1 Department of Pediatric Dentistry and Orthodontics, College of Dentistry,
King Saud University, Riyadh, Saudi Arabia.
2College of Dentistry, King Saud University, Riyadh, Saudi Arabia.
Corresponding author email: e_shayea@hotmail.com
Article Publishing History
Received: 20/06/2021
Accepted After Revision: 15/08/2021
The purpose of the present study is to undertake an up-to-date assessment of the knowledge and skills of Saudi orthodontists, regarding the time frame required before the commencement of orthodontic tooth movement, and their views of best orthodontic management of traumatized teeth. A cross-sectional study was performed by utilizing survey research techniques. The short self-administered questionnaire used here consisted of demographic data, clinician’s opinion of the most appropriate time frame to receive orthodontic treatment, and the clinician’s approach and management for patients with different types of traumatized teeth cases. This questionnaire was mailed electronically to all Saudi orthodontists. A total of 166 orthodontists participated in the study.
A period of three months was recommended by most participants as necessary before moving crown and crown/root-fractured teeth, root canal treated teeth, and teeth with injury to the periodontium. On the other hand, the survey shows that the best time to initiate orthodontic movement for patients with root-fractured teeth was after twelve months. The majority of respondents prefer performing regular radiographic examination, opted for reducing the applied orthodontic forces, and performing regular pulp vitality tests as the best follow-up management of a traumatized teeth with different types of dental trauma. The study reveals the imperativeness of performing an accurate history documentation of any previous dental trauma and to make such an inquiry a major part of every orthodontic diagnosis. Lastly, when dealing with traumatized teeth, it is important to perform a thorough clinical and radiographic evaluation before and during the orthodontic treatment.
Dental Trauma, Traumatized Dentition, Orthodontic Management, Orthodontic Tooth Movement
Eman I.A, Lina M.A, Rana M.A, Norah A.A, Rahaf H.A. Orthodontic Management of Traumatized Teeth: Saudi Orthodontists’ Perspectives. Biosc.Biotech.Res.Comm. 2021;14(3).
Eman I.A, Lina M.A, Rana M.A, Norah A.A, Rahaf H.A. Orthodontic Management of Traumatized Teeth: Saudi Orthodontists’ Perspectives. Biosc.Biotech.Res.Comm. 2021;14(3). Available from: <a href=”https://bit.ly/3jLZupE“>https://bit.ly/3jLZupE</a>
Copyright ©Eman et al., This is an open access article distributed under the terms of the Creative Commons Attribution License (CC-BY) https://creativecommns.org/licenses/by/4.0/, which permits unrestricted use distribution and reproduction in any medium, provide the original author and source are credited.
INTRODUCTION
Dental trauma is a common, inevitable and serious oral health problem among both adolescents and children with boys being more affected than girls (Chadwick and Pendry 2004; Al-Malik 2009; Damé-Teixeira et al. 2013; Tewari et al 2020; Abdel Malak et al 2021).Although there are limited reports available on the epidemiology of dental injuries in Saudi Arabia, a review of the literature shows various prevalence rates for traumatic dental injuries in individuals younger than 18; with some arguing for as low a range as 5%, and others as high as 17.5% occurrence (Chadwick and Pendry 2004; Azami-Aghdash et al. 2015; Van Gorp et al. 2020).
Furthermore, dental trauma is a frequent finding in patients with orthodontic treatment needs. It is estimated that over 10% of young patients admitted for orthodontic treatment has a history of dental trauma (Bauss et al. 2004). Since the malocclusion is considered as the third common oral health problem in dental public health priorities worldwide, specific malocclusions, such as occlusal relationship, increased overjet with prominent incisors, insufficient lip closure are predisposing factors that require early orthodontic intervention necessary to reduce the risk of dental trauma (Petti 2015; Alhammadi et al. 2018; Batista et al. 2018; Van Gorp et al. 2020).
Such kinds of dental trauma, most frequently, involve the upper incisors that usually cause esthetic and phonetic problems, which negatively impacts the quality of life and psychosocial distress of individuals (Kindelan et al. 2008; Fakhruddin et al. 2008; Enabulele et al. 2016; Van Gorp et al. 2020). Nonetheless, orthodontic tooth movement (OTM) has possible undesirable effects such as root resorption. Thus, excessive number of orthodontic forces combined with previous dental trauma may further increase the susceptibility to root resorption (Poi et al. 2007; Kindelan et al. 2008).
Dental injuries vary from simple fractures affecting the enamel to a more complex fractures that could complicate and delay orthodontic treatment. Furthermore, since the rate of trauma in patients seeking an orthodontic treatment is increasing, a comprehensive dental history along with radiographic and clinical examinations are essential to a successful orthodontic movement of traumatized teeth before and during the course of any orthodontic treatment.
Each case should be evaluated and treated based on several factors including the patient’s age, dental and anatomical development status, general health of the patient, previous orthodontic treatment, severity, time, and type of the trauma (Bauss et al. 2004; Poi et al. 2007; Kindelan et al. 2008; Owtad et al. 2015; Joybell et al. 2019).
Although no standard guidelines have been established in regards to the time required before the initiation of OTM and for the appropriate management of traumatized teeth cases, the literature agree that there is a different observation period for each type of trauma, depending on the severity of the injury and the knowledge and skills of the physician (Bauss et al. 2004; Malmgren and Malmgren 2007; Kindelan et al.2008; Owtad et al. 2015).
However, there has been limited research conducted to further explore possible adverse effects of traumatized teeth undergoing OTM, thus making definitive conclusions hard to draw. Hence, the aim of this study is to obtain an up-to-date assessment of the knowledge and skills of Saudi orthodontists towards the time required before the initiation of OTM, and the best orthodontic management of traumatized teeth.
MATERIAL AND METHODS
For the purpose of data collection, a survey is designed as a useful method in the present cross-sectional study. The study was approved by the Institutional Review Board (IRB) at the College of Dentistry, King Saud University [E-20-5111]. The short-self-administered questionnaire consisted of 11 questions, including demographic data questions such as age, job title, years of practice, and type of practice, followed by descriptive questions to evaluate the clinician’s opinion on the most appropriate time for receiving orthodontic treatment of patients with different types of traumatized tooth cases.
Furthermore, additional questions are designed to analyze the clinician’s approach and treatment management for different dental trauma cases. This questionnaire was mailed electronically in a Google Forums format, a web-based survey, with a link provided to all of orthodontists and orthodontic resident members of Saudi Commission for Health Specialities and the Saudi Orthodontic Society for a period between July, 2020 to Octoer, 2020.
A Pilot study consisting of 20 participants was conducted to validate the questionnaire and modifications were done accordingly and was reviewed and assessed by an orthodontist. The entire procedure and the aim of the study were thoroughly explained via the email to participants who voluntarily agreed to participate in the study. The study ensured the anonymous identity of the participants and data was kept protected to ensure confidentiality. The responses were assessed to determine the knowledge of the clinicians regarding orthodontic management and movement of traumatized teeth.
For statistical analysis, the collected data were recorded and analyzed by using SPSS version 26.0.0 (IBM Corporation, Armonk, NY, USA). G*Power software analysis was used to calculate the statistical power and estimate the sample size for the studied group. A sample size of 148 out of the total number of Saudi orthodontists was needed to achieve a 95% confidence level (AlBaker et al. 2017).
However, to avoid a low response rate which may affect the sample size, a survey of a larger sample was conducted which should be more than that calculated in the assumption. Frequency distributions and descriptive statistics for age, gender, years of practice, type of practice, number of patients and patient age range with dental trauma treated in their practice were calculated.
In addition, a comparison and cross tabulation of participants’ job title and inquiry about previous dental trauma during initial orthodontic assessment of patients was conducted. Furthermore, another cross tabulation of participants’ job title and their responses regarding the most appropriate time to initiate OTM for patients with different types of dental trauma were investigated.
Both investigations were conducted by using Pearson’s chi-squared test. In all statistical assessments performed, the level of significance was recognized at 95% level of confidence (p<0.05) to indicate the statistical significance between the studied variables.
RESULTS AND DISCUSSION
A total of 166 Orthodontists participated in this study consisting of 91 females and 75 males, with a response rate of 70%. All trainees with less than one year of experience were excluded. Demographic characteristics of the participants were presented in Table 1. More than half of the participants were females (54.8%), and the majority were in the age group of 31-40 years (43.9%), followed by the age group of 41-50 years (22.3%). The university hospital setting was the main practice area of the participants (33.1%).
Furthermore, participants were categorized according to their job title and the number of years they have been practicing as shown in Table 1. Thus, those who were consultant orthodontists and have been practicing for 6-10 years were the majority of the participants (48.8%, and 23.5%, respectively). On the other hand, the lowest percentage of participants were among general practitioners (GPs) with interest in orthodontics, and those who have been practicing for 1-2 years (1.8%, and 12.6%, respectively). In addition, most of the participants reported seeing patients with history of dental trauma in the previous 12 to 18 months (87.3%).
The largest group of participants reported treating a range of 1 to 3 patients with history of dental trauma in their previous 12 to 18 months (59%). The frequency distribution of patients’ age, at the start of orthodontic treatment following trauma revealed that the patients from 11 to 15 years old with a history of dental trauma had the highest percentage of orthodontic visitations than any other patients groups, which was 52% (n=79). On the other hand, patients who were more than 31 years of age had the lowest percentage (2%, n=3) (Table 1).
Table 1. Demographic characteristics of the participants
| Socio-demographic Participants Characteristics | N | % | |
| Gender | Female
Male |
91
75 |
54.8%
45.2% |
| Age Groups | 30 and less
31-40 41-50 51-60 Above 60 |
28
73 37 23 5 |
16.9%
43.9% 22.3% 13.9% 3% |
| Job Title | Consultant orthodontists
Specialist orthodontists Orthodontic residents GP with training in orthodontics GP with interest in orthodontics |
81
47 23 12 3 |
48.8%
28.3% 13.9% 7.2% 1.8% |
| Years of Experience | 1-2 years
3-5 years 6-10 years 11-20 years More than 20 years |
21
38 39 36 32 |
12.6%
22.9% 23.5% 21.7% 19.3% |
| Working Sector | University clinical setting
Hospital setting Private practice Primary care Other |
55
52 48 7 4 |
33.1%
31.3% 29% 4.2% 2.4% |
| Number of patients seen with history of dental trauma in previous 12-18 months | None
1-3 patients 4-6 patients 7-12 patients More than 12 patients |
21
98 25 10 12 |
12.7%
59% 15.1% 6% 7.2% |
| patients’ age, at the start of orthodontic treatment following trauma | 7-10 years old
11-15 years old 16-20 years old 21-30 years old Above 31 years old |
26
79 36 8 3 |
17%
52% 23.7% 5.3% 2% |
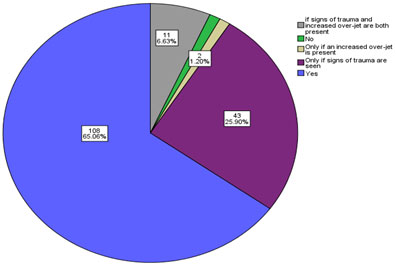
It is clear from the results that the majority of the participants reported a routine inquiry about any previous dental trauma during their initial orthodontic assessment (65.1%, n=108) as shown in the pie chart (Figure 1). On the other hand, 25.9% of the participants inquire about history of dental trauma only for patients with signs of trauma. Other participants inquired about history of dental trauma only for patients with clear signs of trauma and an increased overjet (6.6%). The minority of the participants were those who do not ask about any previous dental trauma and those who ask only if an increased overjet was clearly present, and both had equal percentages of 1.2% (n=2) (Figure 1).
Figure 1: Pie chart showing frequency distribution of participants’ enquiry about a history of previous dental trauma during initial orthondoctic assesment of patients
According to the survey, responses regarding the most appropriate time to initiate OTM for patients with different types of dental trauma were presented in different charts in Figure 2. These responses were as follows: most of the participants prefer to wait for three months before moving crown and crown/ root-fractured teeth (n=83; 50%). Similarly, the majority of the participants (n=101; 60.8%) reported waiting three months before moving traumatized teeth with minor damage to the periodontium such as concussion, and before moving traumatized teeth with moderate to severe injury to the periodontium such as intrusion luxation (n=64; 38.5%).
On the other hand, eighty-nine participants believed that the best time to initiate OTM for patients with root-fractured teeth was after twelve months (53.6%). For teeth treated with root canal treatment (RCT) due to trauma, the majority of the participants prefer to wait three months before moving a tooth (n=71; 42.7%), followed by a number of participants who prefer an immediate orthodontic movement of RCT teeth (n=62; 37.3%). Table 2 shows that there is statistically significant relationship between participants’ job title and the predisposition to inquire about dental traumas during initial orthodontic assessment of patients (χ2 = 34.1, P = 0.005, P <0.05).
It revealed that orthodontic residents, specialists, and consultants are more inclined to ask about previous dental trauma. Similarly, the results also showed that there was a statistically significant association between participants’ job title and their responses regarding the most appropriate time to initiate OTM for patients with different types of dental trauma. The majority of orthodontic residents, specialists, and consultants were in agreement in most of their responses as shown in Table 3.
Table 2. Cross Tabulation of participants’ job tile and inquiry about previous dental trauma during initial orthodontic assessment of patients.
| Inquiry about any previous dental trauma during initial orthodontic assessment of patients. | Chi-Square Tests | ||||||
| Job Title | No | Only if signs of trauma are seen | Only if an increased over-jet is present | if signs of trauma and increased over-jet are both present | Yes | Value | P.value |
| GPs interested in
Orthodontics |
0 | 1 (33.3%) | 2 (66.7%) | 0 | 0 |
34.1 |
0.005** |
| GPs training in orthodontics | 2(16.7%) | 4 (33.3%) | 0 | 0 | 6 (50%) | ||
| Consultant Orthodontist | 0 | 22 (27.2%) | 0 | 6 (7.4%) | 53 (65.4%) | ||
| Specialist Orthodontist | 0 | 12 (25.5%) | 0 | 5 (10.6%) | 30 (63.8%) | ||
| Resident Orthodontist | 0 | 4 (17.4%) | 0 | 0 | 19 (82.6%) | ||
| Total | 2 (1.2%) | 43 (25.9%) | 2 (1.2%) | 11 (6.6%) | 108(65.1%) | ||
Figure 2: Different charts for the participants’ responses regarding the most appropriate time to initiate orthodontic tooth movement for patients with different types of dental trauma.

Table 3. Cross Tabulation of participants’ job tile and their responses regarding the most appropriate time to initiate orthodontic tooth movement for patients with different types of dental trauma.
| Trauma Type | Job Title | Immediately | 3 mon. | 12 mon. | I don’t know | Refer patients to other orthodontists | Chi-square | Sig. |
| Crown and
crown/root fractures |
GP interested in
orthodontics |
2 (66.7%) | 0 | 0 | 0 | 1 (33.3%) | 37.889a | 0.002 |
| GPs training in
orthodontics |
2 (16.7%) | 4 (33.3%) | 2 (16.7%) | 2 (16.7%) | 2 (16.7%) | |||
| Consultant Orthodontist | 7 (8.6%) | 41 (50.6%) | 24 (29.6%) | 7 (8.6%) | 2 (2.5%) | |||
| Specialist Orthodontist | 7 (14.9%) | 27 (57.4%) | 13 (27.7%) | 0 | 0 | |||
| Orthodontist Resident | 4 (17.4%) | 11 (47.8%) | 5 (21.7%) | 3 (13%) | 0 | |||
| Root
Fractures |
GPs interested in
orthodontics |
2 (66.7%) | 0 | 0 | 0 | 1 (33.3%) | 29.684a | 0.02 |
| GPs training in
orthodontics |
1 (8.3%) | 1 (8.3%) | 5 (41.7%) | 3 (25%) | 2 (16.7%) | |||
| Consultant Orthodontist | 7 (8.6%) | 12 (14.8%) | 49 (60.5%) | 10 (12.3%) | 3 (3.7%) | |||
| Specialist Orthodontist | 6 (12.8%) | 8 (17%) | 28 (59.6%) | 4 (8.5%) | 1 (2.1%) | |||
| Orthodontist Resident | 5 (21.7%) | 6 (26.1%) | 7 (30.4%) | 4 (17.4%) | 1 (4.3%) | |||
| Minor damage to the periodontium (concussion) | GPs interested in
orthodontics |
2 (66.7%) | 0 | 0 | 0 | 1 (33.3%) | 36.859a | 0.002 |
| GPs training in
orthodontics |
1 (8.3%) | 7 (58.3%) | 1 (8.3%) | 2 (16.7%) | 1 (8.3%) | |||
| Consultant Orthodontist | 18 (22.2%) | 54 (66.7%) | 7 (8.6%) | 1 (1.2%) | 1 (1.2%) | |||
| Specialist Orthodontist | 14 (29.8%) | 28 (59.6%) | 4 (8.5%) | 1 (2.1%) | 0 | |||
| Orthodontist Resident | 7 (30.4%) | 12 (52.2%) | 2 (8.7%) | 2 (8.7%) | 0 | |||
| Moderate to
severe injury to the periodontium (Intrusion) |
GPs interested in
orthodontics |
2 (66.7%) | 0 | 0 | 0 | 1 (33.3%) | 58.243a | 0.000 |
| GPs training in
orthodontics |
6 (50%) | 0 | 1 (8.3%) | 3 (25%) | 2 (16.7%) | |||
| Consultant Orthodontist | 19 (23.5%) | 37 (45.7%) | 21 (25.9%) | 3 (3.7%) | 1 (1.2%) | |||
| Specialist Orthodontist | 16 (34%) | 13 (27.7%) | 17 (36.2%) | 1 (2.1%) | 0 | |||
| Orthodontist Resident | 2 (8.7%) | 14 (60.9%) | 5 (21.7%) | 2 (8.7%) | 0 | |||
| A tooth
treated with RCT due to trauma |
GPs interested in
orthodontics |
2 (66.7%) | 0 | 0 | 0 | 1 (33.3%) | 50.926a | 0.000 |
| GPs training in
orthodontics |
2 (16.7%) | 4 (33.3%) | 1 (8.3%) | 3 (25%0 | 2 (16.7%) | |||
| Consultant Orthodontist | 36 (44.4%) | 38 (46.9%) | 4 (4.9%) | 2 (2.5%) | 1 (1.2%) | |||
| Specialist Orthodontist | 13 (27.7%) | 22 (46.8%) | 10 (21.3%) | 2 (4.3%) | 0 | |||
| Orthodontist Resident | 9 (39.1%) | 7 (30.4%) | 5 (21.7%) | 2 (8.7%) | 0 |
*Sig – approximate significance, where P-value at 0.05 level
The participants’ responses regarding the best management of a traumatized tooth with different types of dental trauma during OTM were presented in Figure 3. The majority of the participants preferred to perform regular radiographic examination, followed by reducing orthodontic forces when treating cases with crown and crown/root fracture (65.7%, and 57.8%, respectively), root fracture (70%, and 42.8%, respectively), concussion (56%, and 54.8%, respectively), and intrusion luxation (69.3%, and 57.2%, respectively).
In addition, performing regular pulp vitality test was reported among the participants when managing a traumatized tooth with crown and crown/root fracture (39.2%), root fracture (34.3%), concussion (28.9%), and cases with intrusion luxation (43.4%). For management of traumatized teeth treated with RCT, more than half of the participants preferred to perform regular radiographic examination (53%), while 44% of the participants preferred to treat patients with RCT the same way they treat non-traumatized cases.
Other methods of management, with lesser percentages, were reported among participants. Such methods included reducing the orthodontic forces (41%), short recall intervals (19%), regular pulp vitality tests (16.3%), and leave the tooth off the arch wire (8.4%). For management of ankylosed teeth, more than half of the participants opted for leaving the tooth off the arch wire (n = 94, 56.6%), and performing regular radiographic examination (n= 48, 28.9%).
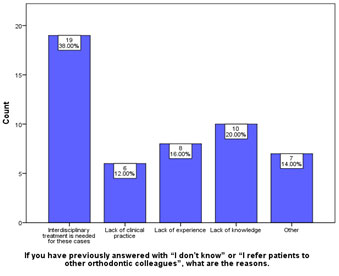
Furthermore, the participants who answered the two questions (the most appropriate time to initiate orthodontic movement, and the best orthodontic management of a traumatized tooth with different types of dental trauma) with answers such as “I don’t know” or “I refer patients to other orthodontic colleagues”, were asked to kindly state their reasons. It was found that 38% of the participants referred patients to their colleagues because they believed that interdisciplinary treatment was needed, 20% of responses were due to lack of knowledge, 16% of responses were due to lack of experience, and the last reason for referral was due to lack of clinical practice which was 12% (Figure 4).
The participants’ responses regarding the best management of a traumatized tooth with different types of dental trauma during OTM were presented in Figure 3. The majority of the participants preferred to perform regular radiographic examination, followed by reducing orthodontic forces when treating cases with crown and crown/root fracture (65.7%, and 57.8%, respectively), root fracture (70%, and 42.8%, respectively), concussion (56%, and 54.8%, respectively), and intrusion luxation (69.3%, and 57.2%, respectively). In addition, performing regular pulp vitality test was reported among the participants when managing a traumatized tooth with crown and crown/root fracture (39.2%), root fracture (34.3%), concussion (28.9%), and cases with intrusion luxation (43.4%).
For management of traumatized teeth treated with RCT, more than half of the participants preferred to perform regular radiographic examination (53%), while 44% of the participants preferred to treat patients with RCT the same way they treat non-traumatized cases. Other methods of management, with lesser percentages, were reported among participants. Such methods included reducing the orthodontic forces (41%), short recall intervals (19%), regular pulp vitality tests (16.3%), and leave the tooth off the arch wire (8.4%). For management of ankylosed teeth, more than half of the participants opted for leaving the tooth off the arch wire (n = 94, 56.6%), and performing regular radiographic examination (n= 48, 28.9%).
Furthermore, the participants who answered the two questions (the most appropriate time to initiate orthodontic movement, and the best orthodontic management of a traumatized tooth with different types of dental trauma) with answers such as “I don’t know” or “I refer patients to other orthodontic colleagues”, were asked to kindly state their reasons. It was found that 38% of the participants referred patients to their colleagues because they believed that interdisciplinary treatment was needed, 20% of responses were due to lack of knowledge, 16% of responses were due to lack of experience, and the last reason for referral was due to lack of clinical practice which was 12% (Figure 4).
Figure 3: Different charts for the participants’ responses regarding the best management of a traumatized tooth with different types of dental trauma during orthodontic movement.
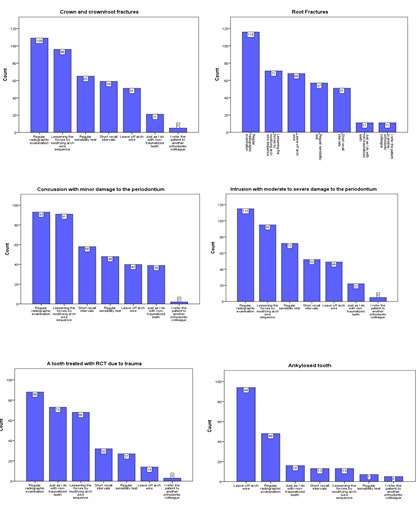
Figure 4. The participants’ responses for the reasons why they refer patients with a history of different types of dental trauma to other orthodontic colleagues.
The evaluation and rather careful monitoring of the traumatized tooth before and during OTM are very important in cases in which emergency management is required to enhance the prospects of successful prognosis. There are limited number of researches available on orthodontic management of traumatized teeth in Saudi Arabia. Hence, the purpose of the present study is to obtain current assessment of the knowledge and skills of Saudi orthodontists towards the time required before the initiation of OTM, and the best orthodontic management of traumatized teeth.
The evaluation of the traumatized tooth must include: timing of the injury, any previously performed treatment, pulp vitality, and pulp sensibility tests (thermal and electric) to determine the state of pulpal health by assessing the condition of the dental pulp nerves and blood flow.
In addition, thorough evaluation including transillumination of enamel infraction lines in traumatized teeth, examination for any sinus tracts or swelling, investigation of tooth mobility, in both a horizontal and vertical directions, palpation over the tooth apex for any tenderness, and percussion tests diagnosing ankylosis and root fracture are all needed and imperative for comprehensive diagnosis and treatment plan (Kindelan et al. 2008; Batista et al. 2018).
In the present study, most of the participants reported having treated patients with history of dental trauma in the previous 12-18 months. In the research design, this period was categorized as a relatively long enough to ensure that orthodontists were able to see patients with traumatic cases, as this survey was carried out during the Covid-19 lockdown.
Furthermore, it was found that the patients from 11 to 15 years old with a history of dental trauma had the highest percentage of orthodontic visitations than any other patients’ groups. This finding is consistent with the conclusion drawn by other researchers who found that the dental trauma is common among children and adolescents seeking orthodontic treatment (Bauss et al. 2004; Kindelan et al. 2008; Damé-Teixeira et al. 2013; Azami-Aghdash et al. 2015).
During the initial orthodontic assessment of patients, more than half of the participants routinely inquire about their patients’ dental trauma history, which underscores the importance of appropriate history investigation, and hence enabling orthodontists to provide an adequate management course customized according to each case’s need, to better prepare for any possible future complications, and to enhance the prognosis of traumatized teeth during OTM as reported in the literature (Kindelan et al. 2008; Duggal et al. 2015).
Moreover, 25.9% of the participants do inquire about their patients’ dental trauma history only if signs of trauma are evident and observable. Similar finding was illustrated by Sandler et al. (2019) who concluded a wide variation in the orthodontic management of traumatized teeth among UK-based orthodontists (Sandler et al., 2019). Fewer participants in the study inquire about history of trauma if both signs of trauma and increased overjet are present (6.6%), while others inquire only if there is an increase in overjet (1.2%).
This finding could be attributed to the fact that an increased overjet of more than 3mm is one of the predisposing factors that require early orthodontic intervention in order to reduce the risk of dental trauma (Petti 2015; Alhammadi et al. 2018; Batista et al. 2018).
The significant relationship in the present study between participants’ job title and their tendency to inquire about previous dental trauma during initial orthodontic assessment of patients indicates that those with more experience are more inclined to ask about previous dental traumas more frequently compared to those with less experience or less training in orthodontics. Some of the consequences of dental trauma investigated in this research included crown fracture, root fracture, RCT of traumatized teeth, ankylosis, concussion, and intrusion luxation.
In regards to the time required before the initiation of OTM for traumatized teeth, it has been agreed upon in the literature that there is a different observation period for each type of trauma, depending on the severity of the injury based on the expert opinion (Malmgren and Malmgren 2007; Kindelan et al. 2008; Duggal et al. 2015; Sandler et al. 2019).
When the participants were asked about the time required before the initiation of OTM in cases of crown, crown\root fractures, teeth with concussion, and teeth with intrusion luxation, the majority agreed that three months are sufficient observation period prior to the initiation of an active OTM in order to avoid any serious complication such as inflammation and pulpal necrosis. Moreover, most of the participants reported that teeth with root fractures and ankylosed teeth due to severe traumatic injuries should have 12-months observation period prior to the orthodontic treatment.
These findings are consistent with the guidelines and recommendations reported by several researchers, except for intrusion luxation, for which the recommended observation period prior to OTM is 6-12 months if no ankylosis can be detected. On the other hand, different responses were reported when participants were asked about the observation period prior to OTM needed for root canal treatment of closed apex teeth due to trauma (Zachrisson and Jacobsen 1974; Malmgren and Malmgren 2007; Kindelan et al. 2008; Hermann et al. 2012; Duggal et al. 2015; Sandler et al., 2019).
Most of the participants (42.7%) believed that a 3-months of observation following a well-cleaned, good quality obturated root filling, and good seal are adequate to commence OTM, while 37.3% of the participants recommended an immediate OTM of root canal treated teeth. These findings are consistent with previous findings in the literatures (Drysdale et al.1996; Sandler et al. 2019). They, however, contradict other studies that concluded a period of one year was recommended prior to commencement of orthodontic treatment and necessary to increase the possibility of complete healing without ankylosis (Drysdale et al. 1996; Malmgren and Malmgren 2007).
In the present study, statistically significant differences were found among the participants opinions regarding the recommended observation period prior to the initiation of an active OTM for patients with different types of dental trauma. In contrast to GPs interested and trained in orthodontics, the majority of orthodontic residents, specialists, and consultants were in agreement of most of their responses as observed in Table 3. This could be attributed to the lack of knowledge and clinical judgment of the GPs compared to those who have specialized and experienced in the field of orthodontics (Duggal et al. 2015).
The majority of responses in this study opted toward performing regular radiographic examination, reducing the applied orthodontic forces, and performing regular pulp vitality tests as the best follow-up management of a traumatized tooth with different types of dental trauma, including crown and crown/root fractures, root fracture, minor and severe damage to the periodontium, during OTM.
This finding is consistent with the conclusion of several studies and it could be explained and supported by the fact that traumatized teeth or teeth showing signs of pretreatment root resorption undergoing OTM are known to have a low response to vitality testing, high rate of pulpal canal obliteration, and high risk of increased root resorption as a result of orthodontic forces (Duggal et al. 2015).
Hence, it has been recommended to follow-up with these patients after being treated orthodontically with regular radiographic examination and pulp vitality tests at consecutive intervals (Brin et al. 1991; Malmgren and Malmgren 2007; Kindelan et al. 2008; Duggal et al. 2015; Jaradat and Rahhal 2016; Sandler et al. 2019).
Furthermore, most of the participants responded that taking regular radiographic examination is the proper management of traumatized teeth treated with RCT. This finding corresponds with Malmgren et al. (2007), who advocate radiographic monitoring by taking radiographs of root filled teeth before OTM begins, and to be repeated in six months after the start of orthodontic therapy (Malmgren et al. 2007).
In contrast, 44% of the participants reported that managing traumatized teeth treated with RCT should be dealt with same way they treat non-traumatized teeth. Similar finding was reported by Sandler et al. (2019).This can be attributed to the conclusion that there is no significant difference in the root resorption in both root canal treated teeth and vital teeth subjected to the same orthodontic forces (Esteves et al. 2007; Sandler et al. 2019).
Nonetheless, when the participants were asked about the management of root fractures and ankylosed teeth due to severe traumatic injuries, the majority of responses were to perform regular radiographic examination for root fractured tooth, and to leave off arch wire for ankylosed tooth (70%, and 56.6%, respectively). These findings are similar to the previously reported studies which concluded that a long-term follow-up of applying light orthodontic forces and radiographic evaluation are recommended for root fractured and ankylosed cases (Kindelan et al. 2008; Bauss et al.
2008; De Souza et al.2015; Sandler et al. 2019). In contrast to the previous groups that answered with specific treatment plans and clear management course of OTM, fifty participants (30%) have answered with “I don’t know” or “I refer patients to other orthodontic colleagues” (Sandler et al. 2019).
In addition, 38% of the participants preferred to refer such patients to their colleagues due to the fact that interdisciplinary treatment is needed for such cases, while 20% and 16% of participants either had insufficient knowledge or lack of sufficient experience, respectively. This illustrates the lack of guidelines in the literature regarding orthodontic movement of traumatized teeth, and highlights the necessity for further increasing the orthodontist’ awareness regarding the management techniques required for different cases of traumatized teeth.
Finally, it is necessary to mention that the present study has some limitations. Most importantly is the small sample size and sample distribution representing the Saudi orthodontists’ knowledge and skills towards the time required before the initiation of OTM, and the best orthodontic management of traumatized teeth.
Therefore, further studies are required to increase the sample size and improve sample distribution to include other regions of Saudi Arabia and larger number of Saudi orthodontists. In addition, another study is needed to assess how to orthodontically manage different types of traumatized teeth such as alveolar fractures, extrusion luxation, avulsed teeth, immature traumatized teeth, and auto-transplanted teeth (Sandler et al. 2019).
CONCLUSION
The findings of the present study suggests that it is imperative for any orthodontist to perform an accurate history investigation about any previous dental trauma, and make such an inquiry a major part of every orthodontic diagnosis. In addition, when dealing with traumatized teeth, it is necessary to perform a thorough clinical and radiographic evaluation before and during the orthodontic treatment.
Some of the traumatized teeth require endodontic approaches, while others need splinting or even surgical or orthodontic repositioning such as intruded traumatized teeth before initiating the orthodontic treatment. It is; therefore, essential to evaluate any traumatic teeth for pulp vitality, root resorption, and signs of ankylosis that may complicate the course of orthodontic treatment. In regard to the time required before initiating orthodontic movements of traumatized teeth cases, it has been concluded that there is a different observation period for each type of trauma, depending on the severity of the injury based on expert evaluation.
ACKNOWLEDGEMENTS
The authors would like to thank Prof. Abdullah Alhammadi for his help and valuable contribution in this research.
Conflict of Interest: None we certify that this work has not been published previously and is not under consideration by another journal.
REFERENCES
Abdel Malak C, Chakar C, Romanos A, et al. (2021) Prevalence and Etiological Factors of Dental Trauma among 12- and 15-Year-Old Schoolchildren of Lebanon: A National Study. ScientificWorldJournal. 2021:5587431. doi: 10.1155/2021/5587431.
AlBaker AA, Al-Ruthia YSH, AlShehri M, et al. (2017) The characteristics and distribution of dentist workforce in Saudi Arabia: A descriptive cross-sectional study. Saudi Pharm J. 25(8):1208-1216.
Alhammadi MS, Halboub E, Fayed MS, et al. (2018) Global distribution of malocclusion traits: A systematic review. Dental Press J Orthod. 23(6):40 e41–40 e10.
Al-Malik M (2009) Oral injuries in children attending a hospital in Saudi Arabia. J Maxillofac Oral Surg 8(1), 34–39.
Azami-Aghdash S, Ebadifard Azar F, Pournaghi Azar F, et al. (2015) Prevalence, etiology, and types of dental trauma in children and adolescents: systematic review and meta-analysis. Med J Islam Repub Iran. 29(4):234. PMID: 26793672; PMCID: PMC4715389.
Batista KBSL, Thiruvenkatachari B, Harrison JE, et al. (2018) Orthodontic treatment for prominent upper front teeth (class II malocclusion) in children and adolescents. Cochrane Database Syst Rev.3:CD003452.
Bauss O, Rohling J, and Schwestka‐Polly R (2004) Prevalence of traumatic injuries to the permanent incisors in candidates for orthodontic treatment. Dent Traumatol. 20:61–6.
Bauss O, Röhling J, Sadat-Khonsari R, et al. (2008) Influence of orthodontic intrusion on pulpal vitality of previously traumatized maxillary permanent incisors. Am J Orthod Dentofac Orthoped. 134(1):12-7.
Brin I, Ben-Bassat Y, Heling I, et al. (1991) The influence of orthodontic treatment on previously traumatized permanent incisors. Eur J Orthod. 13(5):372–377.
Chadwick B, and Pendry L (2004) Children’s Dental Health in the United Kingdom, 2003. Non-carious Dental Conditions. London: Office for National Statistics:13–21.
Damé-Teixeira N, Alves LS, Susin C, et al. (2013) Traumatic dental injury among 12-year-old South Brazilian schoolchildren: prevalence, severity, and risk indicators. Dent Traumatol. 29(1):52-8. doi: 10.1111/j.1600-9657.2012.01124.x.
De Souza RF, Travess H, Newton T, et al. (2015) Interventions for treating traumatized ankylosed permanent front teeth. Cochrane Database Syst Rev. 2015(12):CD007820. doi: 10.1002/14651858.CD007820.pub3. doi: 10.1016/j.jsps.2017.09.005. Epub 2017 Sep 14. PMID: 29204070; PMCID: PMC5688227.
Drysdale C, Gibbs SL and Ford TR (1996) Orthodontic management of root-filled teeth. Br J Orthod 23(3): 255–60.
Duggal MS, Kindelan J, and Nazzal H (2015) Upper incisor trauma and the orthodontic patient—principles of management. Semin Ortho. 21(1):59–70. https://doi.org/https://doi.org/10.1053/j.sodo.2014.12.006
Enabulele J, Oginni A, Sede M, et al. (2016) Pattern of traumatized anterior teeth among adult Nigerians and complications from late presentation. BMC Res Notes 9(1):70. doi:10.1186/s13104-016-1871-3
Esteves T, Ramos AL, Pereira CM, et al. (2007) Orthodontic root resorption of endodontically treated teeth. J Endod 33(2): 119–22.
Fakhruddin KS, Lawrence HP, Kenny DJ, et al. (2008) Impact of treated and untreated dental injuries on the quality of life of Ontario school children. Dent Traumatol. 24(3):309-13. doi: 10.1111/j.1600-9657.2007.00547.x. Epub 2008 Apr 9. PMID: 18410390.
Hermann NV, Lauridsen E, Ahrensburg SS, et al. (2012) Periodontal healing complications following concussion and subluxation injuries in the permanent dentition: a longitudinal cohort study. Dent Traumatol. 28(5):386-93.
Jaradat M, and Rahhal A (2016) Orthodontic considerations for traumatized permanent teeth. Brit J Med Res. 15:1-8.
Joybell CC, Kumar MK, and Ramraj B (2019) Knowledge, awareness, and attitude among the employees in emergency ambulance services towards traumatic dental injuries. J Family Med Prim Care. 8(3):1043-1048. doi: 10.4103/jfmpc.jfmpc_343_18. PMID: 31041248; PMCID: PMC6482711.
Kindelan SA, Day PF, Kindelan JD, et al. (2008) Dental trauma: an overview of its influence on the management of orthodontic treatment. Part 1. J Orthodon. 35(2):68-78.
Malmgren O, and Malmgren B (2007) Orthodontic management of the traumatized teeth. In: Andreasen JO, Andreasen FM, Andersson L, editors. Textbook and color atlas of traumatic injuries to the teeth. 4th ed. Oxford: Blackwell Munksgaard; p. 699-715.
Owtad P, Shastry S, Papademetriou M, et al. (2015) Management Guidelines for Traumatically Injured Teeth during Orthodontic Treatment. J Clin Pediatr Dent. 39(3):292-6. doi: 10.17796/1053-4628-39.3.292. PMID: 26208077.
Petti S (2015) Over two hundred million injuries to anterior teeth attributable to large overjet: a meta‐analysis. Dent Traumatol. 31:1–8.
Poi WR, Cardoso Lde C, de Castro JC, et al. (2007) Multidisciplinary treatment approach for crown fracture and crown-root fracture – a case report. Dent Traumatol. 23(1):51-5. doi: 10.1111/j.1600-9657.2005.00373.x. PMID: 17227382.
Sandler C, Barry S, Littlewood S, et al. (2019) Orthodontic management of traumatized teeth: A national survey of UK orthodontists. Dent Traumatol. 35(4-5):241-250. doi: 10.1111/edt.12476.
Tewari N, Mathur VP, Siddiqui I, et al. (2020) Prevalence of traumatic dental injuries in India: A systematic review and meta-analysis. Indian J Dent Res. 31(4):601-614. doi: 10.4103/ijdr.IJDR_953_19.
Van Gorp G, Bormans N, Vanham I, et al. (2020) Orthodontic treatment recommendation and expected adverse reactions in patients with a history of dental trauma: A survey among general dentists, paediatric dentists, and orthodontic specialists. Int J Paediatr Dent. 30(3):360-369. doi: 10.1111/ipd.12603.
Zachrisson BU, and Jacobsen I (1974) Response to orthodontic movement of anterior teeth with root fractures. Trans Eur Orthod Soc :207-14. PMID: 4534972.


