1Department of Physiotherapy, School of Pharmacy and Medical
Sciences, Singhania University, Pacheri Bari, (Rajasthan) India.
2Department of Physiotherapy, School of Pharmacy and Medical Sciences,
Singhania University, Pacheri Bari, (Rajasthan) India.
3Dr. Shakuntala Mishra National Rehabilitation University, Department of
Empowerment of Persons with Disabilities, Lucknow, Uttar Pradesh, India.
Corresponding author email: rajeevnirtar@gmail.com
Article Publishing History
Received: 27/06/2025
Accepted After Revision: 09/08/2025
Lower limb amputations impact mobility, health, social independence, psychological well-being, and economic stability. Accidents are the leading cause in developing countries, like India. affecting amputees’ quality of life. However, pain and dissatisfaction remain challenges. This systematic review aimed to explore the impact of current trends and various factors on patient satisfaction with lower limb prostheses, and their influence on health-related quality of life, drawing insights from qualitative literature. We searched the databases, including Web of Science, Saudi Digital Library (EBSCO), Science Direct and Google Scholar for systematic reviews, involving QOL and functional instruments for lower limb amputees with prostheses. Published articles from 2008 to 2023 were selected. Participant characteristics, inclusion criteria, outcome measures, study design, and results were explicated. Thirteen articles, published between 2008 and 2023, met the inclusion criteria. Factors impacting quality of life include cognitive ability, the cause of the amputation, amputation level, early prosthesis use, employment status, and social and psychological aspects. Additional factors include age, gender, marital status, education, income, and time since amputation.This study explores the relationship between lower limb amputation and quality of life, focusing on factors like amputation level, etiology, physical activity, social and psychological aspects, cognitive ability, pain, comorbidities, discomfort, accessible devices, work status, income, education, and living region. Prosthesis users experience superior QOL.
Health, Prosthesis, Amputation, Lower limb, Quality of life.
Kumar R, Jain A, Kumar R. Assessing Quality of Life in Lower Limb Amputees with Prosthetic Devices: A Systematic Review. Biosc.Biotech.Res.Comm. 2025;18(3).
Kumar R, Jain A, Kumar R. Assessing Quality of Life in Lower Limb Amputees with Prosthetic Devices: A Systematic Review. Biosc.Biotech.Res.Comm. 2024;18(3). Available from: <a href=”https://shorturl.at/7iT52“>https://shorturl.at/7iT52</a>
INTRODUCTION
Lower limb amputations cause inconveniences in walking and affect other daily activities along with psychological and social challenges (Day, Wadey and Strike, 2019). Limb amputation significantly impacts a person’s quality of life, affecting mobility, physical health, social independence, psychological status, and economic status (Sinha, van den Heuvel and Arokiasamy, 2011). Amputations may be due to congenital, pathological, or traumatic events may be the cause of an amputation(Havard, Trauma and 2025, no date). A comprehensive review of studies is required to understand amputees’ quality of life, improve rehabilitation and enhance healthcare professionals’ knowledge.A study published in 2021 revealed that globally, 57.7 million individuals were grappling with limb amputation stemming from traumatic incidents. Among the primary traumatic causes identified were falls (36.2%), road injuries (15.7%), other transportation-related accidents (11.2%), and mechanical forces (10.4%) (McDonald et al., 2021). In India, the overall rate of disability is 4.52%, with locomotor disabilities accounting for 44.70% of cases (Mohanty, Mohanty and Sabut, 2020; Pattnaik et al., 2023).
Accidents are the primary cause of most lower limb amputations in India. Additional investigations from Chennai and Kolkata supports this fact (Pooja and Sangeeta, 2013a; Mukundan et al., 2020). The quality of life is greatly impacted by the role of prostheses; Characteristics with a higher impact include a healthy stump, immediate prosthesis fitting, alignment and gait training, high-quality prostheses, amputee satisfaction, income source, and social and family support(Rafi, 2020). Factors that adversely impact quality of life include older age, duration of time after amputation, lack of family and social support, short amputation level, maximum functional loss, job satisfaction, family education, and the presence of disease (Sinha, van den Heuvel and Arokiasamy, 2011; Davie-Smith et al., 2017; Zaheer et al., 2020; Fatima, 2023).
Amputees can walk and perform daily activities with the help of a suitable prosthetic device, boosting their activity, independence, and happiness (Sindwani et al., 2023). The social reintegration of the patient may benefit even from an aesthetically pleasing prosthetic device. Numerous studies have investigated functional performance, health status, mobility level, and predictive factors in lower limb amputation. However, these findings are rarely associated with prosthetic satisfaction or health-related factors of life(Brunelli et al., 2020; Roberts et al., 2021; Dade Matthews, 2022; Norvell et al., 2024).
Notably, pain, particularly low back pain or phantom pain, significantly impacts a person’s poor quality of life in addition to their physical disability, (Polat et al., 2021). In India, the number of traumatic lower limb amputees is higher than those from other pathological conditions, (Kumar et al., 2020).Younger, healthier traumatic injury patients generally recover faster and adapt to prosthetics more easily, although they may struggle with the psychological impact of sudden limb loss(Sanders et al., 2020). With proper support, they often respond well to rehabilitation. In contrast, Patients with peripheral vascular injuries often experience slower healing and more complications during prosthesis fitting and recovery due to poorer circulation and comorbidities, (Day et al., 2023). Older age and other health conditions can further delay rehabilitation and prosthetic adaptation, emphasizing the need for comprehensive management for successful recovery(Knight, Dearth and Hendershot, 2021). Furthermore, early-life traumatic amputation is often linked to improved quality of life compared to amputation due to other pathological conditions (Vieira et al., 2024).
Strategies to select article between 2008-2023 aimed to understand advancements in prosthesis fitting in lower limb amputees that may affect health related quality of life. “Despite an extensive search conducted over the past 16 years, no systematic review studies addressing quality of life for lower limbs amputees in the context of India and the Asian region were found. “In recent years, the landscape of lower limb prosthetic services in India has witnessed a significant shift with numerous private organizations establishing centers across various regions. These centers have played pivotal roles in technology transfer and innovation. Consequently, both private and government entities have actively engaged in the fitting and provision of lower limb prostheses. This diversification has empowered patients, offering them choices beyond government-run facilities, and free camps(Pal, 2020). Improved financial conditions and income diversification enable individuals to invest in health and quality of life through private healthcare options, fostering employment and integrating prosthetic technology into daily routines, creating a promising avenue in lower limb prosthetics (Baru and Nundy, 2020; Poonekar and Gupta, 2022; Neelakantan and Kulkarni, 2023).
METHODOLOGY
We adhered to the Moher et al. Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (Moher et al., 2009) We screened qualitative studies whose main objective was to use reliable and valid tools, techniques, or systems that might be used to evaluate how prosthetic fitting affected mobility, physical health, and quality of life. Most included studies are sourced from Asian publications, with a limited representation from other geographical regions.
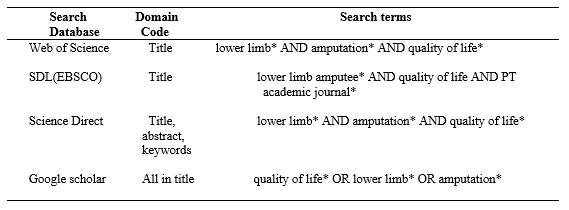
Search Strategy- We searched the following databases: Web of Science, Saudi Digital Library (EBSCO), Science Direct and Google Scholar for studies including QOL for lower limb amputees with prostheses. Key phrases including “quality of life,” “lower limb,” “prosthesis,” “amputation,” and “health” were used to search for relevant information. The database was searched from its creation until 2023, and only English-language journal articles, review papers, and clinical research papers were included. The search was performed by first author (RK) on 24 February 2024.
Table 1. Search strategy for databases.
Inclusion and Exclusion: The study includes individuals with unilateral or bilateral transtibial, knee, transfemoral, or hip joint amputations, as well as prosthesis users, and their quality-of-life issues. We included studies using various research methods including randomized controlled trials, quasi-randomized controlled trials, controlled trials, cohort studies, or cross-sectional studies. Qualitative Studies published between 2008 and 2023 were eligible for inclusion. Participants should have undergone lower limb amputations due to congenital, traumatic, vascular, or tumor-related causes, in consultation with professionals and caregivers. Studies that do not focus on the use of prostheses were excluded. Articles published before 2008 were not considered. Publications in languages other than English were excluded. Studies involving participants below the age of 18 were excluded. Articles including case reports, reviews, editorial opinions, testimonials, biographies/interviews, books, or discussions unrelated to the quality of life in amputees with of their lower limbs were excluded.
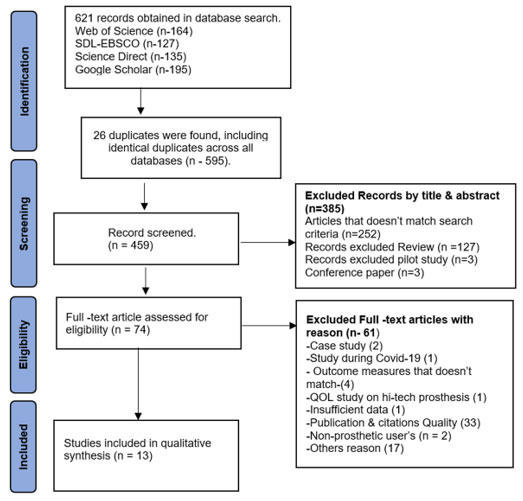
Selection Criteria- All identified studies published between 2008 and 2023 were imported using CSV and BibTeX formats, and subsequently transferred to an Excel (2016) sheet for organization. which were then compiled into the Excel sheet. Duplicate entries were removed, and the remaining data underwent thorough scrutiny based on predefined inclusion and exclusion criteria. Figure-1 illustrates the selection procedure. Investigators R.K independently screened the relevant research articles from Web of Science, Saudi Digital Library (EBSCO), Science Direct and Google Scholar databases. Author -3 (R.K) reviewed exclusion and inclusion criteria, electronic article relevancy, abstract suggestions and instructed to follow PRISMA pattern for the review study. Senior author-2 (AJG) verified the result and finalized the methodological quality of the study. Publications that addressed health-related quality of life were excluded if any of the inclusion criteria were not satisfied.
Figure 1: Flow chart PRISMA assessment.
Data Extraction: Data were retrieved by the first author (RK) regarding the author, Year of publication, Country of publication, publication in a journal and the study characteristics (including participant number, mean age, gender, marital status, education, amputation level, amputation cause, and prosthesis use), inclusion/exclusion, outcome measures, study design, results and conclusion based on Butler et al.’s research design (Butler et al., 2000) The initial search yielded 621 research articles from various databases, from which we extracted 13 records.
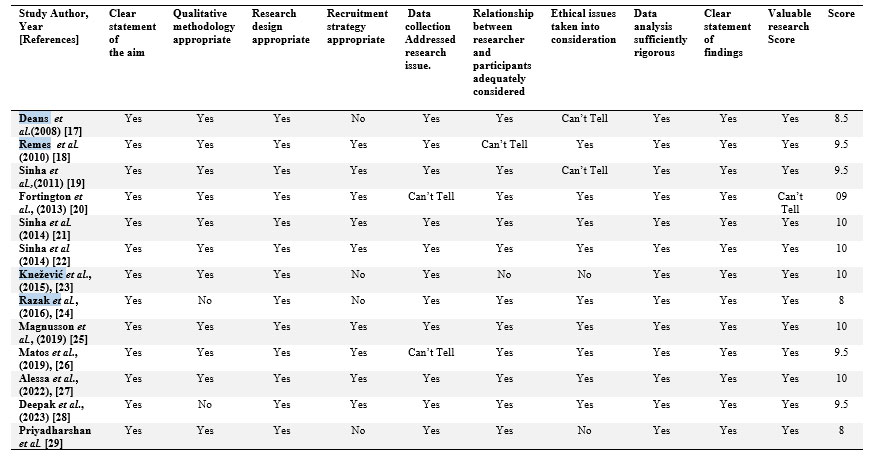
Study Quality: We followed the advice given by Butler et al. (2016) for qualitative studies, using the Critical Appraisal Skills Program (CASP, 2018). A 10-point scale was used for critical evaluation in a quality study we did. Each CASP item received a score of “yes” (1 point), “unsure” (0.5 points), or “no” (0 points). High-quality papers scored between 9 and 10, while moderate quality papers scored 7.5–9. Low quality papers less than 7.5 or less than 6 were excluded. The careful evaluation was done by the first author (RK). Due to the standards suggested by Butler et al. (2016), studies were not ruled out (“Critical Appraisal Skills Programme. CASP,” no date; Butler et al., 2000).
RESULTS AND DISCUSSION
A total of 621 studies were found using four databases: Google Scholar (n =195), SDL-EBSCO (n =127), Science Direct (n =135), and Web of Science (n =164). After reviewing the title and abstract 385 studies were eliminated for not meeting the inclusion criteria, 13 studies were removed as duplicates, and 13 studies were identical duplicates across all four databases. Sixty-one full-text articles were rejected for reasons during the second screening, leaving 74 full-text articles that were still accessed for eligibility. Thirteen research studies are included in this evaluation figure 1. The studies were conducted in India (n = 6), Malaysia (n = 1), Saudi Arabia (n = 1), Serbia (n = 1), the United Kingdom (n = 1), the Netherlands (n = 1), Finland (n = 1), and Brazil (n = 1). The studies included were published between 2008 and 2023.
According to the qualitative assessment result checklist for critical appraisal, all the studies scored between 8 and 10 points on the CASP scales. Ten were of high quality, and three received a moderate score (“Critical Appraisal Skills Programme. CASP,” no date).
Table 2. CASP Quality assessment.
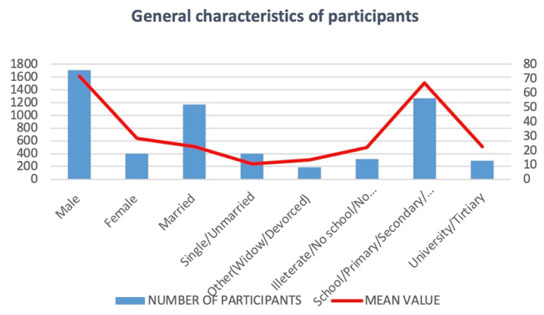
The studies’ heterogeneity led to data synthesis completion through descriptive analysis. There were 2108 participants in the study, with a mean age of 50.55. Of these, 400 (18.95%) were female and 1708 (81.05%) were male. Among the participants, 1169 (66.77%) were married, 397 (22.67%) were single or unmarried, and 185 (10.56%) were divorced or widowed. Only Remes et al. discussed the marital status categories of unmarried, divorced, and widowed together (Remes et al., 2010). Fortington, Knežević, Magnusson, Deepak, and Priyadharshan et al. did not specify the participants marital status (Fortington et al., 2013; Knežević et al., 2015; Magnusson et al., 2019; Priyadharshan et al., 2022; K et al., 2023).
315 individuals (16.71%) reported being illiterate, while 1269 participants (67.65%) reported having received schooling, vocational education, or primary and secondary education. Additionally, 292 participants (15.56%) reported having obtained university or tertiary-level education. It’s worth noting that Fortington et al., Knežević et al., and Priyadharshan et al. did not provide education reporting in their studies (Fortington et al., 2013; Knežević et al., 2015; Priyadharshan et al., 2022, 2022).
Figure 2: General characteristics of participants.
Traumatic injury accounted for 1202 (62.99%) of the participant causes; diabetes mellitus, including vascular disease, accounted for 655 (34.32%); tumors accounted for 70 (3.66%); and congenital conditions accounted for 181(9.48%). While Razak et al. collectively discuss vascular disease and infection in 24 (57.2%) cases, Alessa et al. collectively reported on vascular cases, diabetes, and infection in 96 (40.2%) instances (Razak et al., 2016; Alessa et al., 2022).
Figure 3: Specific characteristics of participants.
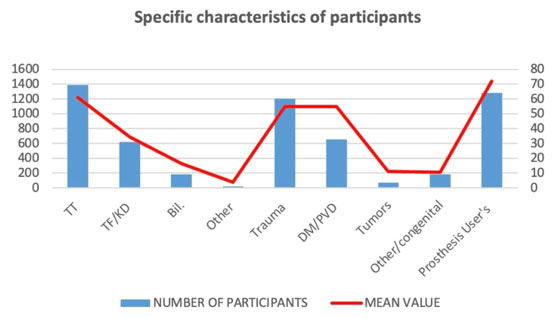
In total number of participants with various amputation levels was 1385 (65.7%) for transtibial amputations, 621 (29.46%) for transfemoral with knee disarticulation, 81 (3.85%) for bilateral amputations, and 21 (0.99%) for others. Among these, 1283 participants (or 60.83.2% of the total) used prostheses. Studies by Fortington et al. indicate that most participants are prosthesis users, while Deans et al., Sinha et al. in 2014 study and Knežević et al. mention prosthesis users in their inclusion criteria (Deans, McFadyen and Rowe, 2008; Sinha, Van Den Heuvel and Arokiasamy, 2011; Fortington et al., 2013; Sinha et al., 2014; Knežević et al., 2015).
The average study looks at adult men and women aged 18 and up who have had a lower limb amputated trans-tibial or trans-femoral, or who had their limb amputated because of diabetes, vascular disease, or an infection, and have been in rehabilitation for at least 6 months. People with severe psychopathology, end-stage cancer, left-side hemiparesis, vision impairment, or other psychiatric disorders were excluded in several studies. Additionally, individuals with clinical dementia, an ipsilateral amputation history, difficulty reading or writing Dutch, and recall bias-related selection more than five days after the amputation were excluded by Fortington et al. Magnusson et al. excluded from their study protrauma, psychiatric illness, patients over the age of eighteen who had lower limb amputations for more than six months, individuals with amputations, post-amputations, refusal to participate, and hearing, speech, or visual function disorders. They also excluded organization staff and students who used prosthetics or orthotics (Fortington et al., 2013; Magnusson et al., 2019)
Most frequently employed outcome measure across the studies reviewed was the MOS SF-36, which encompasses variations such as RAND-36 and SF-12, was utilized a total of seven times Following closely, the PEQ measure was employed in one instance (Harness, Related and 2001, no date; Hays and Morales, no date; Ware, 2000; Condie et al., 2006). TAPES and its revised version, TAPES-R, were each utilized six times, respectively. Furthermore, the WHOQOL-Brief was utilized in five instances among the studies reviewed [38]. Remes et al. also used self-reported life satisfaction scores, the 6-item Brief Social Support Questionnaire, and the Geriatric Depression Scale. Alessa et al. utilized the DASS (Depression, Anxiety, and Stress Scale), 12-item ZBI (Zarit Burden Interview) (Remes et al., 2010) (Deans, McFadyen and Rowe, 2008).
Most of the research talk on participant characteristics such the level and aetiology of amputation. Less often brought up topics are marital status and level of education. Deans et al. have out that social and psychological aspects are critical for improved quality of life, with decreased physical activity being a worry. According to Remes et al., pain and comorbidities are associated with lower QOL, although cognitive ability is positively correlated with higher QOL (Remes et al., 2010). According to Sinha et al. in 2011, prosthesis use, comorbidities, and discomfort relate to lower QOL, but employment status and assistive devices are linked to higher QOL (Sinha, Van Den Heuvel and Arokiasamy, 2011) Sinha et al. in 2014 found that QOL is influenced by employment, prosthesis use, and gender, and that unemployment is linked to poorer social adjustment and QOL (Sinha et al., 2014) (Sinha, Van Den Heuvel and Arokiasamy, 2014) Fortington et al. state that pain, vitality, physical function, social function, and perceived health are the primary elements of an enhanced quality of life [20].
According to Knežević et al., compared to lower amputation levels, transtibial amputations are more functional and have improved health related QOL [23]. Razak et al. discover that while physical domains lead to a lower quality of life, emotional support and psychological components have a stronger effect on QOL (Razak et al., 2016). Magnusson et al. highlight the importance of living area, education level, and income in determining quality of life (QOL), noting that physical handicap lowers QOL (Magnusson et al., 2019). Matos et al. found that prosthesis users had a higher quality of life than non-users, and that major factors contributing to increased QOL were pain, prosthesis adaptation, and psychological well-being (Matos, Naves and de ARAUJO, 2020). Priyadharshan et al. discover that variables like age, time since amputation, and prosthesis use contribute to improved QOL (Priyadharshan et al., 2022). Deepak et al. contend that early prosthesis fitting, and psychological counselling can significantly improve QOL, with delays exacerbating physical burdens and diminishing QOL (K et al., 2023).
Table 3. Summary of study.
| Details of Research Done |
Characteristics of participants – Number (N %) -Age (Mean) – Gender -Marital status -Education -Amputation level -Amputation cause -prosthetic user’s |
Inclusion and Exclusion | Outcome measures | Study design | Result | Conclusion |
| Deans et al. (June 2008), UK/Prosthetics and orthotics international
[17]
|
N- 25
Age (mean)- 66 Gender Male-20 (80%) & Female-5 (20%) Marital status Married -17 (85%) Widowed-3 (15%) Education Secondary -14 (70%) Tertiary- 6 (30%) Amputation level- TT- 22 (89%) & TF-3 (12%) Amputation cause- PVD Prosthesis User’s- 25 (100%) |
Inclusion- Adult men and women who underwent unilateral trans-tibial or trans-femoral lower-limb amputation and were able to wear and use a prosthesis were included in the study. The top age limit was left unspecified at eighteen. | TAPES,
WHOQOL-Brief |
cross-sectional study.
|
• Strong correlation between social elements in questionnaires.
• Significant relationships between scores in Psychological and Social domains. • Statistical correlation between TAPES subscales and WHOQOL-Bref domains. • No relationship between Athletic subscale of TAPES and WHOQOL-Bref domains.
|
The study’s finding that there is less of a correlation between physical activity and amputees’ quality of life highlights the significance of their relationships with peers, family, and friends. |
|
Remes et al. (October 2010), Finland/ Prosthetics &Orthotics international [18] |
N- 59
Age (Mean)- 75.17 year Gender Male- 28 (47%) Female- 31(53% Marital status Married- 21 (36%) Widowed, divorced, unmarried- 38 (64%) Education- Vocational school or learning at work- 20 (34%) College/university- 4 (7%) Amputation level- TT- 13 (22%) TF- 28 (48%) Bil.-18 (30%) Amputation cause- PVD Prosthesis user’s- 25(100%) |
Exclusion- The individuals were excluded due to their inability to respond to all items due to vision impairment, end-state cancer, left-side hemiparesis, or severe psychopathology. | RAND-36
Health-Related QoL instrument, Physical Functioning- and General Health subscales, Geriatric Depression Scale, 6-item Brief Social Support, Questionnaire, and Self-reported Life Satisfaction score. |
Cros-sectional study. | • Depression and anxiety common up to two years post-amputation.
• Cognitive ability crucially affects amputated patients’ quality of life. • Proper management of pain and comorbidity may mitigate depressive symptoms. • Feelings of ‘perceived control’ crucial for maintaining functional ability. • Assessment of depression in elderly crucial as it diminishes quality of life.
|
Institutionalization is linked to depressive symptoms, while home-dwelling amputees have generally good QoL scores. Rehabilitation should integrate QoL assessment with physical disability assessment. |
| Sinha et al., (March 2011), India/ Prosthetics &Orthotics international [19]
|
N- 605
Age (Mean)- 43.7 Gender Male -530 (88%) Marital status Married – 436 (72%). Single -117 (19%). Others – 52 (9%) Education- No schooling/missing – 119 (19%) High school- 428 (71%) University- 57 (9%) Amputation level TF/TK- 151 (25%) Bil. – 29 (5%) Other 15 (2%) Amputation cause Diabetes/vascular -135 (22%) Others 88 -(14%) Missing 1 (1%) |
Exclusion- The individual may experience a range of psychological disturbances, including a lack of participation, hearing or speech impairment, mental incapacity, or the loss of a family member. | MOS SF-36 | cross-sectional study. | • Lower limb amputees had worse QoL compared to the general population.
• Employment status and use of assistive devices were key determinants of QoL • Factors like prosthesis use, comorbidities, phantom-limb pain, and stump pain affected QoL.
|
The study found that lower limb amputees have worse quality of life compared to the general population, with employment status and use of assistive devices playing key roles. |
| Fortington et al., (June 2013),
Netherlands/ Journal of rehabilitation and medicine [20] |
N– 82 (77%) Age (Mean)- 67.8 yearGenderMale- 55 (67%)Female- 27 (33%) Marital status- N/S Education- N/S TT -52 (63%) TF/TK- 30(37%) Amputation cause- PVD Prosthesis user’s- 82(100%)
|
The study included individuals aged 18 and above who had a primary lower limb amputation due to vascular disease, infection, or diabetes.
The study excluded individuals with previous ipsilateral amputation, difficulty reading/writing Dutch, clinical dementia, or those recruited over 5 days after the amputation due to recall bias. |
Dutch version RAND-36
|
longitudinal study. | • The quality of life significantly improved in five of the seven domains.
• The level of physical function stayed below the population standard. • Age groups may see varying effects in various domains.
|
In five out of seven domains, the study indicated a significant increase in quality of life; the majority of these improvements happened within the first six months, while physical function remained below population norms. |
| Sinha et al.(April 2014), India/ Prosthetics & Orthotics international [21]
|
N- 368
Age- (Mean)- 43.13 year Gender Male- 324 (88%) Married -264 (72%). Single -70 (19%). Others – 34 (9%) Education Primary/secondary education – 260 (62%) Tertiary education- 43 (20.3%) TF/KD- 87 (23.7%) Amputation cause Diabetes/vascular 59(16%) Cancer- 14 (3.8%) Others 15 (3.9%) Prosthesis user’s –368 (100%) |
Inclusion- In considering the study’s objective, a cross-section of unilateral and non-congenital amputees who were wearing prosthetic limbs was taken into consideration.
Exclusion-The study excluded participants due to non-participation, hearing or speech impairment, mental incapacities, and limb fitting and gait training for amputees. |
PEQ,
TAPES |
Cross-sectional study. | • Factors influencing adjustments: age, employment, daily prosthesis use, assistive device use.
• Functional satisfaction linked to prosthesis use, phantom pain, employment, and gender. • Unemployed amputees less socially adjusted and restricted in activities.
|
Amputees who are not limited in their activities except for sports and who are generally content with how their prosthesis functions are also considered to be somewhat psychosocially adjusted. Age, occupation, amputation level, co-morbidity, gender, everyday prosthesis use, and assistive device use all affect modifications. |
| Sinha et al., (March 2014), India/ International journal of Rehabilitation [22]
|
N- 368
Age (Mean)- 43.13 Gender Male 324 (88%) Married 264 (72%). Single 70 (19%). Others 33 (9%) Education Primary/secondary education – 260 (62%) Tertiary education- 43 (20.3%) Amputation level TF/KD- 87 (23.7%) Amputation cause Diabetes/vascular- 59(16%) Cancer- 14 (3.8%) Others 15 (3.9%) Prosthesis user’s – 368(100%) |
Inclusion: Individuals with unilateral and non-congenital amputations as well as those utilizing lower limb prosthetics met the inclusion criteria.
Exclusion: After amputation, participants in gait training, limb fitting, or buying a new prosthetic limb were not allowed to participate in the study. |
TAPES
MOS SF-36 |
Cross-sectional study.
|
• QoL is significantly influenced by the adjustments made to a prosthetic limb and amputation.
• Physical and mental quality of life is impacted by residual stump pain and phantom limb discomfort. |
The study demonstrates how knowledge about amputation and prosthetic limb adjustments affects the link between sociodemographic and amputation variables and QoL (physical and mental component summary). The use of an artificial limb and amputation adaptations have a major impact on quality of life (QoL). |
| Knežević et al., (April 2015), Serbia/ Medicinski pregled [23]
|
N- 28
Age (Mean)- 65.36 Gender Male- 21(75%) Female- 7 (25%) Marital status- N/S Education- N/S Amputation level- TT-11 (39%) TF- 17 (61%) Amputation cause- DM/Vascular- All Prosthesis user’s – 28 (100%) |
Inclusion-The study involved patients with lower extremituies, walking ability, and at least 6 months of rehabilitation treatment. Control group included lower extremity presence, independent walking, age and gender homogeneity, and two chronic diseases. | RAND- 36 | Cross-sectional
Study. |
• Patients with lower extremity amputations have reduced quality of life.
• Patients with transtibial amputations are more functional and have better health. • SF-36 questionnaire results show differences in physical function and general health.
|
Lower extremity amputees, regardless of gender, exhibit numerous limitations compared to the control group, while those with lower amputee levels have higher physical functioning. |
| Razak et al.,(June 2016), Malaysia/ Procedia – Social and Behavioural Sciences [24]
|
N- 43
Age (Mean)- N/S Gender Male 24 (55.8%) Female 19 (44.2%) Marital Status- Married 33 (76.7%) Unmarried 8 (18.6%) Divorced 2 (4.7%) Education No Education 2 (4.7%) Primary/ Secondary- 35(81.4%) Tertiary 6 (14.0%) Amputation level Transtibial 23 (54.8%) Transfemoral 16 (38.1%) Bilateral 6 (14.0%) Amputation cause- Trauma 14 (33.3%) Infection /Vascular Disease – 24 (57.2%) Congenital 5 (9.5%) Prosthesis user’s-25 (58.1%) |
The study included adult men and women with unilateral or bilateral lower limb amputations who were undergoing post-amputation rehabilitation programs.
|
WHOQOL-Brief
|
cross-sectional study. | • Psychological domain scored highest, followed by social, environmental, and physical.
• Quality of life satisfaction linked to , psychosocial factors and emotional support. • No significant gender difference in quality of life domains among amputees. • Physical domain had the lowest score, while psychological domain scored highest.
|
Malaysian lower limb amputees’ quality of life is satisfactory, with physical health scoring low but still satisfactory, supported by cultural and psychosocial support and rehabilitation facilities. |
| Magnusson et al., (December 2019) India/
Biomedical Centre [25] |
N- 30 (100%)
Age (Mean) –37.5 Gender Male 15(51%) Female- 15 (49%) Marital Status-N/S Education Attended school -26 (88%) Amputation cause- Accident 16 (53.33%) Gangrene 10 (33.33%) Other 4 (13.33%) Amputation types- TT -19 ( 63.33 %) TF – 11 (36.66 % Prosthesis user’s-30 (100%) |
Inclusion- Participants with lower-limb physical disabilities who received prosthetic or orthotic services from Mobility India within the last three years were included in the disability group.
Exclusion A serious mental illness, severe cognitive impairment, blindness, or deafness were the exclusion criteria. The study did not include any staff or students from Mobility India who used orthotic and prosthetic devices. |
WHOQOL-Brief | cross-sectional study | • Physical disability linked to lower QOL in multiple domains.
• Income, education, and living area influence QOL scores. • Urban slum residents face higher risk of low QOL. • Gender, income, and education impact QOL in various domains.
|
The physical, psychological, and environmental domains of quality of life (QOL) are all adversely affected by physical disabilities. Longer education has a beneficial effect on QOL, however income has an impact on QOL in terms of psychology and surroundings. |
| Matos et al., (December 2019), Brazil/ Estudos de psicologia (campinas) [26]
|
N-49
Age (Mean)- 36.4 years Gender Male 29 (59.2%) Female 20 (40.8%) Marital Status Widowed/separated 3 (6.1%) Education High School: 29 (59.2%) University Education 20 (40.8%) Amputation level TF-34 (69.4%) Amputation cause Accidents 20 (40.85) Tumours 16 (32.7%) Congenital /other 13 (27%) Prosthesis user’s-46(94.0%) |
Inclusion-Patients over 18 years old with a lower limb amputation for over six months, wearing prostheses, and being literate. | TAPES-R
MOS SF-36 |
cross-sectional study. | • Better quality of life is predicted by male gender, time since amputation, and below-knee amputations.
• Quality of life linked to pain, prosthesis adaptation, and psychosocial well-being. • Few studies on quality of life in amputees compared to other pathologies.
|
The survey revealed that below-knee amputations, male gender, and time since amputation were predictive with better quality of life and acclimatization to amputation. |
| Alessa et al., (November 2022), Saudi Arbia/ Cureus Inc. [27] | N- 239
Age(Mean)- 37 year Gender Male 167 (69.9%) Female 72 (30.1%) Marital status Married 113 (47.3%) Single 91 (38.1%) Divorced / widow 35 (14.6%) Education- Below secondary/secondary 157 (65.7%) University / above 82(34.3%) Level of amputation- TT-101 (42.3%) TF/KD- 104 (43.6%) Bil.-34 (14.2%) Cause of amputation Trauma- 94 (39.3%) Infection /diabetes/ vascular- 96 (40.2 %) Cancer- 17 (7.1%) Others- 32 (13.4%) Prosthesis user’s Yes- 104 (43.5%) |
The study excluded participants under the age of 18. | TAPES,
Depression, Anxiety, Stress Scale (DASS) Caregiver-Related Questionnaire Zarit Burden Interview (12-item ZBI) and Short-Form Health Survey (SF-12)
|
cross-sectional study. | • Prosthetics users had higher QOL scores than non-users.
• Caregivers experienced varying levels of burden, with 15.1% high burden. • Psychological adjustment and prosthesis satisfaction correlated with QOL dimensions.
|
The study emphasizes the value of psychological assessment and counselling in amputee treatment by finding a link between TAPES and SF-12 PCS and MCS scores. |
| Deepak et al., (March 2023), India/ Cureus [28] | N- 106
Age (Mean)- 40 year Gender- Male-83(78.30%) Female- 23(21.70%) Marital status- N/S Education- Illiterate- 24.99 (23.58%) school- 49.98 (47.16 %) beyond high school- 29.25%, Amputation level- TT- 67 (63.31%) TF- 37 (34.91%) Other- 2 (1.89%) Amputation cause- RTA- 73 (68.87%) DM/PVD-17 (16.04 %) Tumor-9 (8.49%) Other cause-7 (6.60%) Prosthesis user’s- 65 (37.75%) |
Inclusion- The study aims to involve 18+ patients with unilateral lower limb amputation, post-amputation patients over three months, willing to participate and provide informed consent.
Exclusion-Patients with amputation, post-amputations under three months, refusal to participate, hearing, speech, visual function disorders, polytrauma, and psychiatric illness are excluded. |
WHOQOL-Brief
|
cross-sectional study. | • Physical domain most affected, followed by psychological, social, environmental domains.
• Trauma top cause of amputation, followed by diabetes, cancer, vascular disease. • Transtibial amputees more common than transfemoral. • Majority of patients aged 20-39 years.
|
Delays in prosthesis fitment exacerbate amputees’ physical burden, while early prosthesis and psychological counselling can significantly improve their quality of life.
|
| Priyadharshan et al. (Jan-2022), India/ Prosthetics &Orthotics international [29]
|
N- 106
Age (Mean)- 51.42 year Gender- Male-88(83%) Female- 18 (17%) Marital status –N/S Education- N/S Amputation level TT – 71 (67%) TF/KD/FF – 35 (33 % ) Amputation cause- TA- 44 (41.5%) DM/PVD- 61 (57.6 %) Other cause-1 (0.9%) Prosthesis user’s- Yes- 51(48.1%) |
Inclusion: People who have lost a lower limb and are at least eighteen years of age and have had surgery within the last five years are eligible to participate in the survey.
Exclusion: Amputees who suffer from any type of mental illness or chronic diseases such as cancer, AIDS, or kidney problems may have to have several little or major toe amputations. |
WHOQOL-Brief,
TAPES -R
|
cross-sectional study. | • Amputation has a substantial impact on every aspect of life quality.
• QOL is impacted by age, time since amputation, and prosthetic use. • Individuals who use prosthetic devices live far better lives. |
Amputation significantly impacts quality of life (QOL), with age affecting QOL. Age-related QOL decreases, but 48.1% use prosthetic devices, with better QOL. Residual and phantom limb pain prevalent. |
| Abbreviations: N: number of participants; TT: transtibial; TF: transfemoral; Bil: bilateral; KD: knee disarticulation; FF: forefoot; RTA: road traffic accident. DM: diabetes mellitus; Peripheral vascular disease (PVD) QoL: quality of life; RAND-36: Research and Development Corporation Measure of Quality of Life; HRQOL: health-related quality of life; SF-12: 12-item Short Form Survey; WHOQOL-BREF: World Health Organization Quality of Life-BREF; MOS: Medical Outcome Study; TAPES: Trinity Amputation and Prosthetic Experience Scale; PEQ: Prosthetic Evaluation Questionnaire; N/S: not stated; ©: Number of citations | ||||||
This systematic review offers a comprehensive analysis of the demographic and clinical characteristics influencing the quality of life (QoL) among lower limb amputees across diverse geographical regions. The studies underscore the global burden of lower limb amputations and the multifaceted challenges faced by amputees. Notably, the concentration of studies in India reflects regional disparities in research focus and the prevalence of lower limb amputations due to trauma and vascular diseases.
Demographic Characteristics
Age and Gender: The mean age of participants varied widely, highlighting that lower limb amputations affect a broad age spectrum. Predominantly male participants (81.05%) across studies point to gender-specific risks and exposures, particularly to trauma-related injuries. This gender distribution suggests a need for gender-sensitive rehabilitation programs, as men might face different challenges compared to women in adjusting to life post-amputation.
Marital Status: Married individuals consistently reported better QoL compared to their single, divorced, or widowed counterparts. This finding underscores the critical role of social support systems, particularly spousal support, in enhancing psychological well-being and facilitating rehabilitation. The lack of detailed marital status information in some studies suggests that future research should include more comprehensive demographic data to fully understand the impact of social relationships on QoL (Fortington et al., 2013; Knežević et al., 2015; Magnusson et al., 2019; Priyadharshan et al., 2022; K et al., 2023).
Educational Background: Higher educational levels were associated with better QoL, likely due to improved access to healthcare resources, better understanding of rehabilitation processes, and enhanced socioeconomic status. This relationship indicates the importance of educational interventions in rehabilitation programs, helping amputees leverage their knowledge and skills to navigate post-amputation life more effectively.
Clinical Characteristics: Causes and Levels of Amputation: Etiology: The primary causes of amputation included trauma, diabetes, and peripheral vascular disease (PVD), with trauma being the most prevalent. This reflects the higher incidence of accidents and injuries in developing regions, particularly in India(Pooja and Sangeeta, 2013b). Understanding the aetiology is crucial for developing targeted prevention strategies and tailored rehabilitation programs that address the specific needs of different patient groups (Kumar and Kumar Yadav, 2022; Dean, 2009).
Amputation Levels: Transtibial amputations (below-knee) were more common than transfemoral amputations (above-knee). This distinction is significant because transtibial amputees generally experience better functional outcomes, including greater mobility and ease of prosthetic use. These findings highlight the importance of tailoring rehabilitation programs to the specific amputation level to maximize functional recovery and QoL.
Prosthetic Use and Quality of Life: Prosthetic Utilization: Approximately 60.83% of participants used prosthetic devices, indicating their critical role in enhancing mobility and overall QoL. However, a significant proportion of amputees did not use prosthetics due to issues such as stump pain, mechanical problems, and psychological barriers. This underscores the need for improving prosthetic technology and addressing psychological factors to enhance prosthetic adoption and effectiveness.
Psychosocial Factors: Emotional support, social integration, and psychological counselling emerged as vital components for successful rehabilitation. Studies consistently highlighted the impact of psychosocial factors, such as depression, anxiety, and phantom limb pain, on QoL. Addressing these issues through comprehensive rehabilitation programs that include psychological support can significantly improve outcomes for amputees(Marques, Journal and 2025, no date).
Assessment Tools: The use of various QoL assessment tools, such as the SF-36, WHOQOL-BREF, and TAPES, reflects the multidimensional nature of QoL among amputees. These tools measure physical, psychological, and social domains, providing a holistic view of the impact of amputation on patients. The widespread use of these validated tools underscores their reliability and importance in assessing rehabilitation outcomes (Stanciu et al., no date; Balk et al., 2019)
Key Findings from Individual Studies: Deans et al. (2008) emphasized the importance of social relationships and psychological well-being, finding strong correlations between social elements and QoL scores, underscoring the role of social support in rehabilitation (Deans, McFadyen and Rowe, 2008). Remes et al. (2010) identified cognitive ability and proper management of pain and comorbidities as crucial for maintaining functional ability and QoL, and linked institutionalization to higher depressive symptoms, suggesting the need for community-based support systems (Remes et al., 2010). Sinha et al. (2011) found that employment status and the use of assistive devices were key determinants of QoL, with factors such as prosthesis use, comorbidities, and pain associated with lower QoL, highlighting the multifaceted challenges faced by amputees (Sinha, Van Den Heuvel and Arokiasamy, 2011). Fortington et al. (2013) reported significant improvements in QoL over time, particularly within the first six months post-amputation, though physical function remained below population norms, indicating the need for ongoing support and interventions (Fortington et al., 2013). Matos et al. (2019) demonstrated that better QoL was predicted by male gender, time since amputation, and below-knee amputations, with pain, prosthesis adaptation, and psychosocial well-being being significant factors influencing QoL(Matos, Naves and de ARAUJO, 2020).
Implications for Clinical Practice, Rehabilitation Programs: Effective rehabilitation programs must address both physical and psychological aspects of recovery. Ensuring access to high-quality prosthetic devices, proper fitting, and alignment is crucial. Additionally, integrating psychological counselling and social support services can significantly enhance QoL outcomes for amputees (Shehata et al., 2025).
Educational Interventions: Increasing awareness and education about the importance of prosthetic use and psychological support among amputees and their families can improve rehabilitation outcomes. Tailored educational programs can help patients understand and manage the challenges associated with lower limb amputation.
Policy and Healthcare Services: Policymakers should focus on improving access to prosthetic devices and rehabilitation services, particularly in regions with high rates of trauma-related amputations. Developing comprehensive healthcare policies that address the physical, psychological, and social needs of amputees can enhance their overall well-being (Asano et al., 2008; Baars et al., 2018).
Future Research Directions: Longitudinal Studies: There is a need for more longitudinal studies to track changes in QoL over time and understand the long-term impacts of amputation and prosthetic use. Such studies would provide deeper insights into the rehabilitation process and the evolving needs of amputees.
Regional and Cultural Diversity: Expanding research to include diverse geographical and cultural contexts can help identify unique challenges and best practices globally. This approach would ensure that rehabilitation strategies are inclusive and tailored to the needs of amputees worldwide.
Advanced Prosthetic Technologies: Research into advanced prosthetic technologies and their impact on QoL can provide valuable information for improving prosthetic design and functionality. Innovations in prosthetic technology can significantly enhance mobility and overall QoL for amputees.
CONCLUSION
Lower limb amputations profoundly impact individuals’ physical, psychological, and social well-being. This review highlights the critical factors influencing QoL, including demographic characteristics, cause and level of amputation, prosthetic use, and psychosocial support. Effective rehabilitation must address these multifaceted needs, ensuring that amputees receive comprehensive care to enhance their overall quality of life. Future research should focus on long-term outcomes and include a broader range of geographical and cultural contexts to develop globally applicable rehabilitation strategies.By understanding the diverse factors influencing QoL among lower limb amputees, healthcare providers and policymakers can develop more effective, targeted interventions that address the unique needs of this population, ultimately improving their rehabilitation outcomes and overall quality of life.
Declaration of interest: The authors disclose no conflicts of interest. The format and contents of the paper are solely the responsibility of the authors.
Data Availability: Data are available with the corresponding author on reasonable request
Funding: The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
ACKNOWLEDGEMENTS
We appreciate the School of Life Sciences at Singhania University for giving us the resources we needed. We would also like to express our gratitude to Radhakrishnan Unnikrishnan and Faizan Zaffar Kashoo for their valuable comments and discussions on the manuscript. Thank you very much to Shivam Mishra, Singhania University, for providing technical support.
REFERENCES
Alessa, M. Et Al. (2022) “The Psychosocial Impact Of Lower Limb Amputation On Patients And Caregivers,” Cureus [Preprint]. Available At: Https://Doi.Org/10.7759/Cureus.31248.
Asano, M. Et Al. (2008) “Predictors Of Quality Of Life Among Individuals Who Have A Lower Limb Amputation,” Prosthetics And Orthotics International, 32(2), Pp. 231–243. Available At: Https://Doi.Org/10.1080/03093640802024955.
Baars, E.C. Et Al. (2018) “Prosthesis Satisfaction In Lower Limb Amputees: A Systematic Review Of Associated Factors And Questionnaires,” Medicine (United States). Lippincott Williams And Wilkins. Available At: Https://Doi.Org/10.1097/Md.0000000000012296.
Balk, E.M. Et Al. (2019) “Psychometric Properties Of Functional, Ambulatory, And Quality Of Life Instruments In Lower Limb Amputees: A Systematic Review,” Archives Of Physical Medicine And Rehabilitation. W.B. Saunders, Pp. 2354–2370. Available At: Https://Doi.Org/10.1016/J.Apmr.2019.02.015.
Baru, R. V And Nundy, M. (2020) “History And Characteristics Of Public Private Partnerships (Ppps) In The Health Service System In India,” In Critical Reflections On Public Private Partnerships. Routledge, Pp. 179–213.
Brunelli, S. Et Al. (2020) “A Literature Review Of The Quality Of Life, Health Status And Prosthesis Satisfaction In Older Patients With A Trans-Tibial Amputation,” Canadian Prosthetics & Orthotics Journal, 2(1).
Butler, A. Et Al. (2000) “A Guide To Writing A Qualitative Systematic Review Protocol To Enhance Evidence‐Based Practice In Nursing And Health Care,” Wiley Online Library, 13(3), Pp. 241–249. Available At: Https://Doi.Org/10.1111/Wvn.12134.
Condie, E. Et Al. (2006) Lower Limb Prosthetic Outcome Measures: A Review Of The Literature 1995 To 2005. Available At: Http://Journals.Lww.Com/Jpojournal.
“Critical Appraisal Skills Programme. Casp” (No Date).
Dadematthews, O.D. (2022) “Quality Of Life, Functional Performance, And User Satisfaction Of Lower Limb Prosthesis Clients.” Auburn University.
Davie-Smith, F. Et Al. (2017) “Factors Influencing Quality Of Life Following Lower Limb Amputation For Peripheral Arterial Occlusive Disease: A Systematic Review Of The Literature,” Prosthetics And Orthotics International, 41(6), Pp. 537–547.
Day, J.D. Et Al. (2023) “Determinants Of Healing And Readiness For Prosthetic Fitting After Transtibial Amputation: Integrative Literature Review,” Prosthetics And Orthotics International, 47(1), Pp. 43–53.
Day, M.C., Wadey, R. And Strike, S. (2019) “Living With Limb Loss: Everyday Experiences Of ‘Good’ And ‘Bad’ Days In People With Lower Limb Amputation,” Disability And Rehabilitation, 41(20), Pp. 2433–2442.
Dean, E. (2009) “Physical Therapy In The 21st Century (Part I): Toward Practice Informed By Epidemiology And The Crisis Of Lifestyle Conditions,” Physiotherapy Theory And Practice, 25(5–6), Pp. 330–353. Available At: Https://Doi.Org/10.1080/09593980802668027.
Deans, S.A., Mcfadyen, A.K. And Rowe, P.J. (2008) “Physical Activity And Quality Of Life: A Study Of A Lower-Limb Amputee Population,” Prosthetics And Orthotics International, 32(2), Pp. 186–200. Available At: Https://Doi.Org/10.1080/03093640802016514.
Fatima, S.Z. (2023) “Life Of An Amputee: Predictors Of Quality Of Life After Lower Limb Amputation,” Wiener Medizinische Wochenschrift, 173(13–14), Pp. 329–333.
Fortington, L. V. Et Al. (2013) “Change In Health-Related Quality Of Life In The First 18 Months After Lower Limb Amputation: A Prospective, Longitudinal Study,” Journal Of Rehabilitation Medicine, Pp. 587–594. Available At: Https://Doi.Org/10.2340/16501977-1146.
Harness, N., Related, M.P.-C.O. And And 2001, Undefined (No Date) “Health Related Quality Of Life In Patients With Dysvascular Transtibial Amputation,” Journals.Lww.Com [Preprint]. Available At: Https://Journals.Lww.Com/Clinorthop/Fulltext/2001/02000/Health_Related_Quality_Of_Life_In_Patients_With.23.Aspx?Casa_Token=R0vvcnuwq7oaaaaa:2tcrjruohe5uozyhcel2kvhynddfutlfymn70zhfydl8b0yijgloxbewq29d4fyqoewwz5vpwm8jmiqhvooteq (Accessed: June 8, 2024).
Havard, H., Trauma, S.G.-O. And And 2025, Undefined (No Date) “Amputations Of The Lower Limb: An Overview Of Principles With Surgical Tips And Advances,” Elsevier [Preprint]. Available At: Https://Www.Sciencedirect.Com/Science/Article/Pii/S1877132725000533 (Accessed: September 1, 2025).
Hays, R.D. And Morales, L.S. (No Date) The Rand-36 Measure Of Health-Related Quality Of Life. Available At: Www.Annrned.Org.
K, D. Et Al. (2023) “Quality Of Life In People With Unilateral Lower Limb Amputation At A Tertiary Rehabilitation Centre In Northern India: A Cross-Sectional Study,” Cureus [Preprint]. Available At: Https://Doi.Org/10.7759/Cureus.36985.
Knežević, A. Et Al. (2015) “Assessment Of Quality Of Life In Patients After Lower Limb Amputation,” Medicinski Pregled, 68(3–4), Pp. 103–108. Available At: Https://Doi.Org/10.2298/Mpns1504103k.
Knight, A.D., Dearth, C.L. And Hendershot, B.D. (2021) “Deleterious Musculoskeletal Conditions Secondary To Lower Limb Loss: Considerations For Prosthesis-Related Factors,” Advances In Wound Care, 10(12), Pp. 671–684.
Kumar, A. And Kumar Yadav, W. (2022) Current Prosthetic And Orthotic Technology: Practices And Challenges Covid-19 Impact On The Rehabilitation Of People With Disabilities Using Prosthetic And Orthotic Devices View Project Current Prosthetic And Orthotic Technology View Project 14. Current Prosthetic And Orthotic Technology: Practices And Challenges. Available At: Https://Orcid.Org/0000-0003-3978-8635;
Kumar, D. Et Al. (2020) “A Demographic Study Of Lower Limb Amputees In A North Indian Tertiary Rehabilitation Center,” Indian Journal Of Physical Medicine & Rehabilitation, 31(1), P. 12.
Magnusson, L. Et Al. (2019) “Quality Of Life Of Prosthetic And Orthotic Users In South India: A Cross-Sectional Study,” Health And Quality Of Life Outcomes, 17(1). Available At: Https://Doi.Org/10.1186/S12955-019-1116-Y.
Marques, L., Journal, L.B.-G.H. And 2025, Undefined (No Date) “Well-Being As A Core Element Of Rehabilitation: Preventing Mental Health Challenges In A Global Context,” Elsevier [Preprint]. Available At: Https://Www.Sciencedirect.Com/Science/Article/Pii/S241464472500003x (Accessed: September 1, 2025).
Matos, D.R., Naves, J.F. And De Araujo, T.C.C.F. (2020) “Quality Of Life Of Patients With Lower Limb Amputation With Prostheses,” Estudos De Psicologia (Campinas), 37. Available At: Https://Doi.Org/10.1590/1982-0275202037e190047.
Mcdonald, C.L. Et Al. (2021) “Global Prevalence Of Traumatic Non-Fatal Limb Amputation,” Prosthetics And Orthotics International, 45(2), Pp. 105–114.
Mohanty, R.K., Mohanty, R.C. And Sabut, S.K. (2020) “A Systematic Review On Design Technology And Application Of Polycentric Prosthetic Knee In Amputee Rehabilitation,” Physical And Engineering Sciences In Medicine, 43(3), Pp. 781–798.
Moher, D. Et Al. (2009) “Preferred Reporting Items For Systematic Reviews And Meta-Analyses: The Prisma Statement,” Annals Of Internal Medicine, 151(4), Pp. 264–269.
Mukundan, H. Et Al. (2020) “Dosimetric And Isocentric Variations Due To Patient Setup Errors In Ct-Based Treatment Planning For Breast Cancer By Electronic Portal Imaging,” Medical Journal Armed Forces India, 76(1), Pp. 51–57.
Neelakantan, M. And Kulkarni, A. (2023) “Unifying India’s Healthcare Markets,” Indian Public Policy Review, 4(4 (Jul-Aug)), Pp. 30–69.
Norvell, D.C. Et Al. (2024) “The Effect Of Prosthetic Limb Sophistication And Amputation Level On Self-Reported Mobility And Satisfaction With Mobility,” Archives Of Physical Medicine And Rehabilitation [Preprint].
Pal, B. (2020) “Role Of Government In Health Care System In India: An Overview,” Academic Discourse, 9(1), Pp. 60–70.
Pattnaik, S. Et Al. (2023) “Prevalence, Pattern And Determinants Of Disabilities In India: Insights From Nfhs-5 (2019–21),” Frontiers In Public Health, 11, P. 1036499.
Polat, C.S. Et Al. (2021) “Factors Related To Phantom Limb Pain And Its Effect On Quality Of Life,” Somatosensory & Motor Research, 38(4), Pp. 322–326.
Pooja, G. Das And Sangeeta, L. (2013b) “Prevalence And Aetiology Of Amputation In Kolkata, India: A Retrospective Analysis,” Hong Kong Physiotherapy Journal, 31(1), Pp. 36–40. Available At: Https://Doi.Org/10.1016/J.Hkpj.2012.12.002.
Poonekar, P.D. And Gupta, P.K. (2022) “Ict And Rehabilitation Engineering: Changing Digits,” In Disability Rehabilitation Management Through Ict. River Publishers, Pp. 189–194.
Priyadharshan, K.P. Et Al. (2022) “Quality Of Life In Lower Limb Amputees: A Cross-Sectional Study From A Tertiary Care Center Of South India,” Prosthetics And Orthotics International, 46(3), Pp. 246–251. Available At: Https://Doi.Org/10.1097/Pxr.0000000000000108.
Rafi, S.H. (2020) “Satisfaction Level Of Lower Limb Prosthesis Users In Community Level After Completing Rehabilitation Protocol In Crp.” Bangladesh Health Professions Institute, Faculty Of Medicine, The University ….
Razak, M.M.A. Et Al. (2016) “Quality Of Life Among Lower Limb Amputees In Malaysia,” Procedia – Social And Behavioral Sciences, 222, Pp. 450–457. Available At: Https://Doi.Org/10.1016/J.Sbspro.2016.05.135.
Remes, L. Et Al. (2010) “Quality Of Life Three Years After Major Lower Extremity Amputation Due To Peripheral Arterial Disease Aging Clinical And Experimental Research,” Aging Clin Exp Res, 22(5), Pp. 395–405. Available At: Https://Doi.Org/10.3275/6712.
Roberts, E. Et Al. (2021) “A Qualitative Study Examining Prosthesis Use In Everyday Life In Individuals With Lower Limb Amputations,” Prosthetics And Orthotics International, 45(4), Pp. 296–303.
Sanders, P. Et Al. (2020) “Narratives Of Recovery Over The First Year After Major Lower Limb Loss,” Qualitative Health Research, 30(13), Pp. 2049–2063.
Shehata, S. Et Al. (2025) “Assessment Of Prosthetic Outcomes, Coping Strategies And Social Support Among Patients With Lower Limb Amputation,” Ejnhs.Journals.Ekb.Eg, 6(2). Available At: Https://Ejnhs.Journals.Ekb.Eg/Article_437715_0b44ae2b9846aa96174f2da95046b61a.Pdf (Accessed: September 1, 2025).
Sindwani, P. Et Al. (2023) “Health Related Quality Of Life And Prosthetic Satisfaction In Unilateral Knee Amputated Patients: A Systematic Review,” Eur J Mol Clin Med, 10(1), Pp. 2419–2433.
Sinha, R. Et Al. (2014) “Influence Of Adjustments To Amputation And Artificial Limb On Quality Of Life In Patients Following Lower Limb Amputation,” International Journal Of Rehabilitation Research, 37(1), Pp. 74–79. Available At: Https://Doi.Org/10.1097/Mrr.0000000000000038.
Sinha, R., Van Den Heuvel, W.J.A. And Arokiasamy, P. (2011) “Factors Affecting Quality Of Life In Lower Limb Amputees,” Prosthetics And Orthotics International, 35(1), Pp. 90–96.
Sinha, R., Van Den Heuvel, W.J.A. And Arokiasamy, P. (2011) “Factors Affecting Quality Of Life In Lower Limb Amputees,” Prosthetics And Orthotics International, 35(1), Pp. 90–96. Available At: Https://Doi.Org/10.1177/0309364610397087.
Sinha, R., Van Den Heuvel, W.J.A. And Arokiasamy, P. (2014) “Adjustments To Amputation And An Artificial Limb In Lower Limb Amputees,” Prosthetics And Orthotics International, 38(2), Pp. 115–121. Available At: Https://Doi.Org/10.1177/0309364613489332.
Stanciu, C. Et Al. (No Date) “Enhancing Quality Of Life In Patients With Acute Wounds: The Synergistic Effects Of Negative Pressure Wound Therapy And Physiotherapy,” Mdpi.Com [Preprint]. Available At: Https://Www.Mdpi.Com/2227-9059/13/4/785 (Accessed: September 1, 2025).
Vieira, W.F. Et Al. (2024) “Neuropathic Pain, Mood, And Stress-Related Disorders: A Literature Review Of Comorbidity And Co-Pathogenesis,” Neuroscience & Biobehavioral Reviews, P. 105673.
Ware, J.E. (2000) “Sf-36 Health Survey Update,” Spine, 25(24), Pp. 3130–3139. Available At: Https://Doi.Org/10.1097/00007632-200012150-00008.
Zaheer, A. Et Al. (2020) “Quality Of Life And Depression Among Lower Limb Amputees,” Annals Of King Edward Medical University, 26(2), Pp. 364–368.


