1Department of Pediatric Dentistry and Orthodontics College of Dentistry, King Saud University, Riyadh, Saudi Arabia,
2Dental University Hospital, King Saud University, Riyadh Saudi, Arabia3Security Forces Specialized Polyclinics,
Ministry of Interior, Riyadh Saudi Arabia and 4Primary Healthcare Clinic, Ministry of Health, Riyadh Saudi Arabia
Corresponding author email: talthenyan@ksu.edu.sa
Article Publishing History
Received: 08/12/2020
Accepted After Revision: 15/03/2021
The present was study aimed to assess the treatment needs amongst orthognathic patients attending the Dental University Hospital at King Saud University using the Index of Orthodontic Treatment Need, Dental Health Component (IOTN-DHC) and the Index of Orthognathic Functional Treatment Need (IOFTN). A retrospective study was conducted on records of subjects who had been attending the Dental University Hospital at King Saud University, Riyadh Saudi Arabia, seeking orthodontic/surgical treatment in the period from 2000 to 2017. The pre-treatment sets of study models with their correspondent clinical photographs and radiographs were graded using the IOTN-DHC and the IOFTN. These assessments were undertaken by two calibrated dentists. The Class III skeletal pattern was the most prevalent type of malocclusion (54.5%). In total, 78.2% of the sample was classified by the IOFTN as having great and very great functional needs, as opposed to 91% classified by the IOTN. The most prevalent IOFTN score was 5.4 (open bite ≥ 4 mm, 25.4%), followed by 5.3 (reverse OJ ≥ 3 mm, 18.2%) and 4.2 (increased OJ ≥ 6 mm and ≤ 9 mm, 11%). The IOTN and IOFTN indices were highly correlated in assessing treatment needs for craniofacial problems. The IOFTN is a valid and reliable tool to prioritize treatment addressing functional needs. It is highly correlated with the IOTN in the prioritization of healthcare. The vast majority of patients undergoing orthognathic surgical procedures at the dental university hospital were in the great and very great need categories, and the Class III pattern was the most common type of malocclusion to be addressed by an orthognathic approach.
Indices, IOTN, IOFTN, Functional Needs.
Almoammar K. A, Alqahtani N. D, Alshayea E. I, Althenyan T. M, Alnatheer Y. M, Alqahtani N. H, Alzahrani Z. M, Albarakati S. F. Assessment of Treatment Needs in Orthognathic Patients in a Dental University Hospital in Saudi Arabia. Biosc.Biotech.Res.Comm. 2021;14(1).
Almoammar K. A, Alqahtani N. D, Alshayea E. I, Althenyan T. M, Alnatheer Y. M, Alqahtani N. H, Alzahrani Z. M, Albarakati S. F. Assessment of Treatment Needs in Orthognathic Patients in a Dental University Hospital in Saudi Arabia. Biosc.Biotech.Res.Comm. 2021;14(1). Available from: <a href=”https://bit.ly/3cAttxj”>https://bit.ly/3cAttxj</a>
Copyright © Almoammar et al., This is an open access article distributed under the terms of the Creative Commons Attribution License (CC-BY) https://creativecommns.org/licenses/by/4.0/, which permits unrestricted use distribution and reproduction in any medium, provide the original author and source are credited.
INTRODUCTION
The role of indices in healthcare includes classification of diseases, which can aid in understanding etiology, determining prognosis and possible treatment options, measuring the prevalence and incidence of a disease within a population, and prioritizing healthcare among individuals.Regardless of their purposes, simplicity and clarity, accessibility and feasibility, objectivity, amenability to statistical analysis, sensitivity, reliability, and validity, which is measuring what is supposed to be measured , are the key requirements for developing an ideal index of health, (Waring 2003, Barber 2017).
The word malocclusion lacks an adequate definition because of the wide variations among individuals in the perception of what constitutes an occlusal problem (Bellot-Arcís 2012). Hence, a number of indices are used to prioritize treatment in those with occlusal disorders and monitor the quality of their treatment outcomes, including the Index of Orthodontic Treatment Need (IOTN) (Brook 1989), the Dental Aesthetic Index (DAI) (Cons 1986), the Index of Complexity, Outcome and Need (ICON) (Daniels 2000), the Peer Assessment Rating (PAR) (Richmond 1992), and the Occlusal Index (OI) (Summers 1971).Dentofacial deformity describes a condition in which there are significant deviations in the maxillo-mandibular complex from normal proportions that also negatively affect the intra-arch and inter-arch relationships. Furthermore, breathing, speech, swallowing, chewing, lip closure, and psychosocial health can be adversely affected (Posnick 2013). Consequently, subjects with dentofacial deformities usually require a combination of orthodontic treatment and orthognathic surgery as part of an interdisciplinary approach to reposition the jaw to achieve a normalized and functional relationship. This may involve surgical procedures on the maxilla, mandible, or both jaws, as well as their dentoalveolar segments. Reports indicate that approximately 19% of individuals who attend an orthodontic assessment ideally require orthognathic procedures (Posnick 2013, Olkun et al 2019 Eslamian 2019).
The IOTN is the index most commonly used for prioritizing treatment. It has a dental health component (DHC), which is a modification of the index of treatment priority developed by the Swedish Dental Health Board (Linder-Aronson 1974), and an aesthetic component (AC) that was adapted from the Standardized Continuum of Aesthetic Need (SCAN) index (Evans 1987), both of which record the need for treatment based on dental health, functional grounds, and social-psychological grounds (Brook 1989). The IOTN has been widely applied in the UK National Health Services (NHS) primary care since 2006 (Ireland 2014). It has obtained a high level of agreement amongst examiners compared to different occlusal orthodontic indices (Brook 1989). Moreover, the DHC also shows strengths in the aspects of both time and ease of use (Cardoso 2011). This might be related to the acronym MOCDO (missing, overjet, crossbite, displacement of contact points, and overbite), which is used as a hierarchical scale to grade malocclusion (Richmond 1994). Therefore, the IOTN is the most frequently used index in orthodontic research (Bellot-Arcís 2012). In terms of grading, the DHC appears more reliable in providing constant grading over time, while the AC typically shows improvements during adolescence (Cooper 2000). The purpose of the IOTN-DHC is to assign a score to the occlusal traits that make up a malocclusion. The grading process categorizes the severity and need for treatment from 1 to 5, with grade 1 representing no need for treatment and grade 5 representing a significant need for treatment (Appendix, Table A).
However, there are some limitations in the use of the IOTN. In cases of the DHC, those with functional or facial concerns arising from dentofacial deformities and those not amenable to orthodontic treatment alone are not included. As a result, Ireland et al. recently established a new index, known as the Index of Orthognathic Functional Treatment Needs (IOFTN). Similar to the IOTN-DHC, the IOFTN has five grades —grade 1 shows no need for treatment and grade 5 shows a significant need for treatment (Appendix, Table B). Modifications and additions to the subcategories within the major categories were introduced to reflect the functional need for treatment indicated for orthognathic patients. Generally, the index will be applied to those with complete facial growth (Ireland 2014). Up to our knowledge there has been no attempt to evaluate the need and complexity of individuals undergoing orthodontics with surgical approach in a university setting in Saudi Arabia. Hence, the aim of this retrospective study was to assess the treatment needs among orthognathic patients attending the Dental University Hospital at King Saud University using the IOTN-DHC and the IOFTN.
MATERIAL AND METHODS
This retrospective study was conducted on records of subjects who had been attending the Dental University Hospital at King Saud University, Riyadh Saudi Arabia seeking orthodontic/surgical treatment in the period from 2000 to 2017. Ethical approval for this study was obtained from the Institution Review Board at the College of Medicine, King Saud University, Riyadh KSA (E-17-2644; 06/11/2017). The collected records included pre-treatment study models, photographs and orthopantomographs (OPGs), lateral cephalometric radiographs, and relevant demographic information. Incomplete records, such as missing or damaged study models, missing or poor-quality photographs, and missing or poor-quality radiographs, were excluded from the study.
For all selected samples, demographic characteristics, including age and gender, were recorded. The pre-treatment sets of the study models, with their correspondent clinical photographs, were graded using the IOTN-DHC and the IOFTN. OPG radiographs were used to assess relevant clinical information, such as impacted teeth, missing teeth, and supernumerary teeth. The pre-treatment cephalometric radiographs were used to assess the anteroposterior skeletal relationship. Measurements and assessments were performed by two calibrated dentists. These measurements were done twice over a 10 day nterval to assess the inter- and intra-operator agreement.
Statistical Analysis: Descriptive statistics (mean, standard deviation, frequencies) were used to describe the quantitative and categorical variables. Intraclass correlation was used to quantify the inter-operator and intra-operator consistency in the assessment of the IOFTN and IOTN scale levels. Spearman’s rank correlation was used to quantify the relationship between the two indices. The frequencies of the different components of the IOFTN and IOTN between different genders and malocclusions were compared using Pearson’s chi-square test. Data were calculated using IBM® SPSS® Statistics, Version 22 (International Business Machines Corporation; Armonk, New York, USA) at a predetermined significance level of p < 0.05.
RESULTS AND DISCUSSION
In total, 80 subjects were part of the study; 25 subjects were excluded from the study because of incomplete records. Thus, 55 participants were included in this study. Among these subjects, there were 31 females (56.4) and 24 males (43.6). The age ranged from 18–39 years, with a mean age of 21.3 years and a standard deviation 4.6. Inter-operator agreements for the major categories of the IOTN and the IOFTN were highly correlated (Table 1); the intra-operator agreement for the IOFTN and IOTN was very good (Table 2).The Class III skeletal pattern was the most prevalent type of malocclusion (54.5%) (Table 3). According to Table 4, the most prevalent IOFTN score was 5.4 (open bite ≥ 4 mm, 25.4%), followed by 5.3 (reverse OJ ≥ 3 mm, 18.2%) and 4.2 (increased OJ ≥ 6 mm and ≤ 9 mm, 11%).
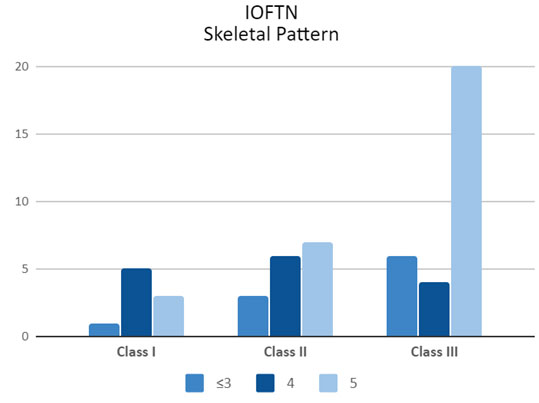
Overall, the percentage of patients who underwent orthognathic surgery scoring grade 4 and grade 5 functional needs was 78.2% according to the IOFTN. The distribution of IOFTN grades is shown in Table 4, while the distribution of IOTN scores is shown in Table 5. In addition, 91% of the patients had great and very great needs, according to the IOTN-DHC. There was no significant difference in gender frequencies for the different components of the IOFTN and the IOTN-DHC when they were re-grouped to grades ≤3, 4, and 5; this difference was observed at the P < 0.05 level. Overall, Class III sagittal skeletal pattern subjects showed a higher percentage (63.3%) of IOFTN grade 5 (very great need); however, subjects with Class II skeletal patterns demonstrated a higher percentage of grade 4 (great need) (Figure 2). Spearman’s correlation between the two indices revealed a highly significant correlation by the two examiners (Table 6). This level of significance is evidence of a sufficient sample size.
Table 1. Inter-operator agreement for the major categories.
| IOTN | IOFTN | ||||
| Examiner | Intraclass correlation | 95% confidence interval | Examiner | Intraclass correlation | 95% confidence interval |
| 1 | 0.95 | 0.83 to 0.99 | 1 | 0.92 | 0.70 to 0.98 |
| 2 | 2 | ||||
Table 2. Intra-operator agreement for the major categories.
| IOTN | IOFTN | ||||
| Examiner | Intraclass correlation | 95% confidence interval | Examiner | Intraclass correlation | 95% confidence interval |
| 1 | 1.00 | 1.00 to 1.00 | 1 | 0.98 | 0.94 to 0.99 |
| 2 | 0.96 | 0.83 to 0.99 | 2 | 0.93 | 0.73 to 0.98 |
Table 3. Sagittal skeletal pattern distribution in the study sample.
| Skeletal Discrepancies | Frequency | Percent | |
| Class I | 9 | 16.4 | |
| Class II | 16 | 29.1 | |
| Class III | 30 | 54.5 | |
| Total | 55 | 100 | |
Table 4. Distribution of the IOFTN functional need scores categories in the study sample.
| IOFTN | Gender | Total (%) | |
| Male | Female | ||
| 1.14 | 2 | 2 | 4 (7.3) |
| 2.9 | 0 | 1 | 1 (1.8) |
| 2.11 | 0 | 1 | 1 (1.8) |
| 3.3 | 2 | 3 | 5 (9.1) |
| 3.4 | 0 | 1 | 1 (1.8) |
| 4.1 | 2 | 1 | 3 (5.5) |
| 4.2 | 2 | 4 | 6 (10.9) |
| 4.4 | 1 | 3 | 4 (7.3) |
| 4.8 | 0 | 1 | 1 (1.8) |
| 5.2 | 2 | 2 | 4 (7.3) |
| 5.3 | 8 | 2 | 10 (18.2) |
| 5.4 | 5 | 9 | 14 (25.4) |
| 5.7 | 0 | 1 | 1 (1.8) |
| Total | 24 | 31 | 55 |
Table 5. Distribution of the IOTN Dental Health Components in the study sample.
| IOTN
(DHC) |
Gender | Total (%) | |
| Male | Female | ||
| 2b | 0 | 1 | 1 (1.8) |
| 3b | 2 | 0 | 2 (3.6) |
| 3d | 0 | 1 | 1 (1.8) |
| 3e | 0 | 1 | 1 (1.8) |
| 4a | 1 | 1 | 2 (3.6) |
| 4b | 2 | 0 | 2 (3.6) |
| 4c | 0 | 2 | 2 (3.6) |
| 4d | 1 | 2 | 3 (5.5) |
| 4e | 2 | 3 | 5 (9.1) |
| 4h | 7 | 9 | 16 (29.1) |
| 5a | 2 | 3 | 5 (9.1) |
| 5h | 5 | 4 | 9 (16.4) |
| 5i | 0 | 3 | 3 (5.5) |
| 5m | 2 | 1 | 3 (5.5) |
| Total | 24 | 31 | 55 |
Figure 1: Distribution of IOTN (DHC) and IOFTN scores between genders.
Figure 2: Relationship between sagittal skeletal patterns and IOFTN grades.
Table 6. Spearman’s Correlation between the two indices.
| Spearman’s rho | IOFTN Examiner 1 | IOFTN Examiner 1 | P Value | ||
| IOFTN Examiner 1 | Correlation Coefficient | 1 | 0.328 | 0.05 | |
| Significance
(two-tailed) |
– | 0.014 | |||
| IOTN Examiner 1 | Correlation Coefficient | 0.328 | 1 | ||
| Significance
(two-tailed) |
0.014 | – | |||
| IOFTN Examiner 2 | IOFTN Examiner 2 | 0.01 | |||
| IOFTN Examiner 2 | Correlation Coefficient | 1 | 0.408 | ||
| Significance
(two-tailed) |
– | 0.002 | |||
| IOTN Examiner 2 | Correlation Coefficient | 0.408 | 1 | ||
| Significance
(two-tailed) |
0.002 | – | |||
Appendix THE IOTN INDEX
Table A. The dental health component of the IOTN, adapted from Brook and Shaw (4).
| Grade 1 (None)
1 Extremely minor malocclusions including displacements less than 1 mm. |
| Grade 2 (Little)
2a Increased overjet 3.6–6 mm with competent lips. 2b Reverse overjet 0.1–1 mm. 2c Anterior or posterior crossbite with up to 1 mm discrepancy between retruded contact position and intercuspal position. 2d Displacement of teeth 1.1–2 mm. 2e Lateral or anterior open bite 1.1–2 mm. 2f Increased overbite 3.5 mm or more, without gingival contact. 2g Prenormal or post. |
| Grade 3 (Moderate)
3a Increased overjet 3.6–6 mm with incompetent lips. 3b Reverse overjet 1.1–3.5 mm. 3c Anterior or posterior crossbites with 1.1–2 mm discrepancy. 3d Displacement of teeth 2.1–4 mm. 3e Lateral or anterior open bite 2.1–4 mm. 3f Increased and complete overbite without gingival trauma. |
| Grade 4 (Great)
4a Increased overjet 6.1–9 mm. 4b Reverse overjet greater than 3.5 mm with no masticatory or speech difficulties. 4c Anterior or posterior crossbites with greater than 2 mm discrepancy between retruded contact position and intercuspal position. 4d Severe displacements of teeth, greater than 4 mm. 4e Extreme lateral or anterior open bites, greater than 4 mm. 4f Increased and complete overbite with gingival or palatal trauma. 4h Less extensive hypodontia requiring pre-restorative orthodontic space closure to obviate the need for a prosthesis. 4l Posterior lingual crossbite with no functional occlusal contact in one or both buccal segments. 4m Reverse overjet 1.1–3.5 mm with recorded masticatory and speech difficulties. 4t Partially erupted teeth, tipped and impacted against adjacent teeth. 4x Supplemental teeth. |
| Grade 5 (Very Great)
5a Increased overjet greater than 9 mm. 5h Extensive hypodontia with restorative implications (more than 1 tooth missing in any quadrant) requiring pre-restorative orthodontics. 5i Impeded eruption of teeth (with the exception of third molars) due to crowding, displacement, the presence of supernumerary teeth, retained deciduous teeth and any pathological cause. 5m Reverse overjet greater than 3.5 mm with reported masticatory and speech difficulties. 5p Defects of cleft lip and palate. 5s Submerged deciduous teeth. |
THE IOFTN INDEX
Table B. The scoring system of the IOFTN, adapted from Ireland et al. (14)
| Grade 1 (None)
1.12 Speech difficulties. 1.13 Treatment purely for TMD. 1.14 Occlusal features not classified above. |
| Grade 2 (Little)
2.8 Increased overbite, but no evidence of dental or soft tissue trauma. 2.9 Upper labial segment gingival exposure < 3 mm at rest with no evidence of gingival/periodontal effects. 2.11 Marked occlusal cant with no effect on the occlusion. |
| Grade 3 (Moderate)
3.3 Reverse overjet ≥ 0 mm and < 3 mm with no functional difficulties. 3.4 Open bite < 4 mm with no functional difficulties. 3.9 Upper labial segment gingival exposure < 3 mm at rest, but with evidence of gingival/periodontal effects. 3.10 Facial asymmetry with no occlusal disturbance. |
| Grade 4 (Great)
4.2 Increased overjet ≥ 6 mm and ≤ 9 mm. 4.3 Reverse overjet ≥ 0 mm and < 3 mm with functional difficulties. 4.4 Open bite < 4 mm with functional difficulties. 4.8 Increased overbite with evidence of dental or soft tissue trauma. 4.9 Upper labial segment gingival exposure ≥ 3 mm at rest. 4.10 Facial asymmetry associated with occlusal disturbance. |
| Grade 5 (Very Great)
5.1 Defects of cleft lip and palate and other craniofacial anomalies. 5.2 Increased overjet > 9 mm. 5.3 Reverse overjet ≥ 3 mm. 5.4 Open bite ≥ 4 mm. 5.5 Complete scissors bite affecting whole buccal segment(s) with signs of functional disturbance and or occlusal trauma. 5.6 Sleep apnoea not amenable to other treatments such as MAD or CPAP (as determined by sleep studies). 5.7 Skeletal anomalies with occlusal disturbance as a result of trauma or pathology. |
According to Ireland et al., the IOFTN was developed to overcome the limitations of the IOTN’s DHC, which does not account for the skeletal components of malocclusion, as well as to assist in prioritizing public resources for orthognathic surgery (Ireland 2014). Reliability is an important requirement for an index. The present study established a very good inter-operator agreement with the IOFTN, as in the results reported by Ireland et al. (0.64–0.88) (Ireland 2014). The inter-operator agreement for the IOTN demonstrated a very good agreement in contrast to the kappa scores reported by Brook and Shaw (0.73–0.79) (Brook 1989). The study showed a very good intra-operator agreement for the IOFTN, in contrast to the findings by Ireland et al. (0.53–0.80) (Ireland 2014). The IOTN intra-operator agreement ranged from a good to a very good agreement, which is comparable to the results reported by Brook and Shaw (0.75–0.84) (Brook 1989).
In the present sample, the most prevalent IOFTN score was 5.4 (open bite ≥ 4 mm, 25.4%), followed by 5.3 (reverse OJ ≥ 3 mm, 18.2%), and 4.2 (increased OJ ≥ 6 mm and ≤ 9 mm, 11%). The findings have been different in the other studies as a study conducted in a University Hospital in Iran and found that the most prevalent score was 5.3, followed by 4.2 and 4.3 (reverse overjet ≥ 0 mm and < 3 mm with functional difficulties) (Borzabadi-Farahani 2016). Harrington et. al.(2017) conducted a study in UK and reported that the most prevalent score was 5.2 (increased overjet > 9 mm), followed by 5.3 and 4.2. In Turkey, Olkun et. al.(2019) conducted study and found that the most prevalent score was 5.3, followed by 4.3 and 5.4 Another study in Iran (Eslamian 2019) reported that the most IOFTN score was 4.3, followed by 5.3 and 5.4. The Class III skeletal pattern was the most prevalent (54.5%) sagittal skeletal relationship, which is similar to the findings of earlier workers, (Eslamian 2019, Olkun 2019, Harrington 2017, Lee 2014, Al-Deaiji 2001) and in contrast to (Borzabadi-Farahani 2016).
These variations are most notably attributed to the different ethnic backgrounds of the samples. More than half of the subjects with the Class III skeletal pattern were categorized as having a great to very great functional need for orthognathic surgery, justifying the proposed treatment offered to these patients. According to the IOFTN, 78.2% of the patients were classified as having great or very great functional needs.
This is dissimilar to previous findings in the UK, Iran and Turkey, reporting 88–95% of patients as having great or very great functional needs (Howard-Bowles 2017, Borzabadi-Farahani 2016, Harrington 2017, Olkun 2019, Eslamian 2019). As stated in Howard-Bowles’ study, the definition of occlusal traits within the major categories of the IOFTN needs to be improved; moreover, a calibration course similar to that for the IOTN is required to reduce ambiguous interpretations of the traits described. Suggestions were made to propose a system resembling that of the IOTN (MOCDO) to ensure efficiency in scoring patients; hence, the acronym OOSGA would follow the hierarchy (overjet, overbite, scissor bite, gingival exposure, and asymmetry) (Howard-Bowles 2017). However, the IOFTN mostly assesses occlusal traits, ignoring the skeletal component of malocclusion. This is particularly important when assessing subjects with well compensated malocclusion, those who have had previous orthodontic treatment, or those who do not necessarily score high using the IOFTN but have severe sagittal, vertical, or transverse skeletal discrepancies.
There are shortcomings in the present study, one of which is that it is retrospective, cross-sectional, and single center in nature. Another limitation lies in the lack of skeletal discrepancy consideration in the use of the IOTN and IOFTN indices. It is imperative to consider that scoring with the IOFTN from study models will require additional information, mainly the presence of the patient to address some subcategories, such as facial asymmetry, upper labial gingival exposure, soft tissue trauma due to excessive overbite, sleep apnea, and any trauma or pathology causing skeletal anomalies with occlusal discrepancy.
CONCLUSION
The IOFTN is a valid and reliable tool for prioritizing treatment addressing functional needs. It is highly correlated with the IOTN in prioritizing healthcare. The vast majority of patients undergoing orthognathic surgical procedures at the Dental University Hospital at King Saud University were in the great and very great need categories. The most common type of malocclusion to be addressed through an orthognathic approach was the Class III pattern. These findings shed a light on the complexity of skeletal malocclusions undergoing orthognathic surgery. A comprehensive nationwide study evaluating the need and complexity of orthognathic surgeries are required, to support in legislations governing health services in the Kingdom.
REFERENCES
Al-Deaiji (2001) Characteristics of dentofacial deformities in a Saudi population. Saudi Dental Journal, 13, 101-105
Barber (2017) Would the introduction of the Index of Orthognathic Functional Treatment Need (IOFTN) affect referrals and acceptance of people for orthognathic treatment? British dental journal, 222(5), 368
Bellot-Arcís (2012) The use of occlusal indices in high-impact literature. Community dental health, 29(1), 45-48
Borzabadi-Farahani (2016). Functional needs of subjects with dentofacial deformities: A study using the index of orthognathic functional treatment need (IOFTN). Journal of Plastic, Reconstructive & Aesthetic Surgery, 69(6), 796-801
Brook (1989) The development of an index of orthodontic treatment priority. The European Journal of Orthodontics, 11(3), 309-320
Cardoso (2011) The Dental Aesthetic Index and dental health component of the Index of Orthodontic Treatment Need as tools in epidemiological studies. International journal of environmental research and public health, 8(8), 3277-3286
Cons (1986) DAI–the dental aesthetic index. College of Dentistry, University of Iowa
Cooper (2000) The reliability of the Index of Orthodontic Treatment Need over time. Journal of orthodontics, 27, 47-53
Daniels (2000) The development of the index of complexity, outcome and need (ICON). Journal of orthodontics, 27, 149-162
Eslamian (2019) An Objective Assessment of Orthognathic Surgery Patients. Journal of Craniofacial Surgery, 30(8), 2479-2482
Evans (1987) Preliminary evaluation of an illustrated scale for rating dental attractiveness. The European Journal of Orthodontics, 9(1), 314-318
Howard-Bowles (2017) The application of the Index of Orthognathic Functional Treatment Need (IOFTN): service evaluation and impact. Journal of orthodontics, 44(2), 97-104
Harrington (2017) A retrospective analysis of dentofacial deformities and orthognathic surgeries using the index of orthognathic functional treatment need (IOFTN). International journal of pediatric otorhinolaryngology, 79(7), pp.1063-1066
Ireland (2014) An index of orthognathic functional treatment need (IOFTN). Journal of orthodontics, 41(2), 77-83
Lee (2014) Dentofacial deformities and orthognathic surgery in Hong Kong and Glasgow. Annals of the Royal Australasian College of Dental Surgeons, 22, 113
Linder-Aronson (1974) Orthodontics in the Swedish Public Dental Health System. Transactions of the European Orthodontic Society, 50, 233–240
Olkun (2019) Orthognathic surgery treatment need in a Turkish adult population: a retrospective study. International journal of environmental research and public health, 16(11), 1881
Posnick (2013) Principles and Practice of Orthognathic Surgery. Elsevier Health Sciences
Richmond (1994) An Introduction to Occlusal Indices. Manchester: Mandent Press
Richmond (1992) The development of the PAR Index (Peer Assessment Rating): reliability and validity. The European Journal of Orthodontics, 14(2), 125-139
Summers (1971) The occlusal index: a system for identifying and scoring occlusal disorders. American Journal of Orthodontics, 59(6), 552-567
Waring (2003) Does the GDP need to know about IOTN?. Dental update, 30(3), 123-130