Department of Biotechnology, University Institute of Engineering and Technology. Kurukshetra University, Kurukshetra, Haryana, India
Corresponding author Email: rkumar2015@kuk.ac.in
Article Publishing History
Received: 16/03/2018
Accepted After Revision: 01/06/2018
Alzheimer’s disease (AD) is a chronic, advancing malady associated with loss of memory or cognition. It is the noted causes of lethality worldwide, there are no such drugs which can cure AD till date and are ineffective in the later stages. Such known drugs only ease the symptoms but do not prevent the onset or progression of the AD. Alzheimer’s is caused by the aggregation of the hyperphosphorylated tau which is one of the common characteristics of the neurodegenerative disorder. There are a number of kinases which hosts the excessive phosphorylation of tau protein. One of the kinase extensively targeted in the AD is GSK-3â (Glycogen Synthase Kinase-3â). As indicated by many studies that by applying appropriate docking methods, a number of phyto compounds have shown enhanced target selectivity than the conventional Alzheimer’s drugs. This review summarizes the known drug targets in the AD, their conventional inhibitors and also the comparison between the current and future AD therapy based on their binding affinities. As a result, large libraries of compounds with inhibitory effect can be screened. It was also studied that Withanolide-A has the potential to be the future drug for Alzheimer’s disease.
Docking; Drugs; Phosphorylation; Tau Protein; Withanolide-A
Joshi A, Sharma A, Kumar R. Docking of GSK-3® With Novel inhibitors, a Target Protein Involved in Alzheimer’s Disease. Biosc.Biotech.Res.Comm. 2018;11(2).
Joshi A, Sharma A, Kumar R. Docking of GSK-3® With Novel inhibitors, a Target Protein Involved in Alzheimer’s Disease. Biosc.Biotech.Res.Comm. 2018;11(2). Available from: https://bit.ly/2MnZVXx
Introduction
Alzheimer’s is a type of dementia associated with memory loss and other intellective abilities, severe enough to intrude with regular routine. Alzheimer’s disease report for 60 to 80 percent of dementia and the present Alzheimer’s disease therapies impaired from in proficient effects on its symptoms such as perception notably in the subsequent stages of the disease (http://www.alz.org). According to the report prepared by Alzheimer’s and related disorders society of India in 2010, there are 3.7 million Indians suffering with dementia while the numbers are anticipated to bifold by 2030. The number of factors is thought to increase the progression of this disease, some of which are; increasing age, family history, previous severe head injuries etc. Over the past decade, much of the research on Alzheimer disease (AD) has focused on radical-effected oxidative stress and its importance in disease pathogenesis. Oxidative stress increases amyloid beta deposits in the brain which results in the synthesis of neurotoxic aggregates. The net effect of oxygen radicals is damaging as it may lead to neuronal cell death and contribute to AD (Smith et al. 1998). Flavonoids also possess antioxidant activity and they regulate the redox status and prevent damage caused by oxidative stress. Protein Kinases are recognised as encouraging target structures considering their involvement in AD breakthrough pathways like pathophysiological tau protein phosphorylation and amyloid beta toxicity. The sound interdependence of tau phosphorylation and pathology has led to the search for Tau protein kinase inhibitors such as GSK3-â and Tyrosine kinase Fyn, which phosphorylates tau and also plays a causative role in amyloid pathway. Hereafter, acting as potential therapeutic agents (Medina, 2018).
Role Of Flavonoids In The Treatment Of Ad
Nature has fascinated us with a lot of natural remedies in the form of fruits, leaves, bark, vegetables, and nuts, etc. The wide varieties of biologically active nutrients existing in these natural products play a vital role in defence and aid of various neurodegenerative diseases. Flavonoids are an array of non-nutrient polyphenolic compounds readily procured from plants. It was realized that the competence of flavonoids to upgrade neurological health was resolved by their antioxidant capability. Flavonoids are endowed with numerous biological activities like anti-inflammatory, anticoagulant, anti-cancer, anti-oxidants, and anti-spasmodic. There is an extensive role of flavonoids and even their metabolites in different signaling pathways by altering the phosphorylation state of target protein put forward their therapeutic potential and beneficial in neurodegeneration(Spencer, 2007). Increasing evidence shows their ability to improve brain function such as memory and learning by interacting with cellular as well as molecular components of the brain resulting in enhanced neuronal function and induce neurogenesis (Spencer, 2010; Baptista et al. 2014).
A study has found the role of plant-derived compounds such as myricetin and epicatechin-5-gallate in abrogating heparin-induced cluster of tau into filaments (Taniguchi et al. 2004). In drug discovery, the dominant secondary metabolites (terpenoids, phenolics, and alkaloids) are of probable remedial relevance. Certain flavonoids such as indirubin and morin are capable of the inhibiting the activity of GSK-3 beta and thereby blocking tau hyperphosphorylation. Kinases are involved in tau phosphorylation and phosphatases reverse this action. Thus, flavonoids also portray a crucial aspect in modulating the activity of phosphatases (Baptista et al. 2014). Genistein (phytoestrogen), a beneficial intermediary for the treatment of AD as it imitates estrogen which is involved in the development of memory and learning along with its neuroprotective activities, (Hussain et al. 2018). It was found that eicosanoyl-5-hydroxytryptamide (EHT), a naturally ocurring component of coffee beans accelerates the activity of serine/threonine protein phosphatase, PP2A and thus provide therapeutic benefits associated with AD (Asam et al. 2017).
Molecular Causes Of Ad
The key events that lead to AD : Beta-amyloid toxicity. The brain of a patient with the AD is characterized by amyloid toxicity. Amyloid beta denotes peptides of 36-43 amino acids long processed from an amyloid precursor protein (APP) which is digested by beta secretase and gamma secretase to yield amyloid beta (A â). This peptide is found in brains of patients suffering from Alzheimer’s (Murphy et al. 2010 Hamley, 2012, Sauer, 2017). Some processes include disruption of amyloid beta aggregates, alterations in the precursor of amyloid beta protein processing through the inhibition of beta-secretase. Thus, modulating the beta-secretase activity is the one suggested a therapeutic avenue to treat AD (Yin et al. 2007). Certain flavonoids may guard to counter the effect of Alzheimer’s disease by interrupting with the generation of beta-amyloid peptides into neurotoxic aggregates. It is a matter of contention that interfering with the activity of beta and gamma-secretase enzymes may disrupt their other functional roles besides playing an important part in amyloidogenic pathways.
Thus such interference using ã secretase can result in skin cancers and cognitive dysfunction (Kikuchi et al. 2017). The decades old theory which aims at implicating beta amyloid as the leading cause of Alzheimer’s has been questioned by a group of scientists. Researchers have tried and failed to prevent Alzheimer’s using drugs targeted at amyloid âprotein. Due to the lack of the utility of amyloid-â-aspired approach in Phase III clinical trials, it was prerequisite to conceive substitute drug discovery strategies for alzheimer’s (Folch et al. 2016). Solanezumab, a drug which acts on amyloid â protein failed some pivotal clinical trials. However, it is still anonymous whether the disease is caused by plaques or they are just the by- products (Ramsey, 2018).
A number of normal patients have been found with amyloid deposists in their brain. It was anticipated that amyloid beta deposition is an anomaly of aging and does not correlate with the AD progression(Kametani et al. 2018). Therefore there is a compulsive need to search policies directed at reducing misfolded tau protien which is one of the disease-causing agents (Bruden et al. 2010). Tau is liable to be the more superior target than the amyloid â as it coordinates efficiently with cognitive impairement, provided clinical symptoms are tangible (Congdon et al. 2018).
Tau Protein Hyperphosphorylation
For more than a decade, researchers have found ‘tau’ protein as one of the causes other than the Beta-amyloid plaques (Underwood, 2016). Accordingly, tau hyperphosphorylation and accumulation of insoluble aggregates is strongly related to reduce cognitive performance. Hence, we can affirm that tau is a reliable marker of the neurodegenerative process (Fig.1). Incorporation of phosphate groups into tau depends on; tau’s confirmation and equity amidst the activity of kinases and phosphatases (Kremer et al. 2011).
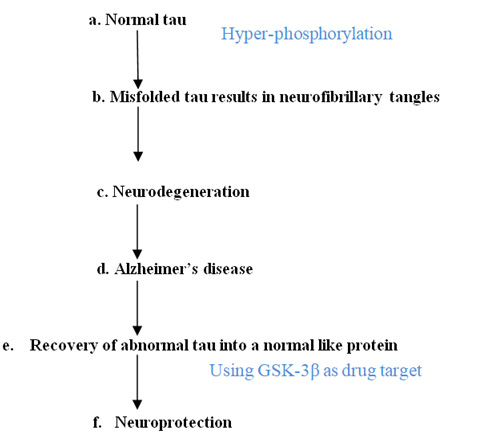 |
Figure 1: Events that are involved in tau mediated neurodegeneration |
Changes in tau confirmation could lead to excessive phosphorylation resulting in the formation of neurotoxic aggregates and tau-mediated neurodegeneration (Dixit et al. 2008). Tau is the member of family of proteins intricated in stabilizing the microtubules. They are common in neurons of Central Nervous System and also present at low levels in CNS astrocytes and oligodendrocytes (Shin et al.1991). The tau proteins have been formed as a result of alternate splicing of MAPT ( microtubule -associated protein tau) gene in humans and is positioned on chromosome 17 (Goedert et al.1989; Jesus et al. 2016).
The hydrophilic nature of the tau protein and its existence as intrinsically disordered protein was unfolded by many biophysical studies. (Porowska et al. 2014).One of the critical function of tau protein is to prevent the depolymerization of microtubules by regulating its stability in two ways: isoforms, and phosphorylation. On the basis of the number of binding domains, six variants of tau protein (352-441 amino acids and apparent molecular weight between 60-74kDa) exist in human brain tissue (Martin et al. 2011). Out of six modifications, three isoforms have 3 tubulin binding domains and other three have 4 tubulin binding domains in the C-terminal half of tau, (Guo et al. 2017).
The domain structure of tau is such that it’s positively charged binding domain is located in carboxy-terminal which binds to the microtubule which is negatively charged. Tau is a phosphoprotein (i.e. posttranslationally modified) with 79 probable Serine (Ser) and Threonine (Thr) phosphorylation sites on the extended tau isoform. It has been reported in a study that phosphorylation is possible in about 30 sites in a normal tau protein. PKN, a serine/threonine kinase is one such enzyme among the plethora of kinases which regulates the phosphorylation of tau (Billingsley et al. 1997). As revealed by primary sequence analysis, the tau molecule has three major domains: N-terminal (acidic), a proline-rich region, C-terminal domain (basic). These domains are characterized on the basis of their amino acid character and even on their microtubule interactions. Thus, tau protein acts as a dipole with two domains having the opposite charge (Kolarova et al. 2012; Porowska et al. 2014). Extreme phosphorylation of the tau protein proceeds to the formation of Paired helical fragments (PHF’s) due to the loss of affinity with microtubules and they bind with one another which further aggregates in neurofibrillary tangles via. Post-translational modifications. Thus, there is a strong correlation between abnormal phosphorylation and self-aggregation of tau (Guo et al. 2017)
When disorganized, this aside from being very soluble protein forms remarkably insoluble tangles or aggregates which commit to the number of neurodegenerative disorders. The mutations in posttranslational modifications are the main cause of this failure i.e. they form nonfunctional aggregates. One of the studies demonstrated that dephosphorylation of the hyperphosphorylated tau converts abnormal tau protein into a normal like protein which then regulates microtubule assembly(Iqbal et al. 2011). Therefore abrogating the abnormal tau and recovery of the microtubule organization are the most promising therapeutic interventions to combat AD.
Gsk-3 Beta As A Drug Target
GSK-3 is encoded by two genes: GSK-3â, located on chromosome 19 and GSK-3â, positioned on chromosome 2. GSK-3 is ubiquitously expressed in mammals as well as in yeast (Medina et al. 2011). GSK3 mediates the augmentation of phosphate molecules to serine and threonine amino acid residues and for this reason termed as serine/threonine protein kinase. The kinase domain of these 2 isoforms are highly homologous ((Stambolic et al. 1994) but are demarcated in the N- and C-terminal regions. GSK3â has a molecular mass of 46-47 kDa consisting of 433 and 420 amino acids in human and mouse respectively. The protein contains an N-terminal domain, a kinase domain, and a C-terminal domain. The substrate Binding domain (BD) provides GSK-3â specific binding sites for the tumor supressor p53 and other protein complexes (Atlas of Genetics and Cytogenetics in Oncology and Haematology). A number of protein kinases are involved in tau phosphorylation such as CdK5 (Cyclin-dependent Kinase 5), JNK (C-Jun amino-terminal Kinase), CK1 (Casein Kinase1), Dyrk1A, AMPK (Adenosine-monophosphate activated protein kinase), MARK5 (Microtubule affinity-regulating Kinases), PKA (Cyclic AMP-dependent protein Kinase), GSK-3â (Glycogen Synthase Kinase-3â) (Crews et al. 2010). But a study has shown that 31% of the therapeutically favorable phosphorylation sites of tau protein are phosphorylated by GSK3â (Martin et al. 2013).
The classical approach to treat misfolding of tau protein provides inhibition of protein kinases (Glycogen synthase kinase 3â) which hosts tau phosphorylation. According to the ‘GSK-3 hypothesis of AD’, tau hyperphosphorylation, memory impairment and enhanced â-amyloid production is due to the overexpression of GSK-3, all of which are characteristic features of the AD. If this hypothesis is consolidated then, inhibition of GSK-3â by novel inhibitors provides a better pathway against the effect of this destructing disorder (Hooper et al. 2008). There are two isoforms of GSK-3 gene; GSK-3 alpha and GSK-3â. GSK3â also exist as longer splice variants (Mukai et al. 2002; Schaffer et al. 2003). Moreover, GSK-3â results in a neuronal decline in the AD because of the fact that it is a causal mediator of apoptosis. Increased level of such protein eventuated in the autopsy evaluation of brain of alzheimer’s victims (Pei et al. 1997). It is also validated that a spatial and temporal pattern of enhanced GSK-3 expression corresponds with the evolvement of neurofibrillary tangles proceeding towards neurodegeneration (Leroy et al. 2002).
Molecular Docking
Drug research is an important tool in the field of medicine. Utility of computers to anticipate the efficiency of binding of a set of small molecules or ligands with the target is an important element of drug discovery and developmental process. There is an ample realm of software packages used to execute molecular docking such as Dock, Autodock, GOLD, ICM, Glide, AutoDock Vina, FlexX etc . Automated docking is generally used for prognosis of biomolecular complexes, in structure and function examination and in computer-aided drug designing. A dozen of mechanism is available, consolidating varied energy evaluation methods. Due to the enhanced docking speed, AutoDock 4.2 has been widely used for virtual screening. It is the ultimate current version which is based upon the Lamarckian genetic algorithm, a hybrid algorithm comprising of both the genetic as well as local search and is more enhanced and accurate than previous version AD3.0. Unlike AD3.0, Autodock 4.2.6 (henceforth AD4.2) and Auto Dock Vina 1.1.2 (henceforth AD Vina) have upgraded results and improved elucidation, (Collignon et al. 2011, Nataraj et al. 2017 and Alvarez et al. 2017).
Two main programs are involved in AutodockTools: Autodock for docking of the ligand within the set of grids (within the binding site) in the target protein and Autogrid for selection of grid parameters, size of the box, its location etc (http://autodock.scripps.edu/). It is particularly suitable for protein-ligand docking in which we presume the pose and orientation of a small molecule when it is articled to a protein receptor. It is used to select likely drug candidates. Typically, ligands are drug candidates and the macromolecule is the protein or receptor of the known three-dimensional structure. In this docking simulation, the ligand being docked was kept as flexible while target protein was kept as rigid. The graphical user interface i.e. Autodock Tools was used to prepare, run, analyzes the docking simulations.
Current And Future Ad Therapy
Till date there are no such drugs/treatments available that can cure AD completely. However, there are several medications developed for Alzheimer’s disease that can temporarily attenuate the symptoms. The Food and Drug Administration (FDA), U.S. has affirmed two medications-acetylcholinesterase inhibitors and Memantine. Drugs such as tacrine, rivastigmine, galantamine, and donepezilare are the widely used conventional drugs to treat AD (Islam et al. 2013). Memantine is a dissociative hallucinogenic and anesthetic drug of the adamantane class of chemicals that are currently used as an FDA approved drug in the treatment of AD (www.alz.org). Therefore, traditional drugs like memantine and donepezil are being extendedly used as the reference in molecular docking studies. Hence, the objective of eventual AD therapy is to discover such novel compounds which can target the tau protein and so that can be utilized for the recovery of neurodegenerative loss (Schneide et al. 2008).
The study related to the AD is focused more towards the traditional medicinal plants and its components such as Withania somnifera (Ashwagandha), Celastrus paniculatus (Jyotismati), Convolvulus pluricaulis (Shankhpushpi), Bacopa monnieri (Brahmi). By analyzing the binding energies of various ligands such as acacatechin, catechin, galangin, scopoletin, silibinin, memantine (as standard), it was observed that flavonoids exhibit binding energy scaled between 7.07 kcal/mol to -4.85 kcal/ mol. Silibinin demonstrate prominent binding energy -7.07 kcal/mol than the standard memantine (-5.89 kcal/mol) (Madeswaran et al. 2013). A phytocompound, Catechin (with binding energy -9.7 kcal/mol) was shown to be the potent target of GSK-3â and showed the same drug-likeness as conventional drug Donepzil (with binding energy-8.9kcal/mol), (Alam et al. 2017).
Withania somnifera, a potential inhibitor of GSK-3â
Withania somnifera commonly called Ashwagandha, Indian ginseng and wind cherry have been recognizes as an important herb in Indigenous and ayurvedic medical system. Historically, the plant has been used therapeutically for boosting the brain function including memory retrieval. It has a cognition promoting effect in adults and children (Singh et al. 2011). It consists of two components: withanolides and withanamides. Withanolide A is extracted from the roots of the plant and promotes antioxidant properties that protect nerve cells from harmful free radicals. Many clinical trials and excessive research on animals support the use of Ashwagandha for anxiety, cognitive and neurological disorders ( Rajasekar et al. 2011). Withanolides have also been used for the treatment of AD (Khan et al. 2016). Withanolide A is used as an inhibitor of acetylcholinesterase activity and reduces beta-amyloid protein formation. Also, it has been involved in the regeneration of pre and postsynaptic neurons. Instead of the root extract, a study also suggested fruits and leaves of Egyptian plant have strong antioxidant activity (Mahrous et al. 2017)
Future Perspectives
Several new therapeutic approaches are currently under investigation which aims at targeting proteins such as Apolipoprotein E which is also responsible for the accumulation and hyperphosphorylation of tau. Anti-tau immunotherapeutic agents have gained much focus due to their specificity and selectivity to combat AD. But a longer follow up period might be required to test the safety and efficacy as the results were promising .Moreover targeting either tau or amyloid beta individually is not apparently the satisfactory approach and therefore, combinational therapies might be thought of as a new proposal, (Coman et al. 2017 Bittar et al. 2018).
Conclusion
Drug research is of utmost importance in the field of medicine. Consequently, the use of computers to foresee the efficiency of binding of a set of molecules or ligands with the target is an important element of drug development process.To explore potent and effective drugs for the treatment of AD, different phytocompounds were compared against the standard using Autodock4. Appropriate ligands were docked into the active site of the receptor GSK-3â and analyzed for the effective protein-ligand interactions. Therefore molecular docking identified many more promising, efficacious, selective new drugs against Alzheimer’s reducing the time span of complex drug discovery process. Appropriate experimental evidences such as ADMET analysis which testifies absorption, penetration and toxicity may also be considered further as a lead in drug discovery process.
Acknowledgements
The authors are thankful to the Department of Biotechnology, University Institute of Engineering and Technology, Kurukshetra (U.I.E.T) for providing the space and resources for this work.
Conflict of Interest Statement
Authors state no conflict of interest. All authors have read the journal’s Publication ethics and publication malpractice statement available at the journal’s website and hereby confirm that they comply with all its parts applicable to the present scientific work.
References
Alam A, Tamkeen N, Imam N, Farooqui A, Ahmed M.M. Ali S. Malik M.Z. and Ishrat R (2017) Pharmacokinetics and Molecular Docking studies of Plant-Derived Natural Compounds to Exploring Potential Anti-Alzheimer Activity Available from: https://arxiv.org/pdf/1709.10374
Alvarez A.C., Costa A.M. and Vilarrasa J (2017) The Performance of Several Docking Programs at Reproducing Protein–Macrolide-Like Crystal Structures. Molecules 22(1), 36 DOI:10.3390/molecules22010136
Alzheimer’s disease and tauopathies.npj Vaccines volume 3, Article number: 9 DOI:
Anja S, Eckhard M. (2008) Tau-Based Treatment Strategies in Neurodegenerative Diseases Neurotherapeutics. The Journal of the American Society for Experimental NeuroTherapeutics [cited 2008 July]; 5: 443-457.Available from: https://www.ncbi.nlm.nih.gov /pmc /articles/ PMC5084246 DOI: 10.1016/j.nurt.2008.05.006
Anna K, Justin V L, Tomasz J, Fred V L. (2011) GSK3 and Alzheimer’s disease: facts and fiction. Frontiers in Molecular Neuroscience [cited 2011]; 4(17):1-10. Available from: https://www.frontiersin.org/articles/10.3389/fnmol.2011.00017/full DOI: 10.3389/fnmol.
Anna MP, Urszula W, Marcelina G, Anna F, Grazyna N.(2014) Tau Protein Modifications and Interactions: Their Role in Function and Dysfunction. Int. J. Mol. Sci. [cited 2014 Mar 18]; 15: 4671-4713. Available from: http://www.mdpi.com/1422-0067/15/3/4671ag DOI: 10.3390/ ijms 15034671
Articles /PMC5425816 DOI: 10.1007/s12551-016-0247-1 articles DOI: 10.3389/fnagi.2016.00262
Arumugam M, Muthuswamy U, Kuppusamy A, Thirumalaisamy S, Varadharajan S, Puliyath J. (2012) Docking studies; In silico lipoxygenase inhibitory activity of some commercially available flavonoids commercially available flavonoids Advances in Tau-focused drug discovery for Alzheimer’s disease and related tauopathies Ban. J Pha. [cited 2012 Jan 15]; 6: 133-138.Available From:https://www.banglajol.Info/Index.php/7055 DOI: 10.3329/ bjp.v6i2.9408
Arumugam M, Muthuswamy U, Kuppusamy A, Thirumalaisamy S, Varadharajan S, Puliyath J. (2013) Computational drug discovery of potential TAU protein kinase I inhibitors using in Silico Docking Studies Ban. J. Pha. 8: 131-135.Available from: http://www.banglajol.info
Asam K, Staniszewski A, Zhang H, Melideo S.L., Mazzeo A, Voronkov M, Huber K.L., Pérez E, Stock M, Stock J.B., Arancio O, and . Nicholls R.E. (2017) Eicosanoyl-5-hydroxytryptamide (EHT) prevents Alzheimer’s disease-related cognitive and electrophysiological impairments in mice exposed to elevated concentrations of oligomeric beta-amyloid. PLoS One 12(12) DOI: 10.1371/journal.pone.0189413
Avila J, Jiménez JS, Sayas CL, Zabala MBCS, Rivas G, Hernández F. (2016) Tau structures. Frontiers in Aging Neuroscience 8(262): 1-10. Availble from: https://www.frontiersin.org/
Baptista FI, Henriques AG, Silva AMS, Wiltfang A, Silva OAB. (2014) Flavonoids as Therapeutic Compounds Targeting Key Proteins Involved in Alzheimer’s Disease. ACS Chem. Neurosci. 5(2): 83−92. Available from: DOI:abs/10.1021/cn400213r.2
Billingsley ML, Kincaid RL. (1997) Regulated phosphorylation and dephosphorylation of tau protein: effects on microtubule interaction, intracellular trafficking, and neurodegeneration. Biochem J. 323(pt3):577-91
Bittar A, Sengupta U and Kayed R (2018) Prospects for strain-specific immunotherapy in
Brunden KR, Trojanowski JQ, Le VMY (2010) Advances in Tau-focused drug discovery for Alzheimer’s disease and related tauopathies. Nat Rev Drug Discov. [cited 2010 apr 1]; 8(10): 783-793.Available from: https:// www.ncbi.nlm.nih.gov/pmc/articles/ PMC/articles/PMC 2787232 DOI: 10.1038/nrd2959
Collignon B, Schulz R, Smith JC, Baudry J. (2011) Task-parallel message passing interface implementation of Autodock4 for docking of very large databases of compounds using high-performance super-computers . J. Comp. Chem. [cited 2011 Sep10]; 32: 1202–1209. Available from: https://onlinelibrary.wiley.com DOI: 10.1002/jcc.21696
Coman H and Neme¸sB (2017) New Therapeutic Targets in Alzheimer’s Disease. International Journal of Gerontology 11(1), Pages 2-6 DOI: https://doi.org/10.1016/j.ijge.2 016.07.003
Congdon E.E, Sigurdsson E.M. (2018) Tau-targeting therapies for Alzheimer disease. Nature Reviews Neurology
Crews L, Masliah E. (2010) Molecular mechanisms of neurodegeneration in Alzheimer’s disease Human Molecular Genetics 19(1): 12-20. Available from: https://www.ncbi.nlm. nih.gov/pmc/articlsgov/pmc/articles/PMC2875049 DOI: 10.1093/hmg/ddq160.
Dixit R, Ross JL, Goldman YE, Holzbaur EL. (2008) Differential regulation of dynein and kinesin motor proteins by tau Science, Feb; 319: 1086–1089. Available from: https:// www .ncbi.nlm.nih.gov/pubmed/18202255 DOI: 10.1126/science.
1152993
Folch J, Petrov D, Ettcheto M, Abad S, Lopez ES, Garcia ML, Olloquequi J, Zarate CB, Auladell C, Camins A (2016) Current Research Therapeutic Strategies for Alzheimer’s Disease Treatment. Neural Plasticity [cited Aug 2016]:1-15.Available from: http://dx.doi.org/10.1155 /2016/850169312
Goedert M, Spillantini MG, Jakes R, Rutherford D, Crowther RA. (1989) Multiple Isoforms of human microtubule-associated protein tau: sequences and localization in neurofibrillary tangles of Alzheimer’s disease. Neuron 3(4): 519-526. Available from: DOI: 10.1016/0896-6273(89)90210-9
Guo T, Noble W, and Hanger D.P. (2017) Roles of tau protein in health and disease. Acta Neuropathol. 133(5): 665–704 DOI: 10.1007/s00401-017-1707-9
Hamley IW (2012) The Amyloid Beta Peptide: A Chemist’s Perspective. Role in Alzheimer’s and Fibrillization. Chemical Reviews 112: 5147–5192. Available from: https://pubs.acs.org DOI: abs/10.1021/cr3000994
Hooper C, Killick R, Lovestone S. (2008) The GSK3 hypothesis of Alzheimer’s disease. J Neurochem. 104(6):1433-1439
Hussain G, Zhang L, Rasul A, Anwar H , Sohail M.U. Razzaq A, Aziz N, Shabbir A, Ali M and Sun T (2018) Role of Plant-Derived Flavonoids and Their Mechanism in Attenuation of Alzheimer’s and Parkinson’s Diseases: An Update of Recent Data Molecules , 23(4), 814 DOI:10.3390/molecules23040814
Kametani F, Hasegawa M. (2018) Reconsideration of Amyloid Hypothesis and Tau Hypothesis in Alzheimer’s Disease Front Neurosci.12: 25. DOI: 10.3389/fnins.2018.00025
Kazunori K, Kiwami K, Takuya T, Taisuke T.(2017) Dysregulated Metabolism of the Amyloid-β Protein and Therapeutic Approaches in Alzheimer Disease. J Cellular Biochemistry 118(12): 4183–4190
Khalid I, Fei L, Cheng XG, Inge GI. (2011) Tau in Alzheimer Disease and Related Tauopathies. Cur. Alzheimer Res. [cited 2011 May 9]; 7(8): 656–664. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3090074
Khan SA, Khan SB, Shah Z, Asiri AM. (2016) Withanolides: Biologically Active Constituents in the Treatment of Alzheimer’s disease. Med Chem. 12(3):238-56. Available from:https://www.ncbi.nlm.nih.gov/pubmed/26527154 DOI:10.2174/ 573406411/ 6661510
Kolarova M, García-Sierra F, Bartos A, Ricny J, Ripova D. Structure and Pathology of Tau Protein in Alzheimer Disease (2012) International Journal of Alzheimer’s disease 2012: 1-13. Available from: http://dx.doi.org/10.1155/2012/731526
Leroy K, Boutajangout A, Authelet M, Woodgett JR, Anderton BH, Brion JP. (2002) The active form of glycogen synthase kinase-3beta is associated with granulovacuolar degeneration in neurons in Alzheimer’s disease . Acta Neuropathol. [cited 2002 feb]; 103: 91–99. Available from: https://www.ncbi.nlm.nih.gov/pubmed/11810173 DOI: 10.1007/ s004010100435
Mahrous RS, Ghareeb DA, Fathy HM, Abu EL-Khair RM, Omar AA. (2017) The Protective Effect of Egyptian Withania somnifera Against Alzheimer’s. Med. Aromat Plants (Los Angeles). 6(2): 1-6. Available from: http/www.omics.org/ DOI:10.4172/2167-0412.100028.
Mark AS, Keisuke H, Karen H, Migu AP, Peggy LRH, Sandra LS, Massimo T, George P. (1998) Amyloid-/3 Deposition in Alzheimer Transgenic Mice Is Associated with Oxidative Stress. J Neurochemistry 70(5): 2212-5
Martin L, Latypova X, Terro F. (2011) Post-translational modifications of tau protein: implications for Alzheimer’s disease. Neurochem. Int. 58(4):458–471. Available from:https://www.ncbi.nlm.nih.gov/pubmed/21215781 DOI:10.1016/j.neuint.2010.12.023
Medina M (2018) An Overview on the Clinical Development of Tau-Based Therapeutics Int. J. Mol. Sci. 19, 1160 Available from http://www.mdpi.com/journal/ijms DOI: 10.3390/ijms19 041160
Medina M, Wandosell F. (2011) Deconstructing GSK-3: The Fine Regulation of Its Activity. International Journal of Alzheimer’s disease. Feb; 2011:1-12. Available from: http://dx.doi. org/10.4061/2011/479249
Mukai F, Ishiguro K, Sano Y, Fujita SC.(2002) Alternative splicing isoform of tau protein kinase I/glycogen synthase kinase 3 beta. J. Neurochem. ; 81(5):1073–1083
Murphy MP, LeVine H. (2010) Alzheimer’s Disease and the â-Amyloid Peptide. J Alzheimers Dis. 19(1):311. Available from: https://www.ncbi.gov/pmc/articles pmc 28135509/DOI:
Natraj S, Pagadala, Syed K, Tuszynski J. (2017) Software for molecular docking: a review Biophys. Rev. 9(2): 91-102. Available from: https://www.ncbi.nlm.nih.gov/pmc/ now everything hinges on an approach that’s already run into trouble
Overview of Alzheimer’s Disease. Chicago (US): Alzheimer’s Association; 2009. Alzheimer’s Disease Facts and Figures; ©2009; [about 80p]. Available from: https:// www.alz.org/national/documents/report_alzfactsfigures 2009
Pei JJ, Tanaka T, Tung YC, Braak E, Iqbal K, Grundke II. (1997) Distribution, levels, and activity of glycogen synthase kinase-3 in the Alzheimer diseased brain. J Neuropathol Exp Neurol. 1997 Jan; 56(1):70-8. Available from: https://www.ncbi.nlm.nih.gov/pubmed
Rajasekar S, Elango R. (2011) Estimation of alkaloid content of Ashwagandha (Withania somnifera) with HPLC methods. Journal of Experimental Sciences 2(5): 39-41. Available from: https://www.ncbi.nlm.nih.gov/pub med/1903170
Ramsey L (2018) The search for new Alzheimer’s treatments just faced another setback – and Sauer A (2017) Has Alzheimer’s Research Been Wrong for 20 Years? https://www.alzheimers.net
Schaffer B, Wiedau-Pazos M, Geschwind DH.(2003) Gene structure and alternative splicing of glycogen synthase kinase 3 beta (GSK-3beta) in neural and non-neural tissues. Gene 302:73–81.Available from: http://europepmc. org/abstract/med/12527198 DOI: 10.1016 /S0378-1119(02)01092-2
Shin RW, Iwaki T, Kitamoto T, Tateishi J. (1991) Hydrated autoclave pretreatment enhances tau immunoreactivity in formalin-fixed normal and Alzheimer’s disease brain tissues. Lab. Invest.64 (5): 693–702. Available from:https://www.ncbi.nlm.nih.gov/Pubmed/1903170
Singh N, Bhalla M, Jager PD, Gilca M. (2011) An Overview on Ashwagandha: A Rasayana (Rejuvenator) of Ayurveda. African Journal of Traditional, Complementary and Alternative Medicines. 8(5): 208-213. Available From:https://www.ncbi.nlm.nih.gov/ pmc/Articles/ PMC3252722 DOI: 10.4314/ ajtcam.v8i5S.9
Spencer JPE. (2007) The interactions of flavonoids within neuronal signaling pathways. Genes Nutr. 2(3): 257–273
Spencer JPE. (2010) The impact of fruit flavonoids on memory and cognition. British J Nutrition 104: S40–S47
Stambolic V, Woodgett JR. (1994) Mitogen inaction of glycogen synthase kinase-3 beta in intact cells via serine 9 phosphorylation. The Biochemical Journal. 303(Pt 3): 701–4. Available from: https://www.ncbi.nlm.nih. gov/pmc/articles/PMC1137602
Taniguchi S, Suzuki N, Masuda M, Hisanaga SI, Iwatsubo T, Goedert M, Hasegawa M. (2004) Inhibition of Heparin-induced Tau Filament Formation by Phenothiazines, Polyphenols, and Porphyrins. The Journal of Biological Chemistry 280(9): 7614–7623. Available from: http://www.jbc.org/content/280/9/7614 DOI: 10.1074/jbc.M408714200
Underwood E. (2016) Tau protein—not amyloid—may be key driver of Alzheimer’s symptoms. Brain & Behavior, Memory Topic Available from: https://www.sciencemag.org /news/2016/05 DOI:10.1126/science.aaf9985.
Yin YI, Bassit B, Zhu L, Yang X, Wang C, Li YM. (2007) ã-Secretase Substrate Concentration Modulates the Aâ42/Aâ40 Ratio Implications For Alzheimer Disease. J Biological Chemistry 282: 23639-23644


