1Institute of Human Genetics, University of Jammu-180006.
2Department of Zoology, University of Jammu-180006.
Corresponding author email: Panjaliya82@gmail.com
Article Publishing History
Received: 09/04/2020
Accepted After Revision: 25/05/2020
Methylenetetrahydrofolate reductase (MTHFR) enzyme is one of the chief players in metabolism of circulating forms of Hcy. Any variation in the MTHFR gene can affect MTHFR enzymatic activity and is associated with serious cardiovascular profile like Myocardial Infarction (MI). The present study is designed to evaluate the association of MTHFR (C677T and G1793A) gene polymorphisms with MI in Jammu region. For the study purpose a total of 109 individuals were recruited (49 cases with MI and 60 unrelated healthy controls). Genotyping was done by PCR-RFLP technique and further data was statistically analysed. The frequencies of variant MTHFR alleles were higher in patient group than in controls (677T=12.24% vs 1.67% and 1793A=16.33% vs 15%). Logistic regression analyses have shown that MTHFR C677T polymorphism was significantly associated with the development of MI whereas MTHFR G1793A polymorphism was not associated with the disease in our study population. The haplotype T-G was giving approximately 8.23-fold risk [OR=8.23 (1.79-37.74), p=0.001] and C-G is conferring 2 folds protection [OR=0.5 (0.26-0.96), p=0.03] towards MI outcome. Based on measure of linkage disequilibrium (LD), the two MTHFR variants (C677T & G1793A) were in complete LD (D’=1, r2=0.02) in patients and in controls (D’=0.99, r2=0). The obtained data proved the association of MTHFR polymorphisms with the progression of MI severity in the population of Jammu region of the J&K State. Although a study comprising of large sample size is required to reach on a final conclusion.
C677t, G1793a, Mi, Mthfr, Polymorphism
Raina J. K, Fotra R, Kumar P, Panjaliya R. K. Methylenetetrahydrofolate Reductase Gene Polymorphisms and Risk of Myocardial Infarction. Biosc.Biotech.Res.Comm. 2020;13(2).
Raina J. K, Fotra R, Kumar P, Panjaliya R. K. Methylenetetrahydrofolate Reductase Gene Polymorphisms and Risk of Myocardial Infarction. Biosc.Biotech.Res.Comm. 2020;13(2). Available from: https://bit.ly/30s7ItN
Copyright © Raina et al., This is an open access article distributed under the terms of the Creative Commons Attribution License (CC-BY) https://creativecommns.org/licenses/by/4.0/, which permits unrestricted use distribution and reproduction in any medium, provide the original author and source are credited.
INTRODUCTION
Recent progresses in the field of genetics and genomics have provided substantial benefits to clinical medicine including facilitation of characterization of disease pathogenesis and diagnosis. Genetics has offered effective approaches to the identification of complex diseases like Myocardial Infarction (MI). It is an important clinical problem because of its large contribution to mortality. MI is multifactorial in origin and involves interplay of various environmental exposures viz. smoking, sedentary lifestyle, altered blood lipid levels, obesity, family history, hypertension and genetic profile. All these exposures in concert are responsible for the commencement of immuno-inflammatory cascade leading to endothelial damage, atherosclerosis, thrombus formation, blockage of arteries and finally event of MI. Elevated circulating levels of homocysteine (Hcy) is a well known predictor for complex cardiovascular phenotypes such as MI (Kaur et al., 2016; Raina et al., 2016a).
Homocysteine [COOH-CH(CH2CH2SH)-NH3] is a homologue of the amino acid cysteine and is synthesised in the body from dietary methionine. Methylenetetrahydrofolate reductase (MTHFR) is a folate and vitamin B12-dependent enzyme which is involved in conversion of Hcy back to methionine. Thus, maintaining plasma Hcy levels (Iqbal et al., 2011). There are two well characterised single nucleotide polymorphisms (SNP) at MTHFR locus viz. C to T transition at nucleotide position 677 in exon 4(rs1801133) and G to A transition at nucleotide position 1793 in exon 11 (rs2274976) which have been identified for bringing up alteration in MTHFR enzyme activity and disturbance in Hcy metabolism (Frosst et al., 1995; Raddy et al., 2002). These polymorphisms are associated with reduced MTHFR enzyme activity by about 70% and 40% in homozygotes and heterogzygotes, respectively (Mao et al., 2008; Kour et al. 2016b Jakó and Sinkó (2017).
Previous reports on MTHFR gene polymorphisms have shown that the said gene is significantly associated with CVD in Jammu region (Raina et al., 2016a; Raina et al., 2016b) but the polymorphisms have not been studied in MI so far. Hence, in the present investigation we have evaluated the association of MTHFR C677T and MTHFR G1793A gene polymorphisms with MI in population of Jammu region (J&K).
MATERIALS AND METHODS
Study population and Ethical Approval: A total of 109 individuals, 49 patients with MI and 60 healthy unrelated, control individuals were recruited for the present study. The patients were enrolled from the Department of Cardiology, ASCOMS, Sidhara, Jammu (J&K) and from private clinics. Sampling for controls was done from University premises. Physically healthy individuals with no history of CAD, hypertension, diabetes, thyroid problem, any form of cancer and other major medical conditions were included as controls. The present study design was approved by institutional Ethical Committee, University of Jammu. A brief health questionnaire covering different parameters such as gender, height, weight, smoking and physical inactivity, along with a consent form was duly filled by every subject enrolled for study. Diagnosis of MI was based on WHO criteria which included clinical history, ECG changes indicating myocardial damage and elevation of biochemical markers (Report of the Joint International Society and Federation of Cardiology, 1979).
Genotyping of MTHFR gene polymorphisms: Genotyping of MTHFR C677T and MTHFR G1793A polymorphisms was performed by polymerase chain reaction-restriction fragment length polymorphism (PCR-RFLP) as described previously (Raina et al., 2016b; Raddy et al., 2002).
Statistical analysis: Statistical analysis was carried out by using SPSS (Chicago, IL, USA) software version 21. Clinical characteristics of all the subjects were expressed as mean ± SD. Allelic frequencies were calculated by the gene-counting method. Hardy-Weinberg equilibrium (HWE) and the genotypic as well as allelic distribution of the C677T polymorphism of MTHFR gene was analyzed using Pearson’s goodness of fit chi-square (χ2) test. The odd-ratios (OR) for MTHFR polymorphisms were calculated with 95% confidence interval (CI) under different genetic models. SHEsis software (Shi and He, 2005) was used to calculate the haplotype frequencies and Linkage disequilibrium (LD) pattern. A p-value of <0.05 was considered as statistically significant.
RESULTS AND DISCUSSION
These 49 cases of MI were further categorised into different subtypes according to ECG patterns and location of infarct. It was found that the inferior wall myocardial infarction (IWMI) was prominent type of heart attack occurring in 21 patients followed by ST- Elevation Myocardial Infarction (STEMI) in 13 patients, Anterior Wall Myocardial Infarction (AWMI) in 10 patients and Non-ST Elevation Myocardial Infarction (NSTEMI) in 5 patients only. The percentage distribution of both MTHFR C677T and MTHFR G1793A polymorphisms are summarised in Table 1. It was observed from the data that the wild CC genotype was the most prevalent one followed by heterozygous GA genotype and then the variant homozygous AA genotype. There was a considerable increase in CT genotype in patient group in judgement to controls (20.41% vs 3.33%). The prevalence of TT-genotype was higher in MI patients (2.04%) whereas there was complete absence of variant genotype in healthy controls. Overall, the frequency of variant T-allele was significantly higher in patients i.e. 12.24% than in controls i.e. 1.67%.
Table 1: Showing genotypic and allelic distribution of MTHFR gene polymorphisms in study participants.
| Genotypes/ alleles/ | MI Cases | Controls
(N=60) |
||||
| MTHFR C677T | IWMI
(n=21) |
AWMI
(n=10) |
STEMI
(n=13) |
NSTEMI
(n=5) |
Total
(N=49) |
|
| CC | 16 (76.19%) | 7 (70%) | 11 (84.62%) | 4 (80%) | 38 (77.55%) | 58 (96.67%) |
| CT | 4 (19.05%) | 3 (30%) | 2 (15.38%) | 1 (20%) | 10 (20.41%) | 2 (3.33%) |
| TT | 1 (4.76%) | 0 | 0 | 0 | 1 (2.04%) | 0 |
| C | 36 (85.71%) | 17 (85%) | 24 (92.31%) | 9 (90%) | 86 (87.76%) | 118 (98.33%) |
| T | 6 (14.29%) | 3 (15%) | 2 (7.69%) | 1 (10%) | 12 (12.24%) | 2 (1.67%) |
| MTHFR G1793A | ||||||
| GG | 15 (71.43%) | 7 (70%) | 9 (69.23%) | 4 (80%) | 35 (71.43%) | 42 (70%) |
| GA | 5 (23.81%) | 2 (20%) | 4 (30.77%) | 1 (20%) | 12 (24.49%) | 18 (30%) |
| AA | 1 (4.76%) | 1 (10%) | 0 | 0 | 2 (4.08%) | 0 |
| G | 35 (83.33%) | 16 (80%) | 22 (84.62%) | 9 (90%) | 82 (83.67%) | 102 (85%) |
| A | 7 (16.67%) | 4 (20%) | 4 (15.38%) | 1 (10%) | 16 (16.33%) | 18 (15%) |
The prevalence of genotypes/ alleles were also studied in different MI categories and it was observed that risk allele (T) was highly prevalent in IWMI patients (14.49%) followed by AWMI (15%), NSTEMI (10%) and then, STEMI (7.69%). As regards of MTHFR G1793A polymorphism, the genotype distribution pattern in both MI patients and control individuals showed that the percentage of wild GG- genotype was higher (71.43% vs 70% respectively) in comparison to heterozygous GA-genotype (24.49% vs 30%% respectively) and risk AA-genotype (4.08% vs 0% respectively). Additionally, the allele percentage of the variant A- allele in MI patients was almost comparable with the control group (16.33% vs 15% respectively). The order of prevalence of A-allele in different MI subtypes was as follows: AWMI (20%), IWMI (16.67%), STEMI (15.38%) and NSTEMI (10%). The observed frequencies of MTHFR polymorphisms were in concordance with HWE in both study groups.
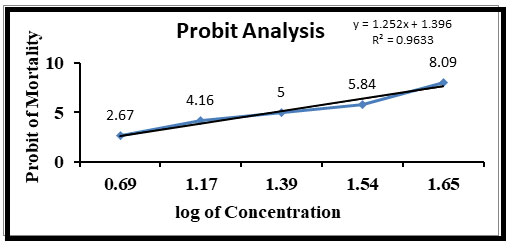
The association of MTHFR gene polymorphisms with risk of MI can be obtained by calculating Odds Ratio (OR) [Table-2 and 3]. For MTHFR C677T polymorphism, there was a significant difference in frequencies of CC vs. CT genotypes between the MI patients and healthy controls (OR=7.63 (1.58-36.76); p=0.004). OR for C vs. T allele showed that the ‘T’ allele was conferring approximately 8.23-folds risk, which was statistically significant for the development of MI in our study population. In context to MTHFR G1793A SNP, none of the applied genetic models were associated with risk of MI occurrence. Allocation of haplotype frequencies of MTHFR C677T and G1793A polymorphism among MI cases and healthy controls is given in Table 4. The haplotype T-G was giving approximately 8.23-fold risk [OR=8.23 (1.79-37.74), p=0.001] and C-G is conferring 2-folds protection [OR=0.5 (0.26-0.96), p=0.03] towards MI outcome. Based on measure of linkage disequilibrium (LD), the two MTHFR variants (C677T & G1793A) were in complete LD (D’=1, r2=0.02) in patients and in controls (D’=0.99, r2=0) (figure).
Table 2: Showing Logistic regression analysis for MTHFR (C677T) polymorphism.
| Genetic Model | Genotypes/
Alleles |
MI (N=49) | Controls (N=60) | OR (95% CI) | p-value |
| Co-dominant | CC | 38 | 58 | 1 (Reference) | |
| CT | 10 | 2 | 7.63 (1.58-36.76) | 0.004 | |
| TT | 1 | 0 | Not possible† | – | |
| Dominant | CT+TT | 11 | 2 | Not possible† | – |
| CC | 38 | 58 | 1 (Reference) | ||
| Recessive | TT | 1 | 0 | Not possible† | – |
| CT+CC | 48 | 60 | 1 (Reference) | – | |
| Allelic | C | 86 | 118 | 1 (Reference) | |
| T | 12 | 2 | 8.23 (1.79-37.73) | 0.001 |
†Some genotype combinations were not observed, so it was not possible to calculate odds ratio.
Table 3: Showing Logistic regression analysis for MTHFR (G1793A) polymorphism.
| Genetic Model | Genotypes/
Alleles |
MI cases (n=49) | Controls (n=60) | OR (95% CI) | p-value |
| Co-dominant | GG | 35 | 42 | 1 (Reference) | |
| GA | 12 | 18 | 0.80 (0.34-1.89) | 0.6 | |
| AA | 2 | 0 | Not possible† | – | |
| Dominant | GA+AA | 14 | 18 | Not possible† | – |
| GG | 35 | 42 | 1 (Reference) | ||
| Recessive | AA | 2 | 0 | Not possible† | – |
| GA+GG | 47 | 60 | 1 (Reference) | ||
| Allelic | G | 82 | 102 | 1 (Reference) | |
| A | 16 | 18 | 1.11 (0.53-2.30) | 0.8 |
†Some genotype combinations were not observed, so it was not possible to calculate odds ratio.
Table 4: Association of MTHFR haplotypes with risk of MI.
| Variant MTHFR C677T/ G1793A | MI Cases (N=49) | Controls (n=60) | OR (95% CI) | p-value |
| C-A | 0.163 | 0.15 | 1.10 [0.53-2.30] | 0.8 |
| C-G | 0.714 | 0.833 | 0.5 [0.26-0.96] | 0.03 |
| T-G | 0.122 | 0.016 | 8.23 [1.79-37.74] | 0.001 |
The general characteristics of the study participants are presented in Table-5. The controls were slightly elder than patients, with a mean age of 48.91 years compared to 46.75 years in the patient group. BMI was significantly higher in patients with a mean value of 23.65±4.58 than in controls with mean value of 22.93±4.09, howsoever the values did not reach a statistical significance (p=0.4). The physiometric characteristics viz. systolic blood pressure (SBP), diastolic blood pressure (DBP) and pulse pressure (PP) were higher in patients in comparison to controls in a significant manner (p<0.0001). In patient group, 53.06% cases were smokers whereas; among controls only 25% were involved in habit of tobacco smoking. OR analysis revealed that smoking was adding nearly 3.39 folds risk to the progression of MI in our population [OR = 3.39 (1.51–7.62); p = 0.003]. Majority of patients as well as controls were living a sedentary lifestyle and hence, lack of association was reported with this parameter.
Table 5: Showing general characteristics of the study participants
| Variables | MI cases (N=49) | Controls (N=60) | OR (95% CI) | p-value |
| Age (yrs.) | 46.75±6.7 | 48.91±7.4 | – | 0.1 |
| Sex
Males Females |
40 (81.63%)
9 (18.37%) |
36 (60%)
24 (40%) |
–
– |
–
– |
| Blood pressure (mmHg)
SBP DBP |
143.33±20.81
87.51±10.44 |
123.05±8.23
80.55±4.65 |
–
– |
<0.0001
<0.0001 |
| Pulse pressure | 55.82±16.74 | 42.50±5.74 | – | <0.0001 |
| BMI | 23.65±4.58 | 22.93±4.09 | – | 0.4 |
| Smoking
Y N |
26 (53.06%)
23 (46.94%) |
15 (25%)
45 (75%) |
3.39 (1.51-7.62)
Ref. (1) |
0.003 |
| Sedentary lifestyle
Y N |
23 (46.94%)
26 (53.06%) |
35 (58.33%)
25 (41.67%) |
0.64 (0.30-1.35)
Ref. (1) |
0.2 |
Figure 1
The incidence of MI in India is relatively higher being 64.37/1000 people (Rao et al., 2014). The disease etiology involves dual interaction of environmental and genetic factors. Homocysteine is a sulphur containing amino acid made from a common dietary amino acid, methionine that inflicts damage to the inner arterial lining and contributes to coronary heart disease and event of MI in longer duration. Henceforth, genes controlling Hcy metabolism are considered as an emerging candidates for progression of MI. With this background the present research work was aimed to study MTHFR (C677T and G1793A) gene polymorphisms with the risk of MI in population of Jammu region. A high prevalence of CC genotype was reported in the present study in comparison to CT and TT genotypes. In fact, a complete absence of TT genotype was observed in MI subtypes including AWMI, STEMI and NSTEMI as well as in healthy controls. Raina and researchers (2106a and 2016b) have also reported extremely higher frequency of CC genotype and lower prevalence of TT genotype in cardiovascular diseases in Jammu region. The results are consistent with other studies done by Markan et al., 2007; Lakshmi et al., 2011; Iqbal et al. 2011; Matam et al., 2014; Ezzat et al. (2014).
The MTHFR 677T-allele was having a significant role in the aetiology MI in our population (C vs T: OR=8. 23, p= 0.001). Gülec et al. (2001); Ezzat et al. (2014), Shaker et al. (2014) and Grek et al. (2015) were also in agreement of association of this polymorphism in onset of MI. Contrary to these observations, there were reports on lack of association of MTHFR C677T polymorphism with increased risk for MI in different population groups (Angeline et al., 2007; Iqbal et al., 2011; Verdoia et al., 2014; Iqbal et al. 2016).
Rady et al. (2002) reported a functional polymorphism (G1793A) in exon 11 of MTHFR gene that results in an arginine to glutamine substitution at codon 594 (R594Q) and is associated with coronary heart diseases. There is scarcity of data establishing a connection of MTHFR (G1793A) genotypes and MI. In the present study it was observed that the prevalence of wild (GG) genotype was higher in MI patients than in controls whereas heterozygous (GA) genotype frequency was lower in patient group when compared to healthy controls. The prevalence of variant (AA) genotype was also low in study population and controls were found to be devoid of AA genotype completely. Among different MI subtypes, variant genotype was present only in IWMI and AWMI. In view of GG-genotype,
Rady and co-associates (2002) also reported a lower prevalence of GA and AA- genotypes in their study populations. The results of our study demonstrated that the MTHFR (G1793A) was not in association with the development of MI. This is consistent with previous studies which have shown lack of MTHFR G1793A polymorphism with cardiovascular diseases (Kebert et al., 2006; Trifonova et al., 2012; Neto et al., 2013).Haplotype analysis was also performed and it has been observed that the haplotype combination T-G was giving approximately 8.23-fold risk whereas C-G was providing 2 folds protection towards MI outcome in population of Jammu region.
CONCLUSION
The results suggested that MTHFR gene is an informative candidate which can be used as a potential diagnostic marker for MI. Thus, further studies are necessary to ascertain the relationship between MTHFR variants and MI.
REFERENCES
Angeline T., Jeyaraj N., Tsongalis G.J. (2007). MTHFR Gene polymorphisms, B-vitamins and hyperhomocystinemia in young and middle-aged acute myocardial infarction patients. Exp Mol Pathol, 82, 227-33.
Ezzat H., Attia F.A., Mokhtar A., et al. (2014). Prevalence of thrombophilic gene polymorphisms (FVL G1691A and MTHFR C677T) in patients with myocardial infarction. The Egyptian Journal of Medical Human Genetics, 15, 113–123.
Frosst P., Blom H. J., Milos R., et al. (1995). A candidate genetic risk factor for vascular disease: A common mutation in methylenetetrahydrofolate reductase. Nat Genet, 10, 111-3.
Grek A.V., Prystupa L.N., Sytnik T.V. (2015). Plasma homocysteine level and C677T polymorphism in MTHFR gene in patients with acute coronary syndrome. J Biomed Clin Res, 8, 46-51.
Gülec S., Aras O., Akar E., et al. (2001). Methylene tetrahydrofolate reductase gene polymorphism and risk of premature myocardial infarction. Clin Cardiol, 24, 281–4.
Iqbal M.P, Iqbal K., Tareen A.K., et al. (2016). Polymorphisms in MTHFR, MS and CBS genes and premature acute myocardial infarction in a Pakistani population. Pak J Pharm Sci, 29, 1901-1906.
Iqbal M.P., Mahmood S., Parveen S., Mehboobali N., Haider G. (2011). Polymorphisms in methylenetetrahydrofolate reductase gene are not associated with acute myocardial infarction in a Pakistani population. Pak J Biochem Mol Bio, 44, 32-35.
Jakó B., Sinkó J. (2017). Role of the Methylene Tetrahydrofolate Reductase (MTHFR) Gene Mutation in Acute Myocardial Infarction. Journal of Cardiovascular Emergencies, 3, 41-43.
Kaur R., Das R., Ahluwalia J., Kumar R.M., Talwar K.K. (2016). Genetic polymorphisms, biochemical factors, and conventional risk factors in young and elderly North Indian patients with acute myocardial infarction. Clinical and Applied Thrombosis/Hemostasis, 22, 178-183.
Kebert C.B., Eichner J.E., Moore W.E., et al. (2006). Relationship of the 1793G-A and 677C-T polymorphisms of the 5,10-methylenetetrahydrofolate reductase gene to coronary artery disease. Disease Markers, 22, 293-301.
Lakshmi S.V.V., Naushad S.M., Rupasree Y., et al. (2011). Interactions of 5’ UTR Thymidylate Synthase polymorphism with 677 C/T Methylene Tetrahydrofolate Reductase and 66 A/G Methyltetrahydrofolate Homocysteine Methyl- Transferase Reductase polymorphisms determine susceptibility to coronary artery disease. Journal of Atherosclerosis and Thrombosis, 18, 56-64.
Mao R., Fan Y., Chen F., Fu S. (2008). Genetic polymorphism of MTHFR G1793A in Chinese populations. Eur J Epidemiol, 23, 363-8.
Markan S., Sachdeva M., Sehrawat B. S., et al. (2007). MTHFR 677 CT/MTHFR 1298 CC genotypes are associated with increased risk of hypertension in Indians. Mol Cell Biochem, 302, 125-31.
Matam K., Khan I.A., Hasan Q., Rao P. (2014). Coronary artery disease and the frequencies of MTHFR and PON1 gene polymorphism studies in a varied population of Hyderabad, Telangana region in south India. Journal of King Saud University – Science, http://dx.doi.org/10.1016/j. jksus.2014.09.002.
Neto A.I.M., de Moura Júnior J.R., Persuhn D.C. (2013). Frequency of MTHFR G1793A polymorphism in individuals with early coronary artery disease: cross-sectional study. Sao Paulo Med J, 131, 296-300.
Rady P.L., Szucs S., Grady J., et al. (2002). Genetic polymorphisms of methylenetetrahydrofolate reductase (MTHFR) and methionine synthase reductase (MTRR) in ethnic populations in Texas; a report of a novel MTHFR polymorphic site, 1793G>A. Am J Med Genet, 107, 162-168.
Raina J.K., Panjaliya R.K., Sharma M., et al. (2016b). Methylenetetrahydrofolate reductase C677T gene polymorphism and predisposition to essential hypertension. International Journal of Genetics, 8, 207-210.
Raina J.K., Sharma M., Panjaliya R.K., et al. (2016a). Methylenetetrahydrofolate reductase C677T and methionine synthase A2756G gene polymorphisms and associated risk of cardiovascular diseases: A study from Jammu region. Indian Heart Journal, 168, 421-430.
Rao V., Rao P., Carvalho N. (2014). Risk Factors for Acute Myocardial Infarction in Coastal Region of India: A Case–Control Study. Heart India, 2, 70-75.
Report of the Joint International Society and Federation of Cardiology/World Health Organization task force on standardization of clinical nomenclature. Nomenclature and criteria for diagnosis of ischemic heart disease (1979). Circulation, 59, 607-609.
Shaker O.G., Ismail M.F. (2014). Association of genetic variants of MTHFR, ENPP1, and ADIPOQ with myocardial infarction in Egyptian patients. Cell Biochem Biophys, 69, 265-74.
Shi Y.Y., He L. (2005). SHE sis, a powerful software platform for analyses of linkage disequilibrium, haplotype construction, and genetic association at polymorphism loci. Cell Res, 15, 97-98.
Trifonova E.A., Spiridonova M.G., Gabidulina T.V., et al. (2012). Analysis of the MTHFR gene linkage disequilibrium structure and association of polymorphic gene variants with coronary atherosclerosis. Russian Journal of Genetics, 48, 1035–1047.
Verdoia M., Schaffer A., Cassetti E., et al. (2014). Atherosclerosis Study Group (NAS). MTHFR polymorphism and risk of periprocedural myocardial infarction after coronary stenting. Nutr Metab Cardiovasc Dis, 24, 532-7.