King Saud Bin Abdulaziz University for Health Sciences, College of Nursing, Jeddah, Saudi Arabia
Article Publishing History
Received: 05/07/2020
Accepted After Revision: 20/09/2020
A growing body of evidence suggests that burnout among oncology nurses is a significant result of the challenging and continuously high-stress work environment. It has been suggested that professionals could be emotionally affected by young age of children receiving chemotherapy, ethical decision making, observing the continuous suffering of children during or after chemotherapy. The main aim of this article is to examine the level of compassion fatigue, satisfaction and burnout experiences of oncology nurses when providing care to pediatric patients during chemotherapy. This article uses the qualitative descriptive (QD) research where it compares qualitative research with other types of qualitative methods. The article concluded that there is a severe shortage in Saudi nurses who works with pediatric oncology settings and highlights the importance to encourage Saudi nurses to work in specialized area with pediatric oncology.
The achieved numerical statistical results have proven that success rates in treating patients at risk are low by about 85% and patients with moderate-risk conditions are about 7%. For patients with high-risk cases, the survival rate for a 3-year-old is 66%, and a 5-year-old is 60%. From the perspective of future actions, it is recommended to conduct in-depth research in brain tumors, retinal tumors, and kidney tumors that include Wilma tumor, neuroma, muscle cancer, soft muscle tissue tumors, germ cell tumors, liver tumors, and bone tumors including bone cancer, cancer Ewing, tissue disorders, such as histiocytosis of Langerhans cells and other rare tumors. It is highly preferred that patients be referred to hospitals before undergoing any major surgery or treatment, in order to present a comprehensive treatment plan to patients and their families, which provides the best opportunity for treatment.
Oncology, Radiation Therapy, Pediatric, Burnout fatigue
Saati H. S. Compassion Fatigue, Satisfaction and Burnout Among Oncology Nurses Working in Pediatric Oncology Setting. Biosc.Biotech.Res.Comm. 2020;13(3).
Saati H. S. Compassion Fatigue, Satisfaction and Burnout Among Oncology Nurses Working in Pediatric Oncology Setting. Biosc.Biotech.Res.Comm. 2020;13(3). Available from: https://bit.ly/3hVUlYg
Copyright © Saati This is an open access article distributed under the terms of the Creative Commons Attribution License (CC-BY) https://creativecommons.org/licenses/by/4.0/, which permits unrestricted use distribution and reproduction in any medium, provide the original author and source are credited.
INTRODUCTION
Nurses work in shifts – usually 8 to 12 hours at a time and communicate with each other and exchange information to ensure that patient care is as smooth as possible when moving from one shift to another. They are usually responsible for caring for multiple patients during a single shift; For example, oncology nurses are responsible for caring for three patients at the same time. This applies most of the time to patients in the ICU due to their poor health and because they may be on special devices such as the ventilator, or receive medications that require constant monitoring and assessments. Also, the nurses lead the care process and take care of the daily needs of patients. Doubtless that caring for patients with cancer generates remarkable work-related stress that can result in nurses’ dissatisfaction and mental exhaustion, (Ferrans, 1990).
As compassion fatigue can influence patient satisfaction and safety, it is important for nurses to become knowledgeable about signs and symptoms of compassion fatigue as well as to be aware of strategies that can be utilized to develop a personal plan of care to avoid compassion fatigue. In the same vein,, a priority for healthcare systems is to provide healthy work environments for their staff and plan to address the needs of nurses who may be experiencing symptoms of compassion fatigue ( Potter et al 2010, Lombardo &Eyre 2011).
On the other hand, patient and careers’ satisfaction of care are crucial since high levels of satisfaction have been associated with higher quality of care and life (von Essen et al., 2002). Stamm (2010) defines professional quality of life as the quality one feels in relation to their work as a helper. Professional quality of life is the combination of both the positive quality (compassion satisfaction) and the negative quality (compassion fatigue). Additionally , In these clinical setting, nurses are expected to be proficient in the use of complex technologies and at the same time, engage in therapeutic communication with patients and families who have multiple needs that lead Pediatric oncology nurses to become overly involved with their patients and work to an extent of crossing professional boundaries (Zadeh, Gamba, Hudson & Wiener, 2012).
In pediatric oncology settings, studies of von Essen et al., (2001; 2002) suggest that competence of the nurses and other healthcare professionals were pointed out as integral aspects of good quality care. Patient satisfaction is also influenced by the relationship between nurses and other healthcare practitioners and patients (Campbell et al., 2000). In a recent study conducted by Wangmo et al. (2016) in Switzerland, several aspects of care were identified as important in increasing the levels of satisfaction of both patients and their careers or family members.
Results of this qualitative study suggest that helpful communication and responsiveness or friendliness of the oncology nurses and other members of the healthcare staff were crucial in helping patients and their parents feel satisfied with the care they receive. Further, participants stated that when healthcare professionals go beyond the duty of care, their level of satisfaction with the care they receive is further increased.
Elbarazi et al (2017) stated that Saudi Arabia is among those Arab countries which despite its higher-income, is classified as a developing country based on international indicators. Elbarazi et al (2017) have reported the presence of a wide range of prevalence of high emotional exhaustion, high depersonalization, and low personal accomplishment. They concluded that the prevalence of burnout may be higher among health care professionals in Arab countries as their health systems and financing models are either weak, overburdened, or rapidly developing and responding to the changing disease patterns and health status of the population.
Many of these countries have a critical shortage of health care professional, particularly in some specialties such as (oncology Pediatrics settings), which may lead to overloading them with work responsibilities and making them prone to burnout. Compassion fatigue is often linked with burnout. The two have been identified as related but separate concepts (Yoder, 2010). Beck (2011) defines burnout as a psychological syndrome of emotional exhaustion, depersonalization, and reduced personal accomplishment. Burnout develops gradually and has been identified as a subtle process during which a person is gradually caught in a state of mental fatigue and is drained of energy (Young, et al (2011); (Potter et al, 2010).
The second component of compassion fatigue, secondary traumatic stress, is a feeling of despair caused by the transfer of emotional distress from a victim to a caregiver that often develops suddenly. In the presence of secondary traumatic stress, the caregiver is empathizing with the victim (Jahrami et al (2013). Although the elements of compassion fatigue are related, secondary traumatic stress is an effect of experiences with specific types of patients, whereas burnout is an effect of environmental stressors and is not unique to health care providers. The effects can be profound and potentially impact both the staff’s personal quality of life as well as the work environment causing decreased productivity, a negative effect on the bottom line, difficulty recruiting, high turnover and increased sick days (White & Reg, 2006).
In the same vein, oncology nurses should provide support for patients and their parents in Pediatric oncology settings. Yoshida et al. (2014) observe that parents find it distressing to witness the suffering of their children, making decisions and preparations for palliative care and realizing that they could not do anything more for their children. The issue of emotional attachment has also been explored in the study of Dowling (2008), which suggests that nurse-patient relationship could help patients that they are better understood. However, the same relationship or intimacy might also impose emotional stress amongst nurses.
Hence, appropriate understanding of the nature of nurse-patient relationship and/or intimacy is needed in order to minimize its negative effects on the nurses or patients. Nurses caring for Pediatric oncology patients would also require support. It has been shown that nurses could feel isolation (Yoo et al., 2008). The ability of oncology nurses to explain technical terms in a simple manner was also singled out as important in increasing satisfaction (Wangmo et al., 2016).
The findings of Wangmo et al. (2016) are also similar to earlier studies (Von Essen et al., 2002; Campbell et al., 2000), which highlight how interpersonal factors are related to higher levels of satisfaction of care. A study that surveyed the level of satisfaction of young children or those who are 7–11 years old showed that caring healthcare providers, good communication and trustworthiness were also factors that influenced the level of satisfaction of the children (Pelander, Leino-Kilpi, & Katajisto, (2007). On the other hand, too little or too much information at the time of diagnosis when everything is difficult for members of the family and the patient to understand, could also lead to dissatisfaction (Clarke and Fletcher, 2003; Beck, 2014).
The most recent critical review of research evidence done by ( Kirshbaum, 2020) is that physical exercise and the treatment of underlying problems, such as anemia or clinical depression, are effective interventions. However, a wide range of practical interventions and complementary therapies are likely to be helpful such as: acupressure and acupuncture, stress management and relaxation, energy conservation measures, anticipatory guidance and preparatory information, and attention-restoring activities.
Significance of the present study: Working in the oncology, emergency and end of life settings can be full of stressful situations for patients, families and healthcare professionals. A growing body of evidence suggests that burnout among oncology nurses is a significant result of the challenging and continuously high-stress work environment. It has been suggested that professionals could be emotionally affected by young age of children receiving chemotherapy, ethical decision making, observing the continuous suffering of children during or after chemotherapy. Moreover, studies abroad have shown that a diagnosis of pediatric cancer causes emotional trauma and financial challenges to families and children. Additionally, Watt et al., (2013) have reported that the family-centred care model should be used when providing care in pediatric oncology settings.
Nurses who are involved in the care of pediatric patients with cancer also experience distress and in need of support in their role. However, there are still no studies conducted in Saudi Arabia and there is also a paucity of literature on the experiences of nurses of compassion fatigue, satisfaction, and burnout. Therefore, the researcher thinks about finding the prevalence of compassion satisfaction, compassion fatigue, and burnout among oncology nurses working in pediatric oncology setting since it affects the quality and safety of delivered care to patients and their families’ satisfaction levels.
Conceptual Framework: Maslow’s hierarchy of needs and Watson’s theory of human caring were applied to guide studies related to compassion Fatigue (CF), burnout, and compassion Satisfaction (CS) (Burtson & Stichler, 2010). A most significant theoretical model developed by Figley (2002) who discovered that CF develops as a result of a caregiver’s exposure to his or her patients’ experiences joined with his or her natural empathy. Later on, Stamm (2010) applied theoretical path analysis diagram, a conceptual framework related to CS, CF, and burnout among nurses was developed to guide this study.
In the current study, the researcher believes that it’s a cause and effect relationship between the individual and the organizational characteristics which may contribute to and have an influence on the development of CS, CF, and burnout. The demographic variables such as age, gender, level of education, years of experiences, hours of work per week, length of shift, are considered independent variables while the development of Compassionate fatigue and CF, and burnout will be the dependent variables in this study.
The main aim of this study was to examine the level of compassion fatigue, satisfaction and burnout experiences of oncology nurses when providing care to pediatric patients during chemotherapy. Specifically, this study aimed to address the following objectives: Describe the level of compassion fatigue and satisfaction of oncology nurses working with Pediatric patients. To Identify the manifestations of burnout experienced by nurse working in Pediatric oncology setting and assess the presence of secondary traumatic stress among nurses working in oncology Pediatrics settings. To explore the association between the nurses’ personal and demographic characteristics and the level of compassion fatigues, satisfaction and burnout. There are three types of BCI systems: invasive, semi-invasive, and non-invasive Gonfalonieri (2018).
METHODOLOGY
Design: across sectional survey was used to achieve the purpose of this study. Study subjects: All registered nurses (RNs) who worked in inpatient and outpatient’s clinic of oncology Pediatrics setting at three hospitals in Jeddah. The inclusion criteria for participation was (a) work at least 8 hr per week in the oncology Pediatrics setting, (b) interact directly with Pediatrics cancer patients and their families at least 8 hr per week, and (c) have at least 1 year of experience in the Pediatric oncology setting. This inclusion criteria was applied to make sure that the recruited nurses were spent enough to traumatic events that contribute to the development of CF and burnout. Minimum of 150 nurses were expected to participate by using a convenient sampling technique.
Data Collection Tools: The tool of the current study consisted of 2 parts as following: 1.A demographic questionnaire which was developed by the researcher and enquire about age, educational level, marital status, years in nursing profession, typical shift length, years of experiences in oncology setting. etc. 2.The Pro QOL scale, version 5, this scale used in this study based on many pervious researches who was used to examine the prevalence of CS, CF, and burnout among nurses Permission to use the Pro QOL instrument was granted via the website of the tool’s author. The Pro QOL tool was first developed in 1995 and has been used, revised, and updated over time. The scale is consisting of 30 items self-report survey that includes three subscales: CS, CF, and burnout (Figley & Stamm, 1996). Testing for convergent and discriminant validity have demonstrated that each scale measures different constructs (Stamm, 2010).
Each subscale is distinct, and the results of each subscale cannot be combined to give single significant score. The Pro QOL scale consists of 3 subscales (compassion satisfaction, burnout, and secondary traumatic stress) used to measure compassion satisfaction and compassion fatigue. Burnout and secondary traumatic stress are components of compassion fatigue, whereas compassion satisfaction is a stand-alone measure. Each subscale has 10 question items and uses a 5-point Likert scale scoring from 1 = never to 5 = very often (Stamm, 2010). The scores of the ProQOL for each subscale were totaled using Stamm’s validated levels: a CS score of 22 or less denotes low levels of CS, a score of 23–41 indicates average levels, and 42 and above suggests high levels of CS. For CF and burnout, a score of 22 or less indicates low levels, 23–41 indicates average levels, and a score of 42 and higher reveals high levels of CF.
Validity And Reliability: The Pro QOL scale was translated into Arabic and back translated into English, verifying whether the translation covers all aspects of the original English version of the questionnaire or not. To ensure the face validity of the final translated Arabic version of the questionnaire it was evaluated by experts who selected based on their qualifications and experience in nursing research and education. Then, the tool was piloted and tested by 10 participants to identify ambiguities, the time required and any difficulties that might be encountered by the participants in reading or understanding. The reliability of the questionnaires was calculated, and Cronbach Alpha for CF, CS and burnout questionnaires will be reported later.
Data Collection and Management: The data were collected primarily through questionnaires specifically developed to address the research objectives. A formal invitation letter was sent through mail or direct contact to qualify registered nurses. The mail contained detailed study information, objectives, data collection process, why they are chosen as participants, the significance of the information sought, and the confidentiality of their information. Once they agreed to participate in the study, a written informed consent was obtained, and participant was assigned an identification code. The scale along with demographic personal data sheet were distributed to the participants and enough time was given to fill the questionnaire since they were busy and overloaded by their work. Data collection for this study were run for a period of maximum 2 -4 weeks. When the subjects returned the questionnaires, the researcher was reviewing its veracity and completeness. In cases of incomplete or incorrectly filled questionnaires, the researcher was had the option to call the participant for clarifications or consider as missed data.
Data were analyzed by using the Statistical Package for the Social Science (SPSS) for Windows, version 22.0 (SPSS Inc.). Item means, standard deviations, medians, and percentages of the descriptive statistics was computed for the level of CS, CF, and burnout. A series of Pearson r correlation, t test, and one-way analysis of variance (ANOVA) used to examine the associations between demographics, work-related characteristics, and the level of CS, CF, and burnout. The statistically significant level calculated at .05. Multiple regression employed to determine which variables of demographics and work-related characteristics contributed to the variation of the level of CS, CF, and burnout among subjects. Using seven selected independent variables to run a multiple regression, this study needs a minimum sample size of 153 subjects to achieve 95% power and a medium effect size (.15) at α = .05.
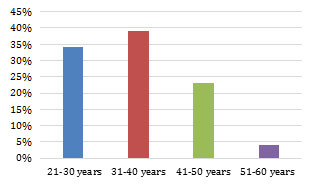
Demographic and personal information: Table 1 shows that the higher percentages of pediatric oncology nurses age group were found with the young ages and the percentage decreases when the age increase.
Table 1. Age group for the participating parents
| Age of the parents | % |
| 21-30 years | 34 % |
| 31-40 years | 39 % |
| 41-50 years | 23 % |
| 51-60 years | 4% |
Figure 1: Age group for the participating parents
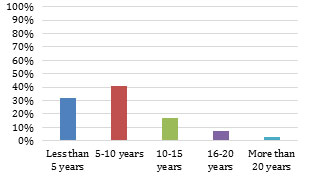
Table 2 Shows the experiences years of nurses who work in pediatric oncology which decreases to 3 % when it is more than 20 years.
Table 2. Years of pediatric oncology nursing experiences
| pediatric oncology nursing experiences | % |
| Less than 5 years | 32 % |
| 5-10 years | 41% |
| 10-15 years | 17% |
| 16-20 years | 7% |
| More than 20 years | 3 % |
| Total | 100 % |
Figure 2: Years of pediatric oncology nursing experiences
Table 3 shows that there was a severe shortage in Saudi nurses who work with pediatric oncology settings and highlights the importance to encourage Saudi nurses to work in specialized area with pediatric oncology.
Table 3. Nationality
| Nationality | % |
| Saudi | 9 % |
| None Saudi | 91 % |
| Total | 100% |
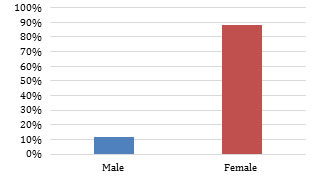
Table 4 shows there is low number of male nurses who works with pediatric oncology settings.
Table 4. Gender
| Gender | % |
| Male | 12 % |
| Female | 88 % |
| Total | 100 % |
Figure 4: Gender
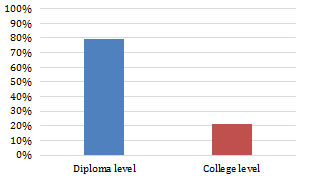
Table 5 shows that most the oncology nurses who works with pediatric settings have diploma level of education.
Table 5. Edcuation
| Level of education | % |
| Diploma level | 79 % |
| College level | 21 % |
| Total | 100% |
Figure 5: Education
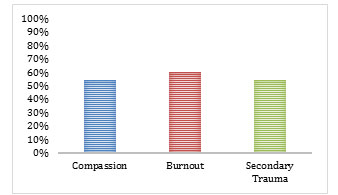
Table 6 shows the Professional quality of life scale (PROQOL) which shows average Level of Compassion (54 %), High Level of Burnout (60 %) and Average Level of Secondary Trauma (54 %).
Table 6. Professional quality of life scale (PROQOL)
| Level | Score |
| Lower than average | 43 or less |
| Average | Around 50 |
| High | 57 or more |
Figure 6: Professional quality of life
Table 7. Professional quality of life
| Professional quality of life | Level | % |
| Compassion Satisfaction status | Average Level of Compassion | 54 % |
| Burnout status | High Level of Burnout | 60 % |
| Secondary Trauma status | Average Level of Secondary Trauma | 54% |
Figure 7: Professional quality of life
RESULTS AND DISCUSSION
group were found with the young ages and the percentage decrease when the age increase, this is due that most of young ages are newly graduate and newly work with pediatric oncology and didn’t experience Burnout or Secondary Trauma while the lower number of old ages present the nurses who manages to cope with the nature in working with pediatric oncology settings. It also reflects on the experiences years of nurses who work in pediatric oncology which decreases to 3 % when it is more than 20 years. There is a severe shortage in Saudi nurses who works with pediatric oncology settings and highlights the importance to encourage Saudi nurses to work in specialized area with pediatric oncology
There is low number of male nurses who works with pediatric oncology settings, this require encouraging male in Saudi Arabia to join nursing as a profession in Saudi Arabia and encourage to work in specialized area like pediatric oncology stings. Most the oncology nurses who works with pediatric settings have diploma level of education, which indicate the sever need to provided programs for bachelor’s degree in nursing for female and male nurses in Saudi Arabia. The Professional quality of life scale (PROQOL) which shows average Level of Compassion (54 %) which indicate the most of the nurses in the sample were showing satisfaction with their profession, High Level of Burnout (60 %) which was noted due to their work with pediatric oncology patient, Average Level of Secondary Trauma (54 %) which indicated the risk to develop Secondary Trauma due to their work with pediatric oncology patients and to deal with these patients for long time.
We reached to the main finding that assure to reduce fatigue severity and distress and its impact on functioning, intensified collaborations and close partnerships between clinicians and researchers are needed, with an emphasis on system‐wide efforts to disseminate and implement these evidence‐based recommendations. The scale of fatigue in children with cancer is a reliable and valid instrument to measure the level of fatigue. The scales are brief, reliable, and feasible to assess multi-dimensional aspects of fatigue among such children. The instrument helps health professionals to monitor fatigue in children with cancer, (Mahdizadeh et al, 2020).
CONCLUSION
Nurses who are involved in the care of Pediatric patients with cancer also experience distress and in need of support in their role. However, there are still no studies conducted in Saudi Arabia and there is also a paucity of literature on the experiences of nurses of compassion fatigue, satisfaction and burnout. Therefore, the research thinks about finding the prevalence of compassion satisfaction, compassion fatigue, and burnout among oncology nurses working in Pediatrics oncology setting since it affects the quality and safety of delivered care to patients and their families’ satisfaction levels. This study clarifies the light on finding the level of compassion fatigue, satisfactions and burnout among nurses working at Pediatric oncology setting since these increased levels of burnout affect not only the quality of nursing interventions provided to the patients but also it has a greater impact on the oncology nurses’ stress-related symptoms, job dissatisfaction, decreased productivity, safety issues, and job turnover within the healthcare system.
REFERENCES
Beck J T., (2011) Secondary Traumatic Stress in Nurses: A Systematic Review; Archives of Psychiatric Nursing Volume 25, Issue 1, Pages 1-10 https://doi.org/10.1016/j.apnu.2010.05.005
Beck, J T. (2014) Improving pediatric hematology/oncology care in the emergency department’, Journal of Oncology Practice, 10(2), pp. 26-28.
Boyle, D.A. (2011). Countering compassion fatigue: A requisite nursing agenda. The Online Journal of Issues in Nursing, 16(1), Manuscript 2. doi: 10.3912/OJIN.Vol16No01Man02
Burtson, P. L., & Stichler, J. F. (2010). Nursing work environment and nurse caring: relationship among motivational factors. Journal of Advanced Nursing, 66, 1819–1831.
Campbell, S., Roland, M. & Buetow, S. (2000) Defining quality of care, Social Science & Medicine, 51(11), pp. 1611-1625.
Clarke, H. & Fletcher, P. (2003) Communication issues faced by parents who have a child diagnosed with cancer’, Journal of Pediatric Oncology Nursing, 20(4), pp. 175-191.
Day, J.R. & Anderson, R. A. (2011). Compassion Fatigue: An application of the concept to informal caregivers of family members with dementia. Retrieved from http://ncbi.nih.gov/pmc/articles on 1/31/12. doi: 10.1155/2011/408024
Dowling, M. (2008) The meaning of nurse- patient intimacy in oncology care settings: From the nurse and patient perspective, European Journal of Oncology Nursing, 12, pp. 319-328.
Ekedahl, M. & Wengström, Y. (2007) Nurses in cancer care- stress when encountering existential issues’, European Journal of Oncology Nursing, 11(3), pp. 228-237.
Elbarazi, T. L, S. Yousef and A. Elias (2017) Prevalence of and factors associated with burnout among health care professionals in Arab countries: a systematic review. BMC Health Services Research BMC series –open, inclusive and trusted 201717:491 https://doi.org/10.1186/s12913-017-2319-8
Ferrans, C. (1990). Quality of life: Conceptual issues. Seminars in Oncology Nursing, 6, 248. doi: 10.1016/0749-2081(90)90026-2
Figley, C. R. (2002). Compassion fatigue: Psychotherapists chronic lack of self-care. Journal of Clinical Psychology, 58(11), 1433–1441.
Gentry, J.E., & Baranowsky, A. (1998). Treatment manual for the Accelerated Recovery Program: Set II. Toronto, Ontario, Canada: Psych Inc.
.Jahrami HA, Thomas Z, Saif F, et al. (2013) The relationship between burnout and job satisfaction among mental health workers in the psychiatric hospital. Bahrain. Arab J Psychiatry. 24(1):69–76.
Joinson, C. (1992). Coping with compassion fatigue. Nursing, 22, 116–120.Journal of Issues in Nursing. 16(1). Retrieved from http://web.ebscohost.com on
Lombardo, B., & Eyre, C. (2011). Compassion fatigue: A nurse’s primer. Online
Journal of Issues in Nursing. 16(1). Retrieved from http://web.ebscohost.com on 1/31/12.
Kirshbaum M (2020) Cancer-related fatigue: a review of nursing interventions, Br J Community Nurs, 2010 May;15(5):214-6, 218-9 DOI: 10.12968/bjcn.2010.15.5.47945
Medical News Today (2010). Nurses bear cost of caring most heavily-compassion Nursing Quarterly. 34(3), 227-234.
Mahdizadeh F, Afsoon Hassani Mehraban, Mohammad Faranoush, Malek Amini, and Maryam Mehdizadeh (2020) Fatigue In Children With Cancer: Reliability And Validity Of The Persian Version Of Child, Parent, And Staff Fatigue Scale Asia Pac J Oncol Nurs. 2020 Apr-Jun; 7(2): 174–179.
Pelander, T., Leino-Kilpi, H. & Katajisto, J. (2007) Quality of pedaitric nursing care in Finland: Children’s perspectives, Journal of Nursing Care Quality, 22(2), pp. 185-194.
Potter, P., Deshields, T., Berger, J., Clarke, M., Olsen, S., & Chen, L. (2013). Evaluation of a compassion fatigue resiliency program on oncology nurses. Clinical Journal of Oncology Nursing, 40(2), 180-7. doi: 10.1188/13.ONF.180-187
Potter, P, Deshields, T., Divanbeigi, J. Berger, J., Cipriano, D., Norris, L. & Olsen, S. (2010). Compassion fatigue and burnout: Prevalence among oncology nurses. Clinical Journal of Oncology Nursing, 14 (5), E56-E62. doi: 10.1188/10.CJON.E56-E62
Slatten LA, Carson KD, Carson PP. (2011) Compassion fatigue and burnout: what managers should know. Health Care Manag (Frederick). 1;30(4):325–
Stamm BH. (2015) The Concise ProQOL Manual. 2nd ed. Pocatello, ID: ProQOL. org; 2010. http://www.proqol.org/uploads/ProQOL_Concise_2ndEd_12-2010.pdf. Accessed April 25, 2015.
Stamm BH. (2002) Measuring compassion satisfaction as well as fatigue: development and history of the compassion fatigue test. In: Figley CR, ed. Treating Compassion Fatigue. New York, NY: Brunner-Routledge; 107–122. Psychological Stress Series.
Stamm, B. H. (2010). The concise ProQOL manual (2nd ed.). Pocatello, ID. Retrieved from http://www.proqol.org/ uploads/ProQOL Concise 2ndEd 12-2010.pdf
Von Essen, L., Enskär, K. & Skolin, I. (2001) Important aspects of care and assistance for parents of children, -18 years of age, on or off treatment for cancer. Parent and nurse perceptions, European Journal of Oncology Nursing, 5(4), pp. 254-264.
Von Essen, L., Enskär, K., Haglund, K., Hedström, M. & Skolin, I. (2002) Important aspects of care and assistance for children 0-7 years of age being treated for cancer, Support care Cancer, 10(8), pp. 601-612.
Wangmo, T., Ruhe, K., Badarau, D., Kühne, T., Niggli, F. & Elger, B. (2016) Parents’ and patients experiences with Pediatric oncology care in Switzerland- satisfaction and some hurdles’, Swiss Medical Weekly, 146 (14309), pp. 1-8 [Online]. Available at: http://www.smw.ch/content/smw-2016-14309/#REF16 (Accessed: 25 June, 2016).
Watt, L., Dix, D., Gulati, S., Sung, L., Klaassen, R., Shaw, N. & Klassen, A. (2013) Family-centred care: a qualitative study of Chinese and South Asian immigrant parents experiences of care in Pediatric oncology Child Care, Health and Oncology, 39(2), pp. 185-193.
White, D. & Reg, N. (2006). The hidden costs of caring: What managers need to know. The Health Care Manager. 25(4), 341-3437.
Yoder, E. A. (2010). Compassion fatigue in nurses. Applied Nursing Research. 23, 191-197.
Yoo, J., Lee, J. & Chang, S. (2008) Family experiences in end-of-life care: A literature review Asian Nurse Research (Korean Social Nursing Science), 2(4), pp. 223-234.
Yoshida, S., Amano, K., Ohta, H., Kusuki, S., Morita, T., Ogata, A. & Hirai, K. (2014) A comprehensive study of the distressing experiences and support needs of parents of children with intractable cancer, Japanese Journal of Clinical Oncology, 44(12), pp. 1181-1188.
Young, J.L., Derr, D.M., Cicchillo,V.J., & Bressler, S. (2011). Compassion satisfaction,
Zadeh, S., Gamba, N., Hudson, C., & Wiener, L. (2012). Taking care of care providers: i:10.1007/978-3-030-01087-4_14