Department of Community Health Sciences, College of Applied Medical Sciences, King Saud University, Riyadh, Saudi Arabia.
Corresponding author email: nalafeef@ksu.edu.sa
Article Publishing History
Received: 10/07/2020
Accepted After Revision: 25/09/2020
Sleep is a physiological process that fulfils an important homeostatic function. Short sleep duration (SSD) is defined as sleep that is substantially shorter than the optimal duration of 8-hours for adolescents and adults (18 years and above), and 9-hours for children (3-17 years). Insufficient sleep is associated with adverse health outcomes such as obesity, type 2 diabetes, stroke, hypertension, coronary heart disease, and other chronic kidney diseases. Globally, 30% of the children with obesity have been reported to experience sleep disorders. The present review has been aimed to describe the association between SSD and weight gain during childhood using a sample of school-going children (5–17 years). Specifically, based on a systematic meta-analysis of original research articles, it aimed to assess the impact of SSD on school-going children. Findings showed that SSD is a risk factor for children aged 5–17 years who experience insufficient sleep (< 9 hours/day). Epidemiological studies such as case-control, observational, follow-up, and meta-analysis studies confirm SSD as a risk factor for the development of obesity and other diseases through various mechanisms. Thus, based on numerous studies on SSD in children, it is confirmed as a risk factor for childhood obesity. It is therefore recommended to prevent SSD to avoid future complications.
Short Sleep Duration, Obesity, Risk-Factors, Childhood Obesity
Alafif N. Association Between Short Sleep Duration and Childhood Obesity in School-Going Children: A Mini Review. Biosc.Biotech.Res.Comm. 2020;13(3).
Alafif N. Association Between Short Sleep Duration and Childhood Obesity in School-Going Children: A Mini Review. Biosc.Biotech.Res.Comm. 2020;13(3). Available from: https://bit.ly/3knof99
Copyright © Alafif This is an open access article distributed under the terms of the Creative Commons Attribution License (CC-BY) https://creativecommons.org/licenses/by/4.0/, which permits unrestricted use distribution and reproduction in any medium, provide the original author and source are credited.
INTRODUCTION
Sleep is defined as the resting state of expected insentience from which any individual can be aroused, (Ezenwanne and research, 2011). It is a multi-faceted and vital physiological mechanism that is assessed using regular sleep logs, actigraphy, and polysomnography. In children, insufficient sleep has been documented to have deleterious effects on health, and sleep duration has been found to be associated with non-communicable diseases (Brazendale et al., 2019). Sleep is considered as food for the brain, as important brain functions occur during sleep, therefore, skipping sleep can be harmful and deadly as well, (Roberts et al., 2020).
The present review has been aimed to describe the association between SSD and weight gain during childhood using a sample of school-going children (5–17 years). Specifically, based on a systematic meta-analysis of original research articles, it aimed to assess the impact of SSD on school-going children. Findings showed that SSD is a risk factor for children aged 5–17 years who experience insufficient sleep (< 9 hours/day). Epidemiological studies such as case-control, observational, follow-up, and meta-analysis studies confirm SSD as a risk factor for the development of obesity and other diseases through various mechanisms. Thus, based on numerous studies on SSD in children, it is confirmed as a risk factor for childhood obesity. It is therefore recommended to prevent SSD to avoid future complications. Sufficient sleep duration contributes to the regulation of hormonal and metabolic processes in children (0–17 Years) (Miller et al., 2015).
According to the National Sleep Foundation (NSF) in the US, the minimum required sleep duration is 14-17 hours for new-borns (aged 0-3 months), 12-15 hours for infants (aged 4-11 months), 11-14 hours for toddlers (aged 1-2 years), 10-13 hours for preschool children (aged 3-5 years), 9-11 hours for school-aged children (aged 6-13 years), 8-10 hours for adolescents (aged 14-17 years), 7-9 hours for young and middle adults (aged 18-25 years and 26-64 years, respectively), and 7-8 hours for older adults (aged over ≥ 65 years) (Foundation, 2019).
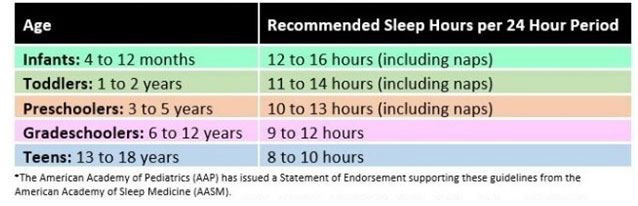
Similar recommendations have been adopted in Canada (Chaput et al., 2016). Similarly, the American Academy of Sleep Medicine (AASM) and Sleep Research Society recommend that adults require 7–9 hours of sleep (Watson et al., 2015, Hirshkowitz et al., 2015, Tobaldini et al., 2019). The sleep requirements for children recommended by AASM have been presented in Figure 1. Short sleep duration (SSD) is defined as a total sleep duration of less than 6 hours/day. It is often identified using polysomnography on a single night. Inadequate sleep is defined as sleep duration that is lesser than age-based recommendations, and it is commonly present in school-going children, (Tambalis et al., 2018).
Figure 1: Showing suggested amount of sleep for pediatric population
Specifically, in children aged 5–16 years, the pressure of extra-curricular activities, disturbances from electronics, noisy environment, and home-work or academic tasks are considered as risk factors for SSD (Glaser and Styne, 2017). In the US, the mean sleep duration for children was 7.1 hours, with 29.2% children sleeping for less than 6 hours. The corresponding figures from Canada and the UK were 11.3% and 9.8% (Itani et al., 2017). The underlying cause of SSD could be sleep disorders, which is a large group of diseases with a nominal incidence in the general population. Insomnia, a well-documented and common sleep problem, is defined as a sleep disorder that is characterized by complications in sustaining sleep. Further, it is associated with impaired daytime functioning. Insufficient sleep often develops into more serious health issues such as insomnia and other sleep disorders. Additionally, SSD is associated with increased incidence of cardiovascular diseases (CVD), hypertension (HTN), and arrhythmias (Tobaldini et al., 2019).
Sleep duration has been found to be associated with innumerable health issues such as chronic diabetes, kidney problems, CVD, and obesity (Rosinger et al., 2018). On the other hand, obesity predicts health issues such as diabetes, CVD, early mortality, HTN, and lower quality of life (Buxton et al., 2010). Previous systematic reviews have confirmed that SSD is associated with major health issues such as mortality, HTN, CVD, stroke, diabetes, obesity, metabolic abnormalities, and atherosclerosis (Gallicchio and Kalesan, 2009, Wu et al., 2014, Leng et al., 2015, Itani et al., 2017). Grandner et al (Grandner et al., 2010) defined SSD as sleep duration of < 6 hours or 1/4th of the day of sleep deficiency. SSD is associated with medical complications at a later age.
Further, overweight in young children is associated with obesity-related conditions such as asthma, HTN, hyperlipidaemia, type 2 diabetes mellitus (T2DM), and higher morbidity and mortality in adulthood, (Taveras et al., 2008). SSD may also lead to psychiatric disorders and cardiometabolic risk factors such as poor glucose homeostasis and dyslipidaemia (Lombardero et al., 2019). Poor sleep in children (aged 0–17 years) puts them at a higher risk for weight gain, which could lead to overweight or obesity. In this context, a meta-analysis of epidemiological and cohort data revealed an unintentional relationship between SSD and health issues (Jike et al., 2018).
Inadequate sleep and childhood obesity: The term overweight and obesity are defined as accumulation of additional fat in the body (Organization, 2019). Obesity is identified using a screening tool known as Body Mass Index (BMI), which is calculated as weight in kilograms divided by the square of height in meters (Khan et al., 2019). A BMI of 30kg/m2 is considered as obesity, that of 25.0 kg/m2–29.9 kg/m2 is considered as overweight, and that of 35 kg/m2–40 kg/m2 or higher is considered as morbid obesity (Khan et al., 2014). Weight gain in children is connected with short and long-term adverse outcomes. In children, the occurrence of childhood obesity has increased due to an increase in the prevalence of SSD (Ash and Taveras, 2017).
Presence of excess body fat in children is known as childhood obesity. Among the common health issues that have been observed in the 21st century, childhood obesity is defined as proning the disease since 2016, with more than 124 million children aged 5–19 years being identified as obese and 213 million children being identified as overweight. Childhood obesity is connected with psychological problems; lower educational attainment; and harmful co-morbidities later in life, such as dyslipidaemia, T2DM, non-alcoholic fatty liver disease (NAFLD), CHD, and HTN (Spinelli et al., 2019). Further, musculoskeletal disorders are one of the undocumented complications associated with obesity and SSD (Al Shehri et al., 2013). Childhood obesity and severe obesity put individuals at risk of CVD, obstructive sleep apnoea, impaired glucose tolerance, increased exposure to bullying, and NAFLD (Carsley et al., 2019).
Globally, childhood obesity has become a major health concern. The increase in childhood obesity has been linked to the simultaneous increase in the tendency to experience the metabolic syndrome (MetS). The future complications of obesity are T2DM, HTN, dyslipidaemia, and MetS. However, cardiometabolic risk factors are considered to be modifiable. Sleep plays a major role in the growth and development of children through its control of the diurnal rhythm that is connected with energy homeostasis, (Seo and Shim, 2019).
The incidence of childhood obesity has tripled in the past decades, leading it to be recognized as a global health threat. It is associated with numerous adverse outcomes such as poor academic performance, psychological conditions, cardiovascular disease, and permanent obesity. The common causes of childhood obesity are sedentary lifestyle with high-calorie eating habits (uncontrolled diet) (Li et al., 2017b). Further, preceding epidemiological studies have confirmed that the increase in the prevalence of obesity is associated with the decrease in sleep duration in children (Kelishadi, 2007, Li et al., 2011). Some previous studies have also documented that SSD during childhood is connected with cardiometabolic risk factors (Chaput et al., 2006, Li et al., 2017a, Touchette et al., 2008). Recently, the global prevalence rate of childhood obesity was estimated to be 6.7%, and it is expected to reach 9.1% by 2020 (Bin-Hasan et al., 2018).
Afshin et al (Afshin et al., 2017) reported that 107.7 million children were obese, with a global prevalence of 5%. The Canadian national government prioritized the implementation of efforts for prevent and manage weight gain (obesity) in children (Carsley et al., 2019). Countries in the Gulf Cooperation Council (GCC) have documented the highest prevalence of T2DM and obesity, and surveillance of childhood obesity is considered central to tackling this obesity epidemic (Al Hammadi and Reilly, 2019).
Statistically, the age-based BMI classification for children defines overweight as the 85th–95th percentile, and obesity as the 95th percentile or above (Sahoo et al., 2015). Based on criteria recommended by the World Health Organization, obesity is defining according to BMI for specific age groups, with a Z-score of >2 defined as overweight and that of >3 defined as obesity. In a multicentric study, children with a BMI of >30 kg/m2 were classified as obese and those with a BMI of > 25kg/m2 were classified as overweight. However, waist circumference was not measured as an indicator of overweight and obesity in children (aged 3–14 years) and adolescents (aged 15–18 years). The prevalence of obesity is considered to be a result of the interaction between genetic, psychological, cultural, socioeconomic, and environmental factors. In previous studies, sleep duration was assessed using self-reported or objective measurements (e.g. actigraph or polysomnography) (Reutrakul et al., 2018).
According to the National Growth Study, the occurrence rate of obesity was 11.3% in school-going children aged 5-18 years. Further, it was 11% in female and 7.8% in male students aged 5-12 years, and 13.8% and 12.1%, among students aged 13-18 years, respectively. Therefore, females were found to be more prone to obesity as compared to males (Al Dhaifallah et al., 2015).
Obesity in school children: Female students aged 5–18 years are more prone to weight gain and obesity as compared to their male counterparts owing to inherent hormonal differences. Consumption of fatty food, inconsistent exercise habits, and inactive lifestyle are the major reasons for obesity; however, apart from these factors, age, gender, family history, and parental lifestyle also lead to obesity (Birch and Fisher, 1998). Lee et al (Lee et al., 2000) confirmed that obesity is linked with socio-economic status, which is further connected with salary, occupation, and educational accomplishment. Among environmental factors, viewing television while consuming food was found to lead to obesogenic eating behaviour and further gain in body weight (Boswell et al., 2019). Polycystic ovarian syndrome (PCOS) was another factor linked with weight gain in female school-going children aged 12–16 years. The relationship between PCOS and obesity is linked to the high production of insulin, leading to irregular and impaired blood glucose level management (Bremer and disorders, 2010, Koivuaho et al., 2019, Witchel et al., 2019).
Apart from this, having a playground in school has also been found to play a critical role in weight management, specifically in female children. Katare et al (Katare et al., 2019) confirmed that BMI is strongly influenced by environmental factors. Another previous study indicated that the consumption of sugary beverages; snacks with a high salt content; lower activity level; family history; and psychological factors such as anxiety, depression, dissatisfaction with one’s body, eating disorders, and emotions lead to childhood obesity, specifically in school-going girls (Sahoo et al., 2015). Excess usage of electronic devices such as watching television for several hours and sedentary lifestyle have been found to contribute to obesity (Tuohino et al., 2019). However, until now, there is no clear strategy for the treatment of obesity [Table 1] (Cuda and Censani, 2018). It is important to note that clinicians and nutritionists can convert obesity from an irreversible to a reversible disease by developing and implementing appropriate guidelines.
Table 1. Diagnosing the BMI based on age factor (Reference: (Cuda and Censani, 2018))
| Infancy
(0-24 Months) |
Toddler
(2-4 Years) |
Early childhood
(5-9 Years) |
Puberty
(10-14 Years) |
Adolescent
(15-18 Years) |
Adult
(≥19 Years)
|
| Weight > Length | BMI ≥ 95th Percentile or ≥85th percentile with couple or more risk factors | BMI ≥ 95th Percentile or ≥85th percentile with couple or more risk factors | BMI ≥ 95th Percentile or ≥85th percentile with couple or more risk factors | BMI ≥ 95th Percentile or ≥85th percentile with couple or more risk factors | BMI ≥ 95th Percentile or ≥85th percentile with couple or more risk factors |
| · Fasting Blood Glucose/ HgA1c
· Fasting Lipid Profile /Random Blood Sugar · ALT, AST and GGT · Consider 25 OH Vitamin D |
· Consider sleep study
· Consider liver ultrasound · Consider uric acid · Consider fasting serum insulin |
|
|
Association between SSD and childhood obesity: Globally, a limited number of systematic reviews and meta-analyses have explored the link between SSD and childhood obesity. According to Li et al. (Li et al., 2017b), though several epidemiological and meta-analysis studies have been conducted to examine this relationship, most studies were based on cross-sectional observations. Patel et al (Patel et al., 2006) cconfirmed the strong association in women because participants whose sleep duration was between < 5–7 hours/day had gained a significant amount of weight. Cappuccio et al (Cappuccio et al., 2008) conducted a meta-analysis on a global population of children (n = 30,002) and adults (n = 6,04,509) with SSD. They reported a consistent increased risk of obesity among children and adults with SSD.
However, in their study on infants, Alamian et al (Alamian et al., 2016) reported a negative association between sleep problems and childhood obesity. In their meta-analysis on SSD and childhood obesity, Chen et al (Chen et al., 2008) reported a significant inverse association between these two variables. Hart et al (Hart et al., 2011) also confirmed that SSD is associated with weight gain, which in turn tends to lead to obesity. Matricciani et al (Matricciani et al., 2012) examined data collected on 0.7 million children over the past 100 years, from 20 different countries. They confirmed that children’s sleep duration was a minimum of 20–25 minutes lower than that of their parents when the latter were of their age. At night, the average sleep duration of school-age and preschool children was 9.4 and 9.6 hours/day, respectively, and that of toddlers and infants was 9.8 and 9.0 hours/day, respectively (2004., 2004). Ash and Taveras, (2017) have confirmed that insufficient sleep is associated with numerous adverse health outcomes in children.
Miller et als (Miller et al., 2018) systemic review and meta-analysis confirmed that SSD is a risk factor for the development of obesity in infants, children, and adolescents. These findings were confirmed and corroborated by similar prior studies (Li et al., 2017b, Marin-Oto et al., 2019, Spinelli et al., 2019, Taveras et al., 2008, Wu et al., 2017, Zhang et al., 2019).
Recommendation: This review article recommends that school-aged children (aged 5–17 years) should receive a minimum of 9–12 hours of sleep per day to avoid future health complications, mainly weight gain, which may in turn lead to childhood obesity.
CONCLUSION
Sleep deprivation is associated with multiple hormonal responses which lead to appetite dysregulation, and negative effects on hunger and satiety, which in turn lead to low leptin and high ghrelin levels. The present review identified sleep as an important modifiable risk factor for obesity in infants, children, adolescents, and adults. Based on numerous studies, SSD is confirmed as a risk factor for obesity in infants, and children. Therefore, this review recommends the prevention of SSD to avoid future health complications.
REFERENCES
Afshin, A., Forouzanfar, M. H., Reitsma, M. B., Sur, P., Patton, G. C., Et Al. 2017. Health Effects Of Overweight And Obesity In 195 Countries Over 25 Years. N Engl J Med, 377, 13-27.
Al Dhaifallah, A., Mwanri, L. & Aljoudi, A. J. S. J. O. O. 2015. Childhood Obesity In Saudi Arabia: Opportunities And Challenges. 3, 2.
Al Hammadi, H. & Reilly, J. J. B. O. 2019. Prevalence Of Obesity Among School-Age Children And Adolescents In The Gulf Cooperation Council (Gcc) States: A Systematic Review. 6, 3.
Al Shehri, A., Al Fattani, A. & Al Alwan, I. J. S. J. O. O. 2013. Obesity Among Saudi Children. 1, 3.
Alamian, A., Wang, L., Hall, A. M., Pitts, M. & Ikekwere, J. J. P. M. R. 2016. Infant Sleep Problems And Childhood Overweight: Effects Of Three Definitions Of Sleep Problems. 4, 463-468.
Ash, T. & Taveras, E. M. J. S. H. 2017. Associations Of Short Sleep Duration With Childhood Obesity And Weight Gain: Summary Of A Presentation To The National Academy Of Science’s Roundtable On Obesity Solutions. 3, 389-392.
Bin-Hasan, S., Katz, S., Nugent, Z., Nehme, J., Lu, Z., Khayat, A., Al-Saleh, S., Amin, R., Narang, I. J. S. & Breathing 2018. Prevalence Of Obstructive Sleep Apnea Among Obese Toddlers And Preschool Children. 22, 511-515.
Birch, L. L. & Fisher, J. O. J. P. 1998. Development Of Eating Behaviors Among Children And Adolescents. 101, 539-549.
Boswell, N., Byrne, R. & Davies, P. S. J. B. O. 2019. Family Food Environment Factors Associated With Obesity Outcomes In Early Childhood. 6, 17.
Brazendale, K., Beets, M. W., Weaver, R. G., Perry, M. W., Tyler, E. B., Hunt, E. T., Decker, L. & Chaput, J.-P. J. S. M. 2019. Comparing Measures Of Free-Living Sleep In School-Aged Children.
Bremer, A. A. J. M. S. & Disorders, R. 2010. Polycystic Ovary Syndrome In The Pediatric Population. 8, 375-394.
Buxton, O. M., Marcelli, E. J. S. S. & Medicine 2010. Short And Long Sleep Are Positively Associated With Obesity, Diabetes, Hypertension, And Cardiovascular Disease Among Adults In The United States. 71, 1027-1036.
Cappuccio, F. P., Taggart, F. M., Kandala, N.-B., Currie, A., Peile, E., Stranges, S. & Miller, M. A. J. S. 2008. Meta-Analysis Of Short Sleep Duration And Obesity In Children And Adults. 31, 619-626.
Carsley, S., Pope, E. I., Anderson, L. N., Tremblay, M. S., Tu, K. & Birken, C. S. J. C. O. 2019. Temporal Trends In Severe Obesity Prevalence In Children And Youth From Primary Care Electronic Medical Records In Ontario: A Repeated Cross-Sectional Study. 7, E351.
Chaput, J.-P., Dutil, C. J. I. J. O. B. N. & Activity, P. 2016. Lack Of Sleep As A Contributor To Obesity In Adolescents: Impacts On Eating And Activity Behaviors. 13, 103.
Chaput, J., Brunet, M. & Tremblay, A. J. I. J. O. O. 2006. Relationship Between Short Sleeping Hours And Childhood Overweight/Obesity: Results From The ‘Quebec En Forme’project. 30, 1080.
Chen, X., Beydoun, M. A. & Wang, Y. J. O. 2008. Is Sleep Duration Associated With Childhood Obesity? A Systematic Review And Meta‐Analysis. 16, 265-274.
Cuda, S. E. & Censani, M. J. F. I. P. 2018. Pediatric Obesity Algorithm: A Practical Approach To Obesity Diagnosis And Management. 6.
Ezenwanne, E. J. A. O. M. & Research, H. S. 2011. Current Concepts In The Neurophysiologic Basis Of Sleep; A Review. 1, 173-180.
Foundation, N. S. 2019. Https://Www.Sleepfoundation.Org/.
Gallicchio, L. & Kalesan, B. J. J. O. S. R. 2009. Sleep Duration And Mortality: A Systematic Review And Meta‐Analysis. 18, 148-158.
Glaser, N. & Styne, D. J. P. 2017. Weighing The Causal Evidence That Associates Short Sleep Duration With Obesity. 140, E20172015.
Grandner, M. A., Patel, N. P., Gehrman, P. R., Perlis, M. L. & Pack, A. I. J. S. M. R. 2010. Problems Associated With Short Sleep: Bridging The Gap Between Laboratory And Epidemiological Studies. 14, 239-247.
Hart, C. N., Cairns, A. & Jelalian, E. 2011. Sleep And Obesity In Children And Adolescents. Pediatr Clin North Am, 58, 715-33.
Hirshkowitz, M., Whiton, K., Albert, S. M., Alessi, C., Bruni, O., Doncarlos, L., Hazen, N., Herman, J., Adams Hillard, P. J., Katz, E. S., Kheirandish-Gozal, L., Neubauer, D. N., O’donnell, A. E., Ohayon, M., Peever, J., Rawding, R., Sachdeva, R. C., Setters, B., Vitiello, M. V. & Ware, J. C. 2015. National Sleep Foundation’s Updated Sleep Duration Recommendations: Final Report. Sleep Health, 1, 233-243.
Itani, O., Jike, M., Watanabe, N. & Kaneita, Y. J. S. M. 2017. Short Sleep Duration And Health Outcomes: A Systematic Review, Meta-Analysis, And Meta-Regression. 32, 246-256.
Jike, M., Itani, O., Watanabe, N., Buysse, D. J. & Kaneita, Y. 2018. Long Sleep Duration And Health Outcomes: A Systematic Review, Meta-Analysis And Meta-Regression. Sleep Med Rev, 39, 25-36.
Katare, B., Chakrovorty, S. J. J. O. H., Population & Nutrition 2019. Association Between Environmental Factors And Bmi: Evidence From Recent Immigrants From Developing Countries. 38, 15.
Kelishadi, R. J. E. R. 2007. Childhood Overweight, Obesity, And The Metabolic Syndrome In Developing Countries. 29, 62-76.
Khan, I. A., Jahan, P., Hasan, Q. & Rao, P. 2019. Genetic Confirmation Of T2dm Meta-Analysis Variants Studied In Gestational Diabetes Mellitus In An Indian Population. Diabetes Metab Syndr, 13, 688-694.
Khan, I. A., Jahan, P., Hasan, Q. & Rao, P. J. J. O. T. R.-A.-A. S. 2014. Angiotensin-Converting Enzyme Gene Insertion/Deletion Polymorphism Studies In Asian Indian Pregnant Women Biochemically Identifies Gestational Diabetes Mellitus. 15, 566-571.
Koivuaho, E., Laru, J., Ojaniemi, M., Puukka, K., Kettunen, J., Tapanainen, J., Franks, S., Järvelin, M.-R., Morin-Papunen, L. & Sebert, S. J. I. J. O. O. 2019. Age At Adiposity Rebound In Childhood Is Associated With Pcos Diagnosis And Obesity In Adulthood—Longitudinal Analysis Of Bmi Data From Birth To Age 46 In Cases Of Pcos. 1.
Lee, A., Cardel, M. & Donahoo, W. T. 2000. Social And Environmental Factors Influencing Obesity. In: Feingold, K. R., Anawalt, B., Boyce, A., Chrousos, G., Dungan, K., Grossman, A., Hershman, J. M., Kaltsas, G., Koch, C., Kopp, P., Korbonits, M., Mclachlan, R., Morley, J. E., New, M., Perreault, L., Purnell, J., Rebar, R., Singer, F., Trence, D. L., Vinik, A. & Wilson, D. P. (Eds.) Endotext. South Dartmouth (Ma): Mdtext.Com, Inc.
Leng, Y., Cappuccio, F. P., Wainwright, N. W., Surtees, P. G., Luben, R., Brayne, C. & Khaw, K.-T. J. N. 2015. Sleep Duration And Risk Of Fatal And Nonfatal Stroke: A Prospective Study And Meta-Analysis. 84, 1072-1079.
Li, L., Fu, J., Yu, X. T., Li, G., Xu, L., Yin, J., Cheng, H., Hou, D., Zhao, X. & Gao, S. J. S. 2017a. Sleep Duration And Cardiometabolic Risk Among Chinese School-Aged Children: Do Adipokines Play A Mediating Role? 40, Zsx042.
Li, L., Pinot De Moira, A. & Power, C. J. T. A. J. O. C. N. 2011. Predicting Cardiovascular Disease Risk Factors In Midadulthood From Childhood Body Mass Index: Utility Of Different Cutoffs For Childhood Body Mass Index. 93, 1204-1211.
Li, L., Zhang, S., Huang, Y., Chen, K. J. J. O. P. & Health, C. 2017b. Sleep Duration And Obesity In Children: A Systematic Review And Meta‐Analysis Of Prospective Cohort Studies. 53, 378-385.
Lombardero, A., Hansen, C. D., Richie, A. E., Campbell, D. G., Joyce, A. W. J. J. O. E. & Health, P. 2019. A Narrative Review Of The Literature On Insufficient Sleep, Insomnia, And Health Correlates In American Indian/Alaska Native Populations. 2019.
Marin-Oto, M., Vicente, E. E. & Marin, J. M. J. M. R. M. 2019. Long Term Management Of Obstructive Sleep Apnea And Its Comorbidities. 14, 21.
Matricciani, L., Olds, T. & Petkov, J. J. S. M. R. 2012. In Search Of Lost Sleep: Secular Trends In The Sleep Time Of School-Aged Children And Adolescents. 16, 203-211.
Miller, A. L., Lumeng, J. C., Lebourgeois, M. K. J. C. O. I. E., Diabetes, & Obesity 2015. Sleep Patterns And Obesity In Childhood. 22, 41.
Miller, M. A., Kruisbrink, M., Wallace, J., Ji, C. & Cappuccio, F. P. J. S. 2018. Sleep Duration And Incidence Of Obesity In Infants, Children, And Adolescents: A Systematic Review And Meta-Analysis Of Prospective Studies. 41, Zsy018.
N.S.F.S.I.A.P.2004.[December 11, 2015]. June 27, 2017. Available At: Https://Sleepfoundation.Org/Sites/Default/Files/Finalsof2004.Pdf.
Organization, W. H. 2019. Global Action Plan On Physical Activity 2018-2030: More Active People For A Healthier World, World Health Organization.
Patel, S. R., Malhotra, A., White, D. P., Gottlieb, D. J. & Hu, F. B. J. A. J. O. E. 2006. Association Between Reduced Sleep And Weight Gain In Women. 164, 947-954.
Reutrakul, S., Anothaisintawee, T., Herring, S. J., Balserak, B. I., Marc, I. & Thakkinstian, A. J. S. M. R. 2018. Short Sleep Duration And Hyperglycemia In Pregnancy: Aggregate And Individual Patient Data Meta-Analysis. 40, 31-42.
Roberts, C., Al Sayegh, R., Ellison, P. R., Sedeek, K. & Carr, M. M. 2020. How Pediatric Anesthesiologists Manage Children With Osa Undergoing Tonsillectomy. Ann Otol Rhinol Laryngol, 129, 55-62.
Rosinger, A. Y., Chang, A.-M., Buxton, O. M., Li, J., Wu, S. & Gao, X. J. S. 2018. Short Sleep Duration Is Associated With Inadequate Hydration: Cross-Cultural Evidence From Us And Chinese Adults. 42, Zsy210.
Sahoo, K., Sahoo, B., Choudhury, A. K., Sofi, N. Y., Kumar, R., Bhadoria, A. S. J. J. O. F. M. & Care, P. 2015. Childhood Obesity: Causes And Consequences. 4, 187.
Seo, S. H. & Shim, Y. S. J. S. R. 2019. Association Of Sleep Duration With Obesity And Cardiometabolic Risk Factors In Children And Adolescents: A Population-Based Study. 9, 1-10.
Spinelli, A., Buoncristiano, M., Kovacs, V. A., Yngve, A., Spiroski, I., Obreja, G., Starc, G., Pérez, N., Rito, A. I. & Kunešová, M. J. O. F. 2019. Prevalence Of Severe Obesity Among Primary School Children In 21 European Countries. 12, 244-258.
Tambalis, K. D., Panagiotakos, D. B., Psarra, G. & Sidossis, L. S. J. J. O. C. S. M. 2018. Insufficient Sleep Duration Is Associated With Dietary Habits, Screen Time, And Obesity In Children. 14, 1689-1696.
Taveras, E. M., Rifas-Shiman, S. L., Oken, E., Gunderson, E. P., Gillman, M. W. J. A. O. P. & Medicine, A. 2008. Short Sleep Duration In Infancy And Risk Of Childhood Overweight. 162, 305-311.
Tobaldini, E., Fiorelli, E. M., Solbiati, M., Costantino, G., Nobili, L. & Montano, N. 2019. Short Sleep Duration And Cardiometabolic Risk: From Pathophysiology To Clinical Evidence. Nat Rev Cardiol, 16, 213-224.
Touchette, É., Petit, D., Tremblay, R. E., Boivin, M., Falissard, B., Genolini, C. & Montplaisir, J. Y. J. S. 2008. Associations Between Sleep Duration Patterns And Overweight/Obesity At Age 6. 31, 1507-1514.
Tuohino, T., Morales-Muñoz, I., Saarenpää-Heikkilä, O., Kiviruusu, O., Paunio, T., Hovi, P., Pietiläinen, K. H. & Paavonen, E. J. J. T. J. O. P. 2019. Short Sleep Duration And Later Overweight In Infants.
Watson, N. F., Badr, M. S., Belenky, G., Bliwise, D. L., Buxton, O. M., Buysse, D., Dinges, D. F., Gangwisch, J., Grandner, M. A., Kushida, C., Malhotra, R. K., Martin, J. L., Patel, S. R., Quan, S. F. & Tasali, E. 2015. Recommended Amount Of Sleep For A Healthy Adult: A Joint Consensus Statement Of The American Academy Of Sleep Medicine And Sleep Research Society. Sleep, 38, 843-4.
Witchel, S. F., Oberfield, S. E. & Peña, A. S. J. J. O. T. E. S. 2019. Polycystic Ovary Syndrome: Pathophysiology, Presentation, And Treatment With Emphasis On Adolescent Girls. 3, 1545-1573.
Wu, Y., Gong, Q., Zou, Z., Li, H. & Zhang, X. 2017. Short Sleep Duration And Obesity Among Children: A Systematic Review And Meta-Analysis Of Prospective Studies. Obes Res Clin Pract, 11, 140-150.
Wu, Y., Zhai, L. & Zhang, D. J. S. M. 2014. Sleep Duration And Obesity Among Adults: A Meta-Analysis Of Prospective Studies. 15, 1456-1462.
Zhang, Y., Ren, R., Yang, L., Zhou, J., Sanford, L. D., Tang, X. J. N. & Reviews, B. 2019. The Effect Of Treating Obstructive Sleep Apnea With Continuous Positive Airway Pressure On Posttraumatic Stress Disorder: A Systematic Review And Meta-Analysis With Hypothetical Model.