1Research Unit College of Applied Medical Sciences, King Saud bin Abdulaziz University for Heath Science, Riyadh, Saudi Arabia
2King Abdullah International Medical Research Center, Riyadh, Saudi Arabia
3 Respiratory Therapy Department College of Applied Medical Sciences,
King Saud bin Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia
4College of Public Health and Health Informatics, King Saud Bin Abdulaziz University for Heath Science, Riyadh, Saudi Arabia
Corresponding author email: Othmanf@ksau-hs.edu.sa
Article Publishing History
Received: 19/03/2021
Accepted After Revision: 10/06/2021
Coronavirus Disease 2019 (COVID-19) is an emerging infectious pandemic, which has led to a worldwide public health emergency. The clinical spectrum of COVID-19 is varied, and has been explored in many studies. there is still a need to quantify the extent of the risk of developing the severe clinical manifestations of COVID-19 that require admission to intensive care unit (ICU) and mechanical ventilation initiation .The present study aims to assess ICU admission among COVID-19 confirmed cases and those who required invasive mechanical ventilation. MEDLINE, Web of Science, and SCOPUS electronic databases were searched for epidemiological studies on confirmed cases of COVID-19 at the end of April 2020. Eligible articles that reported on admission to ICUs and mechanical ventilation were included. A random-effects model was used to pool results.
A total of 23 articles reported on a total of 6124 confirmed COVID-19 cases. The majority of included articles were from China. The proportion of all hospitalized patients with confirmed COVID-19 who required ICU admission was between 0.01% to 53%, with the pooled proportion of 18% (95%CI 22,73%, I2 = 97.2%, p<0.001). The pooled proportion of ICU patients who had required invasive mechanical ventilation ranged from 4% to 94%, with the pooled estimate at 34% (95%CI 24 to 44%, I2 = 99%, p<0.001)Around a fifth of patients with confirmed COVID-19 diagnoses required admission to the ICU, and at least a third of those cases needed invasive mechanical ventilation. Still, there is a need for additional research with careful study design to identify the predictors and pathogenesis of severe cases.
COVID-19, Intensive Care, Invasive Ventilation, Meta-Analysis.
Othman F, Ismaeil T, El-Metwally A. On the Severity of COVID-19 in Intensive Care and the Role of Invasive Ventilation: A Proportion Meta-Analysis. Biosc.Biotech.Res.Comm. 2021;14(2).
Othman F, Ismaeil T, El-Metwally A. On the Severity of COVID-19 in Intensive Care and the Role of Invasive Ventilation: A Proportion Meta-Analysis. Biosc.Biotech.Res.Comm. 2021;14(2). Available from: <a href=”https://bit.ly/3u8uumq“>https://bit.ly/3u8uumq</a>
Copyright © Othman et al., This is an open access article distributed under the terms of the Creative Commons Attribution License (CC-BY) https://creativecommns.org/licenses/by/4.0/, which permits unrestricted use distribution and reproduction in any medium, provide the original author and source are credited.
INTRODUCTION
Coronavirus Disease 2019 (COVID-19) is a novel coronavirus outbreak which first appeared in December 2019 in China, and has now become an international public health emergency, (The Lancet, 2020; Zhu et al., 2020). The causative pathogen for this pandemic is a positive-strand RNA virus named as the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2). Although the original source of SARS-CoV-2 transmission has not yet been identified, by the end of April 2020, there were over 2 million confirmed cases of COVID worldwide (WHO, 2020). In most cases, this pathogen results in a syndrome that leads to a respiratory condition that requires specialized management at intensive care units (ICU) and the usage of mechanical ventilation( Yang et al., 2020; Rodriguez-Morales et al., 2020; Sun et al., 2020).
The clinical spectrum of COVID-19 is varied, and has been explored in many studies (Yang et al., 2020; Rodriguez-Morales et al., 2020). However, it is important to accurately quantify the precise severity of COVID-19 in order to properly understand the clinical burden of this emerging illness. Mortality is one risk that can be used to measure the extent of the COVID-19’s severity. In addition, admission to the ICU and the need for mechanical ventilation could also be used to estimate the likelihood of developing severe COVID-19 complications.
Current research has indicated that older adults, mainly those who had underlying health conditions, were at a higher risk for severe COVID-19 illness(Lian et al., 2020; Wei-jie et al., 2020). In the USA, a study reported that 53% of confirmed cases required ICU admission(Bialek et al., 2020). Recently published reports from meta-analyses and systematic reviews have described the symptoms and comorbidity predictors for severe COVID-19 associated illnesses and complications(J. Yang et al., 2020; Rodriguez-Morales et al., 2020).
However, there is still a need to quantify the extent of the risk of developing the severe clinical manifestations of COVID-19 that require admission to ICU and mechanical ventilation initiation, as this was not explored in those previous reviews. This will help in understanding the epidemiological determinants of those risks, which would allow us to correctly assess the clinical burden of COVID-19. Therefore, this study aims to estimate the proportion of ICU admission among confirmed COVID-19 cases.
METHODS
The present study is a meta-analysis that has been conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (Moher et al., 2009). The protocol of this study has been approved by King Abdullah International Research Center Riyadh KSA, (protocol number RC20/164/R). The main objective of this study is to assess the proportion of ICU admission among confirmed COVID-19 cases and those who required invasive mechanical ventilation.
Search strategy and eligibility criteria: Published studies that referred to the clinical description and prognosis of COVID-19 cases were retrieved from MEDLINE (PubMed), Web of Science, and SCOPUS electronic databases until 31 April 2020. The following search terms were used in defining relevant articles: “SARS-CoV-2″, “Wuhan pneumonia”, “Wuhan coronavirus”, “2019 nCoV”, “severe Acute Respiratory Syndrome Coronavirus 2”, “coronavirus 2019”, “novel coronavirus”, and “COVID-19”, in combination with “hospitalization”, “intensive care” and “ICU”.
Moreover, we searched for additional articles using the reference list and grey literature. Eligible study designs were case series, case-control studies, cohort studies, and case reports ( only ones with a sample size of more than 5 were eligible). Review articles, editorial articles, and surveillance reports which did not present original data were excluded. Language restriction was applied. Thus, we only included articles that have been published in English.
Study selection and data extraction: The articles that resulted from the initial search strategy were first screened based on the information obtained from the title and abstract, and afterwards, were independently reviewed by two authors (FO and TI). The full texts of the potentially relevant articles were assessed for inclusion according to the following outcome: studies that focused on patients with confirmed cases of COVID-19, and documented primary data on the proportion of patients admitted to the ICU and patients undergoing mechanical ventilation. Secondary data on mortality were also collected from those studies. Studies reporting cases with incomplete information were excluded. When more than one article reported on information from the same hospital within the same period of time, the data was obtained from the article with the more recent publication date.
Data extraction forms were filled for each study, including information on the type of publication, the period of collection data, country and area, month of publication, the number of confirmed cases, number of cases at ICU, number of cases who required invasive ventilation, proportion of patients who die, and demographic information. The primary data were the proportion of patients admitted to the ICU and patients who required invasive ventilation.
Assessment of risk of bias in included studies:The risk of bias was assessed using a scoring system for the evaluation. We used the quality assessment tool published by the National Institutes of Health (NIH) to determine the methodological quality of the included studies(National Institutes of Health ,Study Quality Assessment Tools, no date).
The assessment tool has 9 items, of which we used either 0 points or 1 point to score each item, and then calculated the sum of the scores for all items to generate an overall quality score that ranged between 0 and 9. The criteria and each article were reviewed by two independent reviewers, the results were compared, and any conflicts were resolved by the third reviewer.
Statistical approach: The meta-analysis was performed using Stata 15 software system (StataCorp LP, College Station, TX). For study outcomes, we dealt with them as dichotomous variables. The pooled prevalence and their 95% confidence interval (CI) were used to summarize the weighted effect size for each study using the binary random effect model. We adapted the metan command, which is specific to binomial data(Nyaga, Arbyn and Aerts, 2014).
This allowed the computation of proportions using the exact binomial method, as well as allowing the within-study variability to be modelled using the binomial distribution. The heterogeneity among identified studies was statistically assessed using the I2 statistic. A forest plot was used to illustrate the distribution of the outcome and the effect size obtained from each published study. We performed subgroup analysis of the type of population included in the studies (hospitalized or ICU patients).
RESULTS AND DISCUSSION
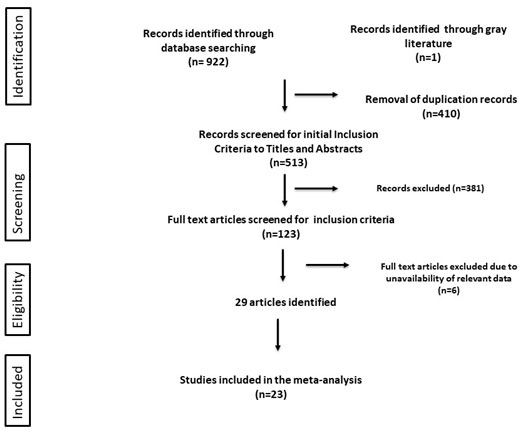
Description of included articles: The flow chart of the search process and study selection is shown in figure 1. The initial search in the electronic databases produced 922 results. After removing duplication, a total of 513 potential articles were screened for eligibility from title and abstract. This yielded 123 full-text articles that had been assessed for eligibility by applying the eligibility criteria. A total of 23 articles were selected as eligible articles, and were all subject to meta-analysis (Arentz et al., 2020; Barrasa et al., 2020; Lian et al., 2020; Mo et al., 2020; N. Chen et al., 2020; R. Wang et al., 2020; Simonnet et al., 2020; T. L. Chen et al., 2020; Wei-jie et al., 2020; X. Yang et al., 2020; Xu et al., 2020; Y. Wang et al., 2020; Bhatraju et al., 2020; Young et al., 2020; Zhang et al., 2020; Zhou et al., 2020; Cao et al., 2020; D. Wang et al., 2020; Du et al., 2020; Grasselli et al., 2020; Huang et al., 2020; J. Chen et al., 2020; Lei et al., 2020). The majority of excluded articles did not include the proportion of patients who had been admitted to the ICU. Two articles were published from the same institution during the same period; therefore, we only included the more recently published one.
Figure 1: Flowchart of the included studies
RESULTS AND DISCUSSION
Description of included articles: The flow chart of the search process and study selection is shown in figure 1. The initial search in the electronic databases produced 922 results. After removing duplication, a total of 513 potential articles were screened for eligibility from title and abstract. This yielded 123 full-text articles that had been assessed for eligibility by applying the eligibility criteria. A total of 23 articles were selected as eligible articles, and were all subject to meta-analysis (Arentz et al., 2020; Barrasa et al., 2020; Lian et al., 2020; Mo et al., 2020; N. Chen et al., 2020; R. Wang et al., 2020; Simonnet et al., 2020; T. L. Chen et al., 2020; Wei-jie et al., 2020; X. Yang et al., 2020; Xu et al., 2020; Y. Wang et al., 2020; Bhatraju et al., 2020; Young et al., 2020; Zhang et al., 2020; Zhou et al., 2020; Cao et al., 2020; D. Wang et al., 2020; Du et al., 2020; Grasselli et al., 2020; Huang et al., 2020; J. Chen et al., 2020; Lei et al., 2020). The majority of excluded articles did not include the proportion of patients who had been admitted to the ICU. Two articles were published from the same institution during the same period; therefore, we only included the more recently published one.
Table 1. Data extracted from each included study.
| Study Author | Country | Study Frame | Population(n) | ICU cases(%) | patients used NIV (%) | Mortality(%) | quality score | mean age(SD) | gender( female (%)) |
| Guan et al(Wei-jie et al., 2020) | China | 11 Dec to 31 Jan | 1590 | 99(6.2) | 50(3.1) | 50(3.1) | 9 | 48.9(16) | 674(42) |
| Huang et al(Huang et al., 2020) | China | 16 Dec to 2 Jan | 41 | 16(39%) | 4(10%) | 6(15%) | 9 | 49(12) | 11 (27) |
| Yang et al(X. Yang et al., 2020) | China | 24 Dec to 26 Jan | 52 | 52(100%) | 33 (63.5%) | 32 (62%) | 7 | 59.7(13) | 17 (33) |
| Du et al(Du et al., 2020) | China | 25 Dec to 15 Feb | 109 | 51 (46.8%) | 33(30) | 100 | 7 | 70.7(10) | 35 (32) |
| Zhou et al(Zhou et al., 2020) | China | 29 Dec to 31 Jan | 191 | 50(26%) | _ | 54 | 8 | 56(15) | 72 (38) |
| Chen N et al(N. Chen et al., 2020) | China | 1 Jan to 20 Jan | 99 | 23(23%) | 4 | 11(11%) | 8 | 55.5(13) | 32(32) |
| Chen TL et al(T. L. Chen et al., 2020) | China | 1 Jan to 1 Feb | 203 | 107(52) | 39(19.2) | 26(12.8) | 8 | 54.7 (20) | 46(22) |
| Wang D et al (D. Wang et al., 2020) | China | 1 Jan to 3 Feb | 138 | 36(26) | 17 (12.32) | 6 (4.3) | 8 | 56.5(20) | 63 (45. |
| Lei et al(Lei et al., 2020) | China | 1 Jan to 12 Feb | 20 | 1 (5.0%) | 2(10) | 0 | 7 | 43.2(14) | 10 (50. |
| Mo et al(Mo et al., 2020) | China | 1 Jan to 5 Feb | 155 | 55(35) | 36(23) | 22(14) | 7 | 54(34) | 69(44) |
| Cao et al(Cao et al., 2020) | China | 3 Jan to 15 Feb | 104 | 18(17.6) | 14(13.7) | 17(16.3%) | 8 | 54(22) | 49(48) |
| Xu et al(Xu et al., 2020) | China | 10 Jan to 26 Jan | 62 | 1(1.6) | — | 0 | 9 | 41(14) | 27(44) |
| Zhang et al(Zhang et al., 2020) | China | 13 Jan to 26 Feb | 28 | 6(21.4) | 10(35.7) | 8(28.6) | 7 | 65(28) | 10(39) |
| Lian et al(Lian et al., 2020)(A) | China | 17 Jan to 12 Feb | 652 | 9(1.38) | 5(0.77) | 0 | 8 | 41.11) | 303(46) |
| Lian et al(Lian et al., 2020)(B) | China | 17 Jan to 12 Feb | 136 | 13(9.56) | 6(4.41) | 0 | 8 | 68(7) | 8(5) |
| Chen J et al(J. Chen et al., 2020) | China | 20 Jan to 6 Feb 6 | 249 | 22(8.8) | __ | 2(0.8%) | 8 | 51(20) | 123(49) |
| Wang R et al(R. Wang et al., 2020) | China | 20 jan 9 Feb | 125 | 19(15.2%) | 4(21) | 0 | 8 | 38 (13) | 54(43) |
| Young et al(Young et al., 2020) | Singapore | 23 Jan to 3 Feb | 18 | 2(11%) | 1(6%) | 0 | 8 | 47(31) | 9(50) |
| Wang Y et al(Y. Wang et al., 2020) | China | 25 Jan to 25 Feb | 344 | 344(100) | 100 (29.1) | 133(38.6) | 7 | 64(7) | 165(47) |
| Grasselli et al(Grasselli et al., 2020) | Italy | 20 Feb to18 March | 1591 | 1591(100%) | 1150 (88) | 405 (26) | 8 | 63(10) | 287 (18) |
| Arentz et al(Arentz et al., 2020) | USA | 20 Feb to 5 March | 21 | 21(100) | 15 (71%) | 11 (52.4) | 6 | 70(14) | 10(48) |
| Bhatraju, et al(Bhatraju et al., 2020) | USA | 24 Feb to 9 March | 24 | 24(100%) | 18(75%) | 12(50) | 8 | 64(18) | 9(38) |
| Barrasa et al(Barrasa et al., 2020) | Spain | 4March to 31 March | 48 | 48(100) | 45(94%) | 6(13) | 7 | 63(12) | 21 (43) |
| Simonnet, et al(Simonnet et al., 2020) | France | 27 March to 5 April | 124 | 124(100) | 85 (68.6%) | 18 (15%) | 7 | 60 (14) | 34(27) |
Quality of Included Studies: All of the included studies were case series analyses and were critically appraised using the quality assessment tool published by NIH. Each article was assigned an overall quality score based on each item in the assessment tool. Although the majority of articles have an overall quality score between 6 to 9, there was some inconsistency between the studies in defining the critical cases that required ICU admission. The studies from China used the WHO-China Joint Mission on COVID-19(Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19), 2020)) to define the more severe cases that required ICU admission while other studies used different criteria. In this meta-analysis, we identified ICU cases as those cases that required ICU admission or used invasive mechanical ventilation.
Figure 2: Forest-plot of the prevalence of ICU admission of confirmed cases
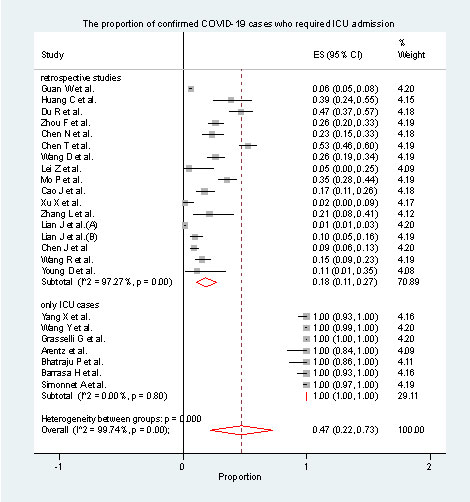
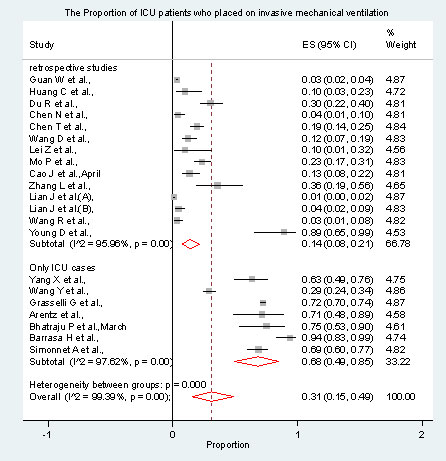
Pooled analysis of patients who were admitted to ICU: Figure 2 demonstrates the pooled ICU admission prevalence. The proportion of all hospitalized patients with confirmed COVID-19 who required ICU admission was between 0.01% to 53%, with the pooled proportion of 18% (95%CI 22,73%, I2 = 97.2%, p<0.001). The pooled proportion of ICU patients who were placed on invasive mechanical ventilation ranged between 4% and 94%, with the pooled estimate at 34% (95%CI 24 to 44%, I2 = 99%, p<0.001) (figure3).
Figure 3: Forest-plot of the prevalence of using mechanical ventilation among ICU admission cases
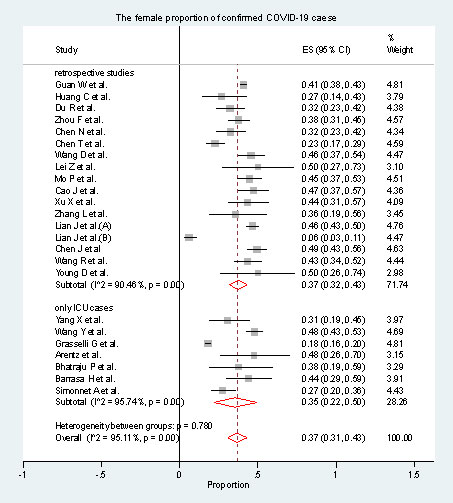
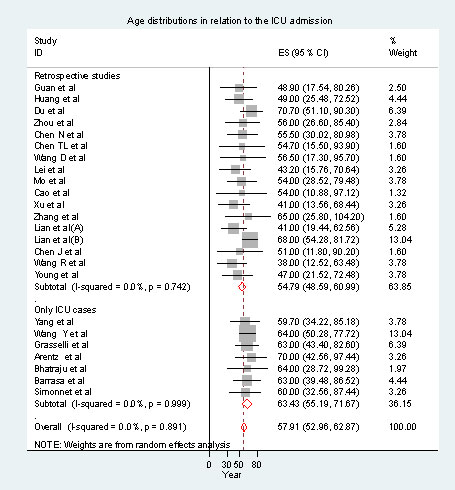
The mortality of all hospitalized patients with confirmed COVID-19 cases is demonstrated in figure 4. Among the cases who required ICU admission, the mortality rate was 34% (95%CI 23-45). In comparison, the overall mortality rate for all hospitalized patients was 13% (95% CI 7-20%). Age and gender distributions in relation to the ICU admission of those studies which only include ICU populations are shown in figure 5. The overall mean age of the patients with confirmed COVID-19 was 57 years (95%CI 52.9-62.8), and 37% (95% CI 31-43%) were female patients.
Figure 4: Forest-plot of the mortality among COVID-19 patients
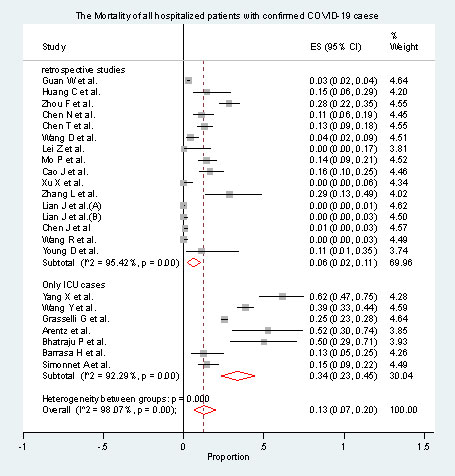
Figure 5: Forest-plot of the propotion of female COVID-19 patients
The COVID-19 pandemic has affected the healthcare sector in all nations around the world. Countries are still facing this epidemic disease and great efforts are still needed to understand its epidemiology, clinical presentation, pathological manifestation, and the appropriate techniques needed for the management of the infected cases. One critical aspect that also needs to be addressed is the severity of the COVID-19 infection associated with the evolution of this emerging epidemic.
This can be examined by estimating the proportion of patients who needed ICU admission and initiation of mechanical ventilation, which is the core of this present meta-analysis. In this study, we tried to initially summarize the clinical data on confirmed COVID-19 cases during the first four months of the outbreak. In this study, we found that 18% of hospitalized subjects with confirmed COVID-19 required ICU admission. The results also indicated that COVID-19 cases that required the use of invasive mechanical ventilation were 14% of all hospitalized subjects with confirmed COVID-19 and 67% of all ICU admissions. The overall mortality among COVID-19 confirmed cases was low (6% and 13% hospital and ICU mortality, respectively).
Figure 6: Forest-plot of the age distrubution of COVID-19 patients
For patients admitted to the ICU, our findings were comparable to previous studies. These previous studies identified that between 18% and 20% of their study population required ICU admission (Rodriguez-Morales et al., 2020; Sun et al., 2020). This is explained by the similarity in the included studies in these meta-analyses. However, the proportion of patient who were admitted to the ICU and required invasive mechanical ventilation have not been examined in previous studies.
Thus, in this study, we examined the number of cases which required mechanical ventilation. The proportion of those patients appeared to vary between the studies. From a critical care perspective, an estimation of the number of patients who required mechanical ventilation is crucial. This can help healthcare authorities in predicting the number of expected severe cases that will require invasive ventilation in terms of allocating the resources. However, there is still a need for more studies that include a cohort follow up of those ICU admitted patients in order to determine the clinical outcome in terms of invasive ventilation requirement.
Strength and limitations: This meta-analysis has some limitations. First, the individual identification information of the patients who had been involved in the published studies was absent. Thus, we could have overestimated the total number of cases in our pooled analysis by referring to the same patients more than once. This risk is especially heightened for most of the earliest studies published from Wuhan hospitals, which collected information during the same period. Although we excluded one study that potentially had the same study population as another, we could not identify this potential bias in other studies.
Second, the majority of the included studies in this meta-analysis were from China, whereas many regions around the world are affected by COVID-19 and have not yet published their clinical data. Although we included data from Spain, Italy, and USA in this analysis, more studies from other countries are still needed in order to expand the growing volume of available data. In addition, the epidemiological understanding of the severity of COVID-19 would be improved through the inclusion of more detailed patient information regarding the ICU course and the mode of invasive mechanical ventilation. It is advisable to set joint case registration across geographical regions as well as allocated identification numbers for each case to allow the epidemiological researcher to better identify risk factors of ICU admission and associated outcomes. On the other hand, this meta-analysis provides useful information regarding the risk of ICU admission and the usage of invasive ventilation in severe COVID-19 case.
CONCLUSION
Around a fifth of patients who are infected with COVID-19 require admission to ICU, and at least a third of those cases need invasive mechanical ventilation. Still, there is a need for additional research with careful study design to identify the predictors and pathogenesis of severe cases.
Author contributions: FO proposed the original idea for the study, planned the study design, provided research materials, performed the statistical analyses, and writing the first draft of the paper. TI helped in planning the study design, extract the data, revising the drafts of the paper. AM contributed to study design and concept, analysis planning, and interpretation of results, as well as to revising the drafts of the paper. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
REFERENCES
Arentz, M. et al. (2020) ‘Characteristics and Outcomes of 21 Critically Ill Patients with COVID-19 in Washington State’, JAMA – Journal of the American Medical Association, 323(16), pp. 1612–1614. doi: 10.1001/jama.2020.4326.
Barrasa, H. et al. (2020) ‘SARS-Cov-2 in Spanish Intensive Care: Early Experience with 15-day Survival In Vitoria’, Anaesthesia Critical Care & Pain Medicine, pp. 1–9. doi: 10.1016/j.accpm.2020.04.001.
Bhatraju, P. K. et al. (2020) ‘Covid-19 in Critically Ill Patients in the Seattle Region — Case Series’, New England Journal of Medicine, pp. 1–11. doi: 10.1056/nejmoa2004500.
Bialek, S. et al. (2020) ‘Severe Outcomes Among Patients with Coronavirus Disease 2019 (COVID-19) — United States, February 12–March 16, 2020’, MMWR. Morbidity and Mortality Weekly Report, 69(12), pp. 343–346. doi: 10.15585/mmwr.mm6912e2.
Cao, J. et al. (2020) ‘Clinical Features and Short-term Outcomes of 102 Patients with Corona Virus Disease 2019 in Wuhan, China’, Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. doi: 10.1093/cid/ciaa243.
Chen, J. et al. (2020) ‘Clinical progression of patients with COVID-19 in Shanghai, China’, Journal of Infection. Elsevier BV. doi: 10.1016/j.jinf.2020.03.004.
Chen, N. et al. (2020) ‘Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study’, The Lancet. Elsevier Ltd, 395(10223), pp. 507–513. doi: 10.1016/S0140-6736(20)30211-7.
Chen, T. L. et al. (2020) ‘Clinical characteristics and outcomes of older patients with coronavirus disease 2019 (COVID-19) in Wuhan, China (2019): a single-centered, retrospective study’, The journals of gerontology. Series A,glaa089. doi: 10.1093/gerona/glaa089.
Du, R. H. et al. (2020) ‘Hospitalization and Critical Care of 109 Decedents with COVID-19 Pneumonia in Wuhan, China’, Annals of the American Thoracic Society, 0, pp. 1–30. doi: 10.1513/AnnalsATS.202003-225OC.
Grasselli, G. et al. (2020) ‘Baseline Characteristics and Outcomes of 1591 Patients Infected with SARS-CoV-2 Admitted to ICUs of the Lombardy Region, Italy’, JAMA – Journal of the American Medical Association. doi: 10.1001/jama.2020.5394.
Huang, C. et al. (2020) ‘Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China’, The Lancet. Lancet Publishing Group, 395(10223), pp. 497–506. doi: 10.1016/S0140-6736(20)30183-5.
Lei, Z. et al. (2020) ‘Comparison of Epidemiological and Clinical Features of Patients with Coronavirus Disease (COVID-19) in Wuhan and Outside Wuhan, China’, SSRN Electronic Journal. doi: 10.2139/ssrn.3546082.
Lian, J. et al. (2020) ‘Analysis of Epidemiological and Clinical features in older patients with Corona Virus Disease 2019 (COVID-19) out of Wuhan’, Clinical infectious diseases : an official publication of the Infectious Diseases Society of America, 2019, pp. 1–8. doi: 10.1093/cid/ciaa242.
Mo, P. et al. (2020) ‘Clinical characteristics of refractory COVID-19 pneumonia in Wuhan, China’, Clinical infectious diseases : ciaa270. doi: 10.1093/cid/ciaa270.
Moher, D. et al. (2009) ‘Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement’, PLoS Medicine. doi: 10.1371/journal.pmed.1000097.
National Institutes of Health ,Study Quality Assessment Tools (no date).
Nyaga, V. N., Arbyn, M. and Aerts, M. (2014) ‘Metaprop: A Stata command to perform meta-analysis of binomial data’, Archives of Public Health. doi: 10.1186/2049-3258-72-39.
Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19) (2020).
Rodriguez-Morales, A. J. et al. (2020) ‘Clinical, laboratory and imaging features of COVID-19: A systematic review and meta-analysis’, Travel Medicine and Infectious Disease. Elsevier USA, 34(101623). doi: 10.1016/j.tmaid.2020.101623.
Simonnet, A. et al. (2020) ‘High prevalence of obesity in severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation’, Obesity, 10.1002/ob. doi: 10.1002/oby.22831.
Sun, P. et al. (2020) Clinical characteristics of 50 466 hospitalized patients with 2019-nCoV infection, Journal of Medical Virology. doi: 10.1002/jmv.25735.
The Lancet (2020) ‘Emerging understandings of 2019-nCoV’, The Lancet. Lancet Publishing Group, 395(10221), p. 311. doi: 10.1016/S0140-6736(20)30186-0.
Wang, D. et al. (2020) ‘Clinical Characteristics of 138 Hospitalized Patients with 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China’, JAMA – Journal of the American Medical Association, 323(11), pp. 1061–1069. doi: 10.1001/jama.2020.1585.
Wang, R. et al. (2020) ‘Epidemiological and clinical features of 125 Hospitalized Patients with COVID-19 in Fuyang, Anhui, China’, International Journal of Infectious Diseases. International Society for Infectious Diseases. doi: 10.1016/j.ijid.2020.03.070.
Wang, Y. et al. (2020) ‘Clinical Course and Outcomes of 344 Intensive Care Patients with COVID-19’, American journal of respiratory and critical care medicine, pp. 1–16. doi: 10.1164/rccm.202003-0736LE.
Wei-jie, G. et al. (2020) ‘Comorbidity and its impact on 1590 patients with Covid-19 in China: A Nationwide Analysis’, The European respiratory journal, 0903–1936. doi: 10.1183/13993003.00547-2020 LK – http://ucelinks.cdlib.org:8888/sfx_local?sid=EMBASE&sid=EMBASE&issn=13993003&id=doi:10.1183%2F13993003.00547-2020&atitle=Comorbidity+and+its+impact+on+1590+patients+with+Covid-19+in+China%3A+A+Nationwide+Analysis&stitle=Eur.+Respir.+J.&title=The+European+respiratory+journal&volume=&issue=&spage=&epage=&aulast=Guan&aufirst=Wei-Jie&auinit=W.-J.&aufull=Guan+W.-J.&coden=&isbn=&pages=-&date=2020&auinit1=W&auinitm=-J.
WHO (2020) Coronavirus disease 2019.
Xu, X. W. et al. (2020) ‘Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-Cov-2) outside of Wuhan, China: Retrospective case series’, The BMJ, 368(January), pp. 1–7. doi: 10.1136/bmj.m606.
Yang, J. et al. (2020) ‘Prevalence of comorbidities and its effects in coronavirus disease 2019 patients: A systematic review and meta-analysis’, International Journal of Infectious Diseases. Elsevier BV, 94, pp. 91–95. doi: 10.1016/j.ijid.2020.03.017.
Yang, X. et al. (2020) ‘Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study’, The Lancet Respiratory Medicine, (20), pp. 30079–5. doi: 10.1016/S2213-2600(20)30079-5.
Young, B. E. et al. (2020) ‘Epidemiologic Features and Clinical Course of Patients Infected with SARS-CoV-2 in Singapore’, JAMA – Journal of the American Medical Association, 323(15), pp. 1488–1494. doi: 10.1001/jama.2020.3204.
Zhang, L. et al. (2020) ‘Clinical characteristics of COVID-19-infected cancer patients: a retrospective case study in three hospitals within Wuhan, China’, Annals of Oncology, S0923-7534(20), pp. 36383–3. doi: 10.1016/j.annonc.2020.03.296.
Zhou, F. et al. (2020) ‘Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study’, The Lancet, (20), pp. 30566–3. doi: 10.1016/S0140-6736(20)30566-3.
Zhu, N. et al. (2020) ‘A novel coronavirus from patients with pneumonia in China, 2019’, New England Journal of Medicine. Massachussetts Medical Society, 382(8), pp. 727–733. doi: 10.1056/NEJMoa2001017.


