1Division of Orthodontics, Department of Pediatric Dentistry and Orthodontics, College of Dentistry, King Saud University, Riyadh, Saudi Arabia and
2General Dentist, Private Clinic, Riyadh, Saudi Arabia
Corresponding author email: Banan.Almashali@gmail.com
Article Publishing History
Received: 01/12/2020
Accepted After Revision: 22/03/2021
In orthodontic bonding, it is crucial to obtain optimal marginal integrity between tooth surface and bonding adhesive. Undermining the intimate contact create gaps at the enamel-adhesive interface, these gaps may affect the bond strength and predispose the enamel to white spot lesions. This study evaluated the effect of leaving excess adhesive resin around orthodontic brackets on marginal integrity in vitro. In this in vitro experimental trial, 24 intact premolars were bonded with a stainless-steel orthodontic bracket using Transbond XT light cure adhesive composites mixed with Rhodamine B fluorescent dye. After positioning the bracket and before light curing, excess adhesive was removed according to the test groups. Group 1: the entire adhesive around the bracket was removed. Group 2, only 1-mm excess around the bracket was left. Group 3, only 2-mm excess around the bracket was left. The angle between enamel surface and bonding adhesive was measured using confocal laser scanning microscopy and data were analyzed by one way analysis of variance and post hoc Tukey test. The presence of excess adhesive significantly increased the angle (p<0.05), group 1 (0mm excess) presented a more favorable marginal integrity (4.5°± 1.5°) compared to groups 2 (14.65°±2.5°) and 3 (19.44°±4°). Excess adhesive around orthodontic brackets did not improve the marginal integrity.
Confocal Laser Scanning Microscopy, Excess Adhesive, Marginal Integrity, Orthodontic Brackets.
Almashali B, Almahdy A, Alqahtani N, Alghamdi H. Marginal Integrity of Peri-bracket Excess adhesive. A Confocal Laser Scanning Microscopic study. Biosc.Biotech.Res.Comm. 2021;14(1).
Almashali B, Almahdy A, Alqahtani N, Alghamdi H. Marginal Integrity of Peri-bracket Excess adhesive. A Confocal Laser Scanning Microscopic study. Biosc.Biotech.Res.Comm. 2021;14(1). Available from: <a href=”https://bit.ly/2MO654x”>https://bit.ly/2MO654x</a>
Copyright © Almashal et al., This is an open access article distributed under the terms of the Creative Commons Attribution License (CC-BY) https://creativecommns.org/licenses/by/4.0/, which permits unrestricted use distribution and reproduction in any medium, provide the original author and source are credited.
INTRODUCTION
In orthodontic bonding, it is crucial to obtain optimal marginal integrity between tooth surface and bonding adhesive for both, bond strength (decreasing bond failure) and tight seal (minimizing passage of bacteria and oral fluid i.e. microleakage), thus, reducing white spot lesions (WSL) around orthodontic brackets. Efforts targeting these two problems have been developed, such as the introduction of new adhesive materials, the use of amorphous calcium phosphate and fluoride, minimizing the number of spots in the interface between the bracket base and the prepared enamel where adhesive might fail to continuously penetrate that space, creating tiny fracture-prone voids, through modifications to enamel etching procedures, or the use of sealants around orthodontic brackets,(Cucu et al., 2002; Daub et al., 2006; Yagci et al., 2010; Canbek et al., 2013; Bilal and Arjumand, 2019; Sonesson et al., 2020 Babanouri et al 2020).
Despite these efforts, questionable marginal integrity, bond failure, and white spot lesions still occur, and each of the aforementioned methods has its own associated disadvantages. This include adding an extra step to bonding procedure, thus increases the complexity of an already technique-sensitive procedure. Additional costs are also added – both in terms of time and resources-, plus, the technical requirements for proper implementation of these procedures may raise issues with compatibility. As well, requiring patient cooperation, which often clearly inadequate (Karandish, 2016; Lee et al., 2020; Sonesson et al., 2020).
Thereby, unless a fundamental change in orthodontic bonding technology occurs, the presence of these deficiencies with the currently used bonding procedure may force us to accept a suboptimal bond between enamel and orthodontic brackets. This suggests that developing a material or a method that takes the patient’s compliance out of the equation and requires no extra chair time or additional cost in the clinic would be promising in the field of preventive care during orthodontic treatment among selected patients. Typical orthodontic sealants work as mechanical barrier to protect the around orthodontic brackets, some have added antimicrobial agents or release fluoride. These sealants are deemed useful for preventing microleakage. However, their efficacy is limited by their antimicrobial activity, color stability, and ability to endure intraoral stresses such as thermal changes and abrasion. An effective sealant material would be one with high abrasion resistance and low thickness facilitating its flow and adaptation (Asefi et al., 2016; Singh et al., 2019; Lee et al., 2020; Linjawi, 2020).
Orthodontic resin bonding materials meets those requirements, but they are not being used for this purpose. The traditional orthodontic bonding procedure using resin composite consists of the application of a bonding agent, often an unfilled resin, to the etched enamel surface followed by a filled resin composite paste applied to the bracket. The clinician positions the bracket on the tooth and press firmly toward the tooth surface. As the bracket is positioned on the tooth surface, excess adhesive typically flows around the bracket base as pressure is applied on the bracket and this standard orthodontic bonding procedure involves a final step of removing the peri-bracket excess adhesives before light curing (Proffit et al., 2013). This excess adhesive is removed for two reasons; 1) preventive reasons, as plaque tends to accumulate on rough surface and 2) aesthetic reasons, excess adhesive may get stained over time. On the other hand, it was suggested that removing the excess adhesive following conventional acid etching and bonding might predispose the enamel to white spot lesions (WSL) due to the washout phenomena of bonding material with time (Farrow et al., 2007; Hilgert et al., 2008; Decha et al., 2019).
For this reason, leaving certain amount of resin around brackets could – theoretically- seal the gap between them and the enamel thus reducing the problems associated with these gaps (Palot et al., 1991; Joseph et al., 1994; Alencar et al., 2016). Therefore, the aim of this in vitro study is to assess the marginal integrity at the enamel adhesive interface by measuring the contact angle between the composite adhesive and enamel surface with and without leaving excess adhesive using confocal laser scanning microscopy (CFLSM).
MATERIAL AND METHODS
The study was approved by the Institutional Review Board (IRB) at the College of Dentistry, King Saud University [E-17-2369]. Twenty-four human premolars were extracted for orthodontic reasons and informed consent was obtained for their use in this study. The extracted teeth were visually examined to be devoid of caries, restorations, fluorosis or abrasion. The extracted teeth were stored in distilled water until use (maximum 6 months) as per the ISO document 11405 (ISO/TS 11405:2015(en), Dentistry — Testing of adhesion to tooth structure, 2015). The teeth were randomly assigned to three equal groups of 8 in each. Immediately before conditioning the enamel, the buccal surfaces were cleaned with a rubber cup and pumice slurry to remove plaque and extrinsic stains. The brackets were bonded on the buccal surfaces according to manufacturer’s instructions.
The area where the bracket is to be bonded was etched in the same manner for all three study groups using 38% phosphoric acid (Pulpdent Corporation, Watertown, USA) for 30 seconds and then rinsed thoroughly with water. The teeth were dried with compressed oil-free air for 5 seconds until a frosted appearance was seen on the enamel surface. Next, A thin layer of unfilled bonding resin (Transbond XT primer; 3M Unitek, Marinova, USA) mixed with fluorescein dye was applied with a microbrush applicator and the surface was lightly blown with air to ensure a uniform layer of primer remains before light curing for 20 seconds. brackets were then bonded using Transbond XT light cure adhesive adhesive (3M Unitek, Marinova, USA) mixed with Rhodamine B dye at concentration of 0.1 mmol/L, Rhodamine B is an inert dye that is used to facilitate visualization of resin under confocal microscope (Kumar et al., 2011). Transbond XT paste was applied to the bracket base and pressed firmly onto the tooth (Farrow et al., 2007).
The teeth in group 1: All excess adhesive around the bracket was removed using an explorer before light curing.
The teeth in group 2: the adhesive around the bracket was removed allowing only 1 mm excess contoured around the bracket.
The teeth in group 3: the adhesive around the bracket was removed allowing only 2 mm excess contoured around the bracket.
The bonding site and amount of the excess resin was controlled using a customized puncher to create a window in a piece of adhesive tape of the corresponding size, which was attached to the specimen prior to bonding procedure. After seating the bracket into position, each bracket was then cured with light-emitting diode curing light (3M Unitek, Monrovia, USA) for a total of 40 seconds, 20 seconds each on mesial and distal aspects to achieve optimal curing of bracket adhesive (Oesterle et al., 1995; Farrow et al., 2007) .
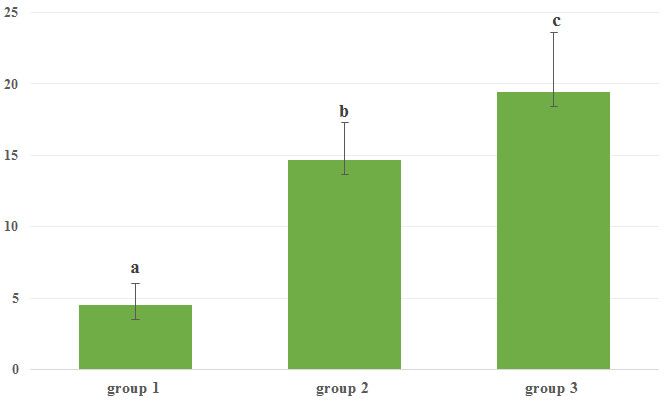
Figure 1: Mean contact angle (in degrees) for the three groups. Vertical bar indicates standard deviation. Dissimilar letters indicate significant difference.
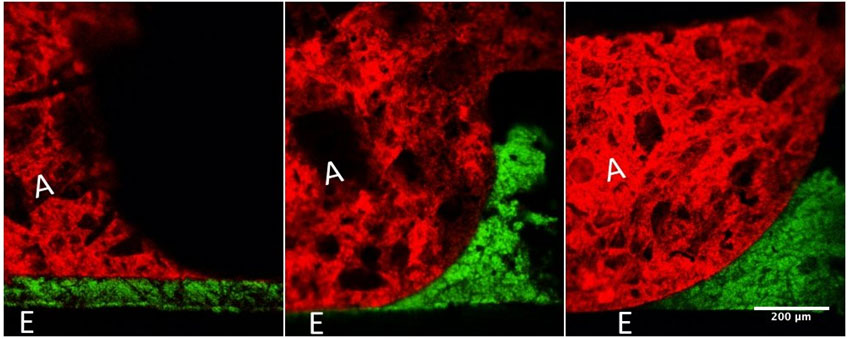
Figure 2: Representative confocal laser scanning microscopy scans (20×/1.4 air objective lens) for each group. The angle between enamel surface and bonding adhesive was measured for each group. The letter (A) indicate the adhesive resin, and the letter (E) indicate the enamel surface.
The teeth were then sectioned labiolingually parallel to the long axis of crown by using a low speed cutting machine (IsoMet, Buehler, Lake Bluff, USA), with a 4-inch circular diamond wheel (MetLab Technologies Limited, UK) under water coolant/lubrication to produce 2 sectioned slabs (Kumar et al., 2011). Prior to examination, each slab was hand polished using 180, 400 and 600 grit Silicone Carbide (SiC) papers and ultrasonicated between each paper grade for 3 minutes. The slabs were examined using a confocal laser scanning microscope (Nikon Instruments Inc., Melville, USA) with a 20×/1.4 air objective lens to assess the enamel–adhesive interface, a double labelling technique was used. For detecting rhodamine B dye fluorescence, the slabs were excited with a 561-nm laser, and the fluorescence signal was detected using 600–630 nm emission filters. Fluorescein was excited at 488 nm and the emission was detected using a 500- to 520-nm filter. The resultant angle between the enamel surface and adhesive around the bracket was calculated using ImageJ software (Wayne Rasband, NIH, USA) and numerical value was scored accordingly.
For the statistical analysis, one-way analysis of variance (ANOVA) was used to analyze the angle formed between enamel surface and composite adhesive in the three groups. The ANOVA test results were significant, therefore, pairwise comparison between the groups was done by post-hoc Tukey test. The significance level (i.e., α value) was 0.05.
RESULTS AND DISCUSSION
There was a significant increase in contact angle value when excess adhesive was left on the tooth. Group 1 had significantly lower contact angle (4.5°± 1.5) compared to groups 2 (14.65°±2.5) and 3 (19.44°±4) P<0.05. there was also significant difference between groups 2 and 3 (Figure 1). Representative CLSM scans for each group are in Figure 2.In orthodontic bonding, microleakage at enamel-adhesive-bracket interfaces decrease the bond strength causing bracket failure, and microleakage between enamel surface and adhesive layers can cause white spot lesions and enamel demineralization (Bilen et al.,2020).
These white spot lesions are usually found around the periphery of orthodontic bracket, under loosened bands and at the areas that are inaccessible by brush or undetectable by the patient. These lesions are considered the most common iatrogenic effect of fixed orthodontic treatment (Bishara and Ostby, 2008; Babanouri et al., 2020; Kamarudin et al., 2020). Poor oral hygiene leading to plaque accumulation is the primary cause of demineralization, however, enamel etching and bonding procedure, in terms of sealant and composite resin selection, also plays a role on the exacerbation of demineralization (Hedayati and Farjood, 2018).
Previous in vitro studies evaluated sealing the enamel margins around orthodontic brackets and reported successful results and reduction in demineralization without affecting the shear bond strength (Behnan et al., 2010; Knösel et al., 2012). However, most of these materials are technique sensitive and they have thin, weak films with low abrasion resistance that may compromise their longevity. From this perspective, our study aimed to investigate the adaption and seal of one of the most commonly used orthodontic bonding adhesive when all excess adhesive is removed as opposed to intentionally leaving 1mm or 2mm excess acting as the sealant material around orthodontic brackets. Resin composites adaptation is determined by its behavior during polymerization, the efficacy of adhesive agent, and the viscosity of resin (Asmussen, 1975, Tay et al., 1995).
Accurate evaluation of marginal seal in vitro is done either by tracer penetration tests, where the penetration of different markers along the interface between the adhesive resin and dental hard tissues of extracted teeth resembles the in vivo bacterial, fluids and other liquids penetration, or by quantitative marginal analysis with a microscope (with or without the use of dyes), where the gaps appearing at the interface resemble the in vivo bacterial, fluids and other liquids penetration (Heintze, 2013). In orthodontic literature, most studies measured these microgaps by dye penetration to reflect microleakage.
Microleakage of resin-based adhesives is evident, a study by Sukontapatipark et al. (2001) evaluated conventionally bonded premolars after extraction and reported the presence of gap approximately 10 µm in width at the enamel-composite interface. these gaps are thought to be a result of polymerization shrinkage commonly reported with resin-based materials and were considered a predisposing factor for bacterial accumulation and subsequent white spot lesion development. For this reason, Buyuk et al. (2013) investigated low-shrinking composites and reported lower microleakage with these composites compared to conventional composites, although they produced insufficient shear bond strength and adhesive remnant scores. Another study did not find significant difference in leakage between the flash-free adhesive and color-change coated adhesive system using ceramic brackets (Kim et al., 2016). Similarly, Arruda et al (2016) tested the bond condition of conventional and flash-free adhesives and reported no statistically significant differences in microleakage between the two, the presence or absence of excess adhesive did not affect the microleakage results.
In our study, the adaptation between the bonding adhesive and enamel surface measured by means of an angle, the exact gap width i.e. microleakage was not measured, therefore only prediction of adhesive clinical behavior can be obtained. The angle we measured is the one formed between adhesive and enamel, an angle closer to 0° reflects better adaptation. Based on our results, group 1 (0mm excess) exhibited a more favorable marginal adaptation, followed by group 2 (1mm excess) and lastly, group 3 (2mm excess). Leaving excess material could provide sealing for the previously etched enamel initially, but according to our results, it may not be sufficient because subsequent failure may occur due to predicted wash out of bonding agent leaving an exposed gap that can provide a passage for bacteria and oral fluids, ending up affecting both the bond strength and enamel integrity.
The currently available orthodontic sealants provide protection against demineralization. Both Pro Seal and Opal Seal, which are fluoride releasing sealants, have been effective against WSL (Premaraj et al., 2017; Bartzela, 2018). Other non-fluoride releasing sealants reported to be of similar effect against WSL, thereby questioning the time and expense of using fluoride releasing materials (Leizer et al., 2010). Unfortunately, all the currently available sealants have sub-optimal longevity and re-application is often required with their use. No clear evidence of the long-term protection function of these materials available, as few information available regarding its integrity and durability which play crucial part in its function to protect against WSL and caries (Şen et al., 2020).
A randomized clinical trial by Şen.et al (2020) investigated the durability and integrity of different orthodontic surface sealants by means of optical coherence tomography. The layer thickness of opal seal and Pro seal significantly reduced after few months of treatment. Loss of integrity, up to 50%, was also reported after only three months.Interestingly, all teeth in group 1 had some excess adhesive, although efforts were taken to remove all excess, some excess remained around the brackets. This was also seen in previous studies (Sukontapatipark et al., 2001; Armstrong et al., 2007). We also noted that the excess adhesive in all groups showed irregular transition from adhesive to enamel surface creating a less smooth surface which may create areas that favor plaque accumulation.
Although excess adhesive was contoured before light curing in our study, the contact between the adhesive and enamel surface was not optimal. These findings could be related to the characteristics of the Transbond XT adhesives used in this study. This adhesive has a relatively large molecular weight and high filler concentration (77% quartz- silica hybrid fillers) which increase the viscosity of the material and although the flow characteristics of Transbond XT is considered acceptable when used for orthodontic bonding in traditional fashion, this might not be the case when excess adhesive is present (Bishara 2004; Vasudevan 2014). In addition, other desirable clinical handling characteristics such as nonstickness might deficient when compared to other composites with thinner viscosities.
CONCLUSION
Our study only gives a general idea of excess adhesive behavior, leaving excess adhesive around orthodontic brackets does not improve the marginal seal of Transbond XT adhesive and provide no benefit of sealing around the periphery of orthodontic brackets. Further researches are necessary to determine the exact effect of excess adhesive on plaque accumulation, white spot lesions formation and bond strength. Enhancement of composite bonding materials and application techniques is needed to overcome problems related to microleakage and gap formation.
ACKNOWLEDGEMENTS
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Authors Contribution: All authors have equal contribution in bringing out this research Work.
Conflict of Interest: None
REFERENCES
Alencar, E.Q. de S. e, Nobrega, M. de L.M., Dametto, F.R., dos Santos, P.B.D., Pinheiro, F.H. de S.L., (2016). Comparison of two methods of visual magnification for removal of adhesive flash during bracket placement using two types of orthodontic bonding agents. Dental Press J Orthod 21, 43–50.
Armstrong, D., Shen, G., Petocz, P., Darendeliler, M.A., (2007). Excess Adhesive Flash Upon Bracket Placement: A Typodont Study Comparing APC PLUS and Transbond XT. The Angle Orthodontist 77, 1101–1108.
Asefi, S., Eskandarion, S., Hamidiaval, S., (2016). Fissure sealant materials: Wear resistance of flowable composite resins. J Dent Res Dent Clin Dent Prospects 10,194–199.
Asmussen, E., (1975). Composite restorative resins: Composition versus wall-to-wall polymerization contraction. Acta Odontologica Scandinavica 33, 337–344.
Babanouri, N., Ghafoori, A.R., Ajami, S., Mahdian, A., (2020). Effect of high concentration nano-hydroxyapatite serum on shear bond strength of metal brackets following three different enamel surface preparation methods: An in vitro study. Int Orthod.
Coordes, S.L., Jost-Brinkmann, PG., Präger, T.M., (2018). A comparison of different sealants preventing demineralization around brackets. J Orofac Orthop 79, 49–56
Bayar Bilen, H., Çokakoğlu, S., (2020). Effects of one-step orthodontic adhesive on microleakage and bracket bond strength: An in vitro comparative study. International Orthodontics 18, 366–373.
Behnan, S.M., Arruda, A.O., González-Cabezas, C., Sohn, W., Peters, M.C., (2010). In-vitro evaluation of various treatments to prevent demineralization next to orthodontic brackets. Am J Orthod Dentofacial Orthop 138, 712.e1–713
Bilal, R., Arjumand, B., (2019). Shear Bond Strength and Bonding Properties of Orthodontic and nano Adhesives: A Comparative In-Vitro Study. Contemp Clin Dent 10, 600–604.
Bishara, S., Soliman, M., R, A., Oonsombat, C., Laffoon, J., Warren, J., (2004). Evaluation of the orthodontic application of two new restorative systems. Hellenic Orthodontic Review 7, 25–32.
Bishara, S.E., Ostby, A.W., (2008). White Spot Lesions: Formation, Prevention, and Treatment. Seminars in Orthodontics 14, 174–182.
Buyuk, S.K., Cantekin, K., Demirbuga, S., Ali Ozturk, M., (2013). Are the low-shrinking composites suitable for orthodontic bracket bonding? Eur J Dent 7, 284–288.
Canbek, K., Karbach, M., Gottschalk, F., Erbe, C., Wehrbein, H., (2013). Evaluation of bovine and human teeth exposed to thermocycling for microleakage under bonded metal brackets. J Orofac Orthop 74, 102–112.
Cucu, M., Driessen, C.H., Ferreira, P.D., Cucu, (2002). The influence of orthodontic bracket base diameter and mesh size on bond strength. SADJ 57, 16–20.
Daub, J., Berzins, D.W., Linn, B.J., Bradley, T.G., (2006). Bond strength of direct and indirect bonded brackets after thermocycling. Angle Orthod 76, 295–300.
Decha, N., Talungchit, S., Iawsipo, P., Pikulngam, A., Saiprasert, P., Tansakul, C.,(2019). Synthesis and characterization of new hydrolytic-resistant dental resin adhesive monomer HMTAF. Des Monomers Polym 22, 106–113.
Farrow, M.L., Newman, S.M., Oesterle, L.J., Shellhart, W.C., (2007). Filled and unfilled restorative materials to reduce enamel decalcification during fixed-appliance orthodontic treatment. Am J Orthod Dentofacial Orthop 132, 578.e1–6.
Hedayati, Z., Farjood, A., (2018). Evaluation of Microleakage under Orthodontic Brackets Bonded with Nanocomposites. Contemp Clin Dent 9, 361–366.
Heintze, S.D., (2013). Clinical relevance of tests on bond strength, microleakage and marginal adaptation. Dental Materials 29, 59–84.
Hilgert, L., Lopes, G., Araújo, E., Baratieri, L., (2008). Adhesive procedures in daily practice: essential aspects. Compendium of continuing education in dentistry 29, 208–218
Joseph, V.P., Rossouw, P.E., Basson, N.J., (1994). Some “sealants” seal—A scanning electron microscopy (SEM) investigation. American Journal of Orthodontics and Dentofacial Orthopedics 105, 362–368.
Kamarudin, Y., Skeats, M.K., Ireland, A.J., Barbour, M.E., (2020). Chlorhexidine hexametaphosphate as a coating for elastomeric ligatures with sustained antimicrobial properties: A laboratory study. Am J Orthod Dentofacial Orthop 158, e73–e82.
Karandish, 2016. Relevance of Micro-leakage to Orthodontic Bonding – a Review. J Dent Biomater 3, 254–260.
Kim, J., Kanavakis, G., Finkelman, M.D., Lee, M., (201). Microleakage under ceramic flash-free orthodontic brackets after thermal cycling. Angle Orthod 86, 905–908.
Knösel, M., Forslund, L., Jung, K., Ziebolz, D., (2012). Efficacy of different strategies in protecting enamel against demineralization during fixed orthodontic treatment. J Orofac Orthop 73, 194–203.
Lee, M.-J., Kim, J.-Y., Seo, J.-Y., Mangal, U., Cha, J.-Y., Kwon, J.-S., Choi, S.-H., (2020). Resin-Based Sealant with Bioactive Glass and Zwitterionic Material for Remineralisation and Multi-Species Biofilm Inhibition. Nanomaterials 10, 1581
Leizer, C., Weinstein, M., Borislow, A.J., Braitman, L.E., (2010). Efficacy of a filled-resin sealant in preventing decalcification during orthodontic treatment. Am J Orthod Dentofacial Orthop 137, 796–800.
Linjawi, A.I., (2020). Sealants and White Spot Lesions in Orthodontics: A Review. J Contemp Dent Pract 21, 808–814.
Oesterle, L.J., Messersmith, M.L., Devine, S.M., Ness, C.F., (1995). Light and setting times of visible-light-cured orthodontic adhesives. J Clin Orthod 29, 31–36.
Palot, C., Marzin, I., Triconnet, L., (1991)The peripheral joint: an unrecognized element in the bonding of orthodontic appliances]. Orthod Fr 62, 893–898.
Premaraj, T.S., Rohani, N., Covey, D., Premaraj, S., (2017) In vitro evaluation of surface properties of Pro Seal® and Opal® SealTM in preventing white spot lesions. Orthodontics & craniofacial research 20, 134–138.
Ramesh Kumar, K.R., Shanta Sundari, K.K., Venkatesan, A., Chandrasekar, S., (2011). Depth of resin penetration into enamel with 3 types of enamel conditioning methods: a confocal microscopic study. Am J Orthod Dentofacial Orthop 140, 479–485.
Şen, S., Erber, R., Orhan, G., Zingler, S., Lux, C.J., (2020). OCT evaluation of orthodontic surface sealants: a 12-month follow-up randomized clinical trial. Clin Oral Invest 10, 1–12.
Singh, C., Kaur, K., Kapoor, K., (2019). Retention of pit and fissure sealant versus flowable composite: An in vivo one-year comparative evaluation. J Indian Soc Pedod Prev Dent 37, 372-377.
Sonesson, M., Brechter, A., Abdulraheem, S., Lindman, R., Twetman, S., (2020). Fluoride varnish for the prevention of white spot lesions during orthodontic treatment with fixed appliances: a randomized controlled trial. Eur J Orthod 42, 326–330.
Sukontapatipark, W., el-Agroudi, M.A., Selliseth, N.J., Thunold, K., Selvig, K.A., (2001). Bacterial colonization associated with fixed orthodontic appliances. A scanning electron microscopy study. Eur J Orthod 23, 475–484.
Tay, F.R., Gwinnett, A.J., Pang, K.M., Wei, S.H., (1995). Variability in microleakage observed in a total-etch wet-bonding technique under different handling conditions. J. Dent. Res. 74, 1168–1178.
Vasudevan, S., Sundareswaran, S., (2014). Bonding Characteristics of Improved Low Viscosity Adhesives for Orthodontic Use. J Indian Orthod Soc 48, 262–266.
Yagci, A., Uysal, T., Ulker, M., Ramoglu, S.I., (2010). Microleakage under orthodontic brackets bonded with the custom base indirect bonding technique. Eur J Orthod 32, 259–263.