1Lecturer, Department of Neurodevelopmental Sciences, National Institute of Speech and Hearing, NISH Road, Aakkulam, Trivandrum, Kerala, India
2Lecturer, Department of Audiology and Speech Language Pathology, National Institute of Speech and Hearing, NISH Road, Aakkulam, Trivandrum, Kerala, India
Corresponding author email: vrinda@nish.ac.in
Article Publishing History
Received: 08/12/2020
Accepted After Revision: 18/03/2021
Tele-rehabilitation is the application of telecommunications technology for the delivery of speech language pathology and audiology services at a distance by linking clinician to client or clinician to clinician for assessment, intervention, and/or consultation. It is an emerging field, but due to the lack of trained professionals, the number of professionals providing tele-rehabilitation in Kerala is few in number. The outbreak of the pandemic COVID 19 has forced the speech language pathologists (SLPs) to shift from the traditional face to face therapy to tele-rehabilitation which was a new experience for most of the speech language pathologists. The present study aimed to understand the challenges faced by the speech language pathologists to provide tele-rehabilitation services to the clients during the outbreak of pandemic COVID-19 and how they overcome those barriers using a self- rated questionnaire developed.
The questionnaire was sent to speech language pathologists through mail and WhatsApp. 105 speech language pathologists responded. Among them, 77 speech language pathologists provided tele-rehabilitation and served clients of all ages and different disorders with language disorder being the most common and dysphagia and apraxia being the least served client population. Tele-rehabilitation was found to be a viable form of service delivery in the field of speech language Pathology. All possibilities of Information and Communication Technology (ICT) were utilized by the SLPs to provide the best services despite the lack of training and non-availability of resources. This survey depicts the need for publishing standard guidelines for providing tele-rehabilitation services and also it emphasizes the need for improved infrastructure and training to professionals to ensure quality services to their clients.
COVID 19, Kerala, Speech Language Pathology, Tele-rehabilitation
Vrinda R, Reni P. S. Survey Based Analysis of Tele-Rehabilitation in the Field of Speech Language Pathology During COVID 19 Outbreak in Kerala. Biosc.Biotech.Res.Comm. 2021;14(1).
Vrinda R, Reni P. S. Survey Based Analysis of Tele-Rehabilitation in the Field of Speech Language Pathology During COVID 19 Outbreak in Kerala. Biosc.Biotech.Res.Comm. 2021;14(1). Available from: <a href=”https://bit.ly/3bnt8go“>https://bit.ly/3bnt8go</a>
Copyright © This is an Open Access Article distributed under the Terms of the Creative Commons Attribution License (CC-BY). https://creativecommons.org/licenses/by/4.0/, which permits unrestricted use distribution and reproduction in any medium, provided the original author and sources are credited.
INTRODUCTION
COVID-19 is a disease caused by a new strain of coronavirus. ‘CO’ stands for Formerly, this disease was referred to as ‘2019 novel coronavirus’ or ‘2019-nCoV.’With the outbreak of pandemic COVID 19, social distancing is practiced all over the world to prevent the spread of the disease. This has led to the exploration of the possibilities of technology in almost every aspect of life. Tele-rehabilitation refers to the use of Information and Communication Technologies (ICT) to provide rehabilitation services to people remotely in their homes or other environments (Brennan et al., 2009; World Health Organization, 2020).
Telepractice in speech language pathology is the application of telecommunications technology to the delivery of speech language pathology and audiology professional services at a distance by linking clinician to client or clinician to clinician for assessment, intervention, and/or consultation (ASHA, 2005a; World Health Organization, 2020). The Special Group Interest (SIG) 18 of American Speech and Hearing Association (ASHA) is Telepractice (Brown, 2014). The aim of SIG 18 is to provide education, leadership, and advocacy for issues in telepractice for audiology and speech-language pathology. More than 1,000 speech-language pathologists and audiologists joined SIG 18 within a span of four years. In India, telepractice in the field of speech language pathology is only a decade old (Brown, 2014).
The launch of a specialised centre for rehabilitation and education through distance mode in 2009, by the All India Institute of Speech and Hearing, Mysore may be considered as a formal beginning of teleservices (Rao and Yashaswini, 2018). There are only a few speech language pathologists in India providing telerehabilitation in the field of speech language pathology. The number of participants in the reported studies from India indicates this (Mohan et al., 2017; Rao and Yashaswini, 2018). The first published article on telepractice in India was a case report of a person with Broca’s Aphasia. The results showed significant improvement in the domains of expression, repetition, naming and memory (Goswami, Bhutada and Jayachandran, 2012; Rao and Yashaswini, 2018). The authors concluded that telepractice is effective in the Indian context and is an upcoming area in the field of speech language pathology (Goswami, Bhutada and Jayachandran, 2012; Rao and Yashaswini, 2018). The first ever survey on telepractice in Speech Language Pathology and Audiology in India was carried out by Mohan et al. (2017).
The questionnaire was emailed to the members of ISHA (Indian Speech and Hearing Association). There were 205 respondents out of which only 25 respondents reported using telepractice to deliver clinical services. The results showed that telepractice services were provided to clients throughout the lifespan. The service provided includes screening, assessment, management, follow-up or monitoring/ guidance and/or professional consultation. Disorders managed via telepractice include various child and adult speech language disorders (Mohan et al., 2017; Rao and Yashaswini, 2018). Among the disorders, speech sound disorders in children ranked first and motor speech disorders were ranked least. Positive feedback from clients about telepractice services was received by fifty-six percent of the tele practitioners. Lack of training was a reported drawback and a short-term training certification course in telepractice was suggested by telepractioners (Rao and Yashaswini, 2018).
The service providers in India had learned to implement telerehabilitation through personal experience rather than formal training. 92% of the tele-practitioners reported that they have not authored a publication on telepractice. This suggests a dearth of research on telerehabilitation in speech-language pathology and audiology in India (Mohan et al., 2017). The shortage of professionals in India to deliver clinical services can be met via the use of telerehabilitation. In a study on tele-speech language pathology and audiology in India, the majority of the participants reported technical issues as barriers for telerehabilitation.
Other challenges reported in the delivery of telerehabilitation were concerns about client and clinician confidentiality, lack of direct feedback and environmental distractions at client end. The benefits identified were improved access of services to clients with linguistic and cultural diversity; increased ease of collaboration among multi-disciplinary team members; and saves travel time with cost benefits for clients (Mohan et al., 2017). India is well equipped to fully develop telerehabilitation to overcome the barriers of distance and amplify the availability of speech language pathology, audiology and other healthcare services. The extensive use of telerehabilitation throughout India would require an improved infrastructure (e.g., to uphold privacy and security); training for professionals; and telerehabilitation policies (Rao and Yashaswini, 2018).
The outbreak of the pandemic COVID 19 has forced the speech language pathologists to shift from the traditional face to face therapy to telerehabilitation which was a new experience for most of the speech language pathologists. The American Speech-Language-Hearing Association (ASHA) has mentioned that telepractice is a viable process for delivering SLP services during COVID-19 pandemic and that both evaluation and treatment were possible through telepractice. Sarsak (2020) emphasized the need of speech language and hearing associations to promote telerehabilitation during the outbreak of COVID-19 (Sarsak 2020).
Courses on telerehabilitation can be conducted by these associations in various countries to increase the awareness of speech therapists on telerehabilitation and also research on this issue is prioritized. It will also improve the attitude of therapists toward telepractice and update their knowledge and skills. These associations must also pursue legal efforts to make these services legitimate (Sarsak 2020). Overall, it is suggested that further measures can be taken by the professional associations to eliminate barriers in the path of therapists and promote telepractice facilitators so that this type of care be used more extensively by SLPs (Tohidast et al., 2020).
The present study aimed to understand the challenges faced by the speech language pathologists to provide telerehabilitation services to the clients during the outbreak of pandemic covid 19, how they overcome those barriers, and benefits of telerehabilitation. Information gathered from this survey results can be used to upgrade the professional performance of speech language pathologists during this COVID 19 pandemic, develop the quality of telerehabilitation delivered to patients, mend existing deficiencies of the services provided through telerehabilitation and create awareness about various aspects of telerehabilitation (Tohidast et al., 2020).
There is a dearth of published literature on telerehabilitation in India and there are no published studies on telerehabilitation in Kerala to the best of the authors’ knowledge. Hence the objectives of the present study were to● Report the status of telerehabilitation in speech-language pathology in Kerala● Compare the opinions of Speech-Language pathologists about telerehabilitation in Kerala.● Report the challenges faced by Speech Language Pathologist during telerehabilitation and the strategies practiced to overcome them. ● Identify the benefits of telerehabilitation in speech-language pathology.
MATERIAL AND METHODS
The study was conducted in three phases; development of the questionnaire, administration of the questionnaire and the analyses of the responses. In phase 1, a questionnaire was developed to gather responses from Speech Language Pathologists practicing in the state of Kerala and it consisted of 25 questions. The questionnaire contained questions to collect the demographic details of the participants and questions to elicit the information about service delivery through telerehabilitation. Twenty-one closed ended questions were used to gather the opinions of SLPs about telerehabilitation. The given questions in the questionnaire addressed the opinions of Speech-Language pathologists about telerehabilitation, the challenges faced by Speech Language Pathologist during telerehabilitation, the strategies practiced to overcome them and the benefits of telerehabilitation.
Most of the questions required a response selected from multiple options and open-ended response options were given for the questions where the participants could provide their comments. The participants could select more than one response from multiple options for some of the questions and some of the questions were answered with either yes or no. The clinicians who have not provided telerehabilitation services could submit the questionnaire after filling the 8th question. Content validity of the questionnaire was done by 5 speech language pathologists and the questionnaire was modified according to the suggestions given data. In the second phase, the developed questionnaire was transformed into a google form.
The google form was sent to speech language pathologists through mail and WhatsApp and 105 speech language pathologists working across the state of Kerala responded to the questionnaire. Informed consent was taken from all the participants. Analysis of the responses was done in the third phase. Descriptive statistics is used to analyse the responses from the participants. Responses were analysed by calculating the percentage values of the questions. This was done separately for each participant and also for the overall responses.
RESULTS AND DISCUSSION
The results of this study give an outline about the status of telerehabilitation in the field of Speech Language Pathology in Kerala and the results were analysed using descriptive statistics. The demographic details are given in Table 1. There were 104 respondents and years of experience ranged for 6 months to 30 years. Majority of the respondents were post graduates and were working in academic institutions, clinics and hospitals. The gender distribution was skewed towards females with 96.2% of the respondents being females. This gender disparity in the field of speech and hearing has already been established (Rowden-Racette, 2013).
Table 1. Demographic details of the participants
| Demographic details | Number | Percentage | |
| Gender | Male | 4 | 3.8 |
| Female | 100 | 96.2 | |
| Years of experience | – | – | 6 months -30 years |
| Educational qualification | MASLP | 54 | 51.9 |
| BASLP | 28 | 26.9 | |
| MSc SLP | 12 | 11.5 | |
| MSc Audiology | 4 | 3.8 | |
| PhD | 4 | 3.8 | |
| MSc Speech and Hearing | 1 | 1 | |
| MSc Deglutology | 1 | 1 | |
| Work set up | Academic institute | 35 | 33.7 |
| Clinics | 22 | 21.2 | |
| Govt hospitals | 11 | 10.6 | |
| Private hospitals | 14 | 13.5 | |
| Private practice | 9 | 8.7 | |
| Special school
|
3 | 2.9 | |
| Block resource center | 2 | 1.9 | |
| Rehabilitation centers | 6 | 5.8 | |
| Urban resource centers | 1 | 1 | |
| NGO | 1 | 1 | |
The tele-rehabilitation services were provided by 74% (N=77) of the participants and 26% (N=27) of the participants did not provide telerehabilitation services during the pandemic COVID 19. The most common reasons for not providing telerehabilitation are given in Table 2. In the survey conducted by Mohan et al. (2017), there were only 25 SLPs doing telepractice in India among the 205 respondents. However, in the current survey in Kerala, 77 SLPs are providing tele-rehabilitation services among 104 participants. The lockdown followed by the pandemic Covid 19 has imposed the SLP’s to shift from the traditional face to face therapy to telerehabilitation which is the best method to provide the required services during Covid 19 (Mohan et al., 2017; Tohidast et al., 2020).
Table 2. Common reasons for not providing telerehabilitation
| Reason | Percentage of respondents |
| No insistence from clinics or institutes | 51 |
| Client population is difficult to handle | 25.9 |
| Not confident in providing telerehabilitation | 11.1 |
| Clients or parents are not interested.
|
14.8 |
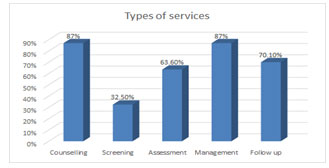
Majority of the SLPs (79.2%) had no experience in telerehabilitation before the outbreak of Covid 19 and 20.8% (N=16) had experience in delivering telerehabilitation. Their experience in providing telerehabilitation ranged from one month to three years. Among the speech language pathologists who provided telerehabilitation, 76.6% people agree that tele rehabilitation is a viable form of service delivery, 15.6% are not sure and 7.8% did not find telerehabilitation as a viable form of service delivery. This finding is in agreement to the earlier survey conducted by Mohan et.al in 2017. Figure 1 shows the percentage of respondents providing various telerehabilitation services. Various services provided through telerehabilitation include counselling, assessment, screening, management and follow up sessions. Similar results were observed by Mohan et al. (2017).
Figure 1: Percentage of respondents who delivered various services
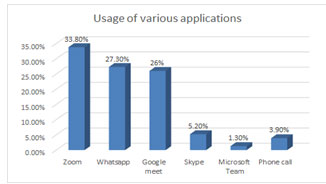
The various online platforms used by SLPs for delivering telerehabilitation included zoom, whatsapp, google meet, phone call, skype and microsoft teams. Percentage of use of each online platform are given in Figure 2. Two participants reported that they may use any of the above mentioned online platforms depending on the comfortability of their clients. The most reported reasons for using the specific apps were familiarity of the clients with the app (64.9%), familiarity of the clinician with the app (36.45%), better video quality (27.3%) and reduced data usage (14.3%).
Initially in India, Skype was used for telerehabilitation. Over the time, many video conferencing applications were developed which were user friendly. Custom made applications were also developed by private centers for their own use, but none of the respondents in the present survey mentioned that (Goswami et al., 2012). In the present study, all were using the free video conferencing applications which are available over the internet. First research paper on telerehabilitation from India reported the extensive use of the skype application for telerehabilitation (Goswami et al., 2012; Mohan et al., 2017).
Figure 2: Percentage of users of various online platforms
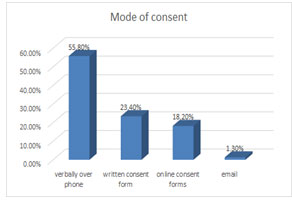
Taking consent before the commencement of telerehabilitation is very important. Lack of ethical guidelines, issues related to privacy and confidentiality on e-platforms, data protection were issues which required immediate attention in telepractice. A well written informed consent may resolve the issue to an extent. Even though the mode of getting consent was different, all SLPs except one had taken consent from the clients (Rao and Yashaswini, 2018).
This shows the awareness regarding this issue among the SLPs. Percentage of clinicians who used different modes of consent is summarised in Figure 3. The guidelines issued by ISHA clearly states the need for getting informed consent prior to the commencement of telepractice. Clients should be well informed regarding the modality of service delivery, its benefits and limitation, their rights and responsibilities including the process for communicating complaints or feedback (ISHA, 2020).
Figure 3: Percentage of clinicians who used different modes of consent.
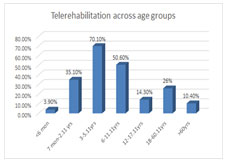
Telerehabilitation services were provided to clients of all ages. Figure 4 depicts the percentage of clinicians providing telerehabilitation for clients across various age groups. Even though telerehabilitation was provided to clients of all age groups, the paediatric population were served the most. Similar results were observed in the survey done by Mohan et al. (2017).
Figure 4: Percentage of clinicians providing telerehabilitation for clients across various age groups.
Through telerehabilitation, clients with various speech and language disorders were served which is summarised in Table 3. Results revealed that language disorders were the most common client population served followed by autism spectrum disorder and speech sound disorder. Dysphagia and apraxia were the least served (Mohan et al., 2017).
Table 3: Percentage of clinicians who served various disorders served through telerehabilitation.
| Disorder/ client population served | Percentage of respondents |
| Language Disorder | 53.2 |
| Autism spectrum Disorders | 46.8 |
| ADHD | 15.6 |
| Learning disabilities | 24.7 |
| Cerebral Palsy | 13 |
| Global developmental delay | 23.4 |
| Speech Sound Disorders | 41.6 |
| Fluency disorders | 39 |
| Aphasia | 23.4 |
| Dysarthria | 14.3 |
| Voice and resonance disorders | 15.6 |
| Cognitive communicative disorders | 10.4 |
| Hearing loss | 24.7 |
| Clients attending auditory verbal therapy | 10.4 |
| Clients using AAC | 9.1 |
| Dysphagia | 1.3 |
| Verbal apraxia of speech | 1.3 |
Table 4 summarizes the responses of the SLPs regarding the client population which are difficult to manage. Even though the majority of the participants have provided services to children with autism spectrum disorder and ADHD, they reported that these children were the most difficult to manage client population while providing telerehabilitation. This could be due to their hyperactivity and inattention which makes it difficult to sit in front of the screen and follow clinician’s instructions. The difficulty to manage dysphagia through telerehabilitation was reported by only one participant and this can be due to the smaller number of SLPs providing telerehabilitation for dysphagia clients.
Managing dysphagia through tele mode may involve many risks. But through proper planning and training of both client and the caregiver, we can successfully treat dysphagia through telerehabilitation. Considerations for the management of dysphagia through telerehabilitation is given by Miles et al., (2020). But both research and clinical practice in this area show that the use of telehealth for dysphagia management can be safe, feasible, and reliable, but several safeguards and considerations need to be in place (Miles et al., 2020).
Table 4. Difficult to manage client population.
| Difficult to handle population | Percentage of respondents |
| Language Disorder | 6.5 |
| Autism spectrum Disorders | 66.2 |
| ADHD | 51.9 |
| Learning disabilities | 1.3 |
| Cerebral Palsy | 20.8 |
| Global developmental delay | 22.1 |
| Speech Sound Disorders | 9.1 |
| Fluency disorders | 6.5 |
| Aphasia | 9.1 |
| Dysarthria | 6.5 |
| Voice and resonance disorders | 11.7 |
| Cognitive communicative disorders | 13 |
| Clients attending auditory verbal therapy | 23.4 |
| Clients using AAC | 16.9 |
| Dysphagia | 2.6 |
The sudden trend in telerehabilitation has led SLPs to face various challenges / barriers. Majority of the respondents did not have any previous experience in telerehabilitation and hence had to face many challenges while implementing telerehabilitation. Table 5 summarizes the client/ clinician related challenges while providing telerehabilitation. Difficult to manage children through online mode was the one of the biggest challenges faced by SLPs followed by scarcity of online resources about telerehabilitation and non-willingness of parents or patients to shift from traditional face to face therapy to telerehabilitation (Miles et al., 2020).
Table 5. Client/ clinician related challenges while providing telerehabilitation.
| Challenges/ Barriers faced | Percentage of respondents |
| Lack of training | 22.1 |
| Lack of online resources | 46.8 |
| Lack of confidence | 5.2 |
| Parents or patients are not willing to attend | 44.2 |
| Difficult to manage children through online mode | 76.6 |
| Non availability of caretaker or parent | 18.2 |
| Non cooperative parents | 27.3 |
| Children with attention issues | 22.1 |
| Others | 7.8 |
Table 6 represents the technical challenges faced by SLPs while implementing telerehabilitation. Among the technical challenges faced, internet connectivity issues stand first followed by inadequate knowledge of clients to use tele-service applications and non-availability of smartphones or computers. SLPs learned through personal experiences rather than formal training. Webinars have become a trend in the Covid season and webinars on telepractice is the only formal kind of information gaining that has happened. Similar results including insufficient resources (i.e., structural framework, technical support, resource materials) to provide appropriate tele-speech-language pathology services and the lack of formal training in India were the major concerns reported by Mohan et al. (2017).
Table 6. Technical challenges.
| Technical challenges | Percentage of respondents |
| Internet connectivity issues | 94.8 |
| No internet connection | 7.8 |
| Non availability of smart phone / computer | 39 |
| Clients not good at using applications | 58.4 |
| Non availability of interactive software | 1.3 |
Even though the participants reported of various challenges faced while providing telerehabilitation, evident effort has also been taken to overcome these challenges which is given in Table 7. The reported solutions tried to overcome the challenges were discussing with the SLPs who have experience in telerehabilitation, trial and error method, attending webinars and reading articles on improving telerehabilitation. Development of professional skills for telepractice, validation of digital resources in the different languages of India; empirical studies on mode of service delivery in telepractice (face-to-face, virtual or hybrid); mechanisms to protect client’s privacy on e-platforms; and revision of code of ethics for speech-language.
pathologists and audiologists who are using telepractice were the immediate concerns as reported in the report on tele speech language pathology and audiology in India and these concerns still remain the same (Rao and Yashaswini 2018). But due to the sudden boom in telerehabilitation, we expect a sudden growth in these areas and in the near future, we will be able to overcome the barriers faced. Despite these challenges, telerehabilitation has a critical role during the infectious pandemics and it will reduce the risk of spreading the infection which are transmitted by person-to-person contact (Smith et al., 2020).
Table 7. Steps taken to overcome the challenges.
| Steps taken | Percentage of respondents |
| Discussed with SLPs who have experience in telerehabilitation | 71.4 |
| Read articles on telerehabilitation | 49.4 |
| Attended webinars on telerehabilitation | 61 |
| Trial and error method | 71.4 |
| Educating parents | 1.3 |
| Watched youtube videos on telerehabilitation | 1.3 |
There were many benefits experienced through telerehabilitation. Table 8 shows the various benefits of telerehabilitation identified by participants. Eliminating long distance travelling thus avoiding the risk of Covid 19 was the benefit cited by majority of the SLPs (92.2%). Other benefits include comfortability of clients in performing activities at the home set-up, increased involvement of parents in therapy, regularity in taking sessions, increased patient reach or access, easy to follow up, easy to perform creative screen-based activities and patient satisfaction (ISHA, 2020).
The benefits of telerehabilitation makes it a viable form of providing services to clients with speech and language impairments and the majority of clinicians could achieve their goals through telerehabilitation. The technological advancements and the benefits can make it a regular form of service even after the COVID 19 season. The scarcity of resources and other issues such as lack of legal guidelines and policies for safe and secure service delivery should be addressed by the concerned authorities at the earliest. Recently Indian Speech and Hearing Association (ISHA) has compiled and published the telepractice guidelines for audiology and speech language pathology services in India including operational and ethical aspects (ISHA, 2020).
Table 8. Benefits identified through telerehabilitation.
| Benefits | Percentage of respondents |
| Regularity in taking sessions | 54.5 |
| Increased patient access or reach | 53.2 |
| Eliminating long distance travel and thus avoiding the risk of Covid 19 | 92.2 |
| Parents could involve more in therapy | 61 |
| Patient satisfaction | 22.1 |
| Easy follow up/ monitoring | 46.8 |
| Clients are comfortable in performing activities at the home set-up. | 84.5 |
| Easy to perform creative screen- based activities | 1.3 |
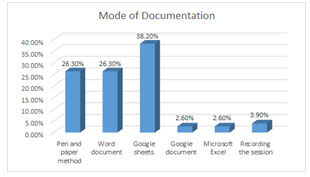
Different methods of documentation used by SLPs were depicted in figure 5. As noted from the chart, the various methods include traditional pen and paper method, word document, google sheets, excel sheets, google docs and recording of sessions were reported. The clinical record is an overall indicator of clinical and service quality, and serves as a basis for planning care and for service continuity (Sutherland, 2006). Documentation style may vary among professionals or organizations but should adhere to specific facility standards. Whatever be the style, clinical records should be consistent in format and style and should use appropriate terminology, approved abbreviations, and correct diagnosis and procedure codes. Majority of the respondents in the survey use various electronic documentation methods. E- records give the flexibility of accessing it anywhere, anytime. Indian Speech Hearing Association had recommended storing all the client related reports and records of the telepractice session using the unique patient identification number in a confidential manner (ISHA, 2020).
Figure 5: Methods of documentation used by SLPs.
Majority of the tele practitioners could achieve the targeted goals through telerehabilitation. 74% (N= 57) of the tele practitioners reported that they could achieve the goals through telerehabilitation. 22.1 % (N=17) were not sure and 3.9 % (N=3) reported that they could not achieve the goals. A small percentage who could not achieve their goals would be those tele-practioners who serve the difficult to handle population such as clients with dysphagia, autism spectrum disorder or ADHD (ISHA, 2020). The feedback from the clients regarding telerehabilitation as reported by the SLPs is shown in Figure 6 and only one SLP among the participants reported that the clients were not satisfied with telerehabilitation (ISHA, 2020).
Figure 6: Feedback from clients.

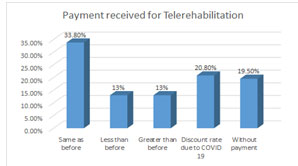
The payment received for telerehabilitation services were differing among SLP’s as depicted in Figure 7. To the best of authors’ knowledge, telerehabilitation services are charged more than the traditional face to face therapy due to the use of high-speed internet data and the increased time required for planning and preparation. But in the present study, only a small percentage (13%) of SLPs have charged more than the charge paid for traditional face to face therapy. Majority (33.8%) has charged the same fees as that of pre COVID face to face therapy. Some provided telerehabilitation services at a discounted rate (20.80%) due to the COVID 19 and some had provided services free of cost (19.50%) (Smith et al., 2020).
Free telerehabilitation services were provided by SLPs working in government services including hospitals and institutes. To the best of authors’ knowledge, none of the previous studies had mentioned the fees charged for telerehabilitation. Regardless of the fees charged, telerehabilitation is the best method to provide the required services during Covid 19 (Tohidast et al., 2020). To fulfil the need for continuous therapy sessions for children and adults with speech-language disorders, the implementation of telepractice in the field of Speech Language Pathology is necessary which will also help to prevent the transmission of COVID-19, and thereby guaranteeing the health of SLPs and patients (Smith et al., 2020).
Figure 7: Payment received for telerehabilitation.
CONCLUSION
The present survey was conducted using a self-rated questionnaire and reported the status of telerehabilitation in the field of speech-language pathology in Kerala, the challenges faced by Speech Language Pathologist during telerehabilitation, the strategies practiced to overcome them and the benefits of telerehabilitation in speech-language pathology. Even though all of the participants were practicing traditional face to face therapy before the outbreak of COVID 19 pandemic, majority of them easily shifted to a tele-mode of providing services during the COVID 19 pandemic outbreak.
This survey depicted the need for publishing standard guidelines for providing telerehabilitation services. At the time of data collection, there were no published standard guidelines in India for providing telerehabilitation. But in November 2020, Indian Speech and Hearing Association (ISHA) came forward with the guidelines for telepractice which will help the telerehabilitation service providers to provide better services to their clients. It also emphasizes the need for improved infrastructure and training to professionals to ensure quality services to their clients.
Conflict of Interest: Authors declares no conflicts of interests to disclose.
Ethical Clearance Statement: The Current Research Work Was Ethically Approved by the Institutional Review Board (IRB) of National Institute of Speech and Hearing, NISH Road, Aakkulam, Trivandrum, Kerala, India.
ACKNOWLEDGEMENTS
We thank National Institute of Speech and Hearing, Trivandrum, Kerala for permitting us to conduct the survey and also all the fellow professionals across Kerala for participating in this study.
REFERENCES
American Speech-Language-Hearing Association. (2005a). Audiologists providing clinical services via telepractice: Position statement [Position Statement]. Available from www.asha.org/telepractice.htm
Brennan, D.M., Mawson, S. and Brownsell, S., (2009). Telerehabilitation: enabling the remote delivery of healthcare, rehabilitation, and self-management. Stud Health Technol Inform, 145(231), p.48.
Brown, J., (2011). ASHA and the evolution of telepractice. Perspectives on Telepractice, 1(1), pp.4-9.
Brown, J., (2014). The State of Telepractice in 2014: Telepractice is an ever-expanding service-delivery option, with more US speech-language pathologists and audiologists adopting it every day. But reimbursement policies continue to lag behind the trend. The ASHA Leader, 19(12), pp.54-57.
Goswami, S.P., Bhutada, A. and Jayachandran, K., (2012). Telepractice In A Person With Aphasia. Journal of the All India Institute of Speech & Hearing, 31.
Grillo, E.U., (2017). Results of a survey offering clinical insights into speech-language pathology telepractice methods. International journal of telerehabilitation, 9(2), p.25.
Gunjawate, D.R., Ravi, R., Yerraguntla, K., Rajashekhar, B. and Verma, A., (2020). Impact of coronavirus disease 2019 on professional practices of audiologists and speech-language pathologists in India: A knowledge, attitude and practices survey. Clinical Epidemiology and Global Health.
Indian Speech and Hearing Association. (2020). Telepractice guidelines for audiology and speech, language pathology services in India. Available from https://www.ishaindia.org.in/pdf/announce/Telepractice_Guidelines_Audiology_and_SLP.pdf
Miles, A., Connor, N.P., Desai, R.V., Jadcherla, S., Allen, J., Brodsky, M., Garand, K.L., Malandraki, G.A., McCulloch, T.M., Moss, M. and Murray, J., (2020). Dysphagia care across the continuum: a multidisciplinary Dysphagia Research Society Taskforce report of service-delivery during the COVID-19 global pandemic. Dysphagia, pp.1-13.
Mohan, H.S., Anjum, A. and Rao, P.K., (2017). A survey of telepractice in speech-language pathology and audiology in India. International journal of telerehabilitation, 9(2), p.69.
Rao, P.K.S. and Yashaswini, R., (2018). Telepractice in speech-language pathology and audiology: Prospects and challenges. Journal of Indian Speech Language & Hearing Association, 32(2), p.67.
Rowden-Racette, K., (2013). Where the boys aren’t. The ASHA Leader, 18(8), pp.46-51.
Sarsak, H.I., (2020). Telerehabilitation services: A successful paradigm for occupational therapy clinical services. Int Phys Med Rehabil J, 5(2), pp.93-98.
Smith, A.C., Thomas, E., Snoswell, C.L., Haydon, H., Mehrotra, A., Clemensen, J. and Caffery, L.J., (2020). Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID-19). Journal of telemedicine and telecare, p.1357633X20916567.
Sutherland Cornett, B., (2006). Clinical documentation in speech-language pathology: essential information for successful practice. The ASHA Leader, 11(12), pp.8-25.
Tohidast, S.A., Mansuri, B., Bagheri, R. and Azimi, H., (2020). Provision of speech-language pathology services for the treatment of speech and language disorders in children during the COVID-19 pandemic: Problems, concerns, and solutions. International journal of pediatric otorhinolaryngology, 138, p.110262.
World Health Organization, (2020). Mental health and psychosocial considerations during the COVID-19 outbreak, 18 March 2020 (No. WHO/2019-nCoV/MentalHealth/2020.1). World Health Organization.


