Department of Basic Medical Education, Qilu Medical University, Zibo, 255213, China.
Corresponding author email: wql_zcq@126.com
Article Publishing History
Received: 10/12/2020
Accepted After Revision: 23/02/2021
The traditional discipline-centered teaching mode is no longer adapt to the changes of current medical modes and the social demand for medical services owing to disjointed from clinical practice, knowledge separation and lack of connection between basic medical courses and clinical medical courses. Therefore, China has implemented the National Excellent Doctor Training plan and vigorously promoted the integrated reform of clinical medicine curriculum. In this study we compared the change of teaching effect between reform class and control class. We randomly selected 1 class from the 5-year clinical medicine major to carry out a series of pilot teaching reforms with curriculum integration, and at the same time, 1 class was selected for parallel control. Then the effect of the reform was evaluated from the aspects of test scores and 6-STATION OSCE. Student achievement and clinical skills are effectively improved through the integration of basic medical courses. The results showed that student achievement and clinical skills are effectively improved through the integration of basic medical courses It is concluded that we further need to integrate the various foundational and clinical disciplines into an organ-system based curriculum for the National Excellent Doctor Training plan.
Curriculum Integration, Basic Medical Curriculum, Medical Education, Discipline-Centered Teaching Mode
Wei L, Zhang L, Li C, Xu M, Li S, Wang Y, Fan R, Li M, Cheng H, Wang Q. Evaluation of Basic Medical Curriculum Integration Based on the Training of Chinese Excellent Category Doctors. Biosc.Biotech.Res.Comm. 2021;14(1).
Wei L, Zhang L, Li C, Xu M, Li S, Wang Y, Fan R, Li M, Cheng H, Wang Q. Evaluation of Basic Medical Curriculum Integration Based on the Training of Chinese Excellent Category Doctors. Biosc.Biotech.Res.Comm. 2021;14(1). Available from: <a href=”https://bit.ly/3vdTLwr“>https://bit.ly/3vdTLwr</a>
Copyright © This is an Open Access Article distributed under the Terms of the Creative Commons Attribution License (CC-BY). https://creativecommons.org/licenses/by/4.0/, which permits unrestricted use distribution and reproduction in any medium, provided the original author and sources are credited.
INTRODUCTION
Under Flexner’s influence, medical curricula around the world came to be structured into: Preclinical medicine learned in lecture theatres, laboratories, dissecting rooms, libraries and Clinical medicine learned in wards and operating theatres of teaching hospitals. Since the 1950s, medical colleges in Europe and The United States have proposed and implemented the teaching reform featuring the integration of medical curriculum. Curriculum integration involves the organization of teaching to interrelate or unify subjects frequently taught in separate academic courses or departments (Harden, et al. 1984, Scheffer, et al. 2012 Seethe and Khan 2019).
Most of the medical colleges in China are following the traditional system that is teacher centered, discipline based and opportunistic. With the development of global medical education and interdisciplinary integration, the model of Chinese medical education has also changed in the past decade. There were some defects in the traditional medical education pattern such as overlapping content of teaching, more time span, students learning burden, and comprehensive ability between various disciplines. Integration is an important means of dealing with overload of information, fragmented teaching of basic and clinical sciences, and the need for relevant and meaningful learning (Yamani and Rahimi 2016).
In this study, we have analyzed the problems in the process of integrated medical foundation course, and then really broke the barriers between disciplines, and integrated the systematic anatomy, histology and embryology, physiology, pathology, pathophysiology, pharmacology to “Two Introduction and Multiple Systems”. We put forward the training of clinical ability, which is helpful to realize the training of students’ clinical in the whole process of medical education. It is of great significance to realize the educational goal of “early clinical, multiple clinical and repeated clinical” and improve the training quality of medical talents.
MATERIAL AND METHODS
This study was granted an exemption by our Institutional Review Board since it evaluated outcomes of an existing mandatory component of the curriculum. We made an analysis the current research about the integration of basic medical courses based on published literature, and then carry out empirical research on medical colleges and universities that have integrated their courses, so as to provide scientific theoretical guidance and reference for the subject research.
Description of course integration: Six basic medical courses including systematic anatomy, histology and embryology, physiology, pathology, pathophysiology and pharmacology were selected as the subjects of course integration. The knowledge content of subject was decomposed into “knowledge points” to form “granulated resources”. Guided by the cultivation of clinical thinking ability, the “granulated resources” will be centered on “organ-system”, and the systematic teaching content will be reintegrated and reconstructed to form a modular curriculum system of “Two Introduction and Multiple Systems”.
Two Introduction is an introduction to human body form and function and the Multiple Systems are the respiratory system, circulatory system, digestive system, urinary system, blood system, nerve system, endocrine system, sensory system and reproductive system. According to the relevant requirements and procedures of the curriculum standards, the curriculum standards of the integrated curriculum were formulated. Then we organized the research team to compile “Introduction to human body morphology and mechanics” and 9 “organ-system” modules as case textbooks.
Teaching implementation of basic medical curriculum integration: In the five-year clinical medicine class of 2015, a 36-person pilot class for teaching reform was established based on the principle of mutual selection between the two sides, and other classes of the clinical medicine undergraduate course were taken as the control group.
The pilot class of educational reform was organized for teaching according to the integrated teaching contents of basic medical courses, while the control group was taught according to the current talent training program. The teaching reform pilot class was taught based on integration of “teaching of early clinical probation” and the integrated course of basic medicine to form the idea of early clinical probation.
The process of “setting questions, seeking answer and basic clinical combination” was designed and directly applied to teaching. The teaching mode combining case-based teaching and PBL teaching was adopted to carry out teaching based on suitable early internship cases and combined with PBL or CBL teaching. The goal of the implementation of special teaching was to cultivate students’ clinical thinking ability and improve students’ ability to solve practical problems. The teaching methods of the control group were carried out according to the discipline-centered methods.
Evaluation of teaching effect: The teaching reform pilot class adopts the method of formative evaluation, summative evaluation and comprehensive evaluation. In the teaching process, the formative evaluation was highlighted, and the existing problems in the learning process are fed back to the students in time. The formative evaluation runs through the whole teaching activity. After the teaching activity of each course is finished, the summative evaluation based on comprehensive and case questions was adopted.
After the learning of all the integrated courses of basic medicine, the comprehensive evaluation of learning effect was carried out by means of the basic stage assessment of simulated clinical practitioners. In addition to formative evaluation, summative evaluation and comprehensive evaluation were carried out in both the teaching reform class and the control class. The summative evaluation and assessment contents are generally consistent, but the teaching reform class was assessed according to the integrated curriculum, and the control class was assessed according to the unintegrated curriculum. Comprehensive evaluations were conducted in the same manner.
OSCE setting: A comprehensive 6-station OSCE was administered to the teaching reform and control class of five-year clinical medicine class of 2015. The examination was conducted after the clinical practice. The assessment of clinical skills includes the following aspects: Patient care skills, Interpersonal and communication skills, Professionalism skills, Practice-based learning and improvement skills, Systems-based practice skills and Medical knowledge skills; The OSCE consisted of 6 clinical problems; each clinical problem consists of six core competencies defined by the Accreditation council for Graduate Medical Education (ACGME) (Yang, et al. 2011).
Standardized patients should be used as a reference in the specific assessment. At each station, the summary scores were the sum of all the checklist items, and the six core competency sub scores were the sum of specific items for each competency. When presented, all scores were translated into 100 percentages. Please refer to the article of Yang et al. for more details (Yang, et al 2011).
Statistical analysis: All data were processed by SPSS 18.0 (SPSS Inc., Chicago, IL, USA). All data were presented as mean ± standard deviation. Comparison between groups was conducted using single-factor ANOVA followed by Tukey’s test. P<0.05 indicated significance, and P<0.01 indicated extreme significance.
RESULTS AND DISCUSSION
We have a teaching reform pilot class size of 36 students per year and control class size of 47 students. The students of teaching reform pilot class studied “Two Introduction and Multiple Systems” and the students of control class studied Six basic medical courses. Biochemistry and molecular biology as a comparative analysis course are taught in every class (see Table 1).
Table 1. Average score in teaching reform pilot class and control class
| Class | Students number | Course | Semester | Average score |
| Teaching reform pilot class | 36 | Introduction to Human Morphology | 1,2 | 71.3 |
| Introduction to human mechanics | 2 | 67.47 | ||
| Respiratory system | 3 | 77 | ||
| Digestive system | 3,4 | 81.72 | ||
| Circulatory system | 3 | 68.25 | ||
| Blood system | 4 | 76.72 | ||
| Urinary system | 4 | 79.94 | ||
| Sensory system | 4 | 79.83 | ||
| Nerve system | 5 | 73.19 | ||
| Endocrine system | 5 | 75.25 | ||
| Reproductive system | 5 | 77.11 | ||
| Biochemistry and molecular biology | 2 | 71.8 | ||
| Control Class | 47 | Systematic anatomy | 2 | 51.98 |
| Histology and embryology | 3 | 76.36 | ||
| Physiology | 3 | 73.09 | ||
| Pathology | 5 | 78.47 | ||
| Pathophysiology | 5 | 72.3 | ||
| Pharmacology | 5 | 77.55 | ||
| Biochemistry and molecular biology | 4 | 77.91 |
Average score (75.25) not including Biochemistry and molecular biology in teaching reform pilot class was higher than that (71.63) in control class. And however, Biochemistry and molecular biology was lower than that in control class. This results showed our teaching reform increased students’ score. Next, the score of teaching reform pilot class and control class was further analyzed based on Biochemistry and molecular biology as a comparative analysis course are taught by same teacher.
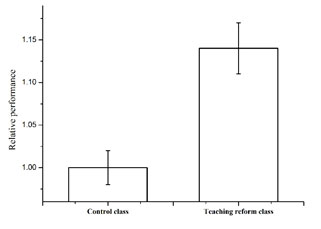
The calculating method is Relative performance= (Teaching reform subject Average score/ Biochemistry and molecular biology score) / (Traditional subject Average score/ Biochemistry and molecular biology score). The results from Figure 1 showed that relative performance in teaching reform pilot class was higher than that in control class.
Figure 1: relative performance in teaching reform pilot class and control class
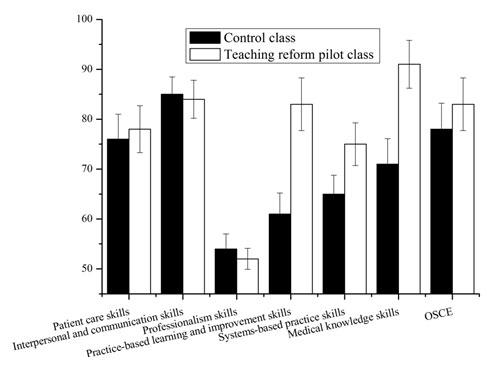
Analysis of OSCE: In Figure 2, a significant difference in the performance between different aspects of core competency (p < 0.05) was noted. Teaching reform pilot class had the higher pass rate in the aspect of Practice-based learning and improvement skills (83%), Systems-based practice skills (75%) and Medical knowledge skills (91%), whereas the lower pass rate was noted in the aspect of professionalism (52%). Interestingly, teaching reform pilot class had the higher pass rate in the OSCE than that of control class.
Figure 2: Overall pass rate (%) of each domain of ACGME competency and overall OSCE
In 1989, Shoemaker proposed a concept about integrated curriculum that is “Education that is organized in such a way that it cuts across subject matter lines, bringing together various aspects of the curriculum into meaningful association to focus upon broad areas of study (Betty 1989).” To this day, there is an ongoing discussion about whether medical curriculum should be discipline based or integrated.
Abraham Flexner thought that students should first learn basic and biomedical sciences and then move to clinical sciences; however, a common criticism of this approach was that students would not see the relevance of basic and biomedical sciences applied to clinical practice, and it was preferable to encourage students to think as doctors from the day they enter medical school (Harden 1986).
Integration of medical curriculum was importance for medical education because basic science learning was placed in the context of clinical and professional practice and was considered by students to be more meaningful and relevant (Quintero, et al. 2016). After a discussion of the health-illness concept, we constructed a theoretical basis of this process that changed our traditional discipline-based learning perspective. The meaning of the health-illness process changed was defined as a social, cultural, biological, and psychological process embedded and determined socially and culturally by group of human beings (Fanwei, et al. 2019).
As this approach implies that society and culture are no longer simply risk or etiological factors, our medical curriculum had to evolve into a new structure based on a “Two Introduction and Multiple Systems” concept of health and illness.In this study we randomly selected 1 class from the 5-year clinical medicine major to carry out a series of pilot teaching reforms with curriculum integration, and at the same time, 1 class was selected for parallel control. Then the effect of the reform was evaluated from the aspects of test scores and 6-STATION OSCE. The results showed that student achievement and clinical skills are effectively improved through the integration of basic medical courses.
CONCLUSION
The results demonstrated that student achievement and clinical skills are effectively improved through the integration of basic medical courses. We need further to integrate the various foundational and clinical disciplines into an organ-system based curriculum for a better National Excellent Doctor Training plan (China).
ACKNOWLEDGEMENTS
This work was supported by Research project on teaching reform of undergraduate colleges and universities in Shandong Province (Z2016M067, M2020103, M2018X0100).
Ethical Clearance Statement: The Current Research Work Was Ethically Approved by the Institutional Review Board (IRB) of Ethical Clearance Certificate No 201501005.
Conflict of Interest: None. All authors contributed equally to this work
REFERENCES
Anthroposophic Medicine (ICURAM). Patient Educ Couns.89(3): 447-454.
Betty S. (1989) Integrative Education: A Curriculum for the Twenty-First Century. OSSC Bulletin.33(n2.
Fanwei Q.U., Jin H.E., Hua M.A., Yanling J., Wenlan Z., et al. (2019) A Comparative Analysis of Medical Education Models and Curriculums of A Medical University and A Medical Education Center. JNMA J Nepal Med Assoc.57(215): 45-49.
Harden R.M., Sowden S., Dunn W.R. (1984) Educational strategies in curriculum development: the SPICES model. Med Educ.18(4): 284-297.
Harden R.M. (1986) Approaches to curriculum planning. Med Educ.20(5): 458-466.
Quintero G.A., Vergel J., Arredondo M., Ariza M.C., Gomez P., et al. (2016) Integrated Medical Curriculum: Advantages and Disadvantages. J Med Educ Curric Dev.3(
Sethi A. and Khan R.A. (2019) Curriculum integration: From Ladder to Ludo. Med Teach.1-3.
Scheffer C., Tauschel D., Neumann M., Lutz G., Cysarz D., et al. (2012) Integrative medical education: educational strategies and preliminary evaluation of the Integrated Curriculum for Medical Education. 65 No 3 670-678
Yamani N. and Rahimi M. (2016) The Core Curriculum and Integration in Medical Education.
Yang Y.Y., Lee F.Y., Hsu H.C., Huang C.C., Chen J.W., et al. (2011) A core competence-based objective structured clinical examination (OSCE) in evaluation of clinical performance of postgraduate year-1 (PGY(1)) residents. J Chin Med Assoc.74(5): 198-204.


