Department of Restorative Dentistry, College of Dentistry King Saud University, Riyadh, Saudi Arabia
Corresponding author email: Zalhaf101@gmail.com
Article Publishing History
Received: 15/01/2020
Accepted After Revision: 10/03/2020
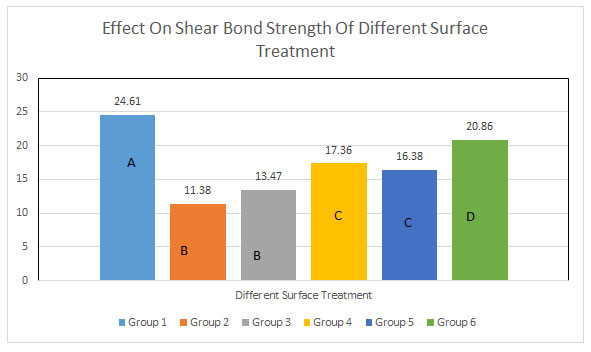
The current study was performed to analyse the shear bond strength of resin composite of bioactive restorative materials (Activa) using mechanical and chemical surface treatments. A total of 60 bioactive composite discs were prepared using a putty index mould and further divided into 6 groups (n= 10) each undergoing different surface treatment procedures. Study groups included, a control group (Group 1-no ageing, no surface treatments), Group 2- Aged non treated, Group 3- Acid etch/adhesive, Group 4- Acid etch-Silane/adhesive, Group 5- Grinding and Group 6 Grinding–Silane adhesive. All Activa discs were tested for shear bond strength using universal testing machine. Ten samples from each group were assessed for modes of failure. Data was assessed using analysis of variance and Tukey multiple comparisons test. In addition, among the mechanical and chemical surface treatment employed the highest mean value was of group 6 (20.86 (± 2.41) and least value of group 3 13.47 (±2.23). Among all groups the most common type of observed failure was adhesive followed by the admixed type. ANOVA displayed a significant difference between types of surface treatments on SBS of the repaired material (p<0.01) thus testifying the hypothesis. To increase surface energy for bonding of Bioactive (Activa) material, mechanical and chemical surface treatments are a prerequisite. A combination of mechanical grinding and silane adhesive (chemical) surface treatments produced desirable outcomes.
Bioactive material; Repair; Resin composite; Silane; Grinding; Adhesive Bond
Alsahhaf A. Bond Strength of Resin Composite of Bioactive Restorative Materials Using Different Surface Treatments. Biosc.Biotech.Res.Comm. 2020;13(1).
Alsahhaf A. Bond Strength of Resin Composite of Bioactive Restorative Materials Using Different Surface Treatments. Biosc.Biotech.Res.Comm. 2020;13(1). Available from: https://bit.ly/2TIHAFL
Copyright © Alsahhaf, This is an open access article distributed under the terms of the Creative Commons Attribution License (CC-BY) https://creativecommons.org/licenses/by/4.0/, which permits unrestricted use distribution and reproduction in any medium, provide the original author and source are credited.
INTRODUCTION
Restorative repair is one of the immense challenges faced by clinicians. Many clinicians believe that total replacement of the restoration is the best way for long term integrity of the filling. However, the risk of removing tooth structure along with defaulted restoration is a commonly associated problem with total replacement. In contrast, repairing a defaulted restoration is considered a more conservative approach, which increases the serviceability of the restoration. Adhesive dentistry has created the possibility to employ a conservative approach to save the tooth from the extensive widening of the tooth cavity. The tooth is repaired based on two important factors the cavity preparation size reduction and the materials bonding ability (resin-based composite) to tooth structure, (Fernández et al., 2015 Zhang et al., 2017).
Using resin composite is a challenge in this type of approach as it undergoes degradation over time. The salivary enzymes, pH and wet environment are the factors that are responsible for early degradation process (Fernández et al., 2015). Previously the reparation of the composite was difficult because aging causes degradation of the available unsaturated double bond (Bektas et al., 2012). In addition, water sorption, chemical degradation and constituent leaching out also influence the bonding between old and repair material (Neis et al., 2015, Bektas et al., 2012). Bioactive materials (Activa) are resin glass ionomer, which provides the advantage to chemically bond and create a seal against microleakage by releasing calcium, phosphate and fluoride (Garcia-Godoy and Morrow, 2015, Garcia-Godoy et al., 2014). Activa is one of the first ionic resin mixtures that bears a shock-absorbing resin component and bioactive fillers exhibiting similar chemical and physical properties as the teeth (Kaushik and Yadav, 2017, Amaireh et al., 2019).
In addition, it continuously recharges the environment with calcium, phosphate and fluoride,(Tezvergil et al., 2003). This makes the restoration durable and fracture resistant compared to the composites (Garcia-Godoy et al., 2014). Previous studies had observed the repair bond strength based on mechanical and chemical surface treatment on aged resin composite (Wendler et al., 2016, Palasuk et al., 2013). Authors claimed that increased surface roughness is an important factor for the bonding between old and new restoration (Kaushik and Yadav, 2017, Elsaka, 2016). The purpose of the surface treatment is to remove the surface layer contaminated by saliva and increase surface irregularities (Croll et al., 2015). This process exposes the high energy composite surface and increases the surface area (Wendler et al., 2016, Wiegand et al., 2012). However, there is no significant evidence to establish the relation of surface treatment and bonding strength between the composite restorations and Bioactive material (Activa). The present study aims to evaluate the shear bond strength in repaired restoration with the condition applied to different surface treatments. Therefore, the study aimed to investigate the shear bond strength of resin composite to bioactive restorative materials (Activa) using mechanical and chemical surface treatments.
MATERIALS AND METHODS
The present study conducted the shear bond strength test of resin composite of bioactive restorative material using different surface treatment after the approval from institutional research review board. A total of 60 bioactive composite discs were prepared using a putty index mould (Ø 6 mm, depth 3 mm). The materials used in this study and products details are presented in Table 1. For the preparation of the Bioactive disc (Activa) with dimension (5x3mm), the Activa material was condensed into layers in the putty index mold covered by a mylar strip. Each disc layer was light cured with a light intensity of 1100 mW/cm2, as measured by a digital radiometer (Marc Resin CalipratorTM, Blue Light Analytics Inc, Nova Scotia, Canada) for 20 secs at a distance of 1mm. A final curing was performed after removal from the mould.
The prepared disc were stored in the distilled water for 24h at 37°C. All the composite disc except 10 were subject to 100,000 thermocycles at 5 to 55 degree in the thermocycler (THE-1100, SD Mechatronik GmbH, Germany). Each cycle continues for 30 secs with 5 s interval between the baths. This process continues over a period of 7 days. Each specimen disc was embedded in an acrylic resin mould to create a base. Subsequently each disc was polished for 30 seconds to remove the flashes using a number 600 silicon carbide paper discs (CrbiMet® Abrasive Discs, BUEHLER, Lake Bluff, Illinois, USA) on a grinding machine (Automata, Jean Wirtz, Dusseldorf, Germany) driven at a speed of 300 rev/min under water spray followed by air drying.
Out of total 60 disc 10 water aged non thermocycled Activa disc were categorised as a control group for the evaluation of active shear bond strength in repaired material. The remaining disc were divided into 5 groups (n=10) to evaluate the effect of the different chemical and mechanical surface treatment procedures on the shear bond strength of repaired material. After the aging process, there were three major types of surface treatment performed on the aged composite disc: acid etching, grinding or combination of etching/grinding with silane adhesive. Each group was subjected to different treatment protocol. Group 2 consisted of thermocycled specimen disc without any surface treatment. In case of Group 3 and 5, the repair material was applied over a mechanical treated surface (etched with 37 % phosphoric and grinded with abrasive stone) in contrast to group 6 and 4 that were treated by the combination of mechanical and chemical surface treatment (silane adhesive).
Table 1: Study materials and composition
| Material | Product detail |
| Shade A3.5 resin composite | Filtek supreme- 3M |
| Silane coupling agent | 3M™ RelyX™ Ceramic Primer, 2721 |
| 37% phosphoric acid etch | Ivoclar Vivadent AG, FL-9494 Schaan/Liechtenstein |
| Primer-adhesive system | Adper™ Scotchbond™ Multi-Purpose Adhesive |
Preparation and surface treatment of the repaired disc
Group 3 and 4:The specimens were prepared with 400 – 600 grit carbide paper (Buehler) polish under a water coolant spray. Consequently, the surface is etched by 37 % phosphoric acid (Condac 37, FGM, Joinville, SC, Brazil) for 15 seconds, rinsed with water spray for 30 seconds and air dried for 10 seconds. The adhesive system in group 3 is the Scotchbond Multipurpose; however, in group 4 etching is accompanied by silane (relyx ceramic primer) and adhesive (single bond- all in one). The adhesive is applied with a micro brush and after 15 seconds it is air dried for 5 seconds and light cured for 10 seconds.
Group 5 and group 6: The specimen discs were grinded using the abrasive stone (016, Komet, CE 0197, Germany) rotated at 40,000 rpm for 5 secs, in one direction in group 5 whereas the specimen discs in group 6 were coated with silane and adhesive after grinding with abrasion stone. The detailed step by step surface treatment is explained in table 2.
Table 2: Materials and surface treatment details.
| Study Groups | Surface Treatments |
| Group 1-
Control group (non thermocycled) |
No ageing and No treatment was applied to the repair-surface |
| Group 2-
Aged non treated |
Only thermocycled and No treatment was applied to the repair-surface. |
| Group 3-
Acid etch/adhesive |
37% phosphoric acid etching was applied for 15 s, rinsed for 30 s and then air dried for 10 seconds. Subsequently, the adhesive was applied to the repaired surface of the disc for 10 s. After the application, it was air dried for 3 s to remove the excess solvent. |
| Group 4-
Acid etch-Silane/adhesive |
Acid etch was applied as described for group 3. Silane was applied for 1 min according to the manufacturer’s instruction, gently air dried followed by a thin layer of the adhesive (same procedure as mention in group 3). |
| Group 5-
Grinding |
The disc surface was gently grinded using abrasive stone (016, Komet, CE 0197, Germany) rotated at 40,000 rpm with Sirona T2 Revo-R 40 hand piece (Sirona Dental Systems GmbH, Bensheim-Germany), for 5 s in one direction. Each disc cross sectional area before and after grinding was measured using a digital calliper (Mitutoyo, Mitutoyo Corporation, Japan) for standardising the quantity of composite removed. After grinding, the disc was rinsed for 15 s and dried for 3 s. |
| Group 6-
Grinding–Silane adhesive |
Repaired surface was grinded as mentioned above followed by the application of silane adhesive (Similar procedure as described above). |
The Activa discs with an acrylic resin based material (aged and non-aged) were repaired with a resin composite material (3mm x4mm), shade A3.5 with or without any surface treatment. A putty index mould (Ø 3 mm, depth 4 mm) is placed on the top of the Activa disc to support the repair material. Excess cement was removed with the micro brush. Each side was cured for 20 seconds, with the total time for curing 40 seconds using LED light cure (Elipartm S10 LED Curing Light, 3M ESPE, MN, USA) operated with a light intensity of 1100 mW/cm2. The repair material is light cured for additional 20 seconds after the mould removal followed by half of the bonded specimens from each groups were tested after the 24-hour storage in distilled water at 37 °C, whereas the other half underwent thermocycling (5000 cycles, THE-1100, SD Mechatronik GmbH, Germany) in distilled water at 5 °C to 55 °C. Each cycle runs for 30 seconds with an interval of 5 seconds between the cycles.
Shear bond strength:The specimens were transferred onto the universal testing machine (Instron 5965, Instron Corporation, Norwood, MN, USA) to evaluate the shear bond strength. The specimen was positioned in a direction where the 5-kN load cell at 90 degrees applies shear force at a cross speed of 0.5 mm/min on the Activa interface until debonding occurs. Using a digital calliper each bonded Activa-RBC cross sectional area before and after the application of the load was measured in order to calculate shear bond strength in megapascal (MPa) as per respective load applied.
After the debonding, the surface was closely examined under a digital microscope (Hirox KH-8700, Europe) at 40X magnification for determination of the type of fracture at the interface. The fracture can be classified into three types mainly cohesive, adhesive and admixed. Any part of activa observed on the surface of composite resin indicates cohesive fracture whereas debonding at the interface reveals adhesive failure. Any residue of either material indicates the admixed type of fracture.
Statistical analysis:The data collected for the SBS was analysed using Statistical software for social sciences (SPSS 20.0 version), considering p <0.05 statistically significant. The normality of the data was assessed through Kolmogorov-Smirnov test. A brief comparison between the groups can be appreciated through the mean and standard deviation. To determine the significant difference in shear bond strength between different surface treatments group’s analysis of variance (ANOVA) and Tukey’s post hoc test were employed.
RESULTS AND DISCUSSION
Kolmogorov-Smirnov test displayed even distribution of the normality data. The Analysis of variance (ANOVA) displayed a significant difference between different types of surface treatments on SBS of the repaired material (p=0.01). Comparing the mean and standard deviation between the groups, it can be observed that group 1 (24.61 (± 2.18)) demonstrated high value of shear strength bond closely followed by group 6, group 4, group 5, group 3 and group 2 respectively (table 3). Furthermore, under the mechanical and chemical surface treatment employed the highest mean value was for group 6 [20.86 (± 2.41)] and least value for group 3 [13.47 (±2.23)].
Table 3: Means and SD for Shear bond strength values among study groups.
| Study Groups | SBS-Mean (SD) | ANOVA- p value | Tukey HSD |
| Group 1 | 24.61 (2.18) | p <0.01 | A |
| Group 2 | 11.38 (1.74) | B | |
| Group 3 | 13.47 (2.23) | B | |
| Group 4 | 17. 36 (2.45) | C | |
| Group 5 | 16.38 (2.73) | C | |
| Group 6 | 20.86 (2.41) | D |
Note: Tukey HSD. Different alphabets denote a significant difference in study
groups compared.
Figure 1: Comparison between different surface treatments
Note: Tukey HSD. Different alphabets denote a significant difference in a p-value of study groups compared.
Multiple comparison tests clearly displayed that each surface treatment had an effect on the shear bond strength that includes the thermocycling, etching, silane adhesive application, grinding and a combination of etching/ grinding and silane. Nevertheless, the comparable results were appreciated between two groups using different surface treatments such as the no treatment (group 2), and etching group (group 3) (p= 0.0552) and etching with silane (group 4), and grinding group (group 5) (p= 0.7612). The no-treatment group recorded the least mean value with a similar mean value of etched specimens signifying no evident effect of etching independently compared to no treatment. On the other hand, etching with silane adhesive also did not demonstrate a significant difference in mean value in comparison to grinding if used independently.
The digital microscope imaging revealed that the most common type of failure identified was an adhesive fracture, which clearly displayed the assessment of the shear bond strength. Only group 2 (no treatment) showed 100% adhesive failure indicating that surface treatment has a positive effect on the bond strength (table 4). Only 20% to 30% of the specimens demonstrated admixed fracture whereas only 1 or 2 specimens in groups 1, 4 and 6 exhibited cohesive failures.
Table 4: Failure mode among study groups
| Study Groups | Adhesive (%) | Cohesive (%) | Mixed (%) |
| Group 1 | 50 | 20 | 30 |
| Group 2 | 100 | 0 | 0 |
| Group 3 | 70 | 0 | 30 |
| Group 4 | 60 | 10 | 30 |
| Group 5 | 80 | 0 | 20 |
| Group 6 | 70 | 10 | 20 |
The present study aimed to observe the effects of mechanical and chemical surface treatment on the shear bond strength between composite and bioactive material. The results revealed that the major factors affecting the bond strength between old and new restoration include surface roughness, bonding material, repair material, ageing and oral conditions (Palasuk et al., 2013, Wiegand et al., 2012). Theoretically, the bond between each fresh layer depends upon the present oxygen inhibiting layer over unsaturated monomers,(Hamano et al., 2012, Cho et al., 2013). Therefore, it is necessary to perform the surface treatment to expose high energy surface as it is difficult for aged restoration to form bonds, (Carvalho et al., 2012). The study result displayed that there was a significant effect of the mechanical and chemical surface treatment on the bond of repaired material. A multiplicity of explanation can be viewed in the light of similar studies conducted related to application of different surface treatment employed.
The curing of the Activa disc was carried out using a polyester strip matrix thereafter to standardise each specimen according to the oral conditions, to form an oxygen inhibiting layer and a smooth finish (Elsaka, 2016). To further imitate the oral conditions and initiate the aging process (except for 10 specimens) the samples were placed in the distilled water and thermocycled respectively (Bektas et al., 2012, Özcan et al., 2013). The placement of composite in the water removes the free radicals, which can react with new repair material,(Arumugam et al., 2014). In addition, the non thermocycled specimens were used as a positive control against the other groups to display the profound effect of oral condition on the repaired restoration. The purpose was to compare an ideal situation to the real possibilities in an oral cavity in order to test the materials efficacy.The result displayed the superior efficiency of the bioactive material bonding with resin composite under ideal conditions. This can be easily appreciated by comparing group 1 (non thermocycled) with other groups displaying the highest mean value. Analysing the results, it can be observed that there was no significant difference between the only thermocycled and etched samples. Thermocycling ages the material by reducing the unsaturated bonds available for bonding; hence, it compromises the ability to chemically bond (Bektas et al., 2012).
Furthermore, the results revealed that etching with the phosphoric acid presented with the lowest mean value among surface treatments employed. Previous studies explained that the phenomena of etching creates entrance voids upto the fillers that come in contact with water (Takamizawa et al., 2015, Torres‐Gallegos et al., 2012). This deranges the silane layer and stabilises the filler matrix; hence, causing weakening of the bond strength (Rengo et al., 2012). Rengo et al., claimed that change in microstructure of the composite depends upon the variation in the intensity of etching (Rengo et al., 2012). However, an evident difference is observed in the application of silane and adhesive after etching. This indicates that applying silane adhesive creates a silane bridge (Si–O–Si) with the remaining filler particles of the composite and allows easy penetration of the adhesive into etched retentive cavities (Wiegand et al., 2012, Eslamian et al., 2012). Thus, this indicates the microstructure and composition of the composite play an important role in developing bond strength in a repaired material.
Divergent results were appreciated when grinding was used on the samples and compared with other surface treatment. Grinding with an abrasive stone (group 5) demonstrated comparable results to the etching and silane adhesive (group 4); however, when silane adhesive was applied after grinding a significant difference was appreciated. Authors had suggested that grinding the surface with the abrasive grit bur causes the removal of the fillers from the surface leading to voids formation (Özcan and Koc-Dundar, 2014). This reduces the amount of silica to react and form bonds. Therefore, adding the silane and adhesive after grinding causes an increase in the surface activation of bond formation (Lee et al., 2017, Dickens, 2015).
According to Lee et al, they failed to present improve bond strength following above-mentioned procedure (Lee et al., 2017). The authors stated the bond failure was appreciated due to the presence of smear debris (Lee et al., 2017). Whereas, the present study indicates silane and adhesive efficiently bonding with the repaired material. Therefore, it can be concluded that the difference in results might be due to different study materials and types of methodology testing. Hence, it can be appreciated that by comparing the two mechanical surface treatments grinding (singly used) showed better outcomes in contrast to etching and silane adhesive.
The author suggests that the ideal weight to test the shear bond strength is about 15 MPa to 25 MPa, typical resin- dentine bond strength values. In the present study, the samples were tested for shear bond strength under a load of 15 MPa. The adhesive failure was not completely 100% (except group 2) which demonstrated that mechanical and chemical surface treatment has a positive impact on the shear bond strength of the repaired material. Limited failure in the cohesive failure reflected the validity of the test based on bond strength in contrast to material strength (Hickel et al., 2013). Therefore, it can be apposite that surface treatment has an evident effect on the bonding strength of the repaired material.
Analysing the limitation of the study, multitude of barriers can be viewed. The present study was able to efficiently evaluate the shear bond strength of the repaired material; however, the repaired bond strength was not compared with the previous strength of the material. In addition, two particular different substrates were used to evaluate the bond strength. One of the most common problems associated with this material is the aesthetic shade. It has a narrow range of shade available, which limits its use. Therefore, the bioactive material can be used under a sandwich technique to overcome the esthetic compromise. In addition, the literature showed limited data availability on repair bond strength of Activa with a composite resin that intrigued to conduct such study. Thus, the study outcome provides some clinical perspective in using different surface modifications for repair of bioactive material with resins for durable clinical performance. Moreover, the study recommends further in-vitro and in-vivo studies to assess the cohesive strength of non-repaired materials to compare with repaired shear bond strength for validation of current findings.
CONCLUSION
Within the limitations, it was observed that thermocycling has a negative impact on the shear bond strength; therefore, to increase surface energy for bonding of Bioactive (Activa) Material, mechanical and chemical surface treatments are necessary. A combination of mechanical grinding and silane adhesive (chemical) surface treatment produced a desirable outcome.
REFERENCES
Amaireh, A., Al-Jundi, S. and Alshraideh, H. (2019). In Vitro Evaluation Of Microleakage In Primary Teeth Restored With Three Adhesive Materials: Activa™, Composite Resin, And Resin-Modified Glass Ionomer. European Archives Of Paediatric Dentistry, 20(4):359-67.
Arumugam, M. T., Nesamani, R., Kittappa, K., Sanjeev, K. and Sekar, M. (2014). Effect Of Various Antioxidants On The Shear Bond Strength Of Composite Resin To Bleached Enamel: An In Vitro Study. Journal Of Conservative Dentistry: Jcd, 17(1):22.
Bektas, Ö. Ö., Eren, D., Siso, S. H. and Akin, G. E. (2012). Effect Of Thermocycling On The Bond Strength Of Composite Resin To Bur And Laser Treated Composite Resin. Lasers In Medical Science, 27(4):723-8.
Carvalho, R. M., Manso, A. P., Geraldeli, S., Tay, F. R. and Pashley, D. H. (2012). Durability Of Bonds And Clinical Success Of Adhesive Restorations. Dental Materials, 28(1):72-86.
Cho, S., Rajitrangson, P., Matis, B. and Platt, J. (2013). Effect Of Er, Cr: Ysgg Laser, Air Abrasion, And Silane Application On Repaired Shear Bond Strength Of Composites. Operative Dentistry, 2013;38(3):E58-E66.
Croll, T. P., Berg, J. H. and Donly, K. J. (2015). Dental Repair Material: A Resin-Modified Glass-Ionomer Bioactive Ionic Resin-Based Composite. Compend Contin Educ Dent, 36(1):60-5.
Dickens, C. B. (2015). Waterproof Silane-Endcapped Adhesive Mixture. Google Patents.
Elsaka, S. E. (2016). Influence Of Surface Treatments On The Bond Strength Of Resin Cements To Monolithic Zirconia. J Adhes Dent, 18(5):387-95.
Eslamian, L., Borzabadi-Farahani, A., Mousavi, N. and Ghasemi, A. (2012). A Comparative Study Of Shear Bond Strength Between Metal And Ceramic Brackets And Artificially Aged Composite Restorations Using Different Surface Treatments. The European Journal Of Orthodontics, 34(5):610-7.
Fernández, E., Martín, J., Vildósola, P., Junior, O. O., Gordan, V., Mjor, I., Bersezio, C., Estay, J., De Andrade, M. and Moncada, G. (2015). Can Repair Increase The Longevity Of Composite Resins? Results Of A 10-Year Clinical Trial. Journal Of Dentistry, 43(2):279-86.
Garcia-Godoy, F. and Morrow, B. (2015). Wear Resistance Of New Activa Compared To Other Restorative Materials. J Dent Res, 2015;94:3522.
Garcia-Godoy, F., Morrow, B. and Pameijer, C. (2014). Flexural Strength And Fatigue Of New Activa Rmgics. J Dent Res, 93:254.
Hamano, N., Chiang, Y.-C., Nyamaa, I., Yamaguchi, H., Ino, S., Hickel, R. and Kunzelmann, K.-H. (2012). Repair Of Silorane-Based Dental Composites: Influence Of Surface Treatments. Dental Materials, 28(8):894-902.
Hickel, R., Brüshaver, K. and Ilie, N. (2013). Repair Of Restorations–Criteria For Decision Making And Clinical Recommendations. Dental Materials, 29(1):28-50.
Kaushik, M. and Yadav, M. (2017). Marginal Microleakage Properties Of Activa Bioactive Restorative And Nanohybrid Composite Resin Using Two Different Adhesives In Non Carious Cervical Lesions-An In Vitro Study. Journal Of The West African College Of Surgeons, 7(2):1.
Lee, H.-Y., Han, G.-J., Chang, J. and Son, H.-H. (2017). Bonding Of The Silane Containing Multi-Mode Universal Adhesive For Lithium Disilicate Ceramics. Restorative Dentistry and Endodontics, 42(2):95-104.
Neis, C. A., Albuquerque, N. L. G., Albuquerque, I. D. S., Gomes, E. A., Souza-Filho, C. B. D., Feitosa, V. P., Spazzin, A. O. and Bacchi, A. (2015). Surface Treatments For Repair Of Feldspathic, Leucite-And Lithium Disilicate-Reinforced Glass Ceramics Using Composite Resin. Brazilian Dental Journal, 26(2):152-5.
Özcan, M., Corazza, P. H., Marocho, S. M. S., Barbosa, S. H. and Bottino, M. A. (2013). Repair Bond Strength Of Microhybrid, Nanohybrid And Nanofilled Resin Composites: Effect Of Substrate Resin Type, Surface Conditioning And Ageing. Clinical Oral Investigations, 17(7):1751-8.
Özcan, M. and Koc-Dundar, B. (2014). Composite–Composite Adhesion In Dentistry: A Systematic Review And Meta-Analysis. Journal Of Adhesion Science And Technology, 28(21):2209-29.
Palasuk, J., Platt, J., Cho, S., Levon, J., Brown, D. and Hovijitra, S. (2013). Effect Of Surface Treatments On Microtensile Bond Strength Of Repaired Aged Silorane Resin Composite. Operative Dentistry, 38(1):91-9.
Rengo, C., Goracci, C., Juloski, J., Chieffi, N., Giovannetti, A., Vichi, A. and Ferrari, M. (2012). Influence Of Phosphoric Acid Etching On Microleakage Of A Self‐Etch Adhesive And A Self‐Adhering Composite. Australian Dental Journal, 57(2):220-6.
Takamizawa, T., Barkmeier, W. W., Tsujimoto, A., Scheidel, D., Erickson, R., Latta, M. A. and Miyazaki, M. (2015). Effect Of Phosphoric Acid Pre-Etching On Fatigue Limits Of Self-Etching Adhesives. Operative Dentistry, 40(4):379-95..
Tezvergil, A., Lassila, L. and Vallittu, P. (2003). Composite–Composite Repair Bond Strength: Effect Of Different Adhesion Primers. Journal Of Dentistry, 31(8):521-5
Torres‐Gallegos, I., Zavala‐Alonso, V., Patiño‐Marín, N., Martinez‐Castañon, G., Anusavice, K. and Loyola‐Rodríguez, J. (2012). Enamel Roughness And Depth Profile After Phosphoric Acid Etching Of Healthy And Fluorotic Enamel. Australian Dental Journal, 57(2):151-6.
Wendler, M., Belli, R., Panzer, R., Skibbe, D., Petschelt, A. and Lohbauer, U. (2016). Repair Bond Strength Of Aged Resin Composite After Different Surface And Bonding Treatments. Materials, 9(7):547.
Wiegand, A., Stawarczyk, B., Buchalla, W., Tauböck, T. T., Özcan, M. and Attin, T. (2012). Repair Of Silorane Composite—Using The Same Substrate Or A Methacrylate-Based Composite? Dental Materials, 28(3):e19-e25.
Zhang, K., Zhang, N., Weir, M. D., Reynolds, M. A., Bai, Y. and Xu, H. H. (2017). Bioactive Dental Composites And Bonding Agents Having Remineralizing And Antibacterial Characteristics. Dental Clinics, 61(4):669-87.