Department of Cardiovascular and Respiratory Physiotherapy, MAEER’S
Physiotherapy College, Pune, Maharashtra, India
Corresponding author email: drismaarumani@gmail.com
Article Publishing History
Received: 15/10/2021
Accepted After Revision: 21/12/2021
The outcome of covid-19 patients with co-morbidities has reported to be poor. Post covid exercise-based rehabilitation may have a major role in improving exercise tolerance and quality of life in post-covid-19 patients with co-morbidities. This case report discusses the clinical scenario of a 35-year-old person who is a known case of stable rheumatic heart disease since 29 years and recently diagnosed with covid-19 moderate pneumonia. He was referred to post covid outpatient department for post-covid physiotherapy rehabilitation. After one month of structured exercise-based rehabilitation, improvement recorded in his SF-12 and 6-minute walk distance. COVID-19 patients with co-morbidities seemed to have a poor prognosis, according to various studies. Post covid exercise-based rehabilitation may have a major role in improving exercise tolerance and quality of life in post-covid-19 patients with co-morbidities. There is no structured rehabilitative protocol designed for such unusual combination as of now hence our study focuses on this lacunae.
This case report discusses the clinical scenario of a 35-year-old person who is a known case of stable Rheumatic heart disease in the last 29 years and recently diagnosed with COVID-19 moderate pneumonia. He was referred to post covid outpatient department for post-covid physiotherapy rehabilitation. The individual followed a structured exercise-based rehabilitation protocol for one month 6 times/week and improvement recorded in his SF-12 and 6-minute walk distance. There was improvement in six-minute walk distance by 150 meters and rate of perceived exertion was also improved from 9 score to 7 in 6-20 borg scale post one month. In comparison to pre-Rehabilitation, SF-12 improved the quality of life in both physical and mental sore. This case report concluded that there was a definite improvement in the walking distance and quality of life of the patient after post COVID physiotherapy rehabilitation.
Covid-19 Moderate Pneumonia, Post-Covid Rehabilitation, Rheumatic
Heart Disease, Short Form-12, Six Minute Walk Distance.
Rumani I, Jaiswal V, Burman D, Shetty R. Impact of Outpatient-Based Exercise Prescription on Stable Rheumatic Heart Disease and Post Coronavirus Infection Individual- A Case Report. Biosc.Biotech.Res.Comm. 2021;14(4).
Rumani I, Jaiswal V, Burman D, Shetty R. Impact of Outpatient-Based Exercise Prescription on Stable Rheumatic Heart
Disease and Post Coronavirus Infection Individual- A Case Report. Biosc.Biotech.Res.Comm. 2021;14(4). Available from: <a href=”https://bit.ly/3I0l2ZD“>https://bit.ly/3I0l2ZD</a>
Copyright © This is an Open Access Article distributed under the Terms of the Creative Commons Attribution License (CC-BY) https://creativecommons.org/licenses/by/4.0/, which permits unrestricted use distribution and reproduction in any medium, sources the original author and sources are credited.
INTRODUCTION
Rheumatic heart disease (RHD) affects >39 million persons globally, with the highest prevalence is seen in low-income countries having limited health care facilities. It is an after effect of Rheumatic fever which occurs after a single or multiple episodes of sore throat due to group A beta-hemolytic streptococci. For these individuals, the COVID-19 outbreak poses a serious problem, as secondary prophylaxis and access to care is likely to be disrupted, due to possibly disabling effects of the disease. (Melo et al. 2018). Cardiovascular disease is the most common comorbidity found in COVID-19 patients (Enrique et al. 2020; Müller-Wieland et al. 2020). The clinical manifestation of Rheumatic heart disease and COVID-19 is challenging, both diseases could develop fever, chills, dyspnea, fatigue, cough, and myalgia. This case is been recorded with the view of observing the effect of structured exercise program on post covid patient with stable RHD, attending post covid outpatient department (Sanyaolu et al. 2020).
COVID-19 patients display wide spectrum of clinical problems, ranging from respiratory failure, an overactive immune system, coagulation issues, renal failure, endocarditis to reduced exercise tolerance. The SARS-CoV-2 virus has the potential to invade human body cells and systems. COVID-19 predominantly affects the upper respiratory system (sinuses, nose, and throat) and the lower respiratory tract (bronchitis, pneumonia, and bronchitis). Since the virus enters host cells through the receptor for the enzyme angiotensin-converting enzyme 2 (ACE2), which is most prevalent on the surface of type II alveolar cells in the lungs, the lungs are the organs most impacted by COVID-19 (Harrison et al. 2020). The Novel Corona virus can impact the heart and circulatory system, the brain directly (encephalitis) and indirectly (e.g. secondary to hypoxia or vascular thrombosis), the kidney and renal function, blood coagulation, and the gastrointestinal tract, in addition to the respiratory system (Wade 2020; Verdecchia et al. 2020).
As per WHO following a severe COVID-19 sickness, exercise rehabilitation is a vital aspect of recovery. It can aid in improving fitness, reducing dyspnea, increasing muscle strength, improving balance and coordination, improving thinking, reducing stress and improving mood, increasing confidence, and increasing energy level (WHO 2020). There is no structured rehabilitative protocol designed for such unusual combination as of now hence our study focuses on this lacuna.
The outcome measures used to assess the impact of exercise was 6-minute walk distance and for health-related quality of life was SF-12. The 6-minute walk test (6 MWT) is a submaximal exercise test that involves measuring walking distance in 6 minutes. 6-minute walk test routinely performed for patients with moderate to severe pulmonary disease to quantify their functional capacity. 6-minute walk test often captures the coexisting extra pulmonary manifestations of chronic respiratory disease, including cardiovascular disease, frailty, sarcopenia, and cancer (Agarwala and Salzman 2020).
In contrast with cardiopulmonary exercise stress testing, this test does not require complex equipment or technical expertise. The SF-12 is a health-related quality-of-life questionnaire that consists of twelve items that examine physical and mental health by measuring eight health areas. General Health (GH), Physical Functioning (PF), Role Physical (RP), and Body Pain (BP) are all physical health-related dimensions. Vitality (VT), Social Functioning (SF), Role Emotional (RE), and Mental Health Scales are all mental health-related dimensions (Huo et al. 2018; (Agarwala and Salzman 2020).
The aim of rehabilitation is to improve recovery and reduce disability in patients with COVID-19. As of now, no studies have been reported with such unusual combination of RHD and COVID-19 given a physiotherapy rehabilitation protocol, hence this case report will manifest a stepping-stone to form a standard COVID Rehabilitation protocol for rheumatic heart disease patients being affected with COVID-19.
METHODOLOGY
A 35-year-old male, a known case of stable rheumatic heart disease referred to post covid outpatient department, presented with complaints of grade 2 dyspnea on a modified medical research council scale and was gradual in onset. Aggravating factors for dyspnea were climbing stairs, walking more than 5-10 min, and relieving factors were rest or sitting on a chair. He also complained of sore throat and dry cough. After being diagnosed with COVID-19 moderate pneumonia, he was hospitalized for 2 days in a dedicated COVID-19 hospital setup, followed by 14 days of home-quarantine. He was on standard COVID-19 medical management protocol as per the guidelines which included cholecalciferol capsules 1000 IU, vitamin C tablets 500 mg, and azithromycin 500 mg (Launois et al. 2012).
On general examination all his vitals were within the normal limits i.e., blood Pressure was 120/88 mmHg, heart rate was 67 beats per min, respiratory rate was 22 breaths/min, rate of perceived exertion was 11 using standard 6/20 rating of perceived exertion Borg scale. Oxygen saturation, was 98% at rest, measured using a standard pulse oximeter of Meditive Company. Systemic examination of the cardiovascular system revealed pan systolic murmur. He is on regular medication, which is a tablet, digoxin 0.25 mg for Rheumatic heart disease. Respiratory system examination shows reduced chest expansion and chest excursion. On auscultation, his breath sounds; air entry was reduced in bilateral middle and lower zones, bronchial type of breathing were heard which may be due to post covid pulmonary fibrosis, no foreign sounds (Williams 2017).
After the detailed assessment, a six-minute walk test was performed as per American thoracic society guidelines in which the patient completed a distance of 240 meters as compared to age predicted distance of 610 meters. He walked 61% less than the age predicted calculated, by formula. Pre- Six-minute walk test vitals were; blood pressure was 120/88 mm of Hg, a saturation of oxygen was 98% at room air, heart rate was 67 beats/min and the rate of perceived exertion was 9 on a 6-20 Borg scale.
Post-test immediate his vital was; blood pressure 130/92 mm of Hg, oxygen saturation dropped to 93% immediate post 6-minute walk test, heart rate was 55 beats/min and his rate of perceived exertion was 11 on 6-20 Borg scale (Enright and Sherrill 1998; Issues et al. 2002; Williams 2017). Vital parameters settled to baseline in 5 minutes post-test. The exercise protocol was formulated base on the clinical assessment and six-minute walk distance as shown in table 1.
The individualized exercise prescription protocol was of 45mins-1hour duration consisting of warm-up, breathing exercises, circuit training included followed by a cool-down with a 1-month follow-up as shown in table 2. The entire rehabilitation session was uneventful. The outcome measures pre rehabilitation were SF-12 which scored SF-12 is physical score: 37.9548, mental score: 43.25045, and 6-minute walk distance in which the patient walked 8 laps in 6 minutes i.e. 240 meters, and rate of perceived exertion was 9 in 6-20 Borg scale. Written consent is taken from the patient to publish his case.
RESULTS AND DISCUSSION
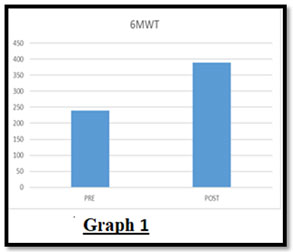
The patient 6-minute walk distance pre rehabilitation was 240 meters and post-rehabilitation, the total 6-minute walk distance increased to 390 meters as shown in Fig 1
Figure 1: Pre and Post 6-minute walk test
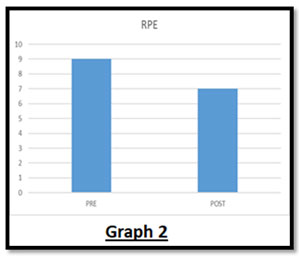
Rate of perceived exertion was 11 in 6-20 Borg scale pre rehabilitation and post-rehabilitation rate of perceived exertion was 7 as shown in Fig 2.
Figure 2: Pre and post rate of perceived exertion
- The quality of life improved as compared to pre-rehabilitation.
- Pre rehabilitation scores of SF-12 were physical score: 37.9548, mental score: 43.25045 and post-rehabilitation scores of SF-12 were increased to, physical score: 44.61544, mental score: 56.83795 as shown in Fig 3.
Figure 3
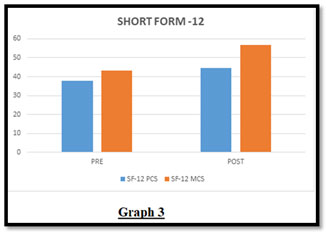
Short form-12 Pre and Post Physical Score (PCS), Pre and Post Mental Score (MCS)
Individuals with stable rheumatic heart disease have reported having reduced exercise tolerance and quality of life, which can be pronounced by post covid sequelae (Melo et al. 2018; Sanyaolu et al. 2020).
Table 1
| AEROBIC | RESISTANCE | |
| FREQUENCY | 4 days per week | 2 days per week |
| INTENSITY | Mild to moderate 40-59% of HRR/ 12-13 OF RPE | 60-70% of 1RM |
| TIME | More than 30 mins per day (min 10 min of 1 bout) | 2-4 set of 8 -12 reps of each of major muscle group |
| TYPE | Cycling and treadmill | Multi gym and free weights |
Table 2
| Warm up
10 minutes 10 reps each |
Cool down
10 minutes 30 sec hold x 3 reps each
|
Breathing exercises
10 reps x 2 set
|
Upper-limb strengthening
10 reps x 2 set |
Lower-limb strengthening
10 reps x 2 set |
| Neck movements:
flexion- extension Side flexion (right-left) Rotations (clockwise and anticlockwise) Shoulder: elevation and depression Rotations (clockwise and anticlockwise) Flexion-extension Abduction-adduction Elbow: flexion-extension Wrist: rotations (clockwise and anticlockwise) Flexion-extension Trunk: rotations (right-left) Side bending (right-left) Pelvis: rotations (clockwise and anticlockwise) Hip: flexion and extension Abduction -adduction Knee: flexion-extension Ankle: rotations (clockwise and anticlockwise) Dorsiflexion Plantarflexion |
Stretching of forearm flexors and extensors, biceps, triceps, trapezius, shoulder capsule, quadriceps, hamstrings, gastrosoleus.
|
Diaphragmatic breathing
Thoracic mobility exercises Pursed-lip breathing in dyspnoea relieving position Segmental expansion exercises
|
Wrist
Flexors Extensors Elbow Flexors (biceps) Extensors (triceps) Shoulder shrugs (upper trapezius) Flexors (anterior deltoid, coracobrachialis, pectoralis major) Abductors (middle deltoid, supraspinatus,) External rotators (posterior deltoid, infraspinatus, teres minor) Seated row and latpulldown (Lattssimusdorsi) Chest protractors (pectoralis major) Retractors (rhomboids major and minor)
|
Squats (quadriceps and gluteus Maximus)
Lunges (quadriceps and gluteus Maximus) Calf raises (gastrocnemius and soleus) Leg curls (hamstrings) Dynamic quads (quadriceps) Hip- flexors (ilio-psoas) Extensors (gluteus maximus) Abductors (gluteus medius and minimus) Adductors (adductor longus, brevis, magnus)
|
Detailed Exercise Program
In the current case report, we observed 61 % lower 6-minute walk distance as compared to the predicted 6-minute walk distance as per age, height & weight. 6-minute walk distance significantly improved after the post covid exercise-based rehabilitation by 150 meters, which is more than the minimal clinical difference change (Wise and Brown 2005). Similar results have reported for improvement in 6-minute walk distance in post-covid-19 patients with co-morbidities. The rate of perceived exertion also significantly improved after the post covid exercise-based rehabilitation by 2 points, which is more than minimal clinical difference. Similarly, Claudio et al. also reported improvement in the rate of perceived exertion after inpatient rehabilitation in post-intensive care unit COVID-19 patients (Ries 2005; Medica et al. 2021). Quality of life has also significantly improved, which measured using the SF-12 scale. SF-12 improvement was 6.71 for the physical score and 13.63 for the mental score, which is more than its minimal clinical difference (Parker et al. 2013; Tozato et al. 2021).
There was not much improvement in physical score pre- and post-rehabilitation, but adequate improvement in mental score by 13.63 points. Hence, there was an overall improvement in quality of life. Studies show improvement in quality of life after post-covid exercise-based rehabilitation. Wenguang Xia et al. also discussed improvement in SF-12 scored post rehabilitation (Li et al. 2021). Exercise training did not only increase the exercise capacity of the patient but also improved the quality of life as well (Luoto et al. 2012). The World Health Organization (WHO) has declared a global coronavirus pandemic for 2019.
Since then, the disease has infected over 12 million people in countries worldwide. Several studies, including one meta-analysis, have reported cardiovascular involvement along with COVID-19 disease. The most common comorbidity in COVID-19 patients is cardiovascular disease. RHD and COVID-19 have similar clinical symptoms, including fever, chills, dyspnea, tiredness, cough, and myalgia in both cases (Murdoch 2009; Tozato et al. 2021).
However, in developing countries, COVID-19 was seen in conjunction with Rheumatic heart disease which is a sequale to infective endocarditis, and initial screening might well be ambiguous. Various studies have reported physiotherapy rehabilitation is beneficial in post COVID patients(Sheehy 2020; CURCI et al. 2020; Demeco et al. 2020). In our case report we have discussed a rehabilitation of an unusual combination of RHD and COVID-19 infection and to our knowledge rehabilitation of similar combination have not been published. Physiotherapy Rehabilitation could be a key strategy for reducing the impact of COVID-19 on an individual’s health and function.
It can also reduce Intensive Care Unit -admission related complications, such as Post Intensive Care Syndrome (PICS), Intensive care unit acquired weakness (ICUAW). The aim of rehabilitation is to improve recovery and reduce disability in patients with COVID-19. As of now, no studies have been reported with such unusual combination of RHD and COVID-19 given a physiotherapy rehabilitation protocol, hence this case report will manifest a stepping-stone to form a standard COVID Rehabilitation protocol for rheumatic heart disease patients being affected with COVID-19 (Barker-Davies et al. 2020).
CONCLUSION
The findings of this case report concluded that there was a definite improvement in the walking distance and quality of life of the patient after physiotherapy rehabilitation. There was improvement in six-minute walk distance by 150 meters and rate of perceived exertion was also improved from 9 score to 7 in 6-20 borg scale post one month. In comparison to pre-Rehabilitation, SF-12 improved the quality of life in both physical and mental sore.
Ethical clearance: Institutional ethics committee clearance was undertaken.
Ref. No. EC/NEW/INST/2019/377/46
Informed Consent: An informed consent was taken from the patient prior to collection of data. All necessary information was given to him and doubts were cleared.
Source of funding: self
Conflict of Interests: Authors declare no conflict of interests to disclose.
Data Availability Statement: The database generated and /or analysed during the current study are not publicly available due to privacy, but are available from the corresponding author on reasonable request.
REFERENCES
Agarwala, P., and Salzman, S.H., (2020). Six-Minute Walk Test: Clinical Role, Technique, Coding, and Reimbursement. Chest 157, 603–611.
Amir, E., Fatemeh, J., Neda, P., et al. (2020). Prevalence of Underlying Diseases in Hospitalized Pa- tients with COVID-19: a Systematic Review and Meta- Analysis. Arch. Acad. Emerg. Med. 8, e35–e35.
Amir, M., Djaharuddin, I., Sudharsono, A. and Ramadany, S., (2020). COVID-19 concomitant with infective endocarditis: a case report and review of management. International Journal of Infectious Diseases, 98, pp.109-112.
Barker-Davies, R.M., O’Sullivan, O., Senaratne, K.P.P., et al. (2020). The Stanford Hall consensus statement for post-COVID-19 rehabilitation. Br. J. Sports Med. 54, 949–959.
CURCI, C., PISANO, F., BONACCI, E., et al. (2020). Early rehabilitation in post-acute COVID-19 patients: Data from an Italian COVID-19 Rehabilitation Unit and proposal of a treatment protocol. Eur. J. Phys. Rehabil. Med. 56, 633–641.
Demeco, A., Marotta, N., Barletta, M., et al. (2020). Rehabilitation of patients post-COVID-19 infection: a literature review. J. Int. Med. Res. 48.
Enright, P.L., and Sherrill, D.L., (1998). Reference Equations for the Six-Minute Walk in Healthy Adults. American journal of respiratory and critical care medicine, 158(5), pp.1384-1387.
Harrison, A.G., Lin, T., and Wang, P., (2020). Mechanisms of SARS-CoV-2 Transmission and Pathogenesis. Trends Immunol. 41, 1100–1115.
Huo, T., Guo, Y., Shenkman, E., et al. (2018). Assessing the reliability of the short form 12 (SF-12) health survey in adults with mental health conditions : a report from the wellness incentive and navigation (WIN) study, 1–8.
Issues, S., Test, M.W., Equipment, R., et al. (2002). American Thoracic Society ATS Statement: Guidelines for the Six-Minute Walk Test 166, 111–117.
Launois, C., Barbe, C., Bertin, E., et al. (2012). The modified Medical Research Council scale for the assessment of dyspnea in daily living in obesity: a pilot study. BMC Pulm. Med. 12.
Li, J.A., Xia, W., Zhan, C., et al. (2021). Effectiveness of a telerehabilitation program for COVID-19 survivors (TERECO) on exercise capacity, pulmonary function, lower limb muscle strength, and quality of life: a randomized controlled trial. medRxiv.
Luoto, R., Moilanen, J., Heinonen, R., et al. (2012). Effect of aerobic training on hot flushes and quality of lifea randomized controlled trial. Ann. Med. 44, 616–626.
Medica, E.M., Curci, C., Negrini, F., et al. (2021). Functional outcome after inpatient rehabilitation in post-intensive care unit COVID-19 patients : findings and clinical implications from a real-practice retrospective study, European Journal of Physical and Rehabilitation Medicine.
Melo, A.L.S.D., Lira, Y.F.B.D., Lima, L.A.B., et al. (2018). Exercise tolerance, pulmonary function, respiratory muscle strength, and quality of life in children and adolescents with rheumatic heart disease. Rev. Paul. Pediatr. 36, 199–206.
Müller-Wieland, D., Marx, N., Dreher, M., et al. (2020). COVID-19 and Cardiovascular Comorbidities. Exp. Clin. Endocrinol. Diabetes.
Murdoch, D.R (2009). Clinical Presentation, Etiology, and Outcome of Infective Endocarditis in the 21st Century. Arch. Intern. Med. 169, 463.
Parker, S.L., Godil, S.S., Shau, D.N., et al. (2013). Assessment of the minimum clinically important difference in pain, disability, and quality of life after anterior cervical discectomy and fusion ; Clinical article. J. Neurosurg. Spine 18, 154–160.
Ries, A.L., (2005). Minimally clinically important difference for the UCSD Shortness of Breath Questionnaire, Borg Scale, and Visual Analog Scale. COPD J. Chronic Obstr. Pulm. Dis. 2, 105–110.
Sanyaolu, A., Okorie, C., Marinkovic, A., et al. (2020). Comorbidity and its Impact on Patients with COVID-19. SN Compr. Clin. Med. 2, 1069–1076.
Sheehy, L.M. (2020). Considerations for postacute rehabilitation for survivors of COVID-19. JMIR Public Heal. Surveill. 6, 1–8.
Sisnieguez, C.E.L., Espeche, W.G. and Salazar, M.R., (2020). Arterial hypertension and the risk of severity and mortality of COVID-19. European Respiratory Journal, 55(6).
Tozato, C., Ferreira, B.F.C., Dalavina, J.P., et al. (2021). Cardiopulmonary rehabilitation in post-COVID-19 patients: case series. Revista Brasileira de Terapia Intensiva, 33(1), pp.167-171.
Verdecchia, P., Cavallini, C., Spanevello, A., et al. (2020). The pivotal link between ACE2 deficiency and SARS-CoV-2 infection. Eur. J. Intern. Med. 76, 14–20.
Wade, D.T., (2020). Rehabilitation after COVID-19:an evidence-based approach. Clinical Medicine, 20(4), 359–364.
Williams, N. (2017). The Borg Rating of Perceived Exertion (RPE) scale. Occup. Med. (Chic. Ill). 67, 404–405.
Wise, R.A., and Brown, C.D. (2005). Minimal clinically important differences in the six-minute walk test and the incremental shuttle walking test. COPD J. Chronic Obstr. Pulm. Dis. 2, 125–129.


