1Associate Professor; Department of Periodontics and Community Dentistry, College of Dentistry, King Saud University. Riyadh, Saudi Arabia,
2Internship Program; College of Dentistry, King Saud University, Riyadh, Saudi Arabia
Corresponding author email: Khalidh@ksu.edu.sa
Article Publishing History
Received: 14/07/2020
Accepted After Revision: 15/09/2020
To achieve desirable functional and esthetic objectives in implant treatment, detailed case study, and planning is required. Since the introduction of 3D-printed technology into multiple fields, such as medicine and engineering, the use of this technology in dentistry is still to be explored. This study aimed to assess implant placement accuracy using two different implant surgical guides: thermoplastic (TP) and 3D-printed. Thirty acrylic resin mandibles missing the second premolar were fabricated with stereolithography (SLA) based on data from the CBCT scan. 15 TP and 15 3D-printed guides were constructed for the placement of the implants in relation to the mental foramen, and virtual implant apex distance from the mental foramen was set as 3.18 mm. 30 dummy 3.5 x 8mm implants were installed into the replica jaw models. Post-placement CBCT scans were compared to the virtual implant placement in relation to the mental foramen with the actual implant placement. The mean±SD of the implant distance to mental foramen for the 3D and TP guides was 3.12±0.36 mm and 2.52± 0.83 mm (P<0.05); respectively. The deviation apex of the implant for the 3D-printed and TP guides was 0.92±0.14 mm and 1.57±0.45 mm (P<0.001); respectively. The angular deviation of the 3D-printed and TP guides was 3.33 ±0.86o and 4.03±1.13o, respectively. Based on this study, the 3D printed guides were more accurate than the TP guides in terms of implant placement accuracy in relation to an important landmark and 3D implant placement.
CBCT, Dental Implant, 3D-Printed Guide
Al-Hamdan K, Al-Oaibi A, AlWadai T, AlFadda A. Accuracy of Implant Placement Utilizing 3D Printed and Thermoplastic Surgical Guides: A CBCT-Analysis. Biosc.Biotech.Res.Comm. 2020;13(3).
Al-Hamdan K, Al-Oaibi A, AlWadai T, AlFadda A. Accuracy of Implant Placement Utilizing 3D Printed and Thermoplastic Surgical Guides: A CBCT-Analysis. Biosc.Biotech.Res.Comm. 2020;13(3). Available from: https://bit.ly/3ipruMC
Copyright © Al-Hamdan et al., This is an open access article distributed under the terms of the Creative Commons Attribution License (CC-BY) https://creativecommons.org/licenses/by/4.0/, which permits unrestricted use distribution and reproduction in any medium, provide the original author and source are credited.
INTRODUCTION
Since the beginning of the implantology era, clinicians paid a great effort to improve implant performance and to minimize adverse effects and procedural errors. The accuracy of surgical implant placement and its relation and proximity to vital structures has always been a concern of the practitioners.Methods such as the use of a clipper measurement system and cone-beam computed tomography (CBCT) in the treatment planning of implant treatment have been used, and both showed some degree of inconsistency (Chen et al., 2008). The traditional method of placing an implant with the help of a surgical guide is to construct a radiographic stent, then transforming it to a surgical guiding device after taking CBCT (Misch 2004). However, the use of the traditional method has complicated lap procedures, limited accuracy, and tricky implant fixture surgical placement (Nickenig and Eitner, 2007). To overcome the shortcoming of the traditional method, computer-aided design/computer-assisted manufacturing (CAD/CAM) technology was introduced in 1971, and it has been used more often recently in dentistry (Kim et al., 2018 Abdou and Lau 2020).
In CAD/CAM system, CAD undergoes a process of scanning and designing, and CAM systems are divided into subtractive manufacturing (SM) and additive manufacturing (AM) (Kim et al., 2018). Solidified blocks are milled in subtractive manufacturing, which provides high accuracy (Kim et al., 2018). However, the waste material cannot be reused; different burs are used for different blokes, and due to bur erosion, errors may occur, which makes the subtractive manufacturing costs high (Kim et al., 2016a, Ortorp et al., 2011 Abdou and Lau 2020).
A potential solution to the problems of subtractive manufacturing is the additive manufacturing, which involves high-intensity laser as an energy source to melt and fuse selective regions of powder, layer-by-layer free-form to build up a 3-dimensional component according to the computer-aided designed structure using different materials (Kim et al., 2017b). For the individual layers to be generated, the CAD data are uploaded to the selective laser melting (SLM) machine for the production of components, the micro-stereolithography (µ-SLA) files have to be processed by the software, such as Magic, to provide support to structures for any overhanging features (Joo et al., 2016). 3D-printed surgical templates are printed with the use of digital light processing (DLP) which uses a layered, ultraviolet (UV)-cured resin material, and only each UV resin layer is only a few microns thick, resulting in a highly precise surgical template (Kim et al., 2017a, Lee and Cho, 2003). Another great advantage is the commercially available software, which allows clinicians to interact with CT scan data. The combination of CT-based treatment planning and (CAD/CAM) of surgical templates allows clinicians to plan treatment in advance (Kim et al., 2016b Abdou and Lau 2020).
This technology is a revolutionary method that is expected to open new and better approaches of treatment (Schneider et al., 2009). 3D-printing was first used as rapid prototyping and rapid tooling technology. Dentistry use of single, personalized objects made a strong relationship between the two fields. Dental labs already started using 3D-printing in accurately manufacturing crowns, bridges, plaster/stone models, orthodontic, and surgical appliances (Kuhl et al., 2013). 3D-printing was also used in manufacturing single titanium dental implants with a promising success (Buser et al., 2012 Abdou Lau 2020). Therefore, this study conducted to assess the accuracy of implant placement using 3D-printed and thermoplastic surgical guides.
MATERIAL AND METHODS
Data acquisition:This study was conducted to evaluate the accuracy of implants placed using two different guided implant surgery materials: thermoplastic versus 3D-printed. Thirty acrylic resin mandibles were fabricated with stereolithography (SLA) based on data from the cone beam computerized tomography (CBCT) scan, which were converted into a Digital Imaging and Communications in Medicine (DICOM) file. The mandible was modified digitally by removing the lower right second premolar by using (zarokhan modifier) and converted to STL file before printing. The planed model of the mandible jaw was then exported for printing and was printed using (FORMALAB2) 3D-printer. Registration of the mental foramen was done clinically and was marked by a Standard composite cube to be accurately located, and a CBCT scan was taken for the resin mandibles.
Surgical plan and template fabrication: The modified CBCT scanned data was exported to an implant planning software (ProDigiDent, ImplaStation for Windows x6464 Bit Beta Version) for planning a specified implant position in relation to the mental foramen. A digital plaster model was then imported and superimposed with the CBCT data and exported to an STL file for the fabrication of the surgical template. All templates were printed using (FORMALAB2) 3D-printer using UV cured acrylic-based resin in 16 um layers. A total of 15 3D-printed surgical guides and 15 thermoplastic surgical guides had been made for the placement of the implants in relation to the mental foramen by the same lab technician and virtual implant apex distance from the mental foramen was set as 3.18 mm. One (ASTRA TECH) 3.5 x 8 mm implant was placed per guide and replica jaw model. Postsurgical CBCT scans were done to compare the virtual implant placement in relation to the mental foramen with the actual implant placement.
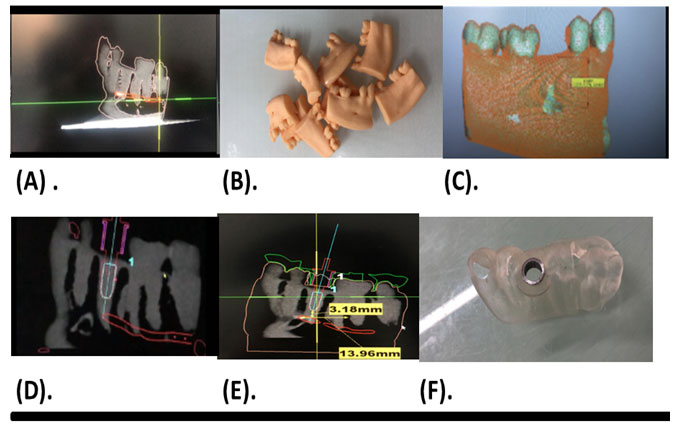
Figure 1: Data acquisition and surgical plan. (A) Mandibular digital model. (B). Resin model, (C). digitel resin model, (D) planned implant position, (E). surgical template created by the software, (F) Surgical template.
Statistical Analysis: Regarding the statistical analysis, Independent Samples Test and post hoc analysis were utilized with a p-value ≤ 0.05 that considered the cut-off point of statistical significance.
RESULTS AND DISCUSSION
All CBCT scans of the surgical template fitted on the plaster model were performed by the same operator. There were 15 implants planned in the software, and no templets were fractured in this study. There were significant differences in all outcome variables (i.e., implant apex to mental foramen, buccal axial section, and lingual axial section) between the thermoplastic and the 3D-printed implant positions.
The mean ± standard deviations (SD) of the implant relation to mental foramen in the 3-D Printed guides were 3.12±0.36 mm, respectively. On the other hand, the mean and SD of thermoplastic guides were 2.52±0.83 mm. The deviation at the apex of the implant of the 3D-printed guides was 0.92±0.14 mm and 1.57±0.45 mm for the thermoplastic guides. For the implant, angular deviation of the 3D-printed guides was 3.33±0.86o and 4.03±1.20o for the thermoplastic guides, respectively.
Table 1. Mental Foramen Distance, Apex Deviation Distance. Head Deviation Degree.
| T-Test | |||||
| Group Statistics | |||||
| Method | N | Mean | SD | p-value | |
| Mental Foramen Distance | Thermoplastic Guide | 15 | 2.52 mm | 0.83 | .0.019 |
| 3D Guide | 15 | 3.12 mm | 0.36 | ||
| Apex Deviation | Thermoplastic Guide | 15 | 1.57 mm | 0.45 | 0.000 |
| 3D Guide | 15 | 0.92 mm | 0.14 | ||
| Head Deviation | Thermoplastic Guide | 15 | 4.03o | 1.20 | 0.076 |
| 3D Guide | 15 | 3.33o | 0.86 | ||
Figure 2: Surgical guide comparison. (Length). Implant apex to mental foramen (Buccal). Buccal axial section, (Lingual), Lingual axial section.
The computer-assisted surgical guide combines the computer 3D-image, which helps identify the anatomical structures of the bone, together with the prosthetic information, in order to find the ideal region to place the implant and to minimize the damage to vital structures. The results of this study showed that; the mean distance for the implant placed using the thermoplastic surgical guide is 2.5±0.83 mm; in contrast, the 3D-printed guide showed a 3.12± 0.36 mm. This difference was highly significant and constant for the 3D-printed guides. This indicates that the 3D-printed guides are more accurate and safe to be used in areas with vital structures. This is in agreement with the findings of a group of researchers who suggested that laboratory-fabricated surgical guides using CBCT data may be reliable in implant placement under prosthodontic considerations in partial edentulism (Behneke et al., 2012)
The deviation at the apex of the 3D-printed guides was 0.92 mm and 1.57 mm for the thermoplastic guides. This in consistent with Bell et al. (2018), who found that thermoplastic showed a difference between 3D-printed guides (0.76 mm) and thermoplastic guides (1.60 mm). In addition, Abduo & Lau (2020) reported 0.71 mm apex deviation for 3D-printed guides, while pilot-guides had 1.14 mm.For the angular deviation of the 3D-printed guides were 3.33o and 4.03o for the thermoplastic guides, respectively. This in agreement with Bell et al. (2018), who reported a deviation of 2.36o for 3D-printed guides and 3.40o thermoplastic guides. Recently Abduo & Lau (2020) found that fully guided had 2.42o deviation while pilot-guided had 4.65o deviation.
CONCLUSION
Based on this study, the 3D printed guides were more accurate than the TP guides in terms of implant placement accuracy in relation to an important landmark and 3D implant placement.
Disclousre: This is study is registered at the Research Center of College of Dentistry King Saud University with registration number CDRC IR 0318. The authors claim to have no financial interests, either directly or indirectly, in the products or information listed in the article.
REFERENCES
Abdou J, Lau D (2020). Accuracy of Static Computer-Assisted Implant Placement in Anterior and Posterior Sites by Clinicans New to Implant Dentistry: In Vitro Comarison of Fully Guided, Pilot-Guided, and Freehand Protocols. Int J Implant Dent 6(10): 10
Behneke A, Burwinkel M, Knierim K, Behneke N (2012). Accuracy assessment of cone beam computed tomography‐derived laboratory(‐based surgical templates on partially edentulous patients. Clinical Oral Implants Research, 23, 137-143.
Buser D, Janner SF, Wittneben JG, Bragger U, Ramseier CA, Salvi GE (2012). 10-year survival and success rates of 511 titanium implants with a sandblasted and acid-etched surface: a retrospective study in 303 partially edentulous patients. Clin Implant Dent Relat Res, 14, 839-51.
Bell CK, Sahl EF, Kim YJ, Rice DD (2018). Accuracy of Implants Placed with surgical guides: thermoplastic versus 3D-printed. Int J Periodontics Restorative Dent, 38(1): 113-119.
Chen LC, Lundgren T, Hallstrom H, Cherel F (2008). Comparison of different methods of assessing alveolar ridge dimensions prior to dental implant placement. J Periodontol 79: 401-5.
Joo HS, Park SW, Yun KD, Lim HP (2016). Complete-mouth rehabilitation using a 3D printing technique and the CAD/CAM double scanning method: A clinical report. J Prosthet Dent 116: 3-7.
Kim CM, Kim SR, Kim JH, Kim HY, Kim WC. (2016a). Trueness of milled prostheses according to number of ball-end mill burs. J Prosthet Dent 115: 624-9.
Kim DY, Jeon JH, Kim JH, Kim H, Kim WC (2017a). Reproducibility of different arrangement of resin copings by dental microstereolithography: Evaluating the marginal discrepancy of resin copings. J Prosthet Dent 117: 260-265.
Kim DY, Kim CM, Kim JH. 2017b. Evaluation of marginal and internal gaps of Ni-Cr and Co-Cr alloy copings manufactured by microstereolithography. J Prosthet Dent 9: 176-181.
Kim DY, Kim JH, Kim HY, Kim WC (2018). Comparison and evaluation of marginal and internal gaps in cobalt-chromium alloy copings fabricated using subtractive and additive manufacturing. J Prosthodont Res 62: 56-64.
Kim J-E, Kim N-H, Park J-H, Shim J-S (2016b). A procedure for the computer-guided implant planning: A narrative review. The Journal of the Korean Dental Association 54: 108-122.
Kuhl S, Zurcher S, Mahid T, Muller-Gerbl M, Filippi A, Cattin P (2013). Accuracy of full guided vs. Half-guided implant surgery. Clin Oral Implants Res 24: 763-9.
Lee IH, Cho D-W (2003). Micro-stereolithography photopolymer solidification patterns for various laser beam exposure conditions. The International Journal of Advanced Manufacturing Technology 22: 410-416.
Misch, CE (2004). Dental Implant Prosthetics-E-Book, Elsevier Health Sciences.
Nickenig HJ, Eitner S (2007). Reliability of implant placement after virtual planning of implant positions using cone beam CT data and surgical (guide) templates. J Craniomaxillofac Surg 35: 207-11.
Ortorp A, Jonsson D, Mouhsen A, VULT VON STEYERN P (2011). The fit of cobalt-chromium three-unit fixed dental prostheses fabricated with four different techniques: a comparative in vitro study. Dent Mater 27: 356-63.
Schneider D, Marquardt P, Zwahlen M, Jung RE. (2009). A systematic review on the accuracy and the clinical outcome of computer-guided template-based implant dentistry. Clin Oral Implants Res (20) Suppl 4: 73-86.