1Department of Dental Clinical Sciences, College of Dentistry, Princess Nourah Bint Abdulrahman University, Riyadh, Saudi Arabia,
2Dental Technologist, Emmendingen, Germany.
3Professor and Chair, Department of Prosthodontics, Tufts University School of Dental Medicine, Boston, United States of America.
Corresponding author email: alhanoof.dr@yahoo.com
Article Publishing History
Received: 15/12/2020
Accepted After Revision: 23/03/2021
Modern dentistry increasingly concentrates on digital procedures, including computer-aided-design and computer-aided-manufacturing (CAD/CAM) technology and the development of fixed and removable protheses based on millable materials. This case-report presents a case of a 67-year-old male having a chronic gastroesophageal reflux disease (GERD) with severe abrasion of upper anterior teeth and loss of bone in edentulous areas. Evaluating the possible modalities of treatment and the associated empirical evidence. In addition, the full mouth rehabilitation with a minimally invasive procedure using veneers on the lower anterior teeth, CAD/CAM restorations on the remaining teeth, and implant-supported fixed dental prostheses in the edentulous areas were chosen considering the patient’s factors such as tooth prognosis, wishes and economic status. Accurate diagnosis, ideal occlusal design with a 3D virtual implant planning and use of contemporary restorative materials can ensure favorable functional and esthetic rehabilitation for long-term prognosis.
Gastroesophageal Reflux Disease (GERD), Tooth Loss, Vertical Dimension of Occlusion (VDO), Cone-Beam Computer Tomography, CAD/CAM.
Aldegheishem A, Bernhard M, Att W. Computer-aided-design and Computer-aided manufacturing of full mouth restoration of a male patient with gastroesophageal reflux disease : A case Report. Biosc.Biotech.Res.Comm. 2021;14(1).
Aldegheishem A, Bernhard M, Att W. Computer-aided-design and Computer-aided manufacturing of full mouth restoration of a male patient with gastroesophageal reflux disease : A case Report. Biosc.Biotech.Res.Comm. 2021;14(1). Available from: <a href=”https://bit.ly/2ZlsiKE”>https://bit.ly/2ZlsiKE</a>
Copyright © Aldegheishem et al., This is an open access article distributed under the terms of the Creative Commons Attribution License (CC-BY) https://creativecommns.org/licenses/by/4.0/, which permits unrestricted use distribution and reproduction in any medium, provide the original author and source are credited.
INTRODUCTION
The use and application of computer-aided design and computer-aided development (CAD/CAM) technology in dentistry has increasingly expanded over the last two decades (Nassani et al., 2021). Dental CAD/CAM systems have been used to produce dental protheses that are excellently and reliably marginally and internally fit and to promote the manufacture of protheses. CAD/CAM systems use highly exacting scanners and software to digitally design the complicated forms required in dentistry. These systems have allowed digital dental treatments to be developed. Untreated tooth wear may lead to several complications such as hypersensitivity, discoloration, loss of occlusal vertical dimension, and impaired function and esthetics (Castrillion et al., 2018; Olley et al., 2017). These complications not only affect teeth and the masticatory system but also influence the quality of life. The incidence and prevalence of tooth wear are increasing and representing a growing concern in the field of dentistry (Atalay et al., 2018; Wei et al., 2016, Son et al., 2021).
One of the most common causes of tooth wear is erosion, which is defined as the loss of tooth structure due to a chemical process. Extrinsic factors such as the consumption of acidic food or drinks are mainly responsible. While intrinsic factors such as gastroesophageal reflux disease (GERD) may equally be responsible. GERD is defined as a condition when the reflux of stomach contents causes troublesome symptoms and/or complications (Van Roekel et al., 2003 Picos et al., 2018). Several factors may intensify GERD such as dietary habits, smoking, physical exercise, and obstructive sleep apnea. Therefore, adequate diagnosis and accurate monitoring are necessary (Strub et al., 2011, Castrillion et al., 2018).
The restoration of worn teeth due to erosion is complex. Various treatments using different materials and techniques to treat patients with dental wear have been described in the literature (Mesko et al., 2016; Moretto et al., 2016). However, there is no strong evidence to help clinicians choose the most appropriate therapy involving aesthetic dental treatment for smile enhancement. This case presents the treatment modalities of a patient with chronic GERD who presented with tooth wear and required full mouth rehabilitation.
Case report
Ethical approval (PNU-011/2020) was obtained from Princes Norah University, Riyadh KSA at the IRB institute and consent form was signed by the patient who was involved in this study. A 67-year old male presented to the clinic with the complaint of impaired ability to masticate and dissatisfaction with his esthetics. The patient wished for a stable, preferably fixed and esthetic prosthetic rehabilitation. His medical history revealed no significant general conditions or allergies except hypertension. The patient was reported with a diagnosis of GERD a few years ago.
The patient’s state of dental hygiene was average. Intraoral assessment of the patient exhibited inharmonic teeth forms and multiple diastemata. The upper central incisors and canines were massively short indicated severe abrasion and the vertical dimension of occlusion (VDO) was also affected (Fig. 1a). The horizontal and vertical bone loss was also diagnosed in edentulous areas. Several deficient crowns and fixed dental prostheses (FDPs) were identified as a result of poor marginal closure, as well as a deficient mandibular removable dental prosthesis (RDP) (Fig. 1b and 1c).
Figure 1: Patient’s preoperative images: (a) close-up view of the smile; (b) intra oral maxillary view with erosion and attrition; and (c) intra oral mandibular view with erosion and attrition.

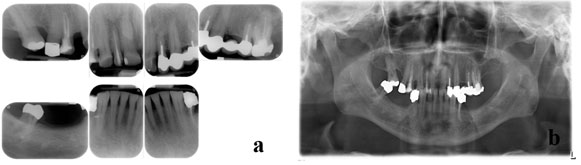
The radiographic assessment showed insufficient root canal fillings on teeth 5,7,10,13,19,21 and apicectomy on teeth 13, 14; and a transverse fracture in the cervical root part of tooth 21 and a mesiodens (Fig. 2a & 2b). he patient was diagnosed with the minor facial asymmetry toward left, multiple insufficient restorations, generalized gingivitis, multiple insufficient root fillings, horizontal root fracture on tooth 34 and compromised esthetics.
Figure 2: Patient’s radiographic analyses: (a) periapical x-rays of maxillary and mandibular teeth showing dental wear in the anterior region and insufficient restorations; and (b) panoramic x-ray showing insufficient root canal fillings on teeth 14,12,22,25,36,34, apicectomy on teeth 25, 26, a transverse fracture in the cervical root part of tooth 34 and a mesiodens.
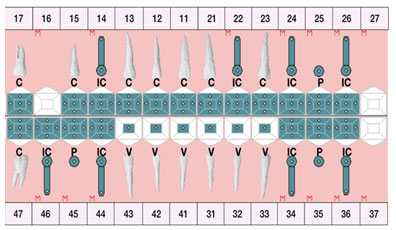
After evaluating the possible treatment modalities and the related scientific evidence, as well as considering the patient’s factors such as tooth prognosis, wishes and economic status. The full mouth rehabilitation with a minimally invasive procedure using veneers on the lower anterior teeth, CAD/CAM restorations on the remaining teeth, and implant-supported fixed dental prostheses in the edentulous areas were selected (Fig. 3).
Figure 3: Final treatment plan with a minimally invasive procedure using veneers (V) on the lower anterior teeth, CAD/CAM restorations on the remaining teeth (C), and implant-supported fixed dental prostheses in the edentulous areas (IC: implant-supported crown, P: pontic, M: Missing).
A full-arch wax-up was created to evaluate the predictability of the final esthetic and functional outcome. The wax-up was transferred into the mouth with the aid of a silicone index via a mock-up to evaluate the esthetic and phonetic parameters (Fig 4a & 4b).
Figure 4: (a) Diagnostic wax-up at proposed occlusal vertical dimension; (b) intraoral evaluation of wax-up via mock-ups.

Accordingly, CAD/CAM provisional restorations were fabricated. After removal of old restorations and extraction of hopeless teeth, teeth were prepared with care, since tooth structure is already lost due to erosion and bruxism, and provisional restorations were cemented. During this phase, two questionable teeth were given a poor prognosis due to thin dentin walls after post removal (tooth #10) and deep caries (tooth #28) and were therefore indicated for extraction. The crown of the anterior maxillary tooth (#7) was lengthened to improve the uneven gingival display. After 4-6 weeks, reevaluation of the pretreatment phase revealed a stable periodontal status with probing depths 2-3 mm and almost no bleeding on probing. The extraction sites healed successfully with no complications. The patient showed better compliance and improved oral hygiene.
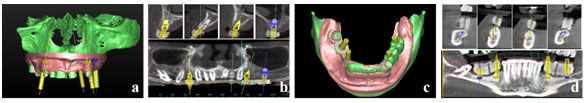
After successful pretreatment, preparations for implant placement took place. A 3D virtual implant planning was carried out based on data from cone-beam computer tomography (CBCT) using planning software Simplant®. Four implants in each of the maxilla and mandible were planned (Fig. 5a, b, c, d).
Figure 5: 3D virtual planning using planning software: (a & b) four implants in the maxilla; (c & d) four implants in mandible.
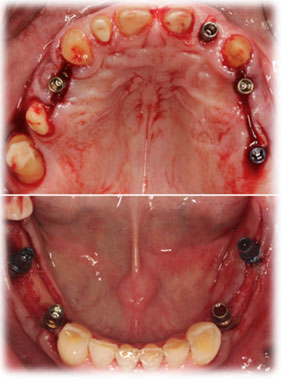
The data were uploaded to the production center, where the fabrication of the surgical guides took place. Using surgical guides, together with a guided surgery kit (Xive surgical kit GS, Dentsply Implant Manufacturing GmbH, Mannheim, Germany), the implants were placed in two separate surgical appointments (Fig. 6). Tooth 5 were placed with an internal sinus lift. Four months after placement, second-stage surgery was performed and healing abutments were fixed onto the implants.After definitive preparation of the abutment teeth, a double cord technique was used for the displacement of the gingival tissues. The implant transfer impression copings were mounted onto the implants and their position was controlled radiographically.
Figure 6: Intraoral occlusal views immediately after implant placement in the mandible and in the maxilla.
Final impressions were taken using custom trays with polyether impression material. Next, face bow transfer and jaw relation records. Next, fabrication of the individual implant abutments using computer aid design CAD (DentalDesigner™, 3shape dental system) was performed. All teeth received monolithic lithium disilicate crowns (e.max), which were adhesively cemented. Layered zirconia crowns were fabricated for the custom implant abutments, which were horizontally screwed. At the one-week follow-up, the patient was satisfied with his new restorations, and a protective night guard was delivered at that time. To improve long-term prognosis, the patient entered a 4-month recall maintenance program and had been followed for 2 years (Fig. 7).
Figure 7: Intraoral frontal view: (a) Pre-treatment and (b) Post-treatment.

DISCUSSION
Tooth wear can be divided, based on its cause into abrasion, attrition and erosion (Warreth et al., 2020). The exact type of tooth wear can be identified by a thorough medical history of the patient as well as clinical examination. However, in some cases, the synergy between the different factors causing wear may exist (Atalay et al., 2018). In this clinical case, wear was seen especially on the palatal and lingual surfaces of the anterior teeth, which indicated that the possible cause of wear in this patient had either a chemical or mechanical origin. A thorough review of the medical and dental history of the patient revealed that he suffered from severe reflux, which remained untreated until he retired. The patient showed also signs of bruxism, which was confirmed by his wife and further confirmed from the clinical examination showing stiff masticatory muscles. Therefore, it was diagnosed that the main reason for tooth wear in this patient was mechanical (bruxism) and chemical (acidic reflux).
It was essential to control all systemic and local etiological factors before starting the prosthodontic treatment. Due to the extensive tooth surface loss, restoring teeth with direct composite restorations was not an option. Moreover, severe occlusal wear was challenging in the rehabilitation of partially edentulous patients. Furthermore, to obtain the correct anatomical contour, it was important to increasing the VDO. Several studies have expressed concerns on VDO augmentation (Al-Zahrani et al., 2020; Abduo et al., 2012); however, evidence associating the procedure with pathological consequences are still lacking. In severe edentulous patients, increasing VDO assists in restorative treatment by aiding the practitioner in optimizing restorative material thickness. Recent reports indicate an increase in VDO entails no significant adverse consequence (Viana et al., 2020; Fabbri et al., 2018).
However, one has to consider with patients with TMD, where increasing the VDO should still be achieved using removable appliances to control TMD-associated symptoms before considering any form of irreversible procedure (Abduo et al., 2012). In this case, the increase of VDO was tested in the provisional stage as it is important to test the patient’s adaptability to the new position. Another important aspect linked to the clinical outcome is implanting surgical technique. In a recent meta-analysis and comparative review on conventional and computer-aided surgery, technology-assisted implant placement exhibited improved accuracy in contrast to free-hand operation (Chen et al., 2019). Another systematic review, reported lower deviation or enhanced accuracy in fully-guided implant surgery as compared to half-guided surgery (Bover-Ramos et al., 2018).
In this context, a systematic review by Schnider et al., (2009) reported that implant survival rates were 91-100% in up to 5-months observation period using computer-aided template-based surgery (Schnider et al., 2009). Computer-aided implant surgery, besides, can streamline operation and optimize implant placement (Geng et al., 2015). In regards to the digital or conventional rehabilitation, CAD/CAM prostheses were within acceptable clinical marginal discrepancy range. However, the type of material used influences the performance of the CAD/CAM system. Lithium disilicate crowns fabricated using heat press gave equivalent or smaller marginal discrepancy compared to those done on a CAD/CAM platform. Crowns produced by slip-casting showed similar or, even, improved marginal accuracy than CAD/CAM fabrications.
Recently, in terms of marginal fit, Freire et al., (2019) described the marginal fit of CAD/CAM monolithic and metal-ceramic crowns were within the acceptable clinical range. Monolithic lithium disilicate restoration (IPS e.max CAD) possessed the lowest discrepancy value compared to monolithic zirconia and metal-ceramic crowns.For the edentulous regions in the mandible, implants with a length of <10mm were inserted due to the vertical loss of alveolar bone. In 2011, the survival rate of short dental implants was evaluated through a systematic review. Several factors such as smoking, implant location, surface characteristics of implants and the influence of bone augmentation were investigated. All factors showed no statistically significant difference in terms of implant survival rate except for smoking and implant location.
In another recent study investigating the relationship between tooth wear, GERD and bruxism, it was confirmed that severe tooth wear was highly related with patients with sleep bruxism (Li et al., 2018). Considering the relationship between GERD and bruxism, tooth wear in patients with sleep bruxism may be a consequence of attrition intensified by intrinsic acids rather than attrition alone, which was exactly the situation in the present case. This finding supports and advances the understanding that tooth wear is a multifarious condition involving multiple mechanisms. To ensure long-term outcomes of the restorations especially that the patient was examined with bruxism, a night guard was fabricated.
CONCLUSION
In conclusion, this case report describes the complete oral recovery of a GERD patient. The patient was successfully treated with traditional all-ceramic and implant-supported restorations to fulfill the patient’s needs and desires for fixed dental prostheses. An individualized maintenance program was placed in place to ensure a favorable long-term prognosis for the patient.
ACKNOWLEDGEMENTS
This research was funded by the Deanship of Scientific Research at Princess Nourah bint Abdulrahman University, Riyadh KSA, through the Fast-track Research Funding Program.
REFERENCES
Abduo, J., Lyons, K. (2012). Clinical considerations for increasing occlusal vertical dimension: a review. Aust Dent J, 57 (1):2–10.
Al-Zahrani, M. S., Alhassani, A, A., & Zawawi, K, H. (2020). Tooth loss as a potential risk factor for deficient sleep: an analysis of a nationally representative sample of adults in the USA. Sleep and Breathing, 1-7.
Atalay, C., Ozgunaltay, G. (2018). Evaluation of tooth wear and associated risk factors: a matched case-control study. Nigerian journal of clinical practice, 21(12):1607–1614.
Bover-Ramos, F., Vina-Almunia, J., Cervera-Ballester, J., Penarrocha-Diago, M., Garcia-Mira, B. (2018). Accuracy of implant placement with computer-guided surgery: a systematic review and meta-analysis comparing cadaver, clinical, and in vitro studies. Int J Oral Maxillofac Implants, 33(1):101–115.
Castrillon, E, E., Exposto, F, G. (2018). Sleep bruxism and pain. Dental clinics of North America, 62(4):657–663.
Chen, S., Ou, Q., Lin, X., Wang, Y. (2019). Comparison between a computer-aided surgical template and the free-hand method: a systematic review and meta-analysis. Implant Dent, 28(6):578–589.
Fabbri, G., Sorrentino, R., Cannistraro, G., Mintrone, F., Bacherini, L., Turrini, R., et al. (2018). Increasing the vertical dimension of occlusion: a multicenter retrospective clinical comparative study on 100 patients with fixed tooth-supported, mixed, and implant-supported full-arch rehabilitations. Int J Periodontics Restorative Dent, 38(3):323–335.
Freire, Y., Gonzalo, E., Lopez-Suarez, C., Suarez, M, J. (2019). The marginal fit of CAD/CAM monolithic ceramic and metal-ceramic crowns. J Prosthodont, 28(3):299–304.
Geng, W., Liu, C., Su, Y., Li, J., Zhou, Y. (2015). Accuracy of different types of computer-aided design/computer-aided manufacturing surgical guides for dental implant placement. Int J Clin Exp Med, 8(6):8442–8449.
Li, Y., Yu, F., Niu, L., Hu, W., Long, Y., Tay, F, R., et al. (2018). Associations among bruxism, gastroesophageal reflux disease, and tooth wear. Journal of clinical medicine, 7(11):417.
Mesko, M, E., Sarkis-Onofre, R., Cenci, M, S., Opdam, N, J., Loomans, B., Pereira-Cenci, T. (2016). Rehabilitation of severely worn teeth: a systematic review. Journal of dentistry, 48:9–15.
Moretto, G., Pupo, Y, M., Bueno, A, L., Araujo, F, O. (2016). Prosthetic rehabilitation of a patient with gastroesophageal reflux disease: five-year follow-up. Operative dentistry, 41(2):132–137.
Nassani, M, Z., Ibraheem, S., Shamsy, E., Darwish, M., Faden, A. & Kujan, O. (2021). A Survey of Dentists’ Perception of Chair-Side CAD/CAM Technology. Healthcare, Multidisciplinary Digital Publishing Institute, 68(9): 1-9.
Olley, R, C., Sehmi, H. (2017). The rise of dentine hypersensitivity and tooth wear in an ageing population. British dental journal, 223(4):293–297.
Picos, A., Badea, M, E., Dumitrascu, D, L. (2018). Dental erosion in gastro-esophageal reflux disease. A systematic review. Clujul medical (1957), 91(4):387–390.
Schneider, D., Marquardt, P., Zwahlen, M., Jung, R, E. (2009). A systematic review on the accuracy and the clinical outcome of computer-guided template-based implant dentistry. Clin Oral Implants Res, 20(4):73–86.
Son, K. & Lee, B, K. (2021). Marginal and Internal Fit of Ceramic Prostheses Fabricated from Different Chairside CAD/CAM Systems: An In Vitro Study. Applied Sciences, 11, 857.
Strub, J, R., Kern, M., Turp, J, C., Witkowski, S., Heydecke, G., Wolfart, S. (2011). Curriculum Prosthetik. Berlin: Quentissenze GmbH Verlag; 20(11):1-3.
Van Roekel, N, B. (2003). Gastroesophageal reflux disease, tooth erosion, and prosthodontic rehabilitation: a clinical report. Journal of prosthodontics: official journal of the American College of Prosthodontists, 12(4):255–259.
Viana, M, M., Do Amaral, S, F., Nakao, E., & Rodrigues, M, C. (2020). Conservative approach to the restoration of vital teeth affected by severe tissue wear. The Journal of prosthetic dentistry, 123, 191-195.
Warreth, A., Abuhijleh, E., Almaghribi, M. A., Mahwal, G. & Ashawish, A. (2020). Tooth surface loss: A review of literature. The Saudi Dental Journal, 32, 53-60.
Wei, Z., Du, Y., Zhang, J., Tai, B., Du, M., Jiang, H. (2016). Prevalence and indicators of tooth wear among Chinese adults. PloS one, 11 (9):e0162181.


