King Saud Bin Abdulaziz University for Health Sciences, College of Nursing, Jeddah, Saudi Arabia
Article Publishing History
Received: 12/07/2020
Accepted After Revision: 14/09/2020
The present study aimed to identify the knowledge, social, physical and psychological effects of children with leukemia and its relationship to gender variables, age, length of treatment, and site of residence. Here comes the role of the psychological counselor to deal with this disease and how to control the situation and the situation in a way that enables the patient to overcome the disease and alleviate the problems that he suffers from. The present study aimed to identify the knowledge, social, physical and psychological effects of children with leukemia and its relationship to gender variables, age, length of treatment, and residence location. The researcher used the questionnaire as a tool to learn the effects. The present study will address this need by gathering insight into the experience, knowledge and perceptions of families having children diagnosed with cancer and received the radiation therapy and investigating the impact of an educational intervention in developing their knowledge and answering their quires about the safety of their children undergoing radiation therapy.
Also, the article investigates the impact of an educational program in developing parents’ knowledge and awareness regarding radiation therapy safety. It is concluded that there are many obstacles to assessing the needs of a caregiver or patient that may include: lack of clarity about best practices needed to identify needs; Identifying possible levels of performance in every need; Measuring the importance of needs; The correlation of needs assessment with satisfaction and quality of life, and the complex relationships between needs themselves; The extent of the use of needs assessment data when designing care programs; The efforts made to evaluate and follow up on improvement. The assessment directed to uncovering the needs of caregivers for cancer patients should focus on the following three dimensions: the experience of total sabotage in life, the extent to which the positive outlook remains, and the attempts made to keep alive. It is recommended that Further research is needed to evaluate outcomes and determine educational approaches that will produce positive changes in nurses’ attitudes toward, knowledge of, and application of complementary therapies.
Oncology, Radiation Therapy, Pediatric.
Saati H. S. Impact of an Educational Intervention in Developing Knowledge, and Awareness of Radiation Therapy Among Families Having Pediatric Oncology Patients. Biosc.Biotech.Res.Comm. 2020;13(3).
Saati H. S. Impact of an Educational Intervention in Developing Knowledge, and Awareness of Radiation Therapy Among Families Having Pediatric Oncology Patients. Biosc.Biotech.Res.Comm. 2020;13(3). Available from: https://bit.ly/3g2XJQm
Copyright © Saati This is an open access article distributed under the terms of the Creative Commons Attribution License (CC-BY) https://creativecommons.org/licenses/by/4.0/, which permits unrestricted use distribution and reproduction in any medium, provide the original author and source are credited.
INTRODUCTION
With the shift to health care and its partial transmission to the home, many cancer patients in various stages of the disease are accompanied by the complications of their needs, they receive care inside the home from (and thus), it is necessary to evaluate the needs of the people with the same family of children with the same family.The medical team and social and psychological care professionals know the needs of the caregivers, how important those needs are, how satisfied they are with the satisfaction of those needs they perceive and feel in order to achieve a complete healing process for the patient and to prevent difficulties that he may be exposed to
The family system and its members. The current study seeks to reveal the needs of caregivers for children with cancer patients and to identify the importance of those needs and the extent to which these needs are met and satisfied and satisfied with that from their point of view.By comparison with adult cancer, pediatric cancer is relatively rare as a disease. Nevertheless, around 100,000 cancer-related deaths in children are reported each year, most of them in developing countries (Al Mutlaq et al., 2015).
In Saudi Arabia, cancer is a significant factor contributing to mortality and morbidity in children, and, as such, represents an important public health issue. A retrospective study using data from the Saudi Cancer Registry collected between 1999 and 2008 found that 8% of all cancer cases developed in children, and their incidence rose over the time period investigated. The most common tumor types were leukemia (34.1%), lymphoma (15.2%), brain (12.4%) and kidney malignancies (5.3%). Notably, the group of very young children and infants (from birth to age 4) were those with the highest incidence of cancers (Al Mutlaq et al., 2015). By focusing high-energy radiation from X or gamma rays, or released by fast-moving protons, radiation therapy acts to damage cellular DNA, thus destroying the cancerous cells (Kidshealth, 2016).
The beam also includes a healthy area surrounding the tumor, to reduce the likelihood of recurrence due to migration of cancerous cells into the adjacent tissues. Therefore, normal cells can also be affected by the radiation process, even though they have better repair mechanisms. To offer patients the highest chance of curing or shrinking malignancies while minimizing side effects, a high dose of radiation therapy is aimed at the tumor, with a minimal dose delivered to the surrounding, healthy cells. In children, the healthcare team needs to carefully monitor the doses administered in order to protect the non-malignant tissues. Radiation oncologists may prescribe different types of radiation therapy, depending on the tumor type, size and stage; location in the body; the patient’s overall health, medical history and comorbidities; and, not in the least, the patient’s age (Lawrence et al., 2008). In children, radiation therapy is used in a range of tumors, including brain, Wilms tumor, and head and neck cancers (Kidshealth, 2016).
In addition, the management plan is personalized to address the child’s disease characteristics and treatment needs; for example, radiation may be offered as standalone treatment, adjuvant to surgery, or in combination with chemotherapy. Radiotherapy, or the combination of radiation and chemotherapy, may show increased effectiveness in some cancer types, albeit at the risk of increased side effects (Lawrence et al., 2008).
Most children receive external radiation therapy, which uses high-power equipment focusing on the affected area. In this case, the radiation dose is split over a number of sessions called fractions, allowing the recovery of healthy tissues between fractions. Pediatric patients with cancers of the head and neck, thyroid, uterus or testes may be prescribed internal radiation therapy (brachytherapy), where a radioactive substance is implanted at the site of the tumor, or in some cases swallowed. As with most anti-cancer therapies, radiation therapy is often accompanied by side effects, some of them acute – developing during treatment, and subsiding soon thereafter – and others chronic – occurring months or even years after treatment has ended (Lawrence et al., 2008).
Acute side effects include site reactions such as skin irritation, or damage to the exposed tissues (salivary glands, hair loss, and lower abdomen problems). Prescribing a radioprotective medication may help ease these side effects, and clinical trials are underway to test such medications. Among chronic side effects, long-term damage to the targeted area can result in fibrosis, infertility, damage to bowels, and the emergence of a second tumor. In children who have received radiation therapy, the risk of a second cancer is higher than in adult patients; for instance, the risk of developing breast cancer was found elevated in girls who had received radiation therapy to the chest for Hodgkin lymphoma (Travis et al., 2008).
As part of the patient-centric approach to cancer management, the radiation oncologist will take into account a child’s genetic factors, family history, presence of comorbidities, and any health or lifestyle issues, before prescribing a course of treatment or establishing a dosing regimen, and will review the treatment plan based on careful monitoring of the child’s response to radiation therapy. Treatment personalization is a cornerstone of the patient-centered approach to care, and that is especially relevant to cancer, a multi-faceted disease that has a wide range of objective (external) and subjective (internal/psychological) implications.
Among pediatric patients, the caretaking aspect of cancer treatment has even higher priority than in the overall cancer patient population. This underlines the role of the oncology health team and of oncology nurses in particular, not only in delivering the clinical aspects of care, but also in handling the emotional implications of diagnosis and therapy (Skilbeck and Payne, 2003).Communication between patients/families and healthcare professionals has been identified as a key barrier to implementing a patient-centered approach in Saudi hospitals (Aljuaid et al., 2016, Hani Almalki, 2020).
In cases such as those of pediatric cancer, communication needs to be tailored to children’s level of understanding and coping mechanisms (Seth, 2010). Simple wording, imagery, and child-friendly materials that convey essential information about the disease, the aims of therapy, milestones of the treatment journey, and advice for children undergoing treatment, can go a long way in promoting a sense of control and clarity. For children’s parents, improving communication relies on full transparency around the diagnosis and available treatment options for those families that require it, and managing expectations regarding treatment response and side effects (Seth, 2010). In Saudi Arabia, patients’ preference for and access to full disclosure of the cancer diagnosis and disease information was demonstrated in a prospective survey of 332 Saudi cancer patients from King Fahd University Hospital (Al-Amri, 2010).
The oncology health team should also reach out to children’s patients or careers to gain a comprehensive understanding of the patient and formulate a treatment plan that addresses and accommodates their needs (Seth 2010). It has been established that poor communication between healthcare practitioners and patients leads to suboptimal patient outcomes and patient dissatisfaction with the healthcare system (Bonds et al., 2003). However, clinicians and nurses often lack the skills needed to communicate in distressing situations, as they fear their ability to manage the emotions expressed by patients may be limited in such scenarios. As a result, they may choose to prioritize practical care and information above emotional support (Tay et al., 2011).
Other communication issues stem from a paternalistic, medicalized outlook to healthcare, which was proposed to have a cultural component in an Indian study of pediatric cancer patients and families (Seth, 2010). In addition, organizational factors, culture, tradition and expectations, as well as nurses’ heavy workloads, can all contribute to a decreased efficiency of communication, as was shown in an Iranian survey (Fakhr-Movahedi et al., 2011, Hani Almalki, 2020).
Patients’ and families’ religious beliefs also shape the way they cope with the cancer diagnosis and their perception of self-efficacy in managing the often-strenuous treatment journey that accompanies it. In studies examining the role of religion in helping patients cope with major illnesses including cancer, subjects commonly indicated that religious beliefs and practices were powerful sources of comfort, hope and a sense of purpose (Koenig, 2002). A survey of 39 Muslim breast cancer survivors found that spirituality was women’s primary source of psychological support, although all participants were also actively engaged with their medical treatment (Harandy et al., 2010). Finally, the level of family support was shown to increase the likelihood of patients undergoing and adhering to their cancer treatment (Grunfeld et al., 2001; Osborne et al., 2005; Morimoto et al., 2010).
Significance of The Study: Although research has shown that when a child is diagnosed with cancer and treatment starts, the whole family is affected (Flury et al, 2012), Soanes et al, (2009). Parents describe their lived experience of going through the child’s cancer treatment as a daily struggle in which the family’s normal daily life is disrupted and they have to focus only on the ill child (Björk, Wiebe, and Hallström (2009). It is a taxing period, and the entire family needs support to ease their burdens and get through the crisis (Björk, Wiebe, and Hallström (2009). Olsen, and Harder (2009). Furthermore, in a study done Ångström-Brännström et al., (2015) asking parent about their suggestion to improve the radiation therapy for their children, they concluded that parents need for information from physicians and the staff at the radiotherapy unit.
They want to have repeated information about their child’s treatment, as questions arise during treatment and they want to understand what is happening especially when they are seeing the image from the radiation–how large a wound it produces and a little about what zone is irradiated, and so on.. Parents can re-explain information, encourage and support their children as they go through their daily treatment with radiotherapy (Delany, and Conwell (2012). Moreover, the parents’ own emotional distress can be relieved by being involved in providing this information to the child and by seeing their child relaxed and calm rather than scared and refusing radiotherapy procedures, (Shrimpton et al., 2012) and, Klosky et al., (2007).
Therefore, the current study will look at investigating the effect of an educational interventions in developing parents’ knowledge about radiation therapy since the importance of parental involvement before, during and after radiotherapy is highly recommended. It is aimed at investigating the impact of an educational program in developing parents’ knowledge and awareness regarding radiation therapy safety.
Patients with a family history of cancer had an increased level of agreement with their treating physicians on their treatment plans compared with patients without such a history. This increase in the level of agreement could be associated with a patient’s previous experience with the shock of a cancer diagnosis of a family member. A patient’s ability to absorb the emotional shock of a family member’s diagnosis might result in a better acceptance of the diagnosis in oneself. Therefore, collection and documentation of a patient’s family history can be used as a tool to estimate a patient’s understanding of the treatment plan. Patients with a family history of cancer are more likely to agree with their treating physicians, as suggested by (Hani Almalki, 2020).
Radiotherapy (RT) is the standard of care following breast-conserving operation in breast cancer patients. The neutrophil-to-lymphocyte ratio (NLR) reflects the systemic change caused as a result of the radiotherapy. We aimed to evaluate the association between RT and the change in NLR following the receipt of RT, and to investigate the prognostic impact. We retrospectively reviewed NLR values of breast cancer patients taken before the administration of the first and the last session of RT. The cut-off point for the NLR was determined using the Youden index and receiver operating characteristic (ROC) curve within the training set. Recurrence-free survival (RFS), distant metastasis free survival, and overall survival were the main outcomes (Chang Ik Yoon, 2020).
Research Hypothesis And Questions:
The current study was examined the effectiveness of an educational program targeting families having children treated with radiation therapy to support or reject these 4 hypotheses:
- Radiation safety educational program is effective to increase Parents’/families’ understanding and acceptance of their children’s cancer diagnosis and care plan, and level of support in implementing this plan, regarding radiation therapy
- This educational program will improve the families’ attitudes toward radiation therapy so, they can teach and predict the sequences and complication that may happen to their children.
- Radiation safety educational program is not effective to increase Parents’/families’ understanding and acceptance of their children’s cancer diagnosis and care plan, and level of support in implementing this plan, in particular with regard to radiation therapy.
- There is no association between families’ knowledge and attitudes toward Radiation therapy treatment and their sociodemographic characteristics.
METHODOLOGY
Study design: A Quasi-experimental, specifically “one group pre-post-test” design will be used in the current study to achieve its objectives.
Setting: study assessing the experience, knowledge and attitudes of having families’(parents) of pediatric oncology patients on key aspects of their cancer diagnosis and radiation treatment at three hospitals in Jeddah, Saudi Arabia.
Subjects: the study was enrolled 65 participants by using convenient sampling technique and they are literate.
Validity and Reliability
The instrument was translated into Arabic and back translated into English, verifying whether the translation covers all aspects of the original English version of the questionnaire or not. To ensure the face validity of the final translated Arabic version of the questionnaire it was evaluated by experts who were selected based on their qualifications and experience in nursing research and education. Then, the tool was piloted and tested by 10 participants to identify ambiguities, the time required and any difficulties that might be encountered by the participants in reading or understanding. The reliability of the questionnaires was calculated and Cronbach Alpha for knowledge and attitudes questionnaires were reported later
Data Management: The data were analyzed using the most resent version of SPSS. Data were reported using descriptive statistics in the form of frequencies, percentages, means and standard deviations. A paired t-test was used to analyze the total scores of the participants’ responses on the pre-test and the post-test. Contributors’ sociodemographic and knowledge differences were analyzed using Chi Square test (χ2). Pearson R was used to test the correlation between families’ knowledge and sociodemographic variables. The significance level is pre-set at p<0.05.
Program description and data collection procedure: When a child has been diagnosed with cancer and has to undergo radiotherapy, parents a devastating feeling of shock and chaos and have to come to terms with the fact of a life-threatening illness. Parents can experience overwhelming feelings like feeling sick and mentally exhausted, as well as uncertainty, distress and fear of the illness and the radiotherapy treatment: They feel that everything concerning the disease and treatment is happening so fast that they cannot absorb the information or understand what is happening. The importance of parental involvement before, during and after radiotherapy must not be underestimated. Parents can re-explain information, encourage and support their children as they go through their daily treatment with radiotherapy. The parents own emotional distress can be relieved by being involved in providing this information to the child and by seeing their child relaxed and calm rather than scared and refusing radiotherapy procedures.
The objectives of the educational program were
- Develop parent’ knowledge about meaning of radiation therapy
- Assist parents to recognize different types of radiation therapy (internal and external treatment)
- Develop parents’ awareness by the short term and long-term side effect and complication of radiation therapy.
- Teach parents’ the appropriate methods which can help them to teach and protect their kids from emotional exhaustion and how their children feel better during treatment as well when to call for medical help.
- Empower parents with the skills of communication, listening, and how to develop a strong relationship with their children to break silence of their fear and motivate them to talk about their fears, emotional pain and traumatic experiences.
Data Collection procedure: Pre-test administration
- A letter with all details of the educational program was explained for parents during their presence with their children to motivate them to participate in the study
- Ethical issues were raised by taking verbal and written consent for participation from every family after explaining the aim of the study and confirming confidentiality of their data.
- Participants were asked to fill the questionnaire at the beginning of the first day of data collection (i.e., before the theoretical session starts).
Program description: The Data were gathered after receiving the approval. The participants were requested to fill up the questionnaires pre, and post the educational program. The educational training program consisted of 2 days (6 consecutive sessions), each part involves 3 sessions and each session will be 45 minutes to 60 minutes.
First part: theoretical part about radiation therapy including definition, types of radiation therapy and difference between internal and external radiation treatment, how radiation is given and what happens during external and internal radiation therapy. Moreover, the parent was informed regarding the common and long-term side effects of radiation. Moreover, the importance of caring behavior for your child and how you can convey.
The second part: this part was demonstrated for the different ways of successful communications with our children to build a trust relationship that motivate them to accept learning by parents and they can inform regarding any emotions without fear. In addition to, the effective methods for parents to protect their children emotional exhaustion and depression.
Encouraging children to talk about their feeling and ask questions by using active listening b) Provide knowledge to their children and convey acceptance and caring behavior c)Teaching their children, by using simulation games, pictures or may be allowed to enter the room of treatment prior the session with help of medical and nursing staff.
Methods of instructions: Power point presentation, Simulation activities, Photos and audio-visual materials and videos and movies. As regard to the effectiveness of instructional methods that were used throughout the program, many studies suggested that audio-visual materials, video showing, role play and modeling are effective methods in teaching.
Post-test administration: Questionnaires were fulfilled again by the parents after implementing the educational program.
RESULTS AND DISCUSSION
Parents’ Background information: 65 parents attend the program. All parents were Saudi and all pediatric patients were Saudis. Table 1 shows the age group for the participating parents which is high between age 40-49 and decrease after that.
Table 1. Age group for the participating parents
| Age of the parents | % |
| 20-29 | 22% |
| 30-39 | 29% |
| 40-49 | 38% |
| 50-59 | 11% |
| Total | 100 |
Table 2 shows the parents educational level which is high at secondary education level. Also, as shown in Table 3 most of the participant were from Jeddah city.
Table 2. Parents educational level
| Parents educational level | % |
| Not educated | 9% |
| Primary | 13% |
| Secondary | 41% |
| Batcheler | 35% |
| Post graduate | 2% |
| Total | 100 |
Table 3. Parents’ Living in Jeddah/or outside Jeddah
| City | % |
| In Jeddah | 64 % |
| Outside Jeddah | 36% |
| Total | 100% |
Table 4 shows Parents Information about their child disease at time of discovering the dieses and initial diagnosis and the high level of shocking at first time hearing the diagnosis (97 %) and it shows the low percentages regarding their information about the dieses, the treatment plans, and sever lack of emotional support at the time of the diagnosis which reflects in their child coping with radiation therapy.
Table 4. Parents Information about their child disease at time of discovering the dieses and initial diagnosis
| Parents Information about the disease at time of discovering the dieses and initial diagnosis | % |
| The initial reaction was shocking at first time hearing the diagnosis | 97 % |
| Awareness regarding the child diagnosis at first time hearing the diagnosis | 28 % |
| Awareness regarding symptoms progression at first time hearing the diagnosis | 24 % |
| Awareness regarding particular tests for cancer at first time hearing the diagnosis | 21% |
| Feeling that there was sufficient information about the dieses available at the time of your diagnosis | 29 % |
| Feeling that there was sufficient information about the treatment plan at the time of your diagnosis | 26% |
| Received psychological counselling before radiation therapy | 20% |
| Feeling that there was emotional support provided by the health team at the beginning of radiation therapy | 27 % |
| Feeling that their child finds have helpful support in coping with radiation therapy | 31 % |
Figure 1: Parents Information about their child disease at time of discovering the dieses and initial diagnosis
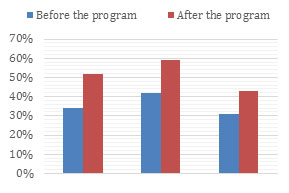
Table 5 compares between the parents Information about the diagnosis and treatment plan before and after the program and it shows improvements in parents information related to understanding regarding their child’s disease, treatment plan and coping with their child diagnosis
Table 5. parents Information about the diagnosis and treatment plan before and after the program
| Parents Information about the diagnosis and treatment plan | before the program | after the program |
| Parents understanding regarding their child’s disease | 34 % | 52% |
| Parents understanding regarding their child’s treatment plan | 42% | 59% |
| Parents coping with their child diagnosis | 31% | 43% |
Figure 2: Parents Information about the diagnosis and treatment plan before and after the program
Table 6. Parents Information about their child Experiences with radiation therapy
| Parents Information about their child Experiences with radiation therapy | % |
| parents Information about their child experience any side effects of radiation therapy | 96 % |
| parents Information about their child’s overall health | 89% |
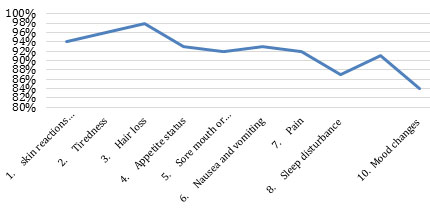
Table 7. Parents Information about their child’s common radiation therapy side effects
| Parents Information | % |
| skin reactions (irritation, redness, sensitivity) | 94% |
| Tiredness | 96 % |
| Hair loss | 98% |
| Appetite status | 93% |
| Sore mouth or tooth decay | 92 % |
| Nausea and vomiting | 93 % |
| Pain | 92 % |
| Sleep disturbance | 87% |
| Infections/fevers recurrence | 91% |
| Mood changes | 84 % |
Figure 3: Parents Information about their child’s common radiation therapy side effects
Table 8 compares between the Parents’ knowledge about their child Experiences with radiation therapy side effects before and after the program and it shows improvements in level of knowledge and comfortable to ask the medical team regarding their child health status.
Table 8. Parents’ knowledge about their child Experiences with radiation therapy side effects before and after the program
| Parents’ knowledge about their child Experiences with radiation therapy | before the program | after the program |
| knowledge toward information provided by (booklet, link to website, simulation session, video) | 38 % | 63 % |
| knowledge providing about lifestyle advice to help manage the side effects of radiation therapy | 35% | 51% |
| Parents knowledge if their child finds these advices were easy to understand | 31 % | 46% |
| Parents knowledge if their child finds these advices were easy to put into practice | 32% | 53% |
| Parents knowledge if their child experiences any learning difficulties or memory loss after radiation therapy | 43% | 55% |
| Parents feels comfortable asking for advice by the medical team | 48% | 59% |
| Parents knowledge regarding the importance of regular monitoring after stopping radiation therapy | 45% | 61% |
| Parents feels comfortable to discuss with medical team about treatments available after radiation therapy | 47% | 64 % |
Figure 4: Parents’ knowledge about their child Experiences with radiation therapy side effects before and after the program
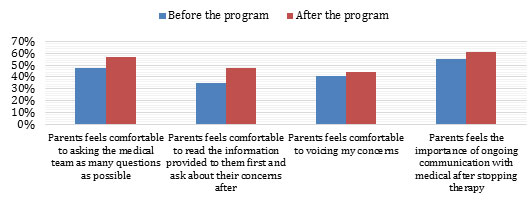
Table 9 compares between the Parents’ Parents Information about the communication with the medical team which was improved after the program.
Table 9. Parents comfortable about the communication with the medical team before and after the program
| Parents Information about the communication with the medical team | before the program | after the program |
| Parents feels comfortable to asking the medical team as many questions as possible | 48% | 57% |
| Parents feels comfortable to read the information provided to them first and ask about their concerns after | 35% | 48% |
| Parents feels comfortable to voicing my concerns | 41% | 44% |
| Parents feels the importance of ongoing communication with medical after stopping therapy | 55% | 61% |
Figure 5: Parents comfortable about the communication with the medical team before and after the program
CONCLUSION
The article examined the effectiveness of an educational program targeting families having children treated with radiation therapy to support or reject these hypotheses:
Radiation safety educational program is effective to increase Parents’/families’ understanding and acceptance of their children’s cancer diagnosis and care plan, and level of support in implementing this plan, in particular with regard to radiation therapy, This educational program improve the families’ attitudes toward radiation therapy so, they can teach and predict the sequences and complication that may happen to their children., Radiation safety educational program is not effective to increase Parents’/families’ understanding and acceptance of their children’s cancer diagnosis and care plan, and level of support in implementing this plan, in particular with regard to radiation therapy. There is no association between families’ knowledge and attitudes toward Radiation therapy treatment and their sociodemographic characteristics. Finally, the current study looks at investigating the effect of an educational interventions in developing parents’ knowledge about radiation therapy since the importance of parental involvement before, during and after radiotherapy is highly recommended.
REFERENCES
Al-Amri A. (2010). Saudi Cancer Patients’ Attitudes towards Disclosure of Cancer Information. Middle East Journal of Cancer, 1(4): pp. 175–180.
Aljuaid M, Mannan F, Chaudhry Z, Rawaf S, Majeed, A. (2016). Quality of care in university hospitals in Saudi Arabia: a systematic review. BMJ. 6: e008988. doi:10.1136/ bmjopen-2015-008988. Updated information found at: http://bmjopen.bmj.com/content/6/2/e008988.
Al-Mutlaq HM, Bawazir AA, Jradi H, Al-Dhalaan ZA, Al-Shehri A (2015). Patterns of childhood cancer incidence in Saudi Arabia (1999–2008). Asian Pac J Cancer Prev. 16(2): pp. 431–435.
Ångström-Brännström Ch., Engval G, Mullaney T., Nilsson K., Wickart-Johansson G., Svärd A., Nyholm T., Lindh J., and Lindh V., (2015); Children Undergoing Radiotherapy: Swedish Parents’ Experiences and Suggestions for Improvement 10(10): e0141086. Published online 2015 Oct 28. doi: 10.1371/journal.pone.0141086. PMCID: PMC4624794
Björk M, Wiebe T, Hallström I. An everyday struggle-Swedish families’ lived experiences during a child’s cancer treatment. J Pediatr Nurs. 2009;24(5):423–32. doi: 10.1016/j.pedn.2008.01.082 [PubMed]
Bonds DE, Zaccaro DJ, Karter AJ, Selby JV, Saad M, Goff DC, Jr. (2003). Ethnic and racial differences in diabetes care: The insulin resistance atherosclerosis study. Diabetes Care. 26: pp. 1040–1046.
Chang Ik Yoon et al. (2020), Radiotherapy-Induced High Neutrophil-To-Lymphocyte Ratio is A Negative Prognostic Factor in Patients with Breast Cancer,
Cancers 2020, 12(7), 1896; https://doi.org/10.3390/cancers12071896 (registering DOI)
Delany C, Conwell M. Ethics and teamwork for pediatric medical imaging procedures: insights from educational play therapy. Pediatr Radiol. 2012;42(2):139–46. doi: 10.1007/s00247-011-2271-4 [PubMed]
Fakhr-Movahedi A, Salsali M, Negharandeh R, Rahnavard Z. (2011). A qualitative content analysis of nurse-patient communication in Iranian nursing. Int Nurs Rev. 58: pp. 171–180.
Flury M, Caflisch U, Ullmann-Bremi A, Spichiger E. Experiences of parents with caring for their child after a cancer diagnosis. J Pediatr Oncol Nurs. 2011;28(3):143–53. doi: 10.1177/1043454210378015[PubMed]
Grunfeld EA, Ramirez AJ, Maher EJ, Peach D, Young T, Albery IP, Richards M. (2001). Chemotherapy for advanced breast cancer: what influences oncologists’ decision-making? Br J Cancer. 84(9): pp. 1172–1178.
Hani Almalki, MBBS; Ahmed Absi, MD; Abdulrahman Alghamdi, MBBS et al (2020) Analysis of Patient-Physician Concordance in The Understanding of Chemotherapy Treatment Plans Among Patients with Cancer, Jama Netw Open. 2020; 3(3): e200341. doi:10.1001/jamanetworkopen.2020.0341
Harandy TF, Ghofranipour F, Montazeri A, Anoosheh M, Bazargan M, Mohammadi E, Ahmadi F, Niknami S. (2010). Muslim Breast Cancer Survivor Spirituality: Coping Strategy or Health Seeking Behavior Hindrance? Health Care for Women International. 31(1): pp. 88–98.
Kidshealth: Radiation therapy (2016). The Nemours Foundation. Available at http://kidshealth.org/en/parents/radiation.html#. Last accessed June 2016.
Klosky JL, Garces-Webb DM, Buscemi J, Schum L, Tyc VL, Merchant TE. Examination of an interactive-educational intervention in improving parent and child distress outcomes associated with pediatric radiation therapy procedures. Children’s Healthcare. 2007;36(4):323–34.
Koenig HG. (2002). An 83-year-old woman with chronic illness and strong religious beliefs. JAMA. 288: pp. 48–493.
Lawrence TS, Ten Haken RK, Giaccia A. (2008). Principles of Radiation Oncology. In: DeVita VT Jr., Lawrence TS, Rosenberg SA, editors. Cancer: Principles and Practice of Oncology. 8th ed. Philadelphia: Lippincott Williams and Wilkins.
Morimoto L, Coalson J, Mowat F, O’Malley C. (2010). Factors affecting receipt of chemotherapy in women with breast cancer. International Journal of Women’s Health. 2: pp. 107–122.
Olsen PR, Harder I. Keeping their world together—meanings and actions created through network-focused nursing in teenager and young adult cancer care. Cancer Nurs. 2009;32(6):493–502. doi: 10.1097/NCC.0b013e3181b3857e [PubMed]
Seth T. (2010). Communication to pediatric cancer patients and their families: a cultural perspective. Indian J Palliat Care. 16(1): pp. 26–29.
Shrimpton BJ, Willis DJ, Tongs CD, Rolfo AG. Movie making as a cognitive distraction for pediatric patients receiving radiotherapy treatment: qualitative interview study. BMJ Open. 2013;3(1). doi: 10.1136/bmjopen-2012-001666 [PMC free article] [PubMed]
Skilbeck J, Payne S. (2003). Emotional support and the role of clinical nurse specialists in palliative care. J Adv Nurs. 43: pp. 521–530.
Soanes L, Hargrave D, Smith L, Gibson F. What are the experiences of the child with a brain tumour and their parents? Eur J Oncol Nurs. 2009; 13(4):255–61. doi: 10.1016/j.ejon.2009.03.009 [PubMed]
Tay LH, Hegney D, Ang E. (2011). Factors affecting effective communication between registered nurses and adult cancer patients in an inpatient setting: A systematic review. Int J Evid Based Health c. 9: pp. 151–164.
Travis LB, Hodgson D, Allan JM, Van Leeuwen FE. (2008). Second Cancers. In: DeVita VT Jr., Lawrence TS, Rosenberg SA, editors. Cancer: Principles and Practice of Oncology. 8th ed. Philadelphia: Lippincott Williams and Wilkins.