*1, 2, 4Department of Pediatric Dentistry and Orthodontics, College of
Dentistry, King Saud University, Riyadh, Saudi Arabia.
3, 5, 6,Dental Department, Security Forces Hospital
Program, Riyadh, Saudi Arabia.
Corresponding author email: hkawari@ksu.edu.sa
Article Publishing History
Received: 27/05/2021
Accepted After Revision: 22/07/2021
The literature contains contradictory evidence on the association between malocclusion and oral health-related quality of life (OHRQoL) in different populations. OHRQoL is a multi-dimensional construct that comprises a subjective assessment of how an individual ‘s oral health impacts their comfort, functional, psychological, social well-being and overall quality of life. This study aimed to evaluate the relationship between gender, age, malocclusion severity and OHRQoL in Saudi patients seeking orthodontic treatment at the King Saud University Dental Hospital in Riyadh, Saudi Arabia. A cross-sectional study was done on a random sample of 108 orthodontic patients aged 14–25 years. The orthodontic treatment needs of each participant were assessed using the Dental Health Component of the Index of Orthodontic Treatment Needs (IOTN-DC). While, the oral heath quality of life was evaluated by asking the participant to complete the Oral Health Impact Profile (OHIP-14) questionnaire.
The participants generally had good OHRQoL. No association was found between their OHIP-14 scores and IOTN-DC grades. The oral health quality of life of participants with “borderline treatment needs” was strongly affected by psychological disability and psychological discomfort. In particular, Females with ‘borderline need of treatment’ showed positive impact on oral health than males. Overall, malocclusion did not have a major impact on OHRQoL. This study found that malocclusion had no discernible detrimental effects on OHRQoL and its domains. Only the borderline treatment group reported that malocclusion had a significant negative impact on psychological discomfort and psychological disability. No variations in the influence of malocclusion on oral health quality were identified between the age groups. However, the female participants reported a significant detrimental impact of malocclusion on their oral health quality.
Ohrqol, OHIP-14, IOTN-DC, Malocclusion, Orthodontics
Alkawari H, Baidas L, Al-Sadhan N, Alkahlan L, Almobarraz R, Bin-Sufayan A. Impact of Malocclusion on Oral Health-Related Quality Among Saudi Orthodontic Patients. Biosc.Biotech.Res.Comm. 2021;14(3).
Alkawari H, Baidas L, Al-Sadhan N, Alkahlan L, Almobarraz R, Bin-Sufayan A. Impact of Malocclusion on Oral Health-Related Quality Among Saudi Orthodontic Patients. Biosc.Biotech.Res.Comm. 2021;14(3). Available from: <a href=”https://bit.ly/3Cw2cGP”>https://bit.ly/3Cw2cGP</a>
Copyright © This is an Open Access Article distributed under the Terms of the Creative Commons Attribution License (CC-BY). https://creativecommons.org/licenses/by/4.0/, which permits unrestricted use distribution and reproduction in any medium, provided the original author and sources are credited.
INTRODUCTION
In recent years, oral health-related quality of life (OHRQoL) has gained traction amongst healthcare professionals in general and orthodontists in particular. According to a US surgeon general, OHRQoL is a multi-dimensional construct that comprises a subjective assessment of how an individual ‘s oral health impacts their comfort, functional, psychological, social well-being and overall quality of life (DeGuzman et al., 1995). In the World Oral Health Report (2003), the World Health Organization (WHO) recognised the influence of oral health on quality of life and presented it as an essential component of its Global Oral Health Program.
Multiple-item questionnaires are the most widely used instruments to assess the impact of personality traits as well as functional and psychosocial aspects on OHRQoL (Feu et al., 2010). Several instruments have been carefully verified to evaluate the psychometric factors, such as validity and reliability. The shortened version of the Oral Health Impact Profile (OHIP-14) is the most efficient and commonly used method for assessing OHRQoL (Slade et al., 1997; Olkun and Sayar, 2019; Baidas et al., 2020; Kolawole and Ayodele-Oja, 2021).
Since malocclusion can be perceived differently by affected individuals (de-Oliveira and Sheiham, 2004; Hassan et al., 2014) and a person’s self-awareness of the malocclusion reported in a manner that does not reflect its severity (Borzabadi-Farahani and Borzabadi-Farahani, 2011), the OHIP-14 can be useful for quantifying how malocclusion impacts an individual’s well-being. Thus, oral health practitioners are encouraged to apply the OHIP-14 in the clinical practice, dental research and dental education. Several indices have been established to address malocclusion, including the Index of Treatment Need (IOTN) and the Index of Complexity Outcome and Need (ICON; Borzabadi-Farahani and Borzabadi-Farahani, 2011).
The IOTN has been widely utilised to assess actual treatment needs in people with varied ethnic backgrounds, owing to its ease of use and its greater diagnostic popularity in the Middle East than the ICON (Hasan and Amin, 2010). Despite the fact that malocclusion is neither a disease nor a harmful condition, it has well-documented physical, social and psychological effects on natural life. According to systematic and meta-analyses, malocclusion has a detrimental influence on an individual’s overall quality of life (Andiappan et al., 2015; Dimberg et al., 2015; Kragt et al., 2016; Kolawole and Ayodele-Oja, 2021).
The association between malocclusion and OHRQoL has been studied in different populations and age groups (Elmahgoub and Abuaffan 2015; Singh et al., 2019; Paes-da-Silva et al., 2020; Elyashkhil et al., 2021; Kolawole and Ayodele-Oja, 2021). For example, one study reported that the impact of malocclusion on OHRQoL in children likely differs from that of adults because of variations in their self-perception and awareness of various oral conditions (de Oliveira and Sheiham, 2004). Moreover, the literature has demonstrated that gender greatly influences the impact of malocclusion on OHRQoL, although perceptions of malocclusion remain a controversial issue (Elmahgoub and Abuaffan, 2015; Elyaskhil et al., 2021).
Crucially, there are conflicting data on the relationship between malocclusion and OHRQoL in adolescents and children. Certain studies found that some adolescents with normative orthodontic treatment needs (as measured by the IOTN-DC) do not have their OHRQoL negatively impacted by malocclusion (de-Oliveira and Sheiham, 2004; Elmahgoub and Abuaffan, 2015).
Overall, the relationships between clinical indicators of malocclusion (IOTN-DC) and subjective indicators of malocclusion impact (OHIP-14) require further investigation (Onyeaso, 2009; Olkun and Sayar, 2019). Hence, the present study evaluated the relationships between gender, age, malocclusion severity and OHRQoL in Saudi patients seeking orthodontic treatment at the King Saud University Dental Hospital.
MATERIAL AND METHODS
This cross-sectional study enrolled 108 adolescents and young adults aged 14–25 years who were either self-referred or referred by their general dental practitioners to the orthodontic clinics at the Faculty of Dentistry, King Saud University which is one of the kingdom’s largest dental treatment and referral hospitals. These clinics provide high-quality care to insured university students, employees and their families. Before they began any orthodontic treatments, the participants were recruited based on their orthodontic screenings. The sample size calculation was carried out using G* Power Software (3.1.19.4 ed.) and based on prior studies (Hassan and Amin, 2010; Hassan et al., 2014).
A sample size of 100 participants was required to show a significant change in their OHRQoL (α=0.05), with an effect size of 0.4 and a power of 90%. This study included participants in good dental and general health who had not undergone any previous orthodontic treatments. Moreover, it excluded individuals who were undergoing active orthodontic treatment and/or required a surgical intervention, had medical conditions, had previously received orthodontic treatment, possessed severe dentofacial anomalies such as cleft lip and palate, had untreated dental caries and/or had poor periodontal health. These criteria were selected to ensure an unbiased assessment of the participants’ quality of life and achieve a homogeneous population.
Ethical Statement: This study was approved by the Clinical Dental Research Centre (FR0276) and the ethics board. All eligible participants or their caregivers gave their written consent after they were fully informed of the nature of this study and had agreed to participate.
OHIP-14: The OHIP-14 is a self-administered questionnaire that measures quality of life using 14 items in seven domains: functional limitation, physical pain, psychological discomfort, physical disability, psychological disability, social disability and handicap. Each dimension is measured with two questions. The participants were asked how frequently they had experienced negative effects in these dimensions. The questionnaire uses a five-point Likert scale: 0=never; 1=hardly-ever; 2=occasionally; 3=fairly often and 4=very often. The participants were asked to rate how frequently they experienced oral health issues. The sum of the domain scores can range from 0 to 8, while the OHIP‑14 scores can range from 0 to 56. High OHIP‑14 scores represent a strong negative impact of oral health issues on OHRQoL (Demirovic et al., 2019; Baidas et al., 2020).
The English version of the OHIP-14 was translated into Arabic and then linguistically and culturally adapted using the forward-back translation technique (Demirovic et al., 2019; Baidas et al., 2020). In this procedure, two bilingual dentists independently translated the English version to Arabic. Next, they conferred and produced an Arabic version, which was then translated back to English by two professional translators who had never seen the original version. The conceptual equivalence between the English version of the OHIP-14 and the back-translated version was confirmed by an expert committee of five dental consultants with different specialties.
The final Arabic version was pilot tested on a convenience sample of 10 participants who were not included in the study sample. The comprehensiveness of the instrument was tested by interviewing each participant after they had filled out the questionnaire. The goal was to identify whether they had understood the meaning of each questionnaire item and their chosen response. Based on the participants’ responses, changes were made to some questions to improve intelligibility. Cronbach’s alpha indicated reasonable internal consistency (α=0.896) for Arabic OHIP‑14 and acceptable reliability.
IOTN-DC: The IOTN‐DC instrument assesses the need for orthodontic treatment in patients, and it determines a grade based on the most severe malocclusion feature: grade 1=no treatment needed, grade 2=minimal treatment needed, grade 3=borderline treatment needed and grades 4 and 5=definite treatment needed. In this study, each participant was clinically examined, and their casts were measured on the missing, overjet, crossbite, displacement and overbite (MOCDO) hierarchical scale to identify their most severe features (Guillemin et al., 1993; Shaw et al., 2007). The IOTN-DC calibration exercises were conducted at the orthodontic clinic by an expert orthodontist. Ten orthodontic study models were evaluated by two examiners using two-week intervals to support inter-examiner and intra-examiner reliability (k=0.86).
Statistical analysis: The data were analysed using the Statistical Package for Social Studies (SPSS 22; IBM Corp., New York, NY, USA). Continuous variables were expressed as means, standard deviations and confidence intervals, whereas categorical variables were expressed as percentages. Cronbach’s alpha was used to assess the reliability and internal consistency of the items in the questionnaire. The t-test compared the differences in the total mean scores of the OHIP-14 between the gender and age groups. One-way analysis of variance (ANOVA) and post-hoc tests evaluated the differences between the domains of the OHIP-14 according to the orthodontic treatment need grades. Multiple linear regression and simple linear regression determined the association between the ordinal factors (i.e., age, gender and treatment need) and the OHIP-14 scores.
RESULTS AND DISCUSSION
As shown in Figure 1, most of the 108 participants were female (75.93%). Moreover, 52.78% of the participants were young adults (20–25 years) and 47.22% were adolescents (14–19 years). Regarding malocclusion severity, 41% of participants had grade 4 malocclusion, indicating a definitive need for treatment. In addition, 24% of the participants had grade 3 malocclusion, 18% had grade 2 malocclusion, 12% had grade 5 malocclusion, and 5% had grade 1 malocclusion (Figure 2).
Figure 1: Distribution of the participants’ genders and ages
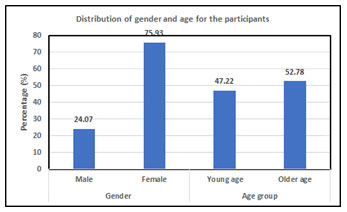
Figure 2: Distribution of the participants’ treatment need grades
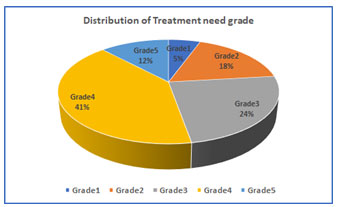
Table 1. displays the means and standard deviations of the OHIP-14 scores and their seven domains. Psychological disability had the highest mean score (2.15), whereas functional limitation had the lowest score (0.81).
Table 1. Means and standard deviations of the OHIP-14 scores
| Domain | Mean* | SD |
| Functional limitation | 0.81 | 1.32 |
| Physical pain | 1.89 | 1.94 |
| Psychological discomfort | 1.91 | 2.52 |
| Physical disability | 1.13 | 1.61 |
| Psychological disability | 2.15 | 2.17 |
| Social disability | 1.40 | 1.90 |
| Handicap | 1.36 | 1.78 |
| OHIP-total | 10.67 | 9.91 |
*Mean score for every domain out of 8 and for the total OHIP score out of 56; SD=standard deviation
Table 2. compares the OHIP-14 scores of the different gender and age groups. There was a statistically significant difference between the mean OHIP-14 scores of the male and female participants (p=0.002), while the difference between the age groups was not statistically significant (p>0.05).
Table 2. Comparison of the OHIP-14 scores between gender and age groups
| Group | Mean | SD | Mean Difference | 95% CI | t test | p value | ||
| Lower | Upper | df | ||||||
| Gender | ||||||||
| Male | 6.35 | 6.78 | -5.69 | -10.00 | -1.38 | -2.62 | 106.00 | 0.002* |
| Female | 12.04 | 10.38 | -5.69 | -9.20 | -2.18 | -3.24 | ||
| Age group | ||||||||
| Young age | 9.33 | 8.74 | -2.53 | -6.30 | 1.25 | -1.33 | 106.00 | 0.182 |
| Older age | 11.86 | 10.79 | -2.53 | -6.26 | 1.21 | -1.34 | ||
| * Significant p-value<0.05; CI: Confidence interval of the difference | ||||||||
Table 3. displays the results of the one-way ANOVA test. Statistically significant differences were found between the OHIP-14 scores of participants with different severities of malocclusion. Clearly, psychological discomfort and psychological disability were significantly affected domains in grade 3 participants. In contrast, only psychological discomfort was significantly affected in grade 4 participants.
Table 3. Comparison of the IOTN-DC grades and the OHIP-14 domains
| IOTN-DC | Grade 1 | Grade 2 | Grade 3 | Grade 4 | Grade 5 | |||||||
| OHIP-14 domains | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | p value | |
| Functional limitation | 0.00 | 0.00 | 0.63 | 1.16 | 0.81 | 1.23 | 0.91 | 1.48 | 1.15 | 1.41 | 0.448 | |
| Physical pain | 1.33 | 1.21 | 2.11 | 2.05 | 2.38 | 2.02 | 1.61 | 1.97 | 1.77 | 1.79 | 0.506 | |
| Psychological discomfort | 1.83 | 2.23 | 2.89 | 2.73 | 3.23* | 2.96 | 1.05* | 1.93 | 0.77 | 1.54 | 0.001* | |
| Physical disability | 0.50 | 0.84 | 0.84 | 1.68 | 1.46 | 1.70 | 1.18 | 1.70 | 1.00 | 1.22 | 0.604 | |
| Psychological disability | 1.67 | 1.63 | 2.58 | 2.52 | 3.19* | 2.51 | 1.45 | 1.55 | 2.00 | 2.24 | 0.018* | |
| Social disability | 1.33 | 1.75 | 1.95 | 2.32 | 2.08 | 2.24 | 0.82 | 1.33 | 1.23 | 1.79 | 0.055 | |
| Handicap | 1.17 | 1.33 | 1.74 | 2.16 | 2.04 | 2.18 | 0.91 | 1.31 | 1.08 | 1.55 | 0.094 | |
| Total OHIP score | 7.83 | 7.60 | 12.74 | 11.67 | 15.26* | 11.40 | 7.93 | 7.88 | 9.00 | 8.24 | 0.027* | |
*ANOVA; significant p value<0.05
Table 4. shows a pairwise comparison of the IOTN-DC grades with the domains of the OHIP-14. When the OHIP-14 domains were compared with the IOTN-DC grade pairs (grade 2 vs grade 4, grade 3 vs grade 4 and grade 5 vs grade 3), significant differences were found (p=0.49, p=0.003 and p =0.026, respectively). When grade 3 was compared to grade 4 with respect to psychological disability, the results showed a significant difference (p=0.011). Likewise, another significant difference was found regarding the total OHIP-14 scores (p=0.025).
Table 4. Pairwise comparison of the IOTN-DC grades and the OHIP-14 domains
| Dependent Variable | Mean Difference | Std. Error | p value | 95% CI | |||
| Lower | Upper | ||||||
| Psychological discomfort | Grade2 | Grade 4 | 1.85* | 0.64 | 0.049 | 0.00 | 3.70 |
| Grade 3 | Grade 4 | 2.19* | 0.58 | 0.003 | 0.52 | 3.85 | |
| Grade 5 | Grade 3 | -2.46* | 0.80 | 0.026 | -4.74 | -0.18 | |
| Psychological disability | Grade 3 | Grade 4 | 1.74* | 0-.52 | 0.011 | 0.26 | 3.22 |
| Social disability | Grade3 | Grade 4 | 1.26 | 0.46 | 0.071 | -0.06 | 2.57 |
| Total OHIP-14 scores | Grade 3 | Grade 4 | 7.34* | 2.37 | 0.025 | 0.53 | 14.14 |
* CI=Confidence interval; post-hoc test; significant p value<0.05
The correlation analysis did not find an association between the OHIP-14 scores and the IOTN-DC grades (r=0.147; p=0.128). Table 5 shows the results of the multivariate regression analysis on the factors (i.e., gender, age group and treatment need) that affected the OHIP-14 scores. The results showed that gender was significantly and positively associated with OHIP-14 score. Female participants had higher impact scores than male participants (B=9.650; p=0.012). This association was also strong in the simple linear regression model (B=5.690; p=0.010; 95% CI=1.383–9.998). There was approximately 6.1% variability amongst genders (r2= 0.061; Table 6).
Table 5. Multivariate linear regression model showing the association between OHIP-14 score and gender, age group and treatment need grade
| Independent Variable | B | t | 95.0% CI for B | p value | |
| Lower | Upper | ||||
| Gender | 9.650 | 2.634 | 2.262 | 17.038 | 0.012* |
| Age group | -1.391 | -.377 | -8.823 | 6.041 | 0.708 |
| Treatment need grade | -1.150 | -.635 | -4.802 | 2.501 | 0.529 |
* Significant p value<0.05; dependent variable: OHIP-14; reference category; young age, male
Table 6. Simple linear regression model showing the association between OHIP-14 score and gender, age group and treatment need grade
| Independent Variable | R2 | B | t | 95.0% CI B | p value | |
| Lower | Upper | |||||
| Gender | 0.061 | 5.690 | 2.619 | 1.383 | 9.998 | 0.010* |
| Age group | 0.016 | 2.526 | 1.327 | -1.249 | 6.302 | 0.187 |
| Treatment need grade | 0.022 | -1.353 | -1.535 | -3.101 | .395 | 0.128 |
* Significant p value<0.05; dependent variable: OHIP-14; reference category; young age, male
How patients evaluate their health-related quality of life is becoming increasingly important to clinicians, and it may prove useful in cosmetic and elective procedures alike (Tsakos et al., 2006; Mandall et al., 2006). Although malocclusion has well-known physical and psychological implications, research on these effects is still contradictory, which could be due to a lack of standardised assessment methods.
The OHIP-14 have been used in both general populations and individuals with specific oral diseases (Mandall et al., 2006). Different studies applied it to evaluate the effects of malocclusion on quality of life (Hassan and Amin, 2010; Borzabadi-Farahani and Borzabadi-Farahani, 2011; Hassan et al., 2014; Andiappan et al., 2015; Dimberg et al., 2015; Elmahgoub and Abuaffan, 2015; Kragt et al., 2016; Singh et al., 2019; Paes-da-Silva et al., 2020; Elyaskhil et al., 2021; Kolawole and Ayodele-Oja, 2021).
Both cross-sectional and longitudinal investigations tested the OHIP’s sensitivity and specificity. Notably, previous studies used the validated Arabic version of the OHIP-14 and the IOTN-DC in Saudi orthodontic patients (Al-Jundi et al., 2007; Hassan and Amin, 2010; Hassan et al., 2014; Baidas et al., 2020). The participants in this study had lower OHIP14 scores, than other studied populations, signifying that their perception of how malocclusion affected their OHRQoL was limited (Elmahgoub and Abuaffan, 2015; Olkun and Sayar, 2019; Singh et al.
2019; Paes-da-Silva et al., 2020; Elyaskhil et al., 2021; Kolawole and Ayodele-Oja, 2021). The participants with grade 3 orthodontic treatment needs reported higher scores on the OHIP-14 scale than those with other grades. The OHIP-14 domains of psychological disability and psychological discomfort were found to significantly affect OHRQoL amongst the grade 3 participants. This observation is consistent with the findings of other studies (Elmahgoub and Abuaffan, 2015; Olkun and Sayar, 2019; Baidas et al., 2020; Elyaskhil et al., 2021).
Moreover, the grade 3 participants had significantly higher psychological discomfort scores than the grade 4 participants. Furthermore, their reported psychological disability scores were significantly higher than those of the grade 4 participants, which seems unreasonable from a clinical perspective. This could be due to the higher percentage of women in the grade 3 group.
According to previous research, women are more self-conscious about their dental appearance than men (Elmahgoub and Abuaffan, 2015; Olkun and Sayar, 2019). Surprisingly, the social disability scores of the grade 3 group were higher than those of the grade 4 group, with a weak but significant difference. This result contradicts previous studies (Hassan and Amin, 2010; Hassan et al., 2014). Overall, this study found that the patients’ perceptions of malocclusion strongly impacted their OHRQoL regardless of their malocclusion severity, which varied from person to person.
The current study found no correlation between orthodontic treatment need and OHRQoL, implying that increased malocclusion severity had no impact on OHRQoL. These findings are in line with previous studies (Elmahgoub and Abuaffan, 2015; Kolawole and Ayodele-Oja, 2021). However, these findings contrast with those of other studies that associated malocclusion severity with a great impact on OHRQoL (Onyeaso, 2009; Hassan and Amin, 2010; Hassan et al., 2014; Demirovic et al., 2019; Olkun and Sayar, 2019; Paes-da-Silva et al., 2020; Elyaskhil et al., 2021). Hence, this study’s findings could be attributed to an IOTN-related shortcoming. The displacement rank may have exaggerated the DHC scale, resulting in high scores for normal occlusion.
Furthermore, the sample, which included different IOTN-DC grades, was randomly collected from patients seeking orthodontic treatment at specific intervals, and this may have influenced the results. Although, the result of this study showed no association between orthodontic treatment need and oral heath related quality of life. It was observed that the standard deviations of all question domains were large when the OHIP-14 scores were assessed with IOTN-DC, gender, and age, suggesting that malocclusion alone did not determine OHRQoL and that other factors may have contributed (Elmahgoub and Abuaffan, 2015; Demirovic et al., 2019; Paes-da-Silva et al., 2020; Kolawole and Ayodele-Oja, 2021).
Most participants in this study were female, which could be because most patients seeking orthodontic treatment are female. In the present study, female participants reported that malocclusion more significantly impacted their quality of life than male participants, which is in agreement with other studies (Elmahgoub and Abuaffan, 2015; Olkun and Sayar, 2019). The regression analysis indicated that gender impacted OHRQoL and female participants reported negative OHRQoL scores. Moreover, aging seemed to decrease quality of life in all aspects. The age groups included in the present study (14–19 and 20–25 years old) who are less reliable in their perception of malocclusion than adults.
This could explain why this study found no significant difference between the age groups regarding their OHIP-14 scores. This finding contradicts previous studies that claimed age positively impacts OHRQoL (Hassan and Amin, 2010; Olkun and Sayar, 2019; Elyaskhil et al., 2021). Because this study’s sample was taken from a single clinical setting, the findings should be interpreted with caution relative to the total Saudi population. To confirm our findings, additional multi-centred studies with larger samples should be conducted.
CONCLUSION
This study found that malocclusion had no discernible detrimental effects on OHRQoL and its domains. Only the borderline treatment group reported that malocclusion had a significant negative impact on psychological discomfort and psychological disability. No variations in the influence of malocclusion on oral health quality were identified between the age groups. However, the female participants reported a significant detrimental impact of malocclusion on their oral health quality.
Source(s) of support: The authors received no support in the form of grants.
Conflicts of interest: The authors declare no conflicts of interest.
Author contribution details: All authors read and approved the final manuscript. The requirements for authorship have been met, and each author believes that the manuscript represents their honest work.
Ethical Clearance Statement: The Current Research Work Was Ethically Approved by the Institutional Review Board (IRB) of College of Dentistry, King Saud University Sauid Arab.
REFERENCES
Al-Jundi MA, Szentpétery A, John MT (2007). An Arabic version of the Oral Health Impact Profile: Translation and psychometric properties. Int Dent J, Vol 57 (2), pp. 84–92. doi: 10.1111/j.1875-595x.2007.tb00443.x
Andiappan M, Gao W, Bernabé E et al (2015). Malocclusion, orthodontic treatment, and the Oral Health Impact Profile (OHIP-14): Systematic review and meta-analysis. Angle Orthod, Vol 85 (3), pp. 493–500. doi: 10.2319/051414-348.1
Baidas LF, AlJunaydil N, Demyati M et al (2020). Fixed orthodontic appliance impact on oral health-related quality of life during initial stages of treatment. Niger J Clin Pract, Vol 23 (9), pp. 1207–1214. doi: 10.4103/njcp.njcp_681_19
Borzabadi-Farahani A, Borzabadi-Farahani A (2011). Agreement between the index of complexity, outcome, and need and the dental and aesthetic components of the index of orthodontic treatment need. Am J Orthod Dentofacial Orthop, Vol 140 (2), pp. 233–238. doi: 10.1016/j.ajodo.2010.09.028
De Oliveira CM, Sheiham A (2004). Orthodontic treatment and its impact on oral health-related quality of life in Brazilian adolescents. J Orthod, Vol 31 (1), pp. 20–27. doi: 10.1179/146531204225011364
DeGuzman L, Bahiraei D, Vig KW et al (1995). The validation of the Peer Assessment Rating index for malocclusion severity and treatment difficulty. Am J Orthod Dentofacial Orthop, Vol 107 (2), pp. 172–176. doi: 10.1016/s0889-5406(95)70133-8
Demirovic K, Habibovic J, Dzemidzic V et al (2019). Comparison of oral health-related quality of life in treated and non-treated orthodontic participants. Med Arch, Vol 73 (2), pp. 113–117. doi: 10.5455/medarh.2019.73.113-117
Dimberg L, Arnrup K, Bondemark L (2015). The impact of malocclusion on the quality of life amongst children and adolescents: A systematic review of quantitative studies. Eur J Orthod, Vol 37 (3), pp. 238–247. doi: 10.1093/ejo/cju046
Elmahgoub FA, Abuaffan AH (2015). Impact of malocclusion on quality of life in Sudanese dental students. Orthodontic Journal of Nepal, Vol 5 (1), pp. 12–17.
Elyaskhil M, Shafai NAA, Mokhtar N (2021). Effect of malocclusion severity on oral health related quality of life in Malay adolescents. Health Qual Life Outcomes, Vol 19 (1), pp. 71. doi: 10.1186/s12955-021-01710-2
Feu D, de Oliveira BH, de Oliveira Almeida MA et al (2010). Oral health-related quality of life and orthodontic treatment seeking. Am J Orthod Dentofacial Orthop, Vol 138 (2), pp. 152–159. doi: 10.1016/j.ajodo.2008.09.033
Guillemin F, Bombardier C, Beaton D (1993). Cross-cultural adaptation of health-related quality of life measures: Literature review and proposed guidelines. J Clin Epidemiol, Vol 46 (12), pp. 1417–1432. doi: 10.1016/0895-4356(93)90142-n
Hassan AH, Amin Hel-S (2010). Association of orthodontic treatment needs and oral health-related quality of life in young adults. Am J Orthod Dentofacial Orthop, Vol 137 (1), pp. 42–47. doi: 10.1016/j.ajodo.2008.02.024
Hassan AH, Hassan MH, Linjawi AI (2014). Association of orthodontic treatment needs and oral health-related quality of life in Saudi children seeking orthodontic treatment. Patient Prefer Adherence, Vol 8, pp. 1571–1579. doi: 10.2147/PPA.S71956
Kolawole KA, Ayodele-Oja MM (2021). Oral health-related quality of life of adolescents assessed with the Malocclusion Impact and Child Perceptions questionnaires. Am J Orthod Dentofacial Orthop, Vol 159 (2), pp.149–156. doi: 10.1016/j.ajodo.2020.09.017
Kragt L, Dhamo B, Wolvius EB, Ongkosuwito EM (2016). The impact of malocclusions on oral health-related quality of life in children-a systematic review and meta-analysis. Clin Oral Investig, Vol 20 (8), pp. 1881–1894. doi: 10.1007/s00784-015-1681-3
Mandall NA, Vine S, Hulland R et al (2006). The impact of fixed orthodontic appliances on daily life. Community Dent Health, Vol 23 (2), pp. 69–74.
Olkun HK, Sayar G (2019). Impact of orthodontic treatment complexity on oral health-related quality of life in Turkish participants: A prospective clinical study. Turk J Orthod, Vol 32 (3), pp. 125–131. doi: 10.5152/TurkJOrthod.2019.18042
Onyeaso CO (2009). Orthodontic treatment complexity and need with associated oral health-related quality of life in Nigerian adolescents. Oral Health Prev Dent, Vol 7 (3), pp. 235–241.
Paes-da-Silva S, Pitchika V, Baumert U et al (2020a). Oral health-related quality of life in orthodontics: A cross-sectional multicentre study on participants in orthodontic treatment. Eur J Orthod, Vol 42 (3), pp. 270–280. doi: 10.1093/ejo/cjz064
Shaw WC, Richmond S, Kenealy PM et al (2007). A 20-year cohort study of health gain from orthodontic treatment: Psychological outcome. Am J Orthod Dentofacial Orthop, Vol 132 (2), pp. 146–157. doi: 10.1016/j.ajodo.2007.04.009
Singh TK, Bhagia P, Gupta U et al (2019). Effect of orthodontic treatment needs on oral health related quality of life amongst the young population in Delhi NCR-region of North India. J Family Med Prim Care, Vol 8 (2), pp. 550–555. doi: 10.4103/jfmpc.jfmpc_431_18
Slade GD (1997). Derivation and validation of a short-form oral health impact profile. Community Dent Oral Epidemiol, Vol 25 (4), pp. 284–290. doi: 10.1111/j.1600-0528. 1997.tb00941.x
The World Oral Health Report (2003). Continuous improvement of oral health in the 21st century—the approach of the WHO Global Oral Health Program. Geneva, World Health Organization.
Tsakos G, Gherunpong S, Sheiham A (2006). Can oral health-related quality of life measures substitute for normative needs assessments in 11 to 12-year-old children? J Public Health Dent, Vol 66 (4), pp. 263–268. doi: 10.1111/j.1752-7325. 2006.tb04079.x


