Department of Pediatric Dentistry and Orthodontics King Saud University, Riyadh, Saudi Arabia.
Corresponding author email: e_shayea@hotmail.com
Article Publishing History
Received: 20/03/2021
Accepted After Revision: 27/05/2021
Even though the impaction of maxillary central incisor during the mixed dentition stage is uncommon, it poses esthetic and phonetic problems that need early detection and management. This case report aims to present a common finding of an 11-year old boy with impacted permanent maxillary left central incisor, affecting the facial aesthetic and the patient’s smile. This impaction was managed by an interceptive orthodontic approach that consisted of surgical removal of the obstruction, and regaining of space for the impacted tooth. This was followed by surgical exposure, orthodontic traction, and proper alignment of the impacted tooth 21. This case report illuminates the importance of early diagnosis of the impacted central incisor and the effectiveness of interceptive orthodontic management in insuring successful long-term aesthetic outcomes.
Impacted Tooth, Orthodontic Traction, Orthodontic Management, Surgical Exposure.
Al-Shayea E. I. Surgical Exposure and Orthodontic Management of Unilateral Impacted Maxillary Central Incisor: A Case Report. Biosc.Biotech.Res.Comm. 2021;14(2).
Al-Shayea E. I. Surgical Exposure and Orthodontic Management of Unilateral Impacted Maxillary Central Incisor: A Case Report. Biosc.Biotech.Res.Comm. 2021;14(2). Available from: <a href=”https://bit.ly/3vioHeB“>https://bit.ly/3vioHeB</a>
Copyright © This is an Open Access Article distributed under the Terms of the Creative Commons Attribution License (CC-BY). https://creativecommons.org/licenses/by/4.0/, which permits unrestricted use distribution and reproduction in any medium, provided the original author and sources are credited.
INTRODUCTION
Impaction is an impeded tooth eruption due to several local and systemic causes leading to a delayed or even failure of eruption of the tooth. Impaction of permanent maxillary incisors usually occurs because of displacement of the tooth bud or pathological obstruction, such as the presence of supernumerary teeth that comprise about 56-60% of permanent incisors impaction (Al‑Zoubi et al., 2017; Syriac et al., 2017; Khandelwal et al., 2018). The pathological obstruction could also happen as a result of odontomas, cysts, as well as root dilaceration following a trauma to the primary incisor tooth (Chokron et al., 2010; Jayam et al., 2014; Narsapur and Choudhari, 2015).
In addition, crowding, early loss, and/or over retained (ankylosed) deciduous tooth are considered among local causes of permanent central incisors impaction (American Academy of Pediatric Dentistry, 2020). Cleidocranial dysplasia, amelogenesis imperfect, and endocrine deficiencies are the most common syndromes of systemic factors for tooth impaction (Choukroune, 2017; Puranik and Gandhi, 2019). Even though the impaction of maxillary central incisor is uncommon, with an impaction prevalence rate of less than 1%, compared to third molars or canines with 1-4% of incidence rate, it poses esthetic and phonetic problems that require early detection and management (Alhammadi et al., 2018; Yemitan, 2018; Alyami et al., 2020).
Interceptive orthodontic treatment is needed to correct any eruption disturbances and to eliminate any functional and/or skeletal interferences (Keerthana et al.,2020; American Academy of Pediatric Dentistry, 2020). Hence, the aim of this article is to present a detailed and informative report on a clinical case with unilateral impaction of permanent maxillary central incisor, in mixed dentition stage, caused by the presence of supernumerary tooth (mesiodens), and managed with a combined surgical-orthodontic approach.
Case Report: An 11-year-old boy was brought by his mother and was admitted into a pediatric clinic, with a chief complaint of delayed eruption of permanent maxillary central incisors at the time of that visit. The pedodontist removed the retained deciduous central incisors to allow for a spontaneous eruption of permanent successors. Following the eruption of the right maxillary central incisor, the pediatric dentist referred the patient to orthodontic clinic for evaluation of delayed eruption of the left maxillary central incisor (tooth # 21) at the Department of Orthodontics, College of Dentistry, King Saud University, Riyadh, Saudi Arabia.
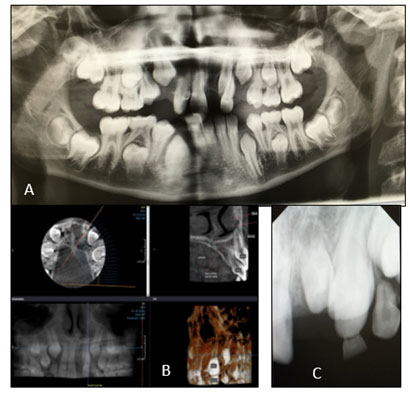
The patient was medically fit and had no history of dental trauma. He was presented with skeletal Class I malocclusion and balanced facial proportions. Intraoral examination revealed upper midline shift to the left side due to missing maxillary permanent left central incisor (tooth 21) that was bulging labially at the mucogingival junction. In addition, an Angle’s Class I molar relationship was observed in the early mixed dentition phase (Figure 1).
Figure 1: pretreatment extraoral and intraoral photographs showing unerupted tooth 21 with midline shift.

Several radiographs were taken for the patient as part of the routine pre-treatment records including, a panoramic (OPG), lateral cephalometric radiographs, and intraoral periapical (PA) radiographs of upper anterior region. The radiographs revealed the presence of supernumerary tooth (mesiodens) in the pre-maxillary region and an impaction of tooth 21 (Figure 2).
Furthermore, a cone-beam computed tomography (CBCT) scan was performed to assess the position and the morphology of the impacted tooth 21. CBCT images showed that tooth 21 is located buccal to tooth 22 and is in direct contact with it. The maxillary left central incisor is positioned superiorly where the tip of the root seems to be close to the nasal cavity (Figure 2).
Therefore, an extra caution was required to avoid any injury to the adjacent lateral incisor or to the nasal cavity. The main objectives of the interceptive treatment were the following. First, to extract the retained deciduous lateral incisor, and remove the supernumerary tooth surgically. In addition, the treatment aimed at regaining space for tooth 21 followed by surgical exposure of the maxillary left central incisor. The final objective was to perform orthodontic traction and proper alignment in to the arch.
The entire treatment procedure was explained to the patient and his mother. Written consent forms for both treatment and publication were signed before starting the interceptive orthodontic treatment. The author ensured the identity of the patient remains anonymous and the data was classified to ensure confidentiality and the privacy of information.
Figure 2: Pretreatment radiographs. A)Panoramic; B) CBCT images; C) intraoral periapical radiographs showing supernumerary tooth, and an impacted permanent left central incisor overlapping with the permanent left lateral incisor.
The patient was scheduled to be fitted with fixed orthodontic appliance following the surgical extraction of the mesiodens with a mucoperiosteal flab. Transpalatal arch with Nance button was fabricated and cemented on the maxillary permanent first molars, as an anchorage device, during the orthodontic traction of tooth 21 and maxillary canines. Furthermore, for teeth leveling and alignment, an orthodontic 0.022″ preadjusted brackets were bonded on the labial surfaces of all maxillary existing teeth, and a 0.016-inch nickel–titanium (NiTi) arch wire was fitted on the maxillary arch of the patient.
In a period of four months, an adequate space for tooth 21 was regained by frequent activation of Ni Ti open coil spring between tooth 11 and tooth 22, and by anchoring a heavy stainless steel arch wire (0.017X0.025-inch). A closed eruption surgical technique was achieved with raised flab, little bone removal with preservation of the mucoperiosteum and gingival tissues, bonding an attachment to tooth 21, and lastly repositioning of the flab to its former position.
Two weeks following the surgical exposure of the impacted tooth, maxillary labial frenectomy was performed in order to correct the inferior position of the maxillary labial fraenum attachment, and before starting the orthodontic traction of the impacted tooth. Following another period of four months, the impacted tooth 21 was erupted into the oral cavity. Repositioning of the attachments on teeth 21 and 23 and a light flexible arch wire (0.016-inch copper NiTi) was used to fully engage these teeth (Figure 3).
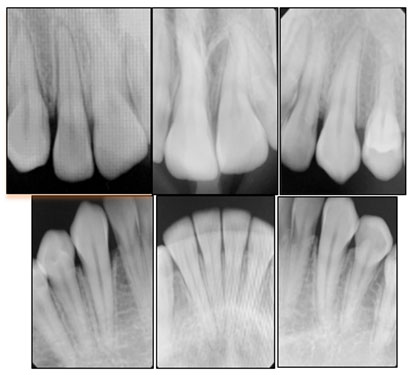
Five months later, the impacted maxillary left permanent central incisor was successfully positioned in and was properly aligned with the rest of the upper teeth and with good periodontal condition. At the same time, the lower arch was scheduled for bracket bonding and aligning of the lower teeth to be in a proper occlusion with the upper arch. Permanent fixed retainers were placed in both arches at the end of the treatment. Successful interceptive orthodontic treatment was completed with ideal alignment of the impacted tooth 21, ideal over jet, ideal over bite, and proper interdigitation.
The clinical examination of the orthodontically treated incisor tooth 21 showed normal vitality test with acceptable gingival margins and attached gingiva (Figure 4). Furthermore, the final radiographs presented intact roots with proper root parallelism and good inclination of the treated teeth (Figure 5). The patient and his mother were satisfied with the results and a three months follow up appointment was scheduled to reevaluate the gingival contour of tooth 21 to assess if further esthetic gingival recontouring is needed.
Figure 3: Intraoral photographs of the orthodontic traction stages of tooth 21. A) Frontal view; B) Occlusal view; and C) Left side view.
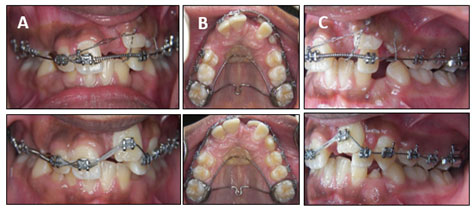
Figure 4: Posttreatment extraoral and intraoral photographs showing the proper alignment of the impacted tooth 21, ideal over jet, ideal over bite, and proper interdigitation.

Figure 5: Posttreatment periapical radiographs showing intact roots with proper root parallelism and good inclination of the treated teeth.
DISCUSSION
The treatment of an impacted permanent central incisor depends on the severity of the impaction, type of malocclusion, and the degree of root completion and dilacerations (Chaushu et al.,2015; American Academy of Pediatric Dentistry, 2020). The literature shows two alternative treatment options for treating such cases that need interdisciplinary approach. The first option includes extraction of the impacted central incisor followed by either closing of the space or prosthetic replacement. The second treatment option includes surgical exposure of the impaction with orthodontic traction followed by an alignment of the impacted central incisor (Singh et al., 2107; Khera et al., 2017; Noorollahian and Shirban, 2018).
Early correction of the impacted central incisor in the present clinical case was recommended by eliminating the cause of the problem, which was the prolonged retention of the deciduous central incisor, as well as, the presence of the supernumerary tooth (mesiodens) in the premaxillary region as confirmed by the two-dimensional (OPG, PA) and three-dimensional (CBCT) imaging. Therefore, early diagnosis is required for an accurate visualization and evaluation of the impacted tooth, and hence formulating an ideal treatment plan (Singh et al., 2107; American Academy of Pediatric Dentistry, 2020).
In this case, the second treatment option, mentioned above was chosen. This option consisted of the following procedures. First, removal of the eruption obstacles (retained deciduous incisor and mesiodens). Second, regaining space for the impacted tooth. Lastly, surgical exposure and orthodontic traction to align the impacted central incisor since spontaneous eruption had not occurred, as recommended in the literatures.
The extraction of the impacted tooth in the present case was not considered as a plan of treatment in order to reduce the risk of alveolar bone loss and to preserve the edentulous alveolar ridge of the impacted tooth 21. In addition, no root resorption was found on tooth 21, and on palpation of the labial sulcus, and there was bulging of the impacted tooth at the mucogingival junction (Sun et al., 2014; Spuntarelli et al., 2015, Khera et al., 2017; Singh et al., 2107; Noorollahian and Shirban, 2018; American Academy of Pediatric Dentistry, 2020).
Moreover, the surgical exposure of the impacted permanent left central incisor was carried out by using a closed eruption technique as suggested by Becker et al. (Becker et al., 2002). This technique is the most common surgical procedure, and it is ideal for high impaction located above the mucogingival junction, which was taken into account for this case in order to obtain an adequate keratinized tissue and a better periodontal condition around the erupting tooth (Shi et al., 2015; Noorollahian and Shirban, 2018; Henner et al., 2108).
The removal of the maxillary labial fraenum by frenectomy is another surgical procedure that was carried out in this case along with the orthodontic traction of tooth 21 to eliminate the inferiorly positioned fraenum that encroaches on the gingival margins, and hence facilitate orthodontic closure of the space between the maxillary central incisors (Naini and Gill, 2018; Kadkhodazadeh et al, 2018).
CONCLUSION
This case report presents a common finding of an 11-year old boy with impacted permanent maxillary left central incisor, affecting the facial aesthetic and the patient’s smile. This impaction was managed by an interceptive orthodontic approach that consists of surgical removal of the obstruction, regaining of space for the impacted tooth. Followed by surgical exposure, orthodontic traction, and proper alignment of the impacted tooth 21. This case report highlights the importance of early diagnosis and the effectiveness of interceptive orthodontic management to ensure a successful long-term aesthetic outcomes.
Data Availability: Data are available from the corresponding author on request.
Ethical Statement: Thank you for submitting your proposal to the King Saud University Institutional Review Board (IRB). Your proposal was evaluated in light of the KSU IRB policy and national regulations that govern the protection of human subjects in research, and concludes that your research project and its procedure does not pose ‘more than minimal risk to the human participants’. The KSU IRB has determined that your proposed study is ‘Exempt’ from further IRB review. Please note that this approval is for the research ethics perspective only. You still need to at least notify or get approval from the department head or unit of KSU/KSUMC or external institution prior to collecting data.
Please note that even though your project is given exemption from IRB review, the research must be conducted according to the ethical guidelines and KSU IRB policies. In case of any significant change(s) to the approved protocol, you must submit a revised protocol along with a request for amendment for IRB approval/ favorable opinion. Any changes to the research protocol may prevent the research from qualifying for exempt review and require to be halted until approval of amendment by the IRB is granted.
Conflicts of Interest: The author declares that there is no conflict of interest regarding the publication of this paper.
REFERENCES
Alhammadi, Asiri, and Almashraqi (2018). Incidence, severity and orthodontic treatment difficulty index of impacted canines in Saudi population. Journal of Clinical and Experimental Dentistry. Vol 10, No 4 Pages e327–e334
Alyami, Braimah, and Alharieth (2020). Prevalence and pattern of impacted canines in najran, south western Saudi Arabian population. The Saudi Dental Journal. Vol 32 No 6 Pages 300–305
Al‑Zoubi, Alharbi, Ferguson, Zafar (2017). Frequency of impacted teeth and categorization of impacted canines: A retrospective radiographic study using orthopantomograms. Eur J Dent. Vol 11 No 1 Pages 117‑121. doi: 10.4103/ejd.ejd_308_16.
American Academy of Pediatric Dentistry (2020). Management of the developing dentition and occlusion in pediatric dentistry. The Reference Manual of Pediatric Dentistry. Chicago, Ill 393-409.
Becker, Brin, Ben-Bassat, Zilberman, Chaushu. (2002) Closed-eruption surgical technique for impacted maxillary incisors: a postorthodontic periodontal evaluation. Am J Orthod Dentofacial Orthop. Vol 122 No 1 Pages 9-14. doi: 10.1067/mod.2002.124998.
Chaushu, Becker, and Becker (2015). Impacted central incisors: factors affecting prognosis and treatment duration. Am J Orthod Dentofacial Orthop Vol 147 No 3 Pages 355-362 doi: 10.1016/j.ajodo.2014.11.019. PMID: 25726403.
Chokron, Reveret, Salmon, Vermelin (2010) Strategies for treating an impacted maxillary central incisor. Int Orthod. Vol 8 No 2 Pages 152-176. doi: 10.1016/j.ortho.2010.03.001.
Choukroune (2017). Tooth eruption disorders associated with systemic and genetic diseases: clinical guide. J Dentofacial Anom Orthod Vol 20 No 4 Page 402-417
Henner, Pignoly, Antezack, Monnet-Corti (2018). Periodontal approach of impacted and retained maxillary anterior teeth. J Dentofacial Anom Orthod Vol 21 Page 204. DOI: 10.1051/odfen/2018053
Jayam, Bandlapalli, Patel, Choudhary (2014). A case of impacted central incisor due to dentigerous cyst associated with impacted compound odontome. BMJ Case Rep. 2014: bcr2013202447.
Published online 2014 Mar 20. doi: 10.1136/bcr-2013-202447
Kadkhodazadeh, Amid, Kermani, Hosseinpour (2018). A modified frenectomy technique: a new surgical approach. Gen Dent. Vol 66 No 1 Pages 34-38. PMID: 29303760.
Keerthana, Gnanashanmugam, Kannan S.Vaibava Keerthana (2020). Interceptive Orthodontics-A review. Dr. Gnanashanmugam Dr.M.S. KannanS.Vaibava Keerthana Dr. Gnanashanmugam Dr.M.S. KannanEuropean Journal of Molecular & Clinical Medicine Vol 7 No 4 Pages 1757-1761
Khandelwal, Rai, Bulgannawar, Hajira, Masih, Jyani (2018). Prevalence, Characteristics, and Morphology of Supernumerary Teeth among Patients Visiting a Dental Institution in Rajasthan. Contemp Clin Dent. Vol 9 No 3 Pages 349-356. doi: 10.4103/ccd.ccd_31_18. PMID: 30166825; PMCID: PMC6104375.
Khera, Rohilla, Tandon, Singh (2017). Orthodontic management of impacted central incisor: A clinical challenge. J Indian Orthod Soc Vol 51 No 1 Pages 46-50.DOI: 10.4103/0301-5742.199249
Naini, Gill (2018). Oral surgery: Labial frenectomy: Indications and practical implications. Br Dent J. Vol 225 No 3 Pages 199–200. https://doi.org/10.1038/sj.bdj.2018.656
Narsapur, Choudhari (2015). Dentigerous cyst with atypical mesiodens: an unusual clinical case report. RSBO (Online) Vol 12 No 2 Pages 220-224. ISSN: Electronic version: 1984-5685
Noorollahian and Shirban (2018). Chair time saving method for treatment of an impacted maxillary central incisor with 15-month follow-up. Dent Res J (Isfahan) Vol 15 No 2 Pages 150–154.
Puranik and Gandhi (2019). Developmental Dental Anomalies of Primary and Permanent Dentition. Journal of Dental Sciences. Vol 4 No 4 Page 000241. DOI: 10.23880/oajds-16000241
Shi, Xie, Quan, Wang, Sun, Zhang, et al. (2015) Evaluation of root and alveolar bone development of unilateral osseous impacted immature maxillary central incisors after the closed‑eruption technique. Am J Orthod Dentofacial Orthop. Vol 148 No 4 Pages 587‑598
Singh, Bagga , Tripathi , Gupta , Singh (2017). Orthodontic management of impacted teeth: An overview. Indian Journal of Orthodontics and Dentofacial Research Vol 3 No 2 Pages 59-63
Spuntarelli, Cecchetti, Arcuri, Testi, Melone, Bigelli, et al. (2015) Combined orthodontic-surgical approach in the treatment of impacted maxillary canines: Three clinical cases. Oral Implantol (Rome) Vol 8 No 2-3 Pages 63–67.
Sun, Wang, Sun, Ye, Dai, Wang X, et al. (2014) Root morphology and development of labial inversely impacted maxillary central incisors in the mixed dentition: A retrospective cone‑beam computed tomography study. Am J Orthod Dentofacial Orthop. Vol 146 No 6 Pages 709‑716. doi: 10.1016/j.ajodo.2014.07.026.
Syriac, Joseph, Rupesh, Philip, Cherian, Mathew (2017). Prevalence, Characteristics, and Complications of Supernumerary Teeth in Nonsyndromic Pediatric Population of South India: A Clinical and Radiographic Study. J Pharm Bioallied Sci. (Suppl 1) Pages S231-S236. doi: 10.4103/jpbs.JPBS_154_17. PMID: 29284970; PMCID: PMC5731020.
Yemitan (2018). Pattern of permanent canine impaction and associated retained deciduous canine of a Nigerian orthodontic patient population. Annals of Clinical Sciences. Vol. 3 No 2 Pages 34–38


