1Department of Ophthalmology and Optometry, SRM Medical College Hospital and Research Centre,
SRM Institute of Science and Technology, SRM Nagar, Kattankulathur, Kanchipuram, Chennai, India.
2Sri Jayendra Saraswathi Institute of Optometry, Chennai, India.
Corresponding author email: premsudl@srmist.edu.in
Article Publishing History
Received: 21/02/2022
Accepted After Revision: 10/05/2022
Silicone Hydrogel Contact Lenses (SiH CL) provides better comfort when compared with hydrogel contact lenses. But the signs that show up in wearers with reduced comfort are unclear. Thus, we aimed to study the association between symptoms and clinical signs of dry eye in SiH CL wearers. Forty-eight SiH CL wearers (mean age: 28.8 ± 5.0 years) underwent ocular assessments with and without contact lens, and completed Contact Lens Dry Eye questionnaire-8 (CLDEQ-8). Contact-lens related dryness was reported by 52.1% (n=25) subjects. A significant (p<0.01) Spearman’s correlation was found between CLDEQ-8 score and pre-lens tear film non-invasive tear break-up time (r=-0.80), pre-ocular tear film non-invasive tear break-up time (r=-0.78), invasive tear break-up time (-0.87), and Schirmer test (r=-0.83). In conclusion, for comfortable SiH CL usage, a healthy tear film is essential, and a thorough clinical evaluation may be beneficial in alleviating discomfort.
CLDEQ-8, Dry Eye, Signs, Silicone Hydrogel, Symptoms.
Lawrence P, Senthilkumar D. Signs and Symptoms of Dry Eye Among Silicone Hydrogel Soft Contact Lens Wearers. Biosc.Biotech.Res.Comm. 2022;15(2).
Lawrence P, Senthilkumar D. Signs and Symptoms of Dry Eye Among Silicone Hydrogel Soft Contact Lens Wearers. Biosc.Biotech.Res.Comm. 2022;15(2). Available from: <a href=”https://bit.ly/3wIpoky“>https://bit.ly/3wIpoky</a>
Copyright © This is an Open Access Article distributed under the Terms of the Creative Commons Attribution License (CC-BY). https://creativecommons.org/licenses/by/4.0/, which permits unrestricted use distribution and reproduction in any medium, provided the original author and sources are credited.
INTRODUCTION
Dry eye is an ocular surface disorder that is caused by a loss of homeostasis in the tear film. This causes instability in the tear film and inflammation or damage to the ocular surface (Craig et al. 2017). Dry eye disease affects between 5% and 50% of people worldwide (Stapleton et al. 2017). In India, the number of people with dry eyes ranges from 15.4% to 45.4% (Rege et al. 2013; Chatterjee et al. 2021).
Age, female gender, Asian ethnicity, contact lens use, environment, drugs, and hormonal imbalances have all been identified as risk factors for dry eye (Wolffsohn et al. 2021). One of the modifiable risk factors for dry eye is contact lens wear. Dryness symptoms are common among contact lens wearers; however, Silicone Hydrogel Contact Lenses (SiH CL) have improved comfort and decreased dryness symptoms as compared to Hydrogel Soft Contact Lenses (Cummings et al. 2020; Wang et al. 2021).
Earlier studies have suggested that contact lens dryness may be caused by various factors, including environmental surroundings, patient-related factors, lens materials and care products, necessitating the use of effective management strategies (Fernández-Jimenez et al. 2021). Hence, when a SiH CL wearer complains of dryness, it may be due to dry eyes or any of the reasons mentioned above. It is important to figure out what is causing the dryness in the first place.
The correlation between signs and symptoms in dry eye patients has been investigated, but not exclusively in SiH CL wearers. The relationship between dry eye symptoms and signs is not linear and varies depending on the type of dry eye disease (Young et al. 2012; Sullivan et al. 2014). However, there is limited understanding about the relationship between the dryness symptoms associated with SiH CL and clinical signs of dry eye. To the best of our knowledge no such study has been done in India. Hence the current study was focused solely on SiH CL to find the association between symptoms and clinical signs of dry eye in SiH CL wearers (Fernández-Jimenez et al. 2021).
MATERIAL AND METHODS
By convenient sampling, 48 SiH CL wearers (mean ± SD age: 28.8 ± 5.0 years, between 18 – 39 years) were recruited from a Hospital in Chennai, India. Subjects were recruited if they were under the age of 40, had been using SiH CL for at least one year on a monthly or biweekly basis, and could understand English. Subjects with any form of contact lens-related complication (except dry eye related complications like conjunctival congestion and staining, filamentary keratitis, mucus clumping, and tear debris); past ocular surgery, lid abnormality, Sjogren’s syndrome, hormonal imbalance, facial nerve palsy, and under medications like anticholinergic effects, anti-histamines, anti-depressants, anti-psychotics, and diuretics, were excluded from the study. The study followed the protocols recommended by the tenets of the Declaration of Helsinki and the methods were approved by the Institutional Review Board and Institutional Ethical Committee of Sri Jayendra Saraswathi Institute of Optometry, number SJSIO/2016/EC/2015/06/07, and informed consents were obtained.
The subjects completed an interviewer-administered questionnaire regarding their personal details, computer usage, contact lens history, systemic & ocular history. Later the subjects underwent an eye examination including visual acuity, objective and subjective refraction, pupil test, cover test, extraocular motility assessment, slit lamp assessment, and retinal examination. To ensure standardization, all of the following tests were performed in the order mentioned. Pre-Lens Tear Film – Non-Invasive Tear Break-up Time (PLTF-NITBUT), contact lens centration and corneal coverage, contact lens post blink movement, contact lens overall fit, grading of palpebral, limbal & bulbar hyperaemia, meibomian glands, and white spots along with film deposits in contact lenses were all measured while the lens was in place (Fernández-Jimenez et al. 2021).
Pre-Ocular Tear Film – Non-Invasive Tear Break-up Time (POTF–NITBUT), tear prism height, Invasive Tear Break-up Time (ITBUT), corneal fluorescein staining (severity and area), conjunctival lens edge staining, blinks/minute, Schirmer test without topical anesthesia were performed after 15 minutes, which was given to re-distribute tear film, after contact lens removal. The flowchart of the methodology is illustrated in Figure 1. The grading of the contact lens and dry eye, its classification, was done in accordance by Young et al. study guidelines, which can be found in Appendix and Table 1 respectively (Young et al. 2012).
The Contact Lens Dry Eye Questionnaire – 8 (CLDEQ-8) was then administered to all the subjects (Chalmers et al. 2012). The cumulative CLDEQ-8 score for all subjects was calculated, and if it was less than 12, it was classified as non-contact lens-related dryness, otherwise as contact lens-related dryness. Spearman’s Correlation analysis was done to test the correlation between CLDEQ-8 score and variables like computer usage (hours), years of lens wear (n), contact lens (hours/day), comfortable contact lens wear (hours/day), PLTF-NITBUT (sec), POTF-NITBUT (sec), invasive TBUT (sec), Schirmer test (mm). Logistic regression was carried out to investigate the relationship between PLTF-NITBUT (sec), POTF-NITBUT (sec), ITBUT (sec), Schirmer test (mm), corneal staining grade, and symptoms of dryness (Fernández-Jimenez et al. 2021).
RESULTS AND DISCUSSION
The percentage of female subjects in the study was 65% (n=31). Best corrected monocular visual acuity of 6/6 and 6/9 was noted in 89.6 % (n=43) and 10.4 % (n=5) of subjects, respectively. Of the 48 subjects, 41 (70 %) used monthly disposable lenses and the remainder used biweekly disposable lenses. There was a moderate association found between contact lens materials and symptoms of dryness (Cramer’s V = 0.55, p < 0.01). Table 1 shows the number of subjects in each diagnostic category of dry eye. There were 47.9 % (n=23) and 52.1 % (n=25) of subjects with non-contact lens related dryness and contact lens related dryness, respectively.
Table 2 summarises the distribution of the 48 subjects in non-contact lens related dryness and contact lens related dryness according to contact lens wearing time (hours/day), duration of comfortable contact lens wearing time (hours/day), and the clinical findings. Table 3 illustrates the distribution of non-contact lens related and contact lens related dryness symptoms in subjects based on the contact lens materials, and dry eye signs. The Spearman’s correlation coefficient (rs) and p value for each factor tested with the CLDEQ-8 Score are shown in Table 4. A strong negative correlation was found between the CLDEQ-8 score and factors like PLTF-NITBUT, POTF-NITBUT, ITBUT, and Schirmer test, which was statistically significant (p< 0.01). A minimal correlation (p< 0.01) was found between contact lens wear (hours/day), and comfortable contact lens wear (hours/day).
Logistic regression was run to determine the effect of dry eye symptoms on the probability of contact lens wearers reporting symptoms of dry eye. The model had five independent variables (PLTF-NITBUT, POTF-NITBUT, ITBUT, Schirmer Test, and Corneal Staining-Severity). The model containing all predictors was statistically significant, c2 (5, n=48) = 44.59, p<0.05, indicating that the model was able to discriminate between subjects with and without dryness. The model showed between 60.5% (Cox and Snell R square) and 80.7% (Nagelkerke R squared) of the variance in dryness symptoms, and correctly identified 93.8% of the subjects. In Table 5, only the PLTF-NITBUT variable had a statistically significant contribution to the model, indicating that for every additional second of PLTF-NITBUT, subjects were 0.29 times less likely to report having complaint of the dryness, controlling for other factors in the model.
Figure 1: Methodology of the study
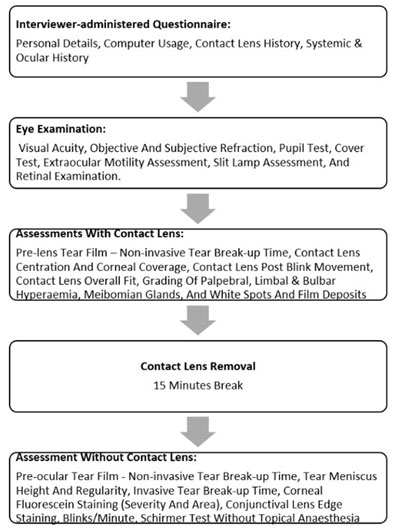
Table 1. Criteria for classification of diagnostic groups of dry eye. Number of subjects in each
diagnostic group among contact lens and non-contact lens related dryness.
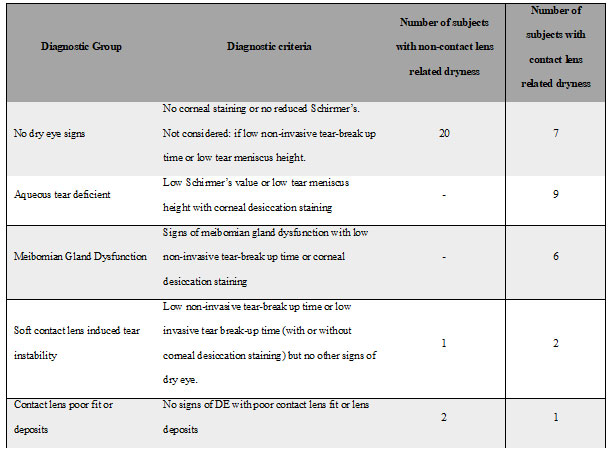
Table 2. Contact lens wearer details and clinical findings
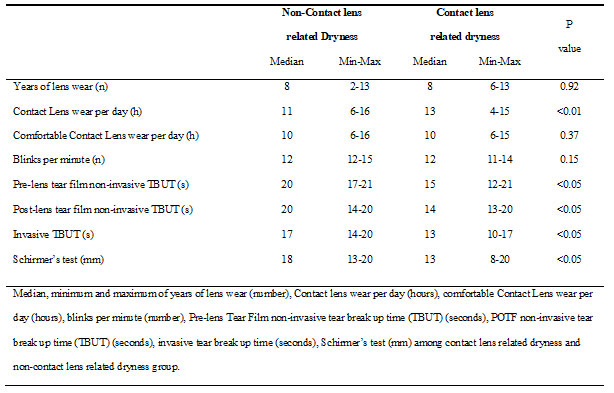
Table 3. Number (percentage) of subjects with non-contact lens-related and contact lens-related dryness1
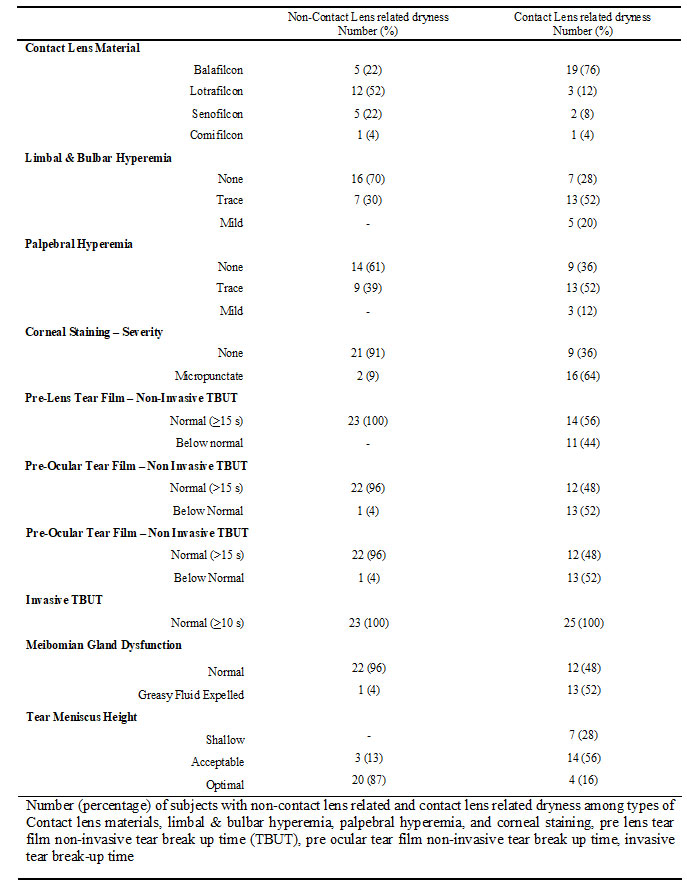
Table 4. Spearman’s correlation coefficient values between CLDEQ-8 scores and factors
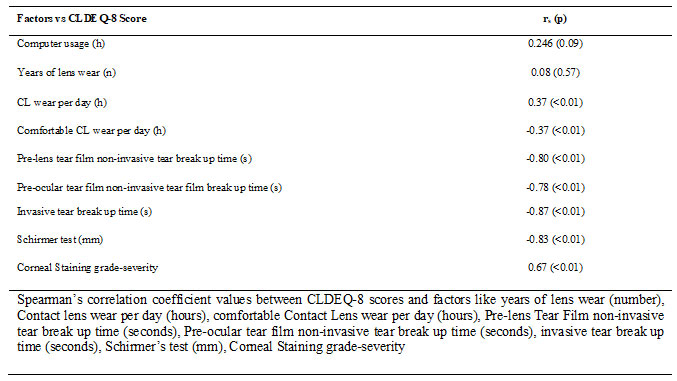
Table 5. Logistic regression analysis
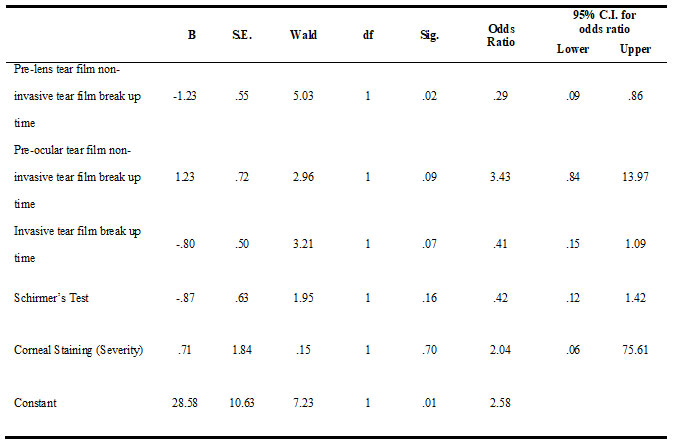
We observed a significant inverse correlation based on statistical analysis, between the symptoms and clinical signs of dry eye in SiH CL wearers. As the CLDEQ-8 score increased, the values of PLTF-NITBUT, POTF-NITBUT, ITBUT, and Schirmer test decreased. The corneal staining grades showed a positive correlation with the CLDEQ-8 scores. We also found that ITBUT, PLTF-NITBUT, and Schirmer test values are significantly associated with the CLDEQ-8 score. The adjusted R2 value is 82.7% of the variance in the CLDEQ-8 score can be explained by PLTF-NITBUT, POTF-NITBUT, ITBUT, Schirmer test, and corneal staining grade. Previous research has shown that the PLTF-NIBUT or ITBUT tests are diagnostic in contact lens wearers, but we found no such attributes in the current study (Molina et al. 2020).
In the present study, 44% of the symptomatic subjects had a lower-than-normal PLTF-NIBUT value (less than 10 secs), and none had an abnormal ITBUT value. Even though the latter test value did not fall into the category of “abnormal,” the CLDEQ-8 score showed a clear association with it. Subjects with contact lens-related dryness had lesser PLTF-NITBUT, POTF-NITBUT, ITBUT, and Schirmer test values of 5 secs, 6 secs, 4 secs, and 5 mm, respectively, then non-contact lens-related dryness subjects (Molina et al. 2020).
However, from a clinical perspective, the signs of dry eye in those with positive symptoms cannot be specified based on the current findings. Our study results indicate that subjects with better tear stability and tear secretion have fewer dry eye symptoms. Thus, clinically, when a SiH CL patient has dry eye symptoms, it could be assumed that the higher the values of tear stability and tear secretion, less symptoms they will have. According to a systematic review by Bartlett et al. there is a low and inconsistent association between dry eye disease and signs (Bartlett et al. 2015). While, our study found a significant relation between the signs and symptoms of dry eye, the difference in findings may be attributed to the questionnaire and study participants (Molina et al. 2020).
The reviewed studies employed questionnaires such as the Ocular Surface Index, 25-item National Eye Institute Visual Function Questionnaire, the Symptom Severity of Discomforts scale, McMonnies’ questionnaire and not the CLDEQ-8 questionnaire. The CLDEQ-8 questionnaire was used in this study because we wanted to identify symptoms of dryness in SiH CL wearers, and it was constructed to assess dry eye symptoms in contact lens users in particular (Chalmers et al. 2012; Molina et al. 2020; (Wolffsohn et al. 2021).
One of the established non-modifiable risk factors for dry eye is female gender (Wolffsohn et al. 2021). Even though the proportion of females in the sample was higher, the male and female ratios in the dry eye diagnostic groups, except for Meibomian gland dysfunction, were relatively similar. As a result, gender as a risk factor in the correlation analysis may not have played a significant role. All subjects in this study who were diagnosed with Aqueous Tear Deficiency and Meibomian gland dysfunction had symptoms of dry eyes. So, we recommended carefully dispensing contact lenses in subjects with low Schirmer value or tear meniscus height, with corneal staining, and signs of Meibomian gland dysfunction with low NITBUT or corneal desiccation staining. A similar recommendation is also given by the study done in a previous study (Molina et al. 2020; Wolffsohn et al. 2021).
In this study, two out of three subjects with Contact Lens Deposits were asymptomatic, implying that clinicians should counsel patients about the importance of maintaining a proper cleaning routine for a healthy ocular condition. In our study, 52% of subjects experienced dryness symptoms while wearing SiH CL which could lead to discomfort. Discomfort with lenses is one of the primary causes of contact lens discontinuation (Pucker and Tichenor 2020).
According to Guillon et al. (2015), a change in the lens care system improved wettability and pre-lens tear film consistency, so this regimen can be attempted in patients who are experiencing contact lens-related discomfort symptoms (Guillon et al. 2015). In our subjects’ lenses, external surface treatment was used in balafilcon A (plasma oxidation), and lotrafilcon B (dense plasma coating), internal treatment was used in senofilcon A (internal wetting agent in the matrix), and no surface treatment was used in comifilcon A. We found a moderate association between the type of contact lens material and symptoms of dryness. Subjects’ wearing balafilcon A had a significant association with dryness symptoms compared to other materials.
Hence, for subjects complaining of dryness, it might be advisable to consider changing the material of the lens to alleviate the dryness symptoms. Contact lens wearers can experience dryness as a result of the lens wetting properties, and this may be attributed to deposits on the lens surface and hydrophobicity (Nichols and Sinnott, 2006). The outcome of vision and comfort during lens wear can be influenced by PLTF thinning. In our study, we observed that every increase in PLTF value resulted in a significant reduction in dry eye symptoms (Pucker and Tichenor 2020).
Earlier studies have found that symptoms of ocular dryness and discomfort in contact lens wearers were more pronounced at the end of the day. It is recommended that contact lens wearers be assessed at the end of the day to best identify symptomatic patients (Begley et al. 2000; Miller et al. 2021). In this study, we found no correlation between the number of hours of contact lens wear per day and the CLDEQ-8 score. However, the subjects were not examined at a fixed time of day, which may be one of the study’s limitations. Another limitation of the present study is that the subjects who were shifted from hydrogel to silicone hydrogel were not noted, as those subjects could have been more symptomatic than old silicone hydrogel users (Miller et al. 2021).
CONCLUSION
The findings of the present study have shown an inverse correlation between dry eye symptoms and clinical signs in SiH CL wearers. The symptoms of dryness were associated with signs of dry eye, a healthy tear film is necessary for comfortable contact lens wear. Before considering refitting or recommending an improvement in the lens care system, eye care professionals should conduct a detailed eye examination.
ACKNOWLEDGEMENTS
The constructive suggestions for this study have been provided by Ms. Ashwini M, Assistant Professor, Department of Optometry, SRM Medical College Hospital & Research Centre.
Funding: Nil
Conflict of Interests: Authors declare no conflicts of interests to disclose.
Data Availablity Statement: The database generated and /or analysed during the current study are not publicly available due to privacy, but are available from the corresponding author on reasonable request.
REFERENCES
Bartlett JD, Keith MS, Sudharshan L, et al. (2015). Associations between signs and symptoms of dry eye disease: a systematic review, Clinical ophthalmology,9(1), 1719–1730. doi:10.2147/OPTH.S89700.
Begley CG, Caffery B, Nichols KK, et al. (2000). Responses of contact lens wearers to a dry eye survey, Optometry and Vision Science, 77(1), 40-6.
Chalmers RL, Begley CG, Moody K, et al. (2012). Contact Lens Dry Eye Questionnaire-8 (CLDEQ-8) and opinion of contact lens performance, Optometry and vision science, 89(10), 1435-42. doi: 10.1097/OPX.0b013e318269c90d.
Chatterjee S, Agrawal D, Sanowar G, et al. (2021). Prevalence of symptoms of dry eye disease in an urban Indian population, Indian Journal of Ophthalmology, 69(5), 1061-1066. doi:10.4103/ijo.IJO_1796_20.
Craig JP, Nichols KK, Akpek EK, et al. (2017). TFOS DEWS II definition and classification report, The ocular surface,15(3), 276-83. doi:10.1016/j.jtos.2017.05.008
Cummings S, Giedd B, and Pearson C (2020). Clinical Performance of a Novel Daily Disposable Soft Contact Lens, Journal of Contact lens Research and Science,4(1), e23-30. doi:0.22374/jclrs.v4i1.39.
Fernández-Jimenez E, Diz-Arias E, and Peral A (2021). Improving ocular surface comfort in contact lens wearers, Contact Lens and Anterior Eye, 25 (1), 101544. doi: 10.1016/j.clae.2021.101544.
Guillon M, Maissa C, Wong S, et al. (2015). Effect of lens care system on silicone hydrogel contact lens wettability. Contact Lens and Anterior Eye, 38(6),435-441. doi: 10.1016/j.clae.2015.06.007.
Miller J, Giedd B, and Subbaraman LN, (2021). Clinical Comparison of a Silicone Hydrogel and a Conventional Hydrogel Daily Disposable Contact Lens, Clinical Ophthalmology,15 (1), 4339–4345. doi: 10.2147/OPTH.S332651.
Molina K, Graham AD, Yeh T, et al. (2020). Not All Dry Eye in Contact Lens Wear Is Contact Lens–Induced, Eye & Contact Lens, 46(4),214-222. doi: 10.1097/ICL.0000000000000661.
Nichols JJ, and Sinnott LT, (2006). Tear film, contact lens, and patient-related factors associated with contact lens–related dry eye. Investigative ophthalmology & visual science, 47(4),1319-1328. doi: 10.1167/iovs.05-1392.
Pucker AD, and Tichenor AA (2020). A review of contact lens dropout, Clinical Optometry,12,85-94. doi: 10.2147/OPTO.S198637.
Rege A, Kulkarni V, Puthran N, et al. (2013). A clinical study of subtype-based prevalence of dry eye. Journal of clinical and diagnostic research, 7(10):2207-2210. doi: 10.7860/JCDR/2013/6089.3472.
Stapleton F, Alves M, Bunya VY, et al. (2017). TFOS DEWS II Epidemiology Report, Ocular Surface, 15(3), 334–365. doi: 10.1016/j.jtos.2017.05.003.
Sullivan BD, Crews LA, Messmer EM, et al. (2014). Correlations between commonly used objective signs and symptoms for the diagnosis of dry eye disease: clinical implications, Acta ophthalmologica, 92(2),161-166. doi: 10.1111/aos.12012.
Wang MT, Muntz A, Mamidi B, et al. (2021). Modifiable lifestyle risk factors for dry eye disease. Contact Lens and Anterior Eye, 44(6), 101409. doi: 10.1016/j.clae.2021.01.004.
Wolffsohn JS, Wang MT, Vidal-Rohr M, et al. (2021). Demographic and lifestyle risk factors of dry eye disease subtypes: a cross-sectional study, The Ocular Surface, 21 (1), 58-63. doi:10.1016/j.jtos.2021.05.001.
Young G, Chalmers R, Napier L, et al. (2012). Soft contact lens-related dryness with and without clinical signs, Optometry and Vision Science, 89(8),1125-1132. doi:0.1097/OPX.0b013e3182640af8.


