Immunology and Cardiology, Biology Department, Faculty of Sciences and Arts-Alkamel Jeddah University, Saudi Arabia
Corresponding author email: Sama.attiyah@gmail.com
Article Publishing History
Received: 16/10/2020
Accepted After Revision: 14/12/2020
The fundamental definition of immunity is the organism’s ability to resist the invasion of micro-organisms and dangerous substances and even unaltered host components. The immune system defends our bodies against the danger of the threat by communicating with chemicals and cells, which are incredibly complex to separate, kill and eliminate potential threats and also can cause disease under some circumstances. The immune system made up of certain and non-certain systems. The non-certain immune system is consisting of two different types of mechanisms (cellular and non-cellular). A certain immune system is completely assisted by lymphocytes and agranular leukocytes. Immune dysfunction or reduced immune competence may be caused by a number of factors such as fatigue, malnutrition and simultaneous infections. Immune-related disorders include allergy, asthma, autoimmune conditions, auto-inflammatory syndromes, and immune deficiency syndromes. Different functions of different immune systems seem to have been the primary driving force in the development of immune systems as a pathogenic diversity defense mechanism.
Evolution of immunity exists over various occasions of the host population lifespan and related to the evolution of pathogen and the frequency shifts in a person’s lymphocyte clone during an infection. The data bases, books and the research published papers in indexed medical and immunological are our references to write the review.This article provides an overview guide in immunity, and describes the properties and classification of the immune system and different types of host defense mechanisms. Focusing on auto-immune diseases, immuno-inflammatory disorders can be categorized as auto-inflammatory or auto-immune inflammasome processes that differ in the presentation of the disease. Therefore, each disease has its properties based on how the immune cells function under certain conditions that result in the cell output becoming abnormal.
Immune, Diseases, Immunology, Leucocytes, System, Innate, Cytokines
Attiyah S. M. N. A Mini Review on Immune System and Immunological Diseases: Properties, Classification and Evolutional Aspects. Biosc.Biotech.Res.Comm. 2020;13(4).
Attiyah S. M. N. A Mini Review on Immune System and Immunological Diseases: Properties, Classification and Evolutional Aspects. Biosc.Biotech.Res.Comm. 2020;13(4). Available from: https://bit.ly/3kK8ZUd
Copyright © Attiyah This is an open access article distributed under the terms of the Creative Commons Attribution License (CC-BY) https://creativecommns.org/licenses/by/4.0/, which permits unrestricted use distribution and reproduction in any medium, provide the original author and source are credited.
INTRODUCTION
The immune system is the most important system that reinforces the immunity and saves humans from all infections, which use a large number of immune cells to function successfully. Immunity operates in a coordinated manner to tackle multiple environmental risks. In order to produce an immune response against disease and certain types of cancer, an adaptive immune system can be activated. The adaptive immune system protects the body against certain external invaders through T and B cell receptors on T and B lymphocyte surfaces (Chaplin 2010). As a result of the recombination of gene fragments, these receptors capable of recognizing different antigens. With contrast, the innate immune response is not antigen-specific, and molecular patterns of a possible future pathogen can be detected using innate immune cells and their mediators (Nicholson, 2016).Bone marrow is primary hematopoietic organ which are responsible for preservation and continuously renewed and differentiation into mature white blood cells (Koliaraki et al., 2020).
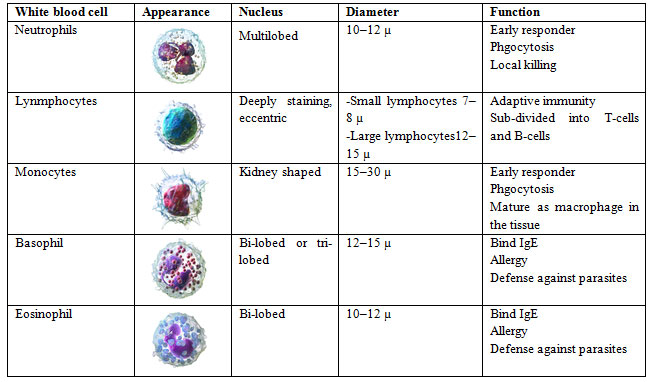
Some of them then undergo important high-school training before being released to patrol the body. Five different white blood cell types will be derived into the bloodstream (Table 1). These population groups can be further subdivided on the basis of proteins expressed in their cell membranes by an immunologist or hematologist. On their surface, the cells express several hundred different receptor forms that can bind to soluble molecules like cytokines. Pattern recognition receptors (PRR) such as duty-like receptors track molecular pathogen patterns and induce specific signaling pathways to trigger the immune system response (Lee, 2016).The natural immunity generated after the first encounter and resists of a particular species of microorganisms. The immunizations of dead or life microorganisms will trigger acquired (adaptive or specific) immunity for the individual. However, acquired immunity can occur in a natural or artificial way (Varadé et al., 2020).
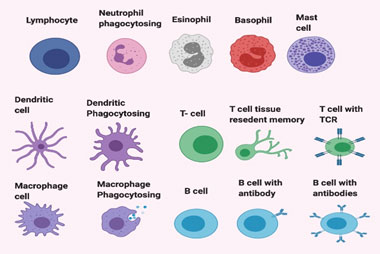
Immune cells: The role of various types of white blood cells is fighting infections. The most common forms of these are cell macrophages and neutrophils of the innate immune system (Figure 1). Macrophages are a specific type involved in the detection. Both macrophages and neutrophils respond rapidly to infectious pathogenic agents producing cytokines that recruit and activate immune cells. They secrete enzymes and chemicals that digest protein. Then they swallow up and digest the damage, a process that is called phagocytosis. Such cells embody adaptation and memory functions, which enable the immune system to respond increasingly specifically and remember individual infection types (Prame et al., 2018).
Natural killer cells (NK) play an important role in managing viral infections and cancers as well as in the regulation of macrophages and dendritic cells(Table 1). Granulocyte cells (basophils, Mast cells, and eosinophils) are able to protect the human body from parasites and modulate immune responses(Brodin, 2017). Furthermore, B lymphocytes’ functional role is the production of “antibody (Ab)” as an effector tool, which is an immunoglobulin molecule biochemically. Memory B cells are key to quick evelopment after re-infection with protective immunity(Laidlaw and Cyster 2020). T lymphocytes are divided into two subclasses according to their surface markers: CD4 and CD8 lymphocytes (Karim et al 2015).
Throughout innate and adaptive crosstalk, dendritic cells demonstrate a key role in the initiation of adaptive immune responses to pathogens (Waisman et al., 2017). Mast cells able to support vascular permeability and accelerate leukocyte recruitment by inducing pro-inflammatory mediators within the immune system (da Silva et al ., 2014). The natural killer cells are similar in terms of morphology with the lymphocytes except that the cytoplasm has granules. Natural killer cells are part of the innate immune system and help in defend the host by killing the foreign pathogen (Bald et al., 2020).
Of the same progenitors natural killer cells evolve but vary into separate sub-sets that vary in development of cytokine, cytotoxicity, homing, and memory (Collins et al., 2019). It was found that, there is a correlation between NK cells and genes that encode immune checkpoint proteins (Wu et al., 2019). Macrophages, B lymphocytes, and dendritic cells are antigen-presenting cells (APC) that can present antigen. Dendritic cell phagocytosis step is the connection point between the two types of the immune system (adaptive and innate), which present the essential dendritic cells in the human body(de Jong et al., 2006).The provision of pathogen defensive immune responses involves unique niches wherein leucocytes are trained by numerous types of cells, including mesenchymal cells (Koliaraki et al., 2020).
Figure 1: Cells of the immune system.
Table 1. White blood cells and their function (Handin et al 2003).
Immunoglobulins: Immunoglobulins are glycoprotein molecules made from plasma cells, also known as antibodies. The first antigen-specific receptor to be identified is immunoglobulin which is usually drawn as a cartoon in the shape of a Y (Table 2). Two identical light and heavy chains are present in the Y shape. Antibodies bind strongly on a target (antigen) and signal immune cells (Figure 2). There are two physical types of antibodies: a soluble form that is secreted from cells free of plasma in the blood. In addition to membrane-bound form attached to the cell surface called the B-cell receptor. There are three effector functions of Abs: neutralization, opsonization, and complement fixation. Nowadays, there are five classes of Ig found in the human body, termed as IgA, IgG, IgM, IgE, IgD (Table 2) (Janeway et al., 2001, Senger et al., 2015).
IgG is the largest monomer circulating antibodies, accounting for 80% and 75% of the total serum antibodies. IgG provides the bulk of pathogens-based antibody immunity.
IgA is a dimeric antibody found in mucous secretions as well as respiratory, genitourinary, gastrointestinal secretions.
IgM is the largest antibody with pentamer structures. It is expressed on the surface of B lymphocyte and can also found in serum.
IgD is monovalent and is found on the B-lymphocyte surface that serves as an antigen receptor for activating B cells in combination with the monomeric IgM.
IgE is a monomeric antibody and usually bound to tissue cells, mostly mast cells and associated with the allergic response.
Figure 2: The diversity of immunoglobulin types.
Table 2. The 5 major classes of immunoglobulin types which have different roles in the immune response (Schroeder& Cavacini 2010 and Vidarsson et al 2014).
| Antibody | Secreted form | Percentage in serum | Cross placenta | No. of antigen binding sits | Function |
| IgA | Dimer | 13 % | No | 4 | Mucosal immunity |
| IgE | Monomer | 0.002 % | No | 2 | Defense against parasites
Allergy |
| IgG | Monomer | 80 % | Yes | 2 | Complement activation
Neonatal immunity |
| IgM | Pentamer | 6 % | No | 10 | Native B-cell receptor
Natural antibodies Complement activation |
| IgD | Monomer | 1 % | No | 2 | Native B-cell receptor |
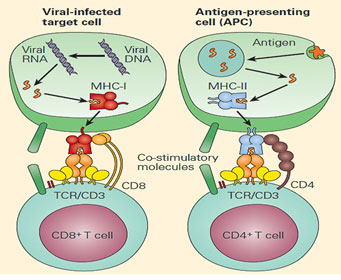
Adaptive immunity: Adaptive immunity has evolved to give both self and non-self-antigens a broader and finer repertoire of recognition. Immunoglobulins (Ig) or antibodies are plasma-cell glycoproteins instructed by specific immunogens (Sotiropoulos and Tsihrintzis 2017). The immunogen interacts with the B cell receptor (BCR) on the cell surface and produces a signal to induce the synthesis of antibody which are highly specific to immunogen that stimulated the B cell. However, the immune system remembers the antigens due to the growth of memory B cells, which triggered a previous reaction as a memory (Bonilla and Oettgen, 2010). Adaptive immunity involves tightly regulation between T and B cells, which facilitate pathogenic pathways of immune effectors, immunological memory generation and the control of host immune homeostasis (McComb et al., 2013).The T-cell function of the immune response is primarily involved in the recognition and removal of infected cells. In addition, T cells can identify antigen peptide fragments that engaged by APC via a phagocytosis or pinocytosis process. The αβ TCR surface expression is the dominant class of T cells. These receptors are primarily developed to identify peptide antigens in a complex comprising MHC proteins of class I or class II (Lee 2019).
Innate immunity: Innate signals are necessary to activate the adaptive immune system. The adaptive immune system takes advantage of an innate system’s ability to discriminate between contact with dangerous pathogens and safety or even useful microbes and environmental factors by using innate signals to help initiate its reactions. The innate and adaptive divisions of the immune response should, therefore, be seen as complementary and collaborative (Chaplin 2010). Innate and adaptive system work side by side as a team against invading microbes, one establish to identify and the other one recognizes and remember specific pathogens. These depend on a group of proteins and phagocytic cells, which recognize and become quickly activated for the destruction of invaders by preserved pathogen characteristics, (Netea et al., 2020).
Major His to compatibility Molecules: The infected cell used to produce future offspring microbes must be detected and destroyed. An important role of the immune response of T cells is the detection and destruction of damaged cells. Moreover, T cells able to identify peptide antigen fragments that were absorbed by APC during phagocytosis or pinocytosis. The identification of damage host cells will be completed using an auto-component and a microbial structure recognized by T cells (Tomar and De 2014).The MHC family of molecules is the elegant way to solve both an auto-structure and a microbial determinant. MHC molecules are cell surface glycoproteins that attach to peptide-protein fragments. Peptides either synthesized in the cell (class I MHC molecules) or absorbed by the cell and then proteolytically processed (Class II MHC molecules)(figure 3) (Godfrey et al., 2004; Wieczorek et al.2017).
Figure 3: CD8 T cells usually recognize the endogenous antigens (left panel), CD4 T cells usually recognize the exogenous antigens (right panel) (Bonini 2012).
MHC I molecules are glycoproteins located on all nucleated cells surface. Their function is to demonstrate peptide fragments within the cell to cytotoxic T cells (CD8+ T Cells). This step will trigger immediate immune system reactions to a specific antigen present with the aid of an I protein in MHC I (Blander 2016). MHC II molecules are glycoproteins, which interact with antigen-presenting cells (APCs) such as dendritic and macrophages cells. APCs engulf foreign particles then present antigen to T and B cells. Phagocytosis contributes to the epitope loading process within the MCH Class II molecule; endocytosis is used to digest extract proteins from lysosomes. Epitopic peptide fragments that arise from this progression is loaded into the MHC Class II molecules before they leave to the cell surface (Rock et al., 2016). Exogenous antigens which initiated extracellularly from foreign organisms such as bacteria will easily recognize by helper T cell lymphocytes (CD4+ T cells) inducing antibody production and attracts immune cells to the infection region (Aluri et al., 2018).
Complements: The complement structure is a significant element within the immunity system. The complement system is prepared by a wide range of separate plasma proteins, reacting with pathogens to induce a variety of inflammatory reactions that serve to combat infection and improve their ability to eliminate microbes and damaged cells from body system, (Carroll 2004). The complements activation process follows several different ways; 1)classical pathway which is activated by direct attachment between complement component C1q and the pathogen surface, or using an antibody. 2) the MB-lectin pathway which is produced by mannan-binding lectin, 3) the alternative pathway that activated directly on pathogen surfaces. All of these pathways generate a crucial enzymatic activity that, in turn, generates the effector molecules of complement. The three key effects of complement activation include pathogens ‘ opsonization, inflammatory cell recruitment and direct killing of pathogens (Spiering 2015 & Kolev and Markiewski 2018).
Cytokines: Cytokines are cell-released proteins, which have a specific effect on cell-to-cell interactions and communication. Pro-inflammatory and anti-inflammatory cytokines are both available. Cytokines are formed by various cell types, however, T cells (Th) and macrophages are the predominant producers. Cytokines work by binding to a receptor, which sends a signal to the receiver cell that leads to a functional or phenotype transition. Such signal cascades are complex and include a variety of environmental considerations. There are currently many more cytokines examined as therapeutic objectives or as therapeutic agents (Seillet et al., 2014)
Toll-Like Receptors: Toll-like receptors are a protein class that shows a critical function in the innate immune system. Ten human Toll-like (TLR) receptors were identified now. They are usually expressed on main cells include macrophages and dendritic cells that identify pathogen-associated molecule patterns (PAMPs) resulting from different microbes. In many respects of the innate immune response to certain pathogens, TLR signaling tends to be divergent and plays an important role, (Kawasaki and Kawai ,2014 & Liu et al., 2020).
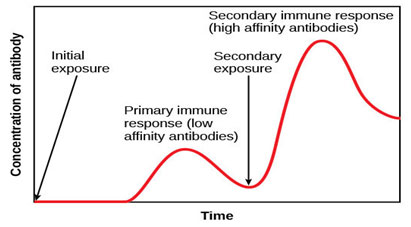
Immune memory: The classical immune memory assessment is based on the reaction of the antibody. Specific antibody level rises after an infection (or vaccination), then decreases over time to lower levels, not as small as in a naive state. Recharging the same stimulus results in faster development of more antibodies and high avidity through the evolution and selection of higher affinity antibodies (figure 4). There are also other shifts, particularly since the prevalent antibody response isotype would typically have shifted to IgG (and IgA or IgE) (Paul 2015).
Figure 4: Primary response shows the initial production of antibodies from plasma cells. Memory cells differentiate to plasma cells after the same microbe will expose. Differentiated plasma cells induce antibodies that will continuously discharge a large number of antibodies (Paul 2015).
Immune system diseases: Immunological disorders are conditions caused by an immune system deficiency or heterogeneous aberrations that cause the system to work against itself. In fact, this condition may occur due to an irregular activation of the immune system because of a regulatory function weakening that has damaged it and triggers a strong reaction to it. Such diseases also serve as one of the world’s leading deaths. (Aribi, 2017). Autoimmunity is conceptually considered as a defect of the lymphocyte selection, either in B or T, with aberrant lymphocytic responses. In recent years the autoimmunity hypothesis has been renewed by an improved genetic understanding of both common and rare diseases, coupled with mutations that represent disturbances of the immune system, ranging from Thyme, B, and T to T regulatory cells (Dosanjh 2015).
Self and Non-self Discrimination: Self-tolerance is called the capacity of the immune response to prevent damaging self-tissues. Therefore, the wide variety of autoimmune diseases underlie self-tolerance failure (Furusawa and Yamaguchi 2016). As a significant aspect of the immune system’s T-cell arm is to detect cells affected by viruses, intracellular bacteria or other intracellular parasites, T-cells can form an advance mechanism that identifies foreign antigens as a complex molecule. T cells are responsible to spot and discover both self-structuring and external antigens when they preserve their self-tolerant (Chaplin and David 2009).
Classifications and properties of immunological diseases: All immunological diseases can appear as a result of purely Autoinflammatory, autoimmune, or a combination of Autoinflammatory–autoimmune mechanisms that interact variably in the expression of disease (McGonagle & McDermott, 2006).The most common immunological diseases (Health, 2003) classified as:
Allergic Diseases: Allergic diseases can form as a result of the response of the immune system to an inappropriate alarm, which spots specific materials such as house dust and grass pollen as very harmful elements to an allergic individual.
Autoimmune Diseases: In recent years, substantial progress has been made towards learning how nearly any part of the immune system leads to systemic autoimmunity, (Tsokos 2020). The specific causes of the autoimmune disease are not exactly known, but this type of disease is appeared when the immune system cells are directed against the body cells and organs due to a break down in the immune system’s recognition apparatus. When a break down happens, the body starts manufacturing auto-antibodies and Misguided T cells. T lymphocyte is the most responsible cells to different diseases such as diabetes, rheumatoid arthritis, systemic lupus erythematosus (SLE). Multiple factors are playing a role in the autoimmune disease that includes certain drugs, viruses, and sunlight. Moreover, Hormones and Heredity seem to have a role in this disease too (Wang et al., 2015).
Immune Complex Diseases: These diseases can develop when Immune complexes trapped in skin tissue, the lungs, joints, the kidneys, or blood vessels. These complexes are a Collection of interlocking antigens. Usually, they quickly removed from the bloodstreams but sometimes they continue to circulate so they trapped in the body tissues. Moreover, these complexes generate several reactions that lead to tissue damage and inflammation. Additionally, these complexes are having a role in many diseases such as viral hepatitis, malaria, and many autoimmune diseases (Carter 1973 & Clarke et al., 2018).
Immunodeficiency Disorders: The human can gain immunodeficiency disorder if the immune system misses one or more of its normal components. Usually, they can be inherited, produced unintentionally by drugs, or acquired through infection. Moreover, immunodeficiency disorder has a role in many diseases such as severe combined immunodeficiency disease (SCID) and AIDS (Justiz 2020).
Auto-inflammation: The inflammasome and intracytoplasmic structure able to produce many proteins when the cell naturally threated, which is considered as an essential sensor. The inflammasome sub-units come together and activate an enzyme that then releases cytokines that encourage inflammation. Such cytokines can cause disease and fever once in circulation. Inflammasome activation is triggered by changes in the environment that cause the subunits to assemble (Libby 2007).
Cancers of the Immune System: This cancer can gain because of the uncontrollable growth of the immune cells such as the uncontrolled growth of leukocytes and antibody-producing plasma cells. On the other hand, this uncontrolled growth of immune system cells can lead to many different kinds of cancers such as leukemia and the cancer of the lymphoid organs (Gonzalez et al., 2018).
Evolution of immune systems: Evolution of immunity takes place at various stages during the lifespan of the host and the evolution of variants of pathogens and the shifts in frequency of lymphocyte clones throughout a person’s infection (Kaufman 2010).Particular cell types are related to multiple conditions and they represent the specific body defense role of that cell type. Neonates have usually a high white blood cell count, which is eventually lowered to adult levels. An exception are the low count of Lymphocytes at birth, which in the first four years of life hits its maximum level and then eventually declines to healthy levels of adults (Katharina et al., 2015). Practically all species provide at least one type of protection to deter organisms that cause diseases. Advanced vertebrate animals, a human group, protect themselves against these microorganisms by the immune system through a complex set of defense responses. This defensive system emerged by basic defense mechanisms, although it is not completely certain which evolutionary twists and turns contributed to its development, (Broecker and Moelling 2019).
CONCLUSION
This review has been focused in particular on the immune system and immunological diseases as well as properties, classifications, and evolution of immunological diseases and immune systems. This review has the potential to shed light on the different roles of each cell in the immunity system and how this system plays an essential role in immunological diseases. Starting with the significant role of an immune system and the human body, ending with the immunological diseases and how they affect this system. The immune system is a complex network of cells, proteins, and signaling that prevent infection in the body. There are many mechanisms in the immune system to combat microbial infection. The mechanisms work together to eliminate many harmful effects and to alter the reaction to specific invading pathogens within the immune response. The formation of immune memory is required to learn and record different pathogens that contribute to the body system to produce successful and rapid immune responses after subsequent exposure to the same pathogens.
Immune system defects can lead to allergy, asthma, immune deficiency and any other autoimmune disorders. The response of the immune cells at these conditions determine the type of disease. In addition, the factors that can have a role in immunological diseases such as heredity, unintentional production by drugs, or the acquisition through infection can cause an imbalance in immunity. Immunological diseases and immunity require more future work and research to suppress and prevent the development of these types of diseases. Understanding the relations between the various immune-effector pathways will allow researchers to discover strong and effector treatment for immunomodulation, in addition, to improve vaccine development.
REFERENCES
Aluri J, Gupta M, Dalvi A, Mhatre S, Kulkarni M, Hule G, Desai M, Shah N, Taur P, Vedam R, Madkaikar M. (2018): Clinical, Immunological, and Molecular Findings in Five Patients with Major Histocompatibility Complex Class II Deficiency from India. Front Immunol.;9:188. [PMC free article] [PubMed]
Aribi, M. (2017): Introductory Chapter: Immune System Dysfunction and Autoimmune Diseases. IntechOpen, 1-8.
Bald, T., Krummel, M.F., Smyth, M.J. et al. (2020): The NK cell–cancer cycle: advances and new challenges in NK cell–based immunotherapies. Nat Immunol 21, 835–847. https://doi.org/10.1038/s41590-020-0728-z.
Blander J. M. (2016): The comings and goings of MHC class I molecules herald a new dawn in cross-presentation. Immunological reviews, 272(1), 65–79. https://doi.org/10.1111/imr.12428
Bonilla, F. A. and Oettgen H.C(2010): Adaptive immunity: Journal of Allergy and Clinical Immunology, Volume 125, Issue 2, S33 – S40
Bonini S. (2012): Immunology IV: Clinical Applications in Health and Disease by Joseph A. Bellanti. The World Allergy Organization Journal, 5(8), 94. doi:10.1097/WOX.0b013e3182641db0
Brodin, P., Davis, M (2017). Human immune system variation. Nat Rev Immunol 17, 21–29. https://doi.org/10.1038/nri.2016.125
Broecker, F. and Moelling, K. Evolution of immune systems from viruses and transposable elements. Front. Microbiol. 10, 51 (2019). https://doi.org/10.3389/fmicb.2019.00051
Carroll MC(2004): The complement system in regulation of adaptive immunity. Nat Immunol.;5:981–986. [PubMed] [Google Scholar]
Carter P. M. (1973): Immune complex disease. Annals of the rheumatic diseases, 32(3), 265–271. https://doi.org/10.1136/ard.32.3.265
Chaplin DD (2010): Overview of the immune response. J Allergy Clin Immunol.;125(2 Suppl 2):S3–S23. doi:10.1016/j.jaci.2009.12.980
Chaplin DD. (2010): Overview of the immune response. J Allergy Clin Immunol. Feb;125(2 Suppl 2):S3-23. doi: 10.1016/j.jaci.2009.12.980. PMID: 20176265; PMCID: PMC2923430.
Chaplin David D. (2010): Overview of the immune response. The Journal of allergy and clinical immunology vol. 125,2 Suppl 2 (S3-23. doi:10.1016/j.jaci.2009.12.980
Clarke, F., Purvis, H.A., Sanchez-Blanco, C. et al. (2018): The protein tyrosine phosphatase PTPN22 negatively regulates presentation of immune complex derived antigens. Sci Rep 8, 12692. https://doi.org/10.1038/s41598-018-31179-x
Collins PL, Cella M, Porter SI, Li S, Gurewitz GL, Hong HS, Johnson RP, Oltz EM, Colonna M. (2019): Gene Regulatory Programs Conferring Phenotypic Identities to Human NK Cells. Cell. Jan 10;176(1-2):348-360.e12. doi: 10.1016/j.cell.2018.11.045. Epub 2018 Dec 27. PMID: 30595449; PMCID: PMC6329660.
da Silva EZ, Jamur MC, Oliver C. (2014): Mast cell function: a new vision of an old cell. J Histochem Cytochem. Oct;62(10):698-738. doi: 10.1369/0022155414545334. Epub 2014 Jul 25. PMID: 25062998; PMCID: PMC4230976.
de Jong, J. M., Schuurhuis, D. H., Ioan-Facsinay, A., Welling, M. M., Camps, M. G., van der Voort, E. I., Huizinga, T. W., Ossendorp, F., Verbeek, J. S., & Toes, R. E. (2006): Dendritic cells, but not macrophages or B cells, activate major histocompatibility complex class II-restricted CD4+ T cells upon immune-complex uptake in vivo. Immunology, 119(4), 499–506. https://doi.org/10.1111/j.1365-2567.2006.02464.x
Dosanjh A. (2015): Autoimmunity and Immunodeficiency. Pediatr Rev. Nov;36(11):489-94; quiz 495. [PubMed]
Furusawa, C., & Yamaguchi, T. (2016): Robust and Accurate Discrimination of Self/Non-Self Antigen Presentations by Regulatory T Cell Suppression. PloS one, 11(9), e0163134. https://doi.org/10.1371/journal.pone.0163134
Godfrey DI, MacDonald HR, Kronenberg M, Smyth MJ, Van Kaer L. (2004): NKT cells: what’s in a name? Nat Rev Immunol.;4:231–237. [PubMed] [Google Scholar]
Gonzalez, H., Hagerling, C., & Werb, Z. (2018): Roles of the immune system in cancer: from tumor initiation to metastatic progression. Genes & development, 32(19-20), 1267–1284. https://doi.org/10.1101/gad.314617.118
Handin RI, Lux SE, Stossel TP (2003): Blood: Principles and Practice of Hematology (2nd ed.). Philadelphia: Lippincott Williams and Wilkins. p. 471. ISBN 9780781719933.
Janeway CA Jr, Travers P, Walport M, et al. (2001): Immunobiology: The Immune System in Health and Disease. 5th edition. New York: Garland Science; The distribution and functions of immunoglobulin isotypes. Available from: https://www.ncbi.nlm.nih.gov/books/NBK27162/
Justiz Vaillant AA, Qurie A. (2020): Immunodeficiency. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK500027/
Justiz Vaillant AA, Ramphul K. (2020): ImmunoglobulinIn: StatPearls. Treasure Island (FL): StatPearls. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513460/
Karim M. Yatim and Fadi G. Lakkis (2015): A Brief Journey through the Immune System. CJASN Jul 2015, 10 (7) 1274-1281; DOI: 10.2215/CJN.10031014
Katharina Simon A., Georg A. Hollander and Andrew McMichael (2015): Evolution of the immune system in humans from infancy to old age. Published by the Royal Society. https://doi.org/10.1098/rspb.2014.3085
Kaufman J. (2010). Evolution and immunity. Immunology, 130(4), 459–462. https://doi.org/10.1111/j.1365-2567.2010.03294.x
Kawasaki T and Kawai T (2014): Toll-like receptor signaling pathways. Front. Immunol. 5:461. doi: 10.3389/fimmu.2014.00461
Kolev, M., & Markiewski, M. M. (2018): Targeting complement-mediated immunoregulation for cancer immunotherapy. Seminars in immunology, 37, 85–97. https://doi.org/10.1016/j.smim.2018.02.003
Koliaraki, V., Prados, A., Armaka, M. et al. (2020): The mesenchymal context in inflammation, immunity and cancer. Nat Immunol 21, 974–982. https://doi.org/10.1038/s41590-020-0741-2
Laidlaw, B.J., Cyster, J.G. (2020): Transcriptional regulation of memory B cell differentiation. Nat Rev Immunol. https://doi.org/10.1038/s41577-020-00446-2.
Lee T. M. (2016): Immunity. Emerging Infectious Diseases, 22(4), 766. doi:10.3201/eid2204.151858
Lee W.J. (2019): Immune System. In: Vitamin C in Human Health and Disease. Springer, Dordrecht. https://doi.org/10.1007/978-94-024-1713-5_4.
Libby P. (2007): Inflammatory mechanisms: The molecular basis of inflammation and disease. Nutr. Rev.;65:S140–S146. doi: 10.1301/nr.2007.dec.S140-S146. [PubMed] [CrossRef] [Google Scholar]
Liu, G., Zhang, H., Zhao, C., & Zhang, H. (2020): Evolutionary History of the Toll-Like Receptor Gene Family across Vertebrates. Genome biology and evolution, 12(1), 3615–3634. https://doi.org/10.1093/gbe/evz266
McComb S., Thiriot A., Krishnan L., Stark F. (2013): Introduction to the Immune System. In: Fulton K., Twine S. (eds) Immunoproteomics. Methods in Molecular Biology (Methods and Protocols), vol 1061. Humana Press, Totowa, NJ
Netea, M. G., Domínguez-Andrés, J., Barreiro, L. B., Chavakis, T., Divangahi, M., Fuchs, E., Joosten, L., van der Meer, J., Mhlanga, M. M., Mulder, W., Riksen, N. P., Schlitzer, A., Schultze, J. L., Stabell Benn, C., Sun, J. C., Xavier, R. J., & Latz, E. (2020): Defining trained immunity and its role in health and disease. Nature reviews. Immunology, 20(6), 375–388. https://doi.org/10.1038/s41577-020-0285-6
Nicholson, L. B. (2016): The immune system. Portland Press Limited on behalf of the Biochemical Society and distributed under the Creative Commons Attribution, 275-301.
Prame Kumar, K., Nicholls, A. J., & Wong, C. (2018): Partners in crime: neutrophils and monocytes/macrophages in inflammation and disease. Cell and tissue research, 371(3), 551–565. https://doi.org/10.1007/s00441-017-2753-2
Rock, K. L., Reits, E., & Neefjes, J. (2016): Present Yourself! By MHC Class I and MHC Class II Molecules. Trends in immunology, 37(11), 724–737. https://doi.org/10.1016/j.it.2016.08.010
Schroeder, H. W., Jr, & Cavacini, L. (2010): Structure and function of immunoglobulins. The Journal of allergy and clinical immunology, 125(2 Suppl 2), S41–S52. https://doi.org/10.1016/j.jaci.2009.09.046
Seillet C, Belz GT, Mielke LA. (2014): Complexity of cytokine network regulation of innate lymphoid cells in protective immunity. Cytokine. 2014 Nov;70(1):1-10. doi: 10.1016/j.cyto.2014.06.002. Epub Jun 25. PMID: 24972988.
Senger K., Hackney J., Payandeh J., Zarrin A.A. (2015): Antibody Isotype Switching in Vertebrates. In: Hsu E., Du Pasquier L. (eds) Pathogen-Host Interactions: Antigenic Variation v. Somatic Adaptations. Results and Problems in Cell Differentiation, vol 57. Springer, Cham
Sotiropoulos D.N., Tsihrintzis G.A. (2017): Immune System Fundamentals. In: Machine Learning Paradigms. Intelligent Systems Reference Library, vol 118. Springer, Cham. https://doi.org/10.1007/978-3-319-47194-5_6.
Spiering MJ. (2015): Primer on the Immune System. Alcohol Res.;37(2):171-5. PMID: 26695756; PMCID: PMC4590614.
Tomar N, De RK.(2014): A brief outline of the immune system. Methods Mol Biol.;1184:3-12. doi: 10.1007/978-1-4939-1115-8_1. PMID: 25048116.
Tsokos, G.C. (2020): Autoimmunity and organ damage in systemic lupus erythematosus. Nat Immunol 21, 605–614. https://doi.org/10.1038/s41590-020-0677-6.
Varadé J, Magadán S, González-Fernández Á. (2020): Human immunology and immunotherapy: main achievements and challenges. Cell Mol Immunol. Sep 2:1–24. doi: 10.1038/s41423-020-00530-6. Epub ahead of print. PMID: 32879472; PMCID: PMC7463107.
Vidarsson, G., Dekkers, G., & Rispens, T. (2014): IgG subclasses and allotypes: from structure to effector functions. Frontiers in immunology, 5, 520. https://doi.org/10.3389/fimmu.2014.00520
Waisman A, Lukas D, Clausen BE, Yogev N. (2017): Dendritic cells as gatekeepers of tolerance. Semin Immunopathol. Feb;39(2):153-163. doi: 10.1007/s00281-016-0583-z. Epub 2016 Jul 25. PMID: 27456849.
Wang L, Wang FS, Gershwin ME. (2015): Human autoimmune diseases: a comprehensive update. J Intern Med. Oct;278(4):369-95. doi: 10.1111/joim.12395. Epub 2015 Jul 25. PMID: 26212387.
Wieczorek M, Abualrous ET, Sticht J, et al.(2017): Major Histocompatibility Complex (MHC) Class I and MHC Class II Proteins: Conformational Plasticity in Antigen Presentation. Front Immunol. 2017;8:292. Published Mar 17. doi:10.3389/fimmu.2017.00292
Wu M, Mei F, Liu W, Jiang J. (2019): Comprehensive characterization of tumor infiltrating natural killer cells and clinical significance in hepatocellular carcinoma based on gene expression profiles. Biomed Pharmacother. 2020 Jan;121:109637. doi: 10.1016/j.biopha.109637. Epub Nov 24. PMID: 31810126.