020, 26 (7). doi:10.3201/eid2607.200885.
Harrel, S. K. and Molinari, J. (2004) ‘Aerosols and splatter in dentistry: a brief review of the literature and infection control implications’, The Journal of the American Dental Association. Elsevier. Available at: https://www.sciencedirect.com/science/article/pii/S0002817714612277.
Hoffmann, M., Kleine-Weber, H., Schroeder, S. et al, (2020). SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. Elsevier, 181(2), pp. 271–280.e8.
Hokett, S.D., Honey, J.R., Ruiz, F., Baisden, M.K. and Hoen, M.M., (2000). Assessing the effectiveness of direct digital: radiography barrier sheaths and finger cots. The Journal of the American Dental Association, 131(4), pp.463-467.
Hu, T., Li, G., Zuo, Y. et al, (2007). Risk of hepatitis B virus transmission via dental handpieces and evaluation of an antisuction device for prevention of transmission. Infection Control & Hospital Epidemiology, 28(1), pp.80-82.
Jamal, M., Shah, M., Almarzooqi, S.H. et al, (2020). Overview of transnational recommendations for COVID‐19 transmission control in dental care settings. Oral Diseases. Available at: https://www.preprints.org/manuscript/202004.0357.
Kampf, G., Todt, D., Pfaender, S. et al, (2020). Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. Journal of Hospital Infection, 104(3), pp.246-251. Elsevier. Available at: https://www.sciencedirect.com/science/article/pii/S0195670120300463.
Lai C.C., Shih T.P., Ko W.C. et al, (2020). Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and corona virus disease-2019 (COVID-19): the epidemic and the challenges. International journal of antimicrobial agents, Elsevier, 55(3), p. 105924.
Li, R.W.K., Leung, K.W.C., Sun, F.C.S. et al, (2004). Severe acute respiratory syndrome (SARS) and the GDP. Part II: implications for GDPs. British dental journal, 197(3), pp.130-134.
Lu, C.W., Liu, X.F. and Jia, Z.F.,( 2020). 2019-nCoV transmission through the ocular surface must not be ignored. Lancet (London, England), 395(10224), p.e39.
Moriyama, M., Hugentobler, W.J. and Iwasaki, A., (2020). Seasonality of respiratory viral infections. Annual review of virology, 7. doi: 10.1146/annurev-virology-012420-022445.
Mukhtar, F. and Mukhtar, N., (2020). Coronavirus (COVID-19): Let’s Prevent Not Panic. Journal of Ayub Medical College Abbottabad, 32(1), pp.141-144. Available at: http://www.ayubmed.edu.pk/jamc/index.php/jamc/article/view/7564
Narayana, T.V., Mohanty, L., Sreenath, G. et al, (2016). Role of preprocedural rinse and high volume evacuator in reducing bacterial contamination in bioaerosols. Journal of oral and maxillofacial pathology: JOMFP, 20(1), p.59.
World Health Organization, (2020). Modes of transmission of virus causing COVID-19: implications for IPC precaution recommendations: scientific brief, 27 March 2020 (No. WHO/2019-nCoV/Sci_Brief/Transmission_modes/2020.1). World Health Organization.
Otter, J.A., Donskey, C., Yezli, S., et al, (2016). Transmission of SARS and MERS coronaviruses and influenza virus in healthcare settings: the possible role of dry surface contamination. Journal of Hospital Infection, 92(3), pp.235-250.
Peng X., Xu X., Li Y. et al, (2020). Transmission routes of 2019-nCoV and controls in dental practice. International Journal of Oral Science, 12(1), pp.1-6.
Perlman, S. and Netland, J., (2009). Coronaviruses post-SARS: update on replication and pathogenesis. Nature reviews microbiology, 7(6), pp.439-450.
Quadri, M.F., Jafer, M.A., Alqahtani, A.S. et al, (2020). Novel corona virus disease (COVID-19) awareness among the dental interns, dental auxiliaries and dental specialists in Saudi Arabia: A nationwide study. Journal of Infection and Public Health.
Rio del, C. and Malani, P.N., (2020) COVID-19—new insights on a rapidly changing epidemic. Jama, 323(14), pp.1339-1340.
Rothe C., Schunk M., Sothmann P. et al, (2020). Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. New England Journal of Medicine, 382(10), pp.970-971.
Samaranayake, L.P., Reid, J. and Evans, D., (1989). The efficacy of rubber dam isolation in reducing atmospheric bacterial contamination. ASDC journal of dentistry for children, 56(6), p.442-444.
Singhal, T., (2020). A review of coronavirus disease-2019 (COVID-19). The Indian Journal of Pediatrics, pp.1-6.
Spagnuolo, G., De Vito, D., Rengo, S. et al, (2020). COVID-19 outbreak: An overview on dentistry. doi: 10.3390/ijerph17062094.
To, K.K.W, Tsang OT‐Y, Leung W‐S et al,( 2020). Temporal profiles of viral load in posterior oropharyngeal saliva samples and serum antibody responses during infection by SARS‐CoV‐2: an observational cohort study. Lancet Infect Dis, 20(5), pp.565-574.
Van Doremalen, N., Bushmaker, T., Morris, et al, (2020). Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. New England Journal of Medicine.
Wu, F., Zhao, S., Yu, B. et al, (2020). A new coronavirus associated with human respiratory disease in China. Nature, 579(7798), pp.265-269.
Xu, H., Zhong, L., Deng, J. et al, (2020). High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa. International journal of oral science, 12(1), pp.1-5.
Zhou, P., Yang, X.L., Wang, X.G. et al, (2020). A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature, 579(7798), pp.270-273.