King Abdulaziz University, Radiation Oncology Department. Jeddah, Saudi Arabia
Corresponding author email: raniahashem@gmail.com
Article Publishing History
Received: 20/10/2020
Accepted After Revision: 12/12/2020
Primary thyroid lymphoma (PTL) is a rare disease, accounting for 5% of all thyroid malignancies. Diffuse B-cell lymphoma (DBCL) is the most common type of PTL, about 50–80% of PTL is DBCL. The case of an 81year-old female, known case of diabetes and heart disease, is presented with large neck mass on the left side, pushing the airway and not associated with B symptoms. On examination, 9 cm neck mass detected on the left side and no cervical lymph nodes. CT scan showed left sizeable soft tissue mass measures 8.7 cm, compressing the trachea. Fine-needle aspiration (FNA) was inconclusive, and the biopsy revealed DBCL, which indicated PTL. PTL originated from B cells, especially DBCL, there is no consensual therapeutic scheme for PTL; each case must be evaluated and treated separately. Treatment included surgery or Radiotherapy to achieve reasonable local disease control, combined with chemotherapy for control spread disease, and improving the outcome. The five-year Over-all survival (OS) for PTL in the literature range from 35% to 100%. PTL considered to be tough to diagnose in the preoperative period; Each case diagnosed with PTL should be evaluated and treated separately, depending on the staging after the diagnosis. Well-organized care and, combined modalities revealed effective management.
Primary Thyroid Lymphoma, Diffuse B-Cell Lymphoma, Radiotherapy, Chemotherapy
Hashem R, Jastaneyah Z, Attar M. Thyroid Lymphoma Treated with Combined Modalities: A Case Report with Literature Review. Biosc.Biotech.Res.Comm. 2020;13(4).
Hashem R, Jastaneyah Z, Attar M. Thyroid Lymphoma Treated with Combined Modalities: A Case Report with Literature Review. Biosc.Biotech.Res.Comm. 2020;13(4). Available from: https://bit.ly/3oLapjH
Copyright © Hashem et al., This is an open access article distributed under the terms of the Creative Commons Attribution License (CC-BY) https://creativecommns.org/licenses/by/4.0/, which permits unrestricted use distribution and reproduction in any medium, provide the original author and source are credited.
INTRODUCTION
Primary thyroid lymphoma (PTL) is an unusual disease; it is mainly occurring in middle age and female predominant (Walsh 2013, Graff-Baker2010). Thyroid malignancies have 5 % PTL; whereas, Extranodal lymphomas have 7 % PTL. (Widder 2004, Stein 2013) B-cell lymphoma (DBCL) is common in PTL; it accounts for 60–80%. (Gupta 2005– Thieblemont 2002, Onal 2011). It is very curable disease, therefore early detection and correct treatment is essential (Gonçalves 2018).In the past, before the introduction of FNA biopsy, surgical resection was the mainstay treatment for thyroid lymphoma (Graff-Baker 2010, Meyer-Rochow 2008). Later the role of surgery has reduced as resection of thyroid is no longer required for diagnosis, histopathological evaluation supplemented by Immunohistochemistry (IHC) is the gold standard for the diagnosis of PTL (Kakkar 2019). It is challenging to diagnose primary thyroid lymphomas because of their rare occurrence (Acar 2109), and its management requires the involvement of an interprofessional team of specialists from different departments (Kesireddy 2020).
Several studies reported improved outcomes in PTL with the combined modality of both radiation and chemotherapy (Vardell2019, Onal 2011, Watanabe 2011).It still remains unclear what optimal treatment methods should be adopted with PTL patients.In this study, we report a case of primary thyroid lymphoma confirmed on histology, presented at the multidisciplinary tumour board at King Abdul-Aziz university hospital in Saudi Arabia and treated by bimodalities chemo-radiotherapy as well we reviewed the relevant literature in order to summarize the management scheme of PTL.
Case Presentation: Eighty-one years old female known case of Diabetes (DM)and, heart disease on medication, there was no family history of thyroid cancer neither previous neck irradiation. She presented with a considerable neck mass on the left side; it was rapidly progressing in size for the last six months, pushing the airway. She complains of dysphagia mainly to solid food; subsequent fine needle aspiration cytology (FNAC) performed from the thyroid gland; and, it was negative for malignancy, followed by Excisional biopsy on 24-2-2018, which showed high-grade B cell lymphoma, consist with DLBCL.Bone marrow biopsy was done on 4-4-2018 and revealed no malignancy.
Diagnostic assessment: Neck ultrasound on 14-2-2018: It showed; enlarged left thyroid lobe; measuring 9.3 x4.6 x 5cm and replaced by a sizeable heterogenous mass with no calcification. The right thyroid lobe appears homogenous, with normal vascularity, no nodules, or masses.
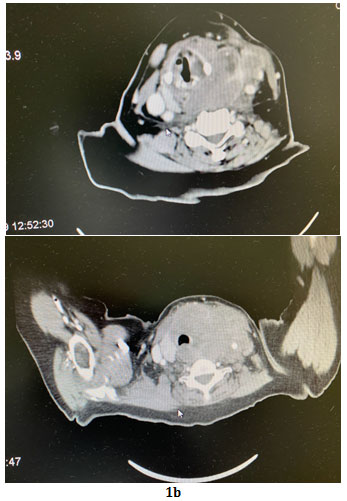
CT Scan of the Neck on 22-2-2018 : It revealed; a large infiltrative left thyroid lobe mass with an area of necrosis. The mass is extending superiorly; to the level of the hyoid bone. It is reaching the thoracic inlet inferiorly by 1.3 cm below the sternal notch. The tumour measured 8×8.7 x6.4 cm.; and compressing the trachea, with narrowest diameter measures 0.9 cm.
Figure 1a and b. No cervical lymph nodes determined in the CT scan.
Figure 1a,1b: Showed an axial neck computed tomography images demonstrate a large ill-defined mass infiltrating the thyroid gland.
Biopsy on 24-2-2018: Showed Diffuse large B-cell lymphoma, the tumour cell CD20 positive and, CD10, CD3 negative. Staging works up (CT chest and abdomen) were negative for metastasis. Although (PET) scan is essential at diagnosis, particularly in patients with (DLBCL), unfortunately, we don’t have a PET scan at our centre.
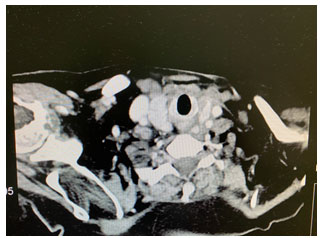
Follow-up and Outcome: The patient received six cycles of chemotherapy (CVP and rituximab), the last chemo was on 23-10-2018 followed by radiotherapy (RT) treatment, a total dose of 36 Gy/18 fractions, 2Gy per fraction, delivered using three‑dimensional conformal Radiotherapy. The clinical target volume (CTV) was encompassing the whole thyroid. The patient completed radiotherapy treatment on 26-12-2018 with no significant toxicity or treatment interruption. On follow up by clinical exam, and computed tomography (CT) scan; we noticed a decrease in size of the neck swelling. CT neck after chemotherapy showed interval disease regression. The mass measured 3.5 cm x 2.5cm. Ultrasound neck on follow up,25-09-2019 showed left thyroid lob measures 1.5 x0.5×1.3 cm. No recurrence or metastasis detected in our case during the follow-up period; we assessed the patient both clinically and radiologically. figure (2).
Figure 2: CT Neck on follow up, showed no recurrence.
DISCUSSION
Typically, the thyroid gland does not include lymphoid tissue and most PTL are non-Hodgkin’s lymphomas, whereas Hodgkin lymphoma and T‑cell NHL are rare, (Chen 2014). PTL is accountable for 2.5% of all lymphomas, (Alzouebi 2012), (Campo 2006). PTL has four types; include diffuse large B-cell lymphoma (DLBCL), marginal zone lymphoma (MALT), follicular lymphoma (FL), and Extranodal small lymphocytic lymphoma, (Derringer 2000).Diffuse B-cell lymphoma (DLBCL) is the most common type of lymphoma in general, (Katna 2013). DLBCL is usually composed of sheets of atypical lymphoid cells has an irregular nuclear membrane, and granular chromatin, with round nucleoli and scant cytoplasm, (Cozzolino 2016).
Several studies have documented that Hashimoto’s thyroiditis (HT) histologically seen in 90% of cases of PTL (Widder 2004), is due to the presence of lymphocytes in HT, and the chronic antigenic stimulation, which predisposes malignant transformation of these lymphocytes, (Green 2006, Kossev 1999). It is very challenging to distinguish Hashimoto’s thyroiditis from PTL on fine-needle aspiration (FNA), (Pasieka 1998 and Chai 2015).
PTL presented as a painless thyroid mass that enlarged and caused symptoms associated with the compression, such as dysphagia, hoarseness of the voice and, dyspnea, (Wirtzfeld 2001). Diffuse neck swelling recognized during the physical examination; neck ultrasound and CT scan. (Katna 2013) Ultrasound is considered an initial diagnostic modality for PTL; By ultrasound findings, PTL can be classified as a nodular, diffuse, or mixed subtype (Ota 2006); however, it is difficult to distinguish PTL from other thyroid diseases. Wang identified in his study that positron emission tomography-computed tomography [PET scan /CT] is a practical image which could distinguish between PTL and chronic thyroiditis, the SUV max was substantially higher; and, the CT density was lower in PTL in comparison with chronic thyroiditis, (Nakadate 2013 Wang 2014).
Ultrasonography plays an important role in monitoring and follow-ups after chemotherapy in patients with PTL, (Li 2019). The gold standard for diagnosing PTL depends on biopsy, which has higher diagnostic accuracy, and the management depended on histology, patient performance status, and co-morbidities (Sharma 2016). Fine‑needle aspiration (FNA) has an essential role in diagnosing PTL, with an accuracy of 25%–90% (Gupta 2005, Nguyen 2005). Still, it has a limited effect to differentiate between thyroid lymphoma, and thyroiditis, which results in increased false‑negative outcomes from sampling error. Sangelli et al documented 4 out of 10 cases MALT thyroid lymphomas discovered by using FNA biopsy in comparison to six out of 7 cases of thyroid DLBCL. (Sangalli et al 2001). Core biopsy is more sensitive than FNA, and still required for confirming the definitive diagnosis of PTL(Vigliar 2013, Sarinah 2010).
Further testing is needed such as flow cytometry, which examines CD markers and improves sensitivity and specificity; (Adhikari 2015). DLBCL has negative CD19-, CD20-and positive CD45-; while MALT lymphoma has CD5-, CD10-, and CD23-negative; and CD19+, CD20+, (Higgins 2008). Recently a study by Travaglino et al identified clinical features associated with high pathological grade in primary thyroid lymphoma includes Age≤55, female sex, lymph node involvement, compressive symptoms and absence of lymphocytic thyroiditis (Travaglino et al., 2020). Once the PTL diagnosis is confirmed by otolaryngologist and the pathologist, the radiation, medical oncologist, and an endocrinologist should participate in the case; further workup and treatment should begin immediately, (Kesireddy 2020).
Treatment option includes surgery, radiotherapy, chemotherapy, and combination treatment with chemotherapy and radiotherapy, (Foppiani 2009). No significant prospective studies are showing the therapeutic approach of PTL; most physicians intend to do multidisciplinary loom. The management of patients with PTL varies according to histology and the stage of the disease; therefore, the concern, in this case, was to differentiate PTL from secondary thyroid lymphoma (STL). The primary thyroid lymphoma common in females, occurs in older women between 6-7th decades, (Pedersen1996). Patient presented with rapidly enlarged painless mass that associated with cough, hoarseness, dysphagia, dyspnea, and pressure symptoms, (Derringer2000). Where as the secondary thyroid lymphoma it occurs in the middle-aged population around 42 years, mostly disseminated disease metastasized to the thyroid and has a higher mortality rate in contrasting with primary thyroid lymphoma which occurs in early stages disease, (Takashima 2000).
The majority of cases diagnosed with stage IE (30–66%) or stage IIE (25%–66%).(Graff-Baker 2010, Stein2013,, Onal 2011, Campo2006, Watanabe2011). Only 20 % present with advanced stage IIIE and IVE disease.The staging of PTL performed according to Ann-Arbor classification. (Table 1)(Carbone 1971). Our patient staged as 1E with no B symptoms and Lymphoma International Prognostic Index (IPI) Score=1, ( Amy2020).
Table 1. Ann-Arbor classification
Stage 1E Confined to the thyroid gland
Stage 2E Locoregional lymph node involvement in addition to
thyroid gland
Stage 3E Involvement of lymph nodes located on both sides of
the diaphragm
Stage 4E Disseminated disease
A: Absence of symptoms
B: At least 10% body weight loss over six months, fever without an infection over 38 degrees, recurrent night sweating.
PTL is highly sensitive to radiation; it is responding rapidly to combined modalities with induction chemotherapy followed by involved-field radiotherapy. (Alzouebi2012, Yahalom2015).RT dose, treatment field, and technique vary, the doses range from 36Gy to 45Gy depends on volume and residual post-chemotherapy and the intent of treatment. (Yahalom2015, Kakkar 2019). They used involved field by including the whole thyroid with or without regional lymph nodes, either with 3D conformal, or intensity-modulated radiotherapy (IMRT). In our case, 36Gy used as the patient was elderly.The chemotherapy that used are usually the same chemo as in Non-Hodgkin Lymphoma, CVP (cyclophosphamide, vincristine, prednisolone), and;CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisolone), and R-CHOP. (Miller1998). Rituximab is immunotherapy (monoclonal antibody) agent which often added to chemotherapy, acts against CD20, and showing a promising result in managements of DLBCL in the form of improved disease-free and overall survival, (Nakadate 2013, Coiffier 2002, Pavlidis 2019).
Our patient received six cycles of chemotherapy (CVP and rituximab); since she had a cardiac disease, and CHOP is known to induce cardiotoxicity in elderly patients who appeared to be at higher risk, (Limat 2003). Several studies have reported that PTL has an excellent prognosis when treated with combined modality, 5-year OS, and DFS in Ha et al. was 64% and 76%, (Ha et al 2001). Further literature by Matsuzuka et al.; reported eight-year over-all survival (OS) 100%for patients who treated with chemo and, radiation, (Matsuzuka et al 1993). Doria et al.; showed that combined therapy had significant improvement in local control over a single modality treatment (surgery, radiotherapy, and chemotherapy) and lowered the relapse rate, (Doria et al., 1994).
The majority of the literature on PTL presented as case series and case reports, with paucity of retrospective studies for this disease. However recently the National Cancer Database (NCDB) reported a large retrospective study on PTL; the results showed patients who were treated with multiagent chemotherapy, have the best survival of all treatment modalities. Surgical resection and radiation therapy both show a significant survival benefit, (Vardell, 2019).The prognosis of PTL determined by disease subtype and histology. (Sakorafas 2010) There are several factors predict a worse prognosis in PTL, includes, age greater than 80 years, advanced stage, size of the tumor more than 10 cm, rapid tumor growth, (mediastinal do worse), and elevated LDH, (Tupchong1986, Aozasa 1986 Onal 2011, Kesireddy 2020).
We calculated the International Prognostic Index (IPI)score for this patient and, it was 1, 4-year progression-free survival is 80 %.( Sehn 2007).The life expectancy for DLBCL in 5 years is 75% and in MALT lymphoma is 96 %. The recurrence classically appears within the first four years. Life expectancy by stage in five years is 86% for stage 1E, stage 2E is 81 %, and 64% for stage 3E-4E (Graff-Baker 2010). A study by Vardel et al. (2019) revealed that the median survival of PTL is 11.6 years and, five years overall survival (OS) is 75%. Although the rarity of PTL; it considered to be a curable condition with any histological subtype. Rituximab provided an excellent outcome in most cases; our patient achieved a complete response with no complication, (Coiffier 2002).Our case also showed that tissue biopsy was the tool for the confirmation of PTL, which revealed DBCL in-addition to the clinical presentation and, the-radiological features of PTL, while FNA was negative for malignancy. PTL is easily misdiagnosed therefore, it’s very necessary to analyze the diagnosis methods and treatment strategy of PTL to clarify the guide of diagnosis and treatment, (Wang 2020).
CONCLUSION
Primary thyroid lymphoma is an uncommon disease and considered to be tough to diagnose in the preoperative period; however, it is curable with suitably overall survival. Each case diagnosed with PTL should be evaluated and treated separately, depending on the staging after the diagnosis, which influences the treatment. Our case report revealed effective management with combined multiagent chemotherapy and radiotherapy treatment. PTL has a good prognosis if the patient received well-organized care from all the specialists promptly.In the future, extensive studies are required to standardize the therapeutic approach; and establish ideal PTL treatment guidelines, furthermore we should consider comparing treatment modalities of chemotherapy alone vs chemoradiation.
Ethical approval: This is a case report, without clinical research involved.
Funding: The authors declare that there were no sources of funding.
Author Contribution: All authors contributed to the content of this manuscript: M. Attar reviewed the manuscript; R. Hashem collected the data for the case report; and wrote the manuscript; Z.Jastaneyah collected the data for radiotherapy.
Conflicts of Interest: The authors declare that they have no conflict of interest.
REFERENCES
Acar N, Acar T, Avcı A, Haciyanlı M. (2019)Approach to primary thyroid lymphoma: case series. Turk J Surg. Jun 13;35(2):142-145. doi: 10.5578/turkjsurg.4132. PMID: 32550320; PMCID: PMC6796069
Adhikari LJ, Reynolds JP, Wakely PE Jr.(2015)Multi-institutional study of fine-needle aspiration for thyroid lymphoma..J Am Soc Cytopathol. 2016 May-Jun;5(3):170-176. doi: 10.1016/j.jasc..11.002. Epub 2015 Nov 11.PMID: 31042520
Amy S Ruppert , Jesse G Dixon , Gilles Salles , Anna Wall David Cunningham , Viola Poeschel , Corinne Haioun (2020) Norbert Schmitz International prognostic indices in diffuse large B-cell lymphoma: a comparison of IPI, R-IPI, and NCCN-IPI Blood Jun 4;135(23):2041-2048.doi: 10.1182/blood.2019002729.
Aozasa K, Inoue A, Tajima K, Miyauchi A, Matsuzuka F, Kuma K.(1986) Malignant lymphomas of the thyroid gland: Analysis of 79 patients with emphasis on histologic prognostic factors. Cancer [Internet]. [cited 2020 Apr 19];58(1):100–4. Available from:https://acsjournals.onlinelibrary.wiley.com/doi/abs/10.1002/1097-0142%2819860701%295
Alzouebi M, Goepel JR, Horsman JM, Hancock BW. (2012).Primary thyroid lymphoma: the 40 year experience of a UK lymphoma treatment centre. Int J Oncol. Jun;40(6):2075–80.
Campo E, Chott A, Kinney MC, Leoncini L, Meijer CJLM, Papadimitriou CS, et al.(2006) Update on extranodal lymphomas. Conclusions of the Workshop held by the EAHP and the SH in Thessaloniki, Greece. Histopathology. Apr;48(5):481–504.
Carbone PP, Kaplan HS, Musshoff K, Smithers DW, Tubiana M.(1971) Report of the Committee on Hodgkin’s Disease Staging Classification. Cancer Res. Nov;31(11):1860–1.
Chai YJ, Hong JH, Koo DH, Yu HW, Lee J-H, Kwon H, et al.(2015) Clinicopathological characteristics and treatment outcomes of 38 cases of primary thyroid lymphoma: a multicenter study. Ann Surg Treat Res. Dec;89(6):295–9.
Chen C, Yang Y, Jin L, Dong L, Zhang X, Xiang Y.(2014) Primary thyroid T-lymphoblastic lymphoma: a case report and review of the literature. Int J Clin Exp Pathol.;7(1):443–50.
Coiffier B, Lepage E, Briere J, Herbrecht R, Tilly H, Bouabdallah R, et al.(2002) CHOP chemotherapy plus rituximab compared with CHOP alone in elderly patients with diffuse large-B-cell lymphoma. N Engl J Med. Jan 24;346(4):235–42
Cozzolino I, Varone V, Picardi M, Baldi C, Memoli D, Ciancia G, et al.(2016) CD10, BCL6, and MUM1 expression in diffuse large B-cell lymphoma on FNA samples. Cancer Cytopathol. Feb;124(2):135–43.
Derringer GA, Thompson LD, Frommelt RA, Bijwaard KE, Heffess CS, Abbondanzo SL. (2000)Malignant lymphoma of the thyroid gland: a clinicopathologic study of 108 cases. Am J Surg Pathol. May;24(5):623–39.
Doria R, Jekel JF, Cooper DL. (1994) Thyroid lymphoma. The case for combined modality therapy. Cancer. Jan 1;73(1):200–6.
Foppiani L, Secondo V, Arlandini A, Quilici P, Cabria M, Del Monte P.(2009) Thyroid lymphoma: a rare tumor requiring combined management. Horm Athens Greece. Sep;8(3):214–8.
Gonçalves M, Gaspar E, Santos L, Carvalho A. (2018) When a Goitre is a Thyroid Lymphoma. Eur J Case Rep Intern Med. Dec 27;5(12):000999. doi: 10.12890/2018_000999. PMID: 30756001; PMCID: PMC6346969.
Graff-Baker A, Sosa JA, Roman SA.(2010) Primary thyroid lymphoma: a review of recent developments in diagnosis and histology-driven treatment. Curr Opin Oncol. Jan;22(1):17–22.
Green LD, Mack L, Pasieka JL.(2006) Anaplastic thyroid cancer and primary thyroid lymphoma: a review of these rare thyroid malignancies. J Surg Oncol. Dec 15;94(8):725–36.
Gupta N, Nijhawan R, Srinivasan R, Rajwanshi A, Dutta P, Bhansaliy A, et al.(2005) Fine needle aspiration cytology of primary thyroid lymphoma: a report of ten cases. CytoJournal. Dec 9;2:21. .
Ha CS, Shadle KM, Medeiros LJ, Wilder RB, Hess MA, Cabanillas F, et al.(2001) Localized non-Hodgkin lymphoma involving the thyroid gland. Cancer. Feb 15;91(4):629–35.
Higgins RA, Blankenship JE, Kinney MC.(2008) Application of immunohistochemistry in the diagnosis of non-Hodgkin and Hodgkin lymphoma. Arch Pathol Lab Med. Mar;132(3):441–61.
Kakkar A, Purkait S, Agarwal S, Mallick S, Gogia A, Karak AK, Sharma MC, Julka PK. (2019)Primary thyroid lymphoma: A series from a tertiary care center in Northern India. J Cancer Res Ther. Jul-Sep;15(3):669-675. doi: 10.4103/jcrt.JCRT_135_17. PMID: 31169238.
Katna R, Shet T, Sengar M, Menon H, Laskar S, Prabhash K, et al.(2013) Clinicopathologic study and outcome analysis of thyroid lymphomas: experience from a tertiary cancer center. Head Neck. Feb;35(2):165–71
Kesireddy M, Lasrado S.(2020) Thyroid Lymphoma. 2020 Sep 8. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; Jan–. PMID: 31335002.
Kossev P, Livolsi V. (1999)Lymphoid lesions of the thyroid: review in light of the revised European-American lymphoma classification and upcoming World Health Organization classification. Thyroid Off J Am Thyroid Assoc. Dec;9(12):1273–80.
Li P, Zhang H. (2019)Ultrasonography in the Diagnosis and Monitoring of Therapy for Primary Thyroid Lymphoma. Ultrasound Q. Sep;35(3):246-252. doi: 10.1097/RUQ.0000000000000414. PMID: 30601440.
Limat S, Demesmay K, Voillat L, Bernard Y, Deconinck E, Brion A, Sabbah A, Woronoff-Lemsi MC, Cahn JY. (2003)Early cardiotoxicity of the CHOP regimen in aggressive non-Hodgkin’s lymphoma. Ann Oncol. Feb;14(2):277-81. doi: 10.1093/annonc/mdg070. PMID: 12562656.
Matsuzuka F, Miyauchi A, Katayama S, Narabayashi I, Ikeda H, Kuma K, et al. (1993) Clinical aspects of primary thyroid lymphoma: diagnosis and treatment based on our experience of 119 cases. Thyroid Off J Am Thyroid Assoc.;3(2):93–9.
Meyer-Rochow GY, Sywak MS, Reeve TS, et al.(2008): Surgical trends in the management of thyroid lymphoma. Eur J Surg Oncol. 34:576-580.
Miller TP, Dahlberg S, Cassady JR, Adelstein DJ, Spier CM, Grogan TM, et al.(1998) Chemotherapy alone compared with chemotherapy plus radiotherapy for localized intermediate- and high-grade non-Hodgkin’s lymphoma. N Engl J Med. Jul 2;339(1):21–6.
Nakadate M, Yoshida K, Ishii A, Koizumi M, Tochigi N, Suzuki Y, et al.(2013) Is 18F FDG PET/CT useful for distinguishing between primary thyroid lymphoma and chronic thyroiditis? Clin Nucl Med. Sep;38(9):709–14.
Nguyen G-K, Lee MW, Ginsberg J, Wragg T, Bilodeau D.(2005) Fine-needle aspiration of the thyroid: an overview. CytoJournal. Jun 29;2(1):12.
Onal C, Li YX, Miller RC, Poortmans P, Constantinou N, Weber DC, et al.(2011) Treatment results and prognostic factors in primary thyroid lymphoma patients: a rare cancer network study. Ann Oncol Off J Eur Soc Med Oncol. Jan;22(1):156–64.
Ota H, Ito Y, Matsuzuka F, et al.(2006) Usefulness of ultrasonography for diagnosis of malignant lymphoma of the thyroid. Thyroid.;16:983–987.
Pasieka JL. (1998) Anaplastic cancer, lymphoma, and metastases of the thyroid gland. Surg Oncol Clin N Am. Oct;7(4):707–20.
Pavlidis ET, Pavlidis TE. A Review of Primary Thyroid Lymphoma:(2019) Molecular Factors, Diagnosis and Management. J Investig Surg Off J Acad Surg Res. Mar;32(2):137–42.
Pedersen RK, Pedersen NT.(1996) Primary non-Hodgkin’s lymphoma of the thyroid gland: a population based study. Histopathology. Jan;28(1):25-32.
Sakorafas GH, Kokkoris P, Farley DR.(2010) Primary thyroid lymphoma (correction of lympoma): diagnostic and therapeutic dilemmas. Surg Oncol. Dec;19(4):e124-129.
Sangalli G, Serio G, Zampatti C, Lomuscio G, Colombo L.(2001) Fine needle aspiration cytology of primary lymphoma of the thyroid: a report of 17 cases. Cytopathol Off J Br Soc Clin Cytol. Aug;12(4):257–63.
Sarinah B, Hisham A-N.(2010) Primary lymphoma of the thyroid: diagnostic and therapeutic considerations. Asian J Surg. Jan;33(1):20–4.
Sehn LH, Berry B, Chhanabhai M, Fitzgerald C, Gill K, Hoskins P, Klasa R, Savage KJ, Shenkier T, Sutherland J, Gascoyne RD, Connors JM. (2007)The revised International Prognostic Index (R-IPI) is a better predictor of outcome than the standard IPI for patients with diffuse large B-cell lymphoma treated with R-CHOP. Blood. 109(5):1857-61.
Sharma A, Jasim S, Reading CC, Ristow KM, Villasboas Bisneto JC, Habermann TM, Fatourechi V, Stan M.(2016) Clinical Presentation and Diagnostic Challenges of Thyroid Lymphoma: A Cohort Study. Thyroid. Aug;26(8):1061-7.
Stein SA, Wartofsky L.(2013) Primary thyroid lymphoma: a clinical review. J Clin Endocrinol Metab. Aug;98(8):3131–8.
Takashima S, Takayama F, Momose M, Shingu K, Sone S.(2000) Secondary malignant lymphoma which simulated primary thyroid cancer. Clin Imaging. Jun;24(3):162–5.
Thieblemont C, Mayer A, Dumontet C, Barbier Y, Callet-Bauchu E, Felman P, et al.(2002) Primary thyroid lymphoma is a heterogeneous disease. J Clin Endocrinol Metab.;87(1):105–11
Travaglino A, Pace M, Varricchio S, Insabato L, Picardi M, Severino A, Pane F, Staibano S, Mascolo M (2020) Clinical features associated with high pathological grade in primary thyroid lymphoma. Pathol Res Pract 216(3):152819
Tupchong L, Hughes F, Harmer CL.(1986) Primary lymphoma of the thyroid: Clinical features, prognostic factors, and results of treatment. Int J Radiat Oncol • Biol • Phys [Internet]. Oct 1 [cited 2020 Apr 19];12(10):1813–21. Available from: https://www.redjournal.org/article/0360-3016(86)90324-X/abstract
Vardell V A, Ermann D A, Griffin E K, et al. (2019) Primary Thyroid Lymphoma: An Analysis of the National Cancer Database . Cureus 11(2): e4088. doi:10.7759/cureus.4088
Vigliar E, Caleo A, Vitale M, Di Crescenzo V, Garzi A, Zeppa P.(2013) Early cytological diagnosis of extranodal stage I, primary thyroid Non-Hodgkin lymphoma in elderly patients. Report of two cases and review of the literature. BMC Surg.;13 Suppl 2:S49
Walsh S, Lowery AJ, Evoy D, McDermott EW, Prichard RS.(2013) Thyroid lymphoma: recent advances in diagnosis and optimal management strategies. The Oncologist. 18(9):994–1003.
Wang J-H, Chen L, Ren K.(2014) Identification of primary thyroid lymphoma with medical imaging: A case report and review of the literature. Oncol Lett. Dec;8(6):2505–8.
Wang Y, Wang S, Liu Z, Liao Q, Chen G, Xu X. (2020)Diagnosis methods and treatment strategy for primary thyroid lymphoma: a retrospective analysis of 41 cases in China. Eur J Cancer Prev. Aug 14. doi: 10.1097/CEJ.0000000000000599. Epub ahead of print. PMID: 32809992.
Watanabe N, Noh JY, Narimatsu H, Takeuchi K, Yamaguchi T, Kameyama K, et al.(2011) Clinicopathological features of 171 cases of primary thyroid lymphoma: a long-term study involving 24553 patients with Hashimoto’s disease. Br J Haematol. 2011 Apr;153(2):236–43.
Widder S, Pasieka JL.(2004) Primary thyroid lymphomas. Curr Treat Options Oncol. Aug;5(4):307–13.
Wirtzfeld DA, Winston JS, Hicks WL, Loree TR.(2001) Clinical presentation and treatment of non-Hodgkin’s lymphoma of the thyroid gland. Ann Surg Oncol. May;8(4):338–41.
Yahalom J, Illidge T, Specht L, Hoppe RT, Li Y-X, Tsang R, et al. (2015) Modern radiation therapy for extranodal lymphomas: field and dose guidelines from the International Lymphoma Radiation Oncology Group. Int J Radiat Oncol Biol Phys. May 1;92(1):11–31.