1Department of Prosthetic Dental Science, College of Dentistry, Jazan University, Jazan, Saudi Arabia.
2Department of Oral and Maxillofacial Surgery, College of Dentistry, Aden University, Yemen.
3 College of Dentistry, Jazan University, Jazan, Saudi Arabia.
4College of Dentistry, Ibn al-Nafis University, Sanaa, Yemen.
Corresponding author email: drmoaleem2014@gmail.com
Article Publishing History
Received: 19/10/2021
Accepted After Revision: 22/12/2021
Hürzeler presented the socket-shield technique (SST) more than 10 years ago. The partial extraction therapy (PET), a collective concept of utilizing the patient’s own tooth root to preserve the periodontium and peri-implant tissue, has been remarkably developed. PET comprises a group of novel techniques for post-extraction implant placement. Several modifications of PET and simultaneous implant placement have been presented since its inception. Since its origin, several alterations have been employed in the methodology of partial extraction of the root and the simultaneous implant placement. A repeatable, predictable protocol is needed to provide tooth replacement in esthetic dentistry. Moreover, a standardized procedure provides a good framework for clinicians to report data relating to the technique with procedural consistency.
This review aims to illustrate a reproducible and systematic protocol for the PET techniques with immediate implant placement at the aesthetic zone. The most used technique is the socket-shield technique, which is potentially offers promising results, minimizing the necessity for invasive bone grafts round implants in the aesthetic area, clinical data to support this is very inadequate. The limited research data existing is cooperated by a deficiency of well-designed prospective randomized controlled investigations. The present case studies and techniques are of actual incomplete technical value. Retrospective studies published in limited records but are of inconsistent plan. At this point, it is indistinct whether the socket-shield technique will offer a stable long-time outcome or not
Partial Extraction Therapy, Pontic Shield, Proximal-Socket Shield, Root Submergence,Socket Shield Technique.
Al Moaleem M. M, Abdulrab A. M. M, Khan H. K, Khawaji A. H, Mawkili L. K, Faris S. M, Alsam S. M, Alalmaie N. I, Eshwi H. I. A. Ten-year Success in the Application of Partial Extraction Therapy: A Systematic Review. Biosc.Biotech.Res.Comm. 2021;14(4).
Al Moaleem M. M, Abdulrab A. M. M, Khan H. K, Khawaji A. H, Mawkili L. K, Faris S. M, Alsam S. M, Alalmaie N. I, Eshwi H. I. A. Ten-year Success in the Application of Partial Extraction Therapy: A Systematic Review. Biosc.Biotech.Res.Comm. 2021;14(4). Available from: <a href=”https://bit.ly/3DEz4N4“>https://bit.ly/3DEz4N4</a>
Copyright © This is an Open Access Article distributed under the Terms of the Creative Commons Attribution License (CC-BY) https://creativecommons.org/licenses/by/4.0/, which permits unrestricted use distribution and reproduction in any medium, sources the original author and sources are credited.
INTRODUCTION
Qualitative and quantitative variations, which arise in the alveolar ridge next tooth removal, can complicate the implant-prosthetic restoration. Several socket and alveolar ridge preservation systems have been developed to minimize the alveolar ridge atrophy. The tooth root can be conserved to limit bone resorption under a fixed or removable denture (Pagni et al. 2012). PET, as a socket shield technique, was first introduced by Hürzeler in (2010) and this process was first carried out on dogs, followed by a single implant placement in a human as a proof‑of‑concept (Hürzeler et al. 2010). Finally, a fabricated screw‑retained abutment was placed with an out‑of‑occlusion provisional crown. Many cases followed the concept and became published (Han et al. 2018; Gluckman et al. 2018; Schwimer et al. 2019).
The concept of PET is composed of four different techniques that aim to preserve slice of the tooth in the bone, thereby minimizing the loss of the bone vasculature and periodontal ligament attachment, thus eliminating the remodeling and resorption of both hard and soft tissues associated with tooth removal. Gluckman et al. (2016a), and Shaheen (2021) found that partial extraction therapy (PET) includes root submergence (RST), socket shield (SST), proximal socket shield (PSST), and pontic-shield (PST) (BUSER et al. 2000; Abadzhiev et al. 2014; Troiano et al. 2014; Al-Dary and Al Hadidi 2015; Durrani et al. 2017; Mitsias et al. 2017; Al-Dary and Alsayed 2017; (Durrani et al. 2017; Esteve-Pardo and Polis-Yanes et al. 2020; Abd-Elrahman et al. 2020).
These systems have provided excellent mechanical, biological, and esthetic outcomes in the hands of experienced operators with meticulous treatment planning and case selection. In addition, a modified SST was presented by (Glocker et al. 2014). Han et al. 2018 used a 1.5-mm thick shield with the most coronal portion, while Guo et al. 2018 modified the SST by placing platelet-rich fibrin (PRF) in the gap between the root fragment and the implant and found that that peri-implant tissue was well preserved by the SST without significant peri-implant tissue resorption (Aslan 2018).
The most commonly used indices for the evaluation of the aesthetic dimension of anterior single-tooth implants are the pink and white aesthetic score (PES/WES) indices, and they have been used in several studies (Belser et al. 2009; Buser et al. 2013; Mangano et al. 2014a; Zhao et al. 2016). Pink esthetic score evaluates the anterior esthetic of the implant-supported single crown on seven points, including mesial and distal papilla, soft-tissue color, contour, level, texture, and deficiency of alveolar (Fonseca 2018 and Mourya et al. 2019).
It comprises 10 variables such as mesial papilla, distal papilla, curvature of the facial mucosa, level of the facial mucosa, the root convexity, soft tissue color, and texture at the facial aspect of the implant site, tooth form, volume, color, surface texture, and translucency. A score of 2, 1 or 0 is assigned to all parameters. All parameters are assessed by direct comparison with the natural, contralateral reference tooth, estimating the degree of match or mismatch (Belser et al. 2009).
Based on the Kaplan–Meier survival estimator, the cumulative implant survival rate (implant-based) was high. The complications were the infection of the root portion, with suppuration and fistula formation, which occurred in four cases at 83, 51, 59, and 12 months after implant insertion) and the infection of the root associated with peri implant mucositis in 1 case (at 113 months from the insertion of the fixture (Mangano et al. 2019).
Infection of the root membrane with fistula was determined in 50% of cases the occurrence of periimplantitis that caused the loss of two implants (at 12 and 59 months after insertion). In the remaining 50% of cases, however, the implant was not affected by the infection (Gluckman et al. 2016; Siormpas. et al. 2018). The prosthetic complications were divided into minor complications, such as no treatment needed or 60 min chair time and additional laboratory costs, repositioning of a loosened abutment, and removal of a fractured abutment or fabrication of new restorations. Static and dynamic occlusions were evaluated using standard occluding papers.
All prosthetic complications were carefully registered and managed if possible, during the follow-up visits. Mangano et al. (2016) and Han et al. (2018) have shown a prosthetic complication such as abutment screw loosening, abutment fracture, and/or chipping/fracture of the ceramic restorations. Al-Dary and Alsayed (2017) replaced missing maxillary 2 central incisors with zircon cantilever bridge (Abd-Elrahman et al. 2020). This review aims to illustrate a reproducible and systematic protocol for the PET techniques with IIP at the aesthetic zone and summarize the clinical outcome of this technique during the last 10 years.
MATERIAL AND METHODS
An electronic exploration was achieved to identify related research. The search was restricted to May (2010) to October (2021), at the time of gathering of the information with the resulting databases from Medline/PubMed, Cochrane, Scopus, EBSCO host, Google website, Web of Science, and Wiley Library. The search terms included “Partial extraction therapy”, “socket shield technique,” “modified SST”, “root membrane technique”, “Pontic-shield technique”, “type of the final restoration”, and “immediate implant placement”, and case report, series, and clinical studies. The study was finalized manually by evaluating the particular reference tilts of similar articles. Studies published from (2010 to 2021) were included if they met the following measures: case report, case series, prospective and retrospective studies, clinical trial study, and involves the use of PET and procedures with IIP after tooth extraction.
The exclusion criteria were clinical studies on human and follow-up not less than 3 months after implant assignment. Two review authors (Al MM and A.M.A) evaluated the title, abstract, and available text of articles documented in the electronic search and the inclusion and exclusion criteria. All published papers related to PET reports were evaluated for relevance, eligibility, and data extraction. For all type of studies, the implant osseointegration, shield exposure, shield infection, shield migration, soft tissue contour, and type of prostheses were recorded. Radiologic result for buccal and/or crestal bone loss were assessed. The selected studies were analyzed for complications and adverse effects stated by corresponding author(s).
All data were extracted, and the contents were screened by the author. Full texts of the associated studies were reviewed for further assessment. This systematic review was designed in accordance with the Preferred Reporting Items for Systematic reviews (Moher et al. 2009) with some modifications specified by recent systematic reviews published in the previous studies (Siormpas et al. 2018; Blaschke and Schwass 2020; Ogawaa et al. 2021; Magadmi 2021).
The extracted data from the nominated studies were as follows: author(s) name, publication year, type of technique used, arch, region, tooth type, causes of extractions, implant placement, loading protocol, final restoration type, complications, survival rate, and follow-up period (Table 1). The quality of each involved study was evaluated by the authors (Al MM and A.M). The included articles were evaluated using the Checklist for Systematic Review, Case Reports and/or Series. Data were organized and summarized in designed tables. The mentioned variables in all collected studies in any form were summarized and analyzed (Blaschke and Schwass 2020; Ogawaa et al. 2021; Magadmi 2021).
RESULTS AND DISCUSSION
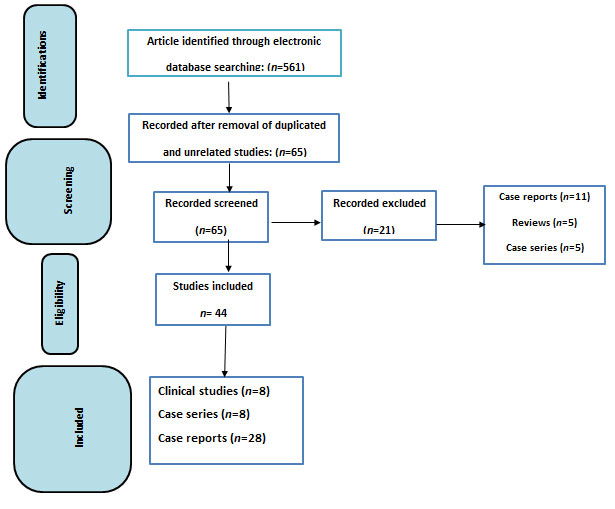
The flowchart for the selection of articles based on their eligibility for the current systematic review is presented in Figure 1. The database search across literature resulted in 561 articles related to questions raised, and these articles were gathered and analyzed. The author further separated the publications and removed similar studies and other papers articles not correlated to the question elevated. A total of 496 studies were removed, because they are duplicates or not related to the study. By screening 65 articles, 21 studies were omitted, because they were not related to the review, leaving 44 studies (Figure 1: Flowchart). Eight studies were included for each of clinical studies and case series, while the remaining articles were case reports (28).
Variables related to PER among clinical studies or both case series and reports were presented in Table 1. The extracted items were included the author(s) name, publication year, type of technique used, arch, region, tooth type, causes of extractions, implant placement, loading protocol, final prostheses type, complications, survival rate, and follow-up period. A total of 44 articles were included in the present review, as shown in Table 1. Eight clinical studies and eight case series were conducted between 2014 and 2021. Majority of the case reports were about SST and immediate implant placement. All cases were followed up with minimum of 3 months and extended up to 10 years. All the parameters’ data are represented and arranged.
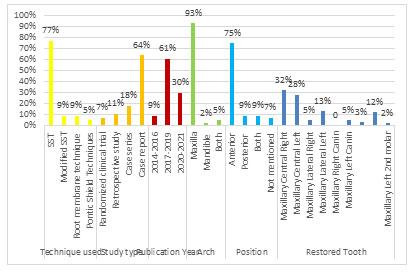
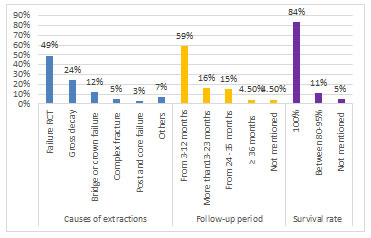
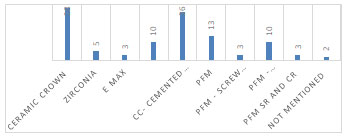
Graph 1 represents the outcome of screened studies in relation to PET with immediate implant. The highest percentage of the type of technique used. The proportion of implant loading technique (immediate vs. delayed), arch involved maxillary or mandibular arch, the place of studies applied, and the ratio of each tooth type are shown. Parameters such as causes of extraction, follow-up period, and survival rate for each study are presented in Graph 2. The details of the materials used for final prosthesis and the number of screws retained or cemented prosthesis are shown in Graph 3.
In addition to that the studies by Arora and Ivanovski (2018), Han et al. (2018); Hana et al. (2020); Mathew et al. (2020) recorded 102,33,25,13,7, and 3 maxillaries central, lateral, canine, 1st and 2nd premolar, and mandibular canines were recorded, respectively. Abadzhiev et al. (2014) (80%), Arora and Ivanovski (2017) (88%), Schwimer et al. (2018) (100 %); Zuhr et al. (2020) (100.00%), Hana et al. (2020) (95%) found high percentage of success with different period of follow-up as recorded after each one. Canti-lever of 6 unites from maxillary canine in the left side into canine on other side with two abutments. Lateral’s incisors were used by Polis-Yan et ai. (2020).
Cemented retained cantilever all ceramic with abutment was lateral incisor and the pontic was the adjacent central incisors, while Abadzhiev et al. (2014) used mixed ceramic and PFM crowns for their final restoration after SST with or without IIP. Other authors used mixed PFM and CC as Arora and Ivanovski (2017) used Screw R PFM, cemented PFM. Pour et al. 2017 used SR CC, while Hinze et al. (2018) used PFM and ceramic crowns (Esteve-pardo and Colombia 2018).
Various PET techniques have provided outstanding biological, mechanical, and aesthetic consequences in hands of knowledgeable clinicians with careful treatment arrangement and case collection. A uniform assessment of PET outcomes needs to be established to provide objective findings, in addition to a consistent protocol for root portions preparation and to place dental implants in the ideal place and achieve long‑term success of treatment. This review aims to determine the advantages of different PET techniques aesthetic outcome IIP in the aesthetic zone and the different types of final prostheses used (Esteve-pardo and Colombia 2018; Oliveira et al. 2021).
Among the PET techniques, SST is the most used technique because of its many advantages in cases of post extraction immediate implant with IIP, such as high stability and well-preserved hard and soft tissue; it preserves the buccal bone marginal and inter-implant papilla with minimum marginal bone loss, maintains alveolar bone level, and does not change soft tissue dimensions (Nguyen et al. 2020; Alone and Niswade 2021; Srivastava et al. 2021; Oliveira et al. 2021). This method is good alternative to preserve BCP in aesthetic area and healthy per-implant tissue, improved buccal contour stability and or better esthetic outcomes can achieved (Dayakar et al. 2018; Patel et al. 2019; Arabbi et al. 2019; Schwimer et al. 2019; Dash et al. 2020).
In a case series by Habashneh et al. (2019) and Alshammari et al. (2020) they show minimally invasive approach that can preserve hard and soft tissue and contour of ridge, and this method was implemented in areas of high aesthetic demands to achieve good esthetic outcomes. SST with IIRP preserved hard and soft tissue and kept it stable without any changes in dimension, resulting in optimum aesthetic results and improving and preserving the buccal contour of ridge areas of high aesthetic demands (maxillary anterior up to premolars) to achieve good esthetic outcomes (Glocker et al. 2014; Mitsias et al. 2017; Habashneh et al. 2019; Mathew et al. 2020; Nguyen et al. 2020; Germi et al. 2020).
Tissue volumes remain unchanged, and good osteointegration was achieved (Troiano et al. 2014; Gluckman et al. 2016b; Baumer et al. 2017). In addition to the above characteristics, a group of clinical studies showed excellent scores for PES and was in clinical studies (Sun et al. 2020; Hana et al. 2020; Abd-Elrahman et al. 2020).
Ideally, a method for the prevention of alveolar ridge resorption should be cost-effective and minimally invasive. Various methods of guided bone regeneration (GBR) have been described to retain the original dimension of the bone after extraction. All these procedures are cost-intensive and technique-sensitive. The presented method is cost-effective but is a technique-sensitive SST that avoids the resorption of the bundle bone by leaving a buccal root segment (socket shield) in place (Mourya et al. 2019; Ogawa et al. 2021).
The SST seems to be beneficial for ridge preservation despite its insufficient documentation. In this case report series, implants were placed immediately after extracting a hopeless tooth by using this technique, and the patient was followed up for 1 year to document functional and esthetic outcomes (Mourya et al. 2019; Ogawa et al. 2021).
PES was between 8–10 and 6–10 after 6 and 12 months, while previous studies recorded 12.2 PES with complete score for central incisors, recorded 13.5 mm, and recorded a mean PES of 12. Only a single article recorded PES and MBL for CIIP of 10.8 and 0. 88 mm by, respectively. The MBL for SST was 0.1 ± 0.2 mm as determined in the previous studies and 0.17-0.22 mm as determined in the previous studies (Baumer et al. 2017; Zhu et al. 2018; Germi et al. 2020; Mathew et al. 2020; Sun et al. 2020; Mathew et al. 2020; Mathew et al. 2020). Other information in relation to case series are available in Table 1 and Graph 1.
Table 1. Qualitative analysis of studies included in this review and arranged ascending
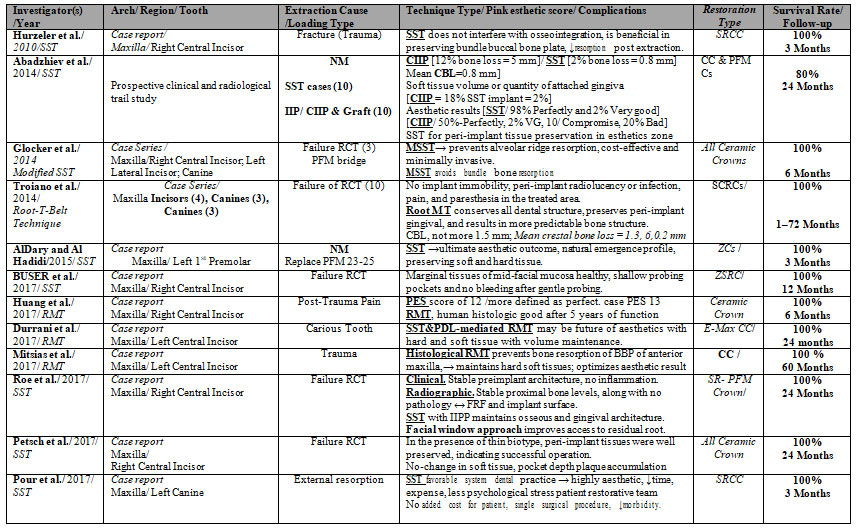
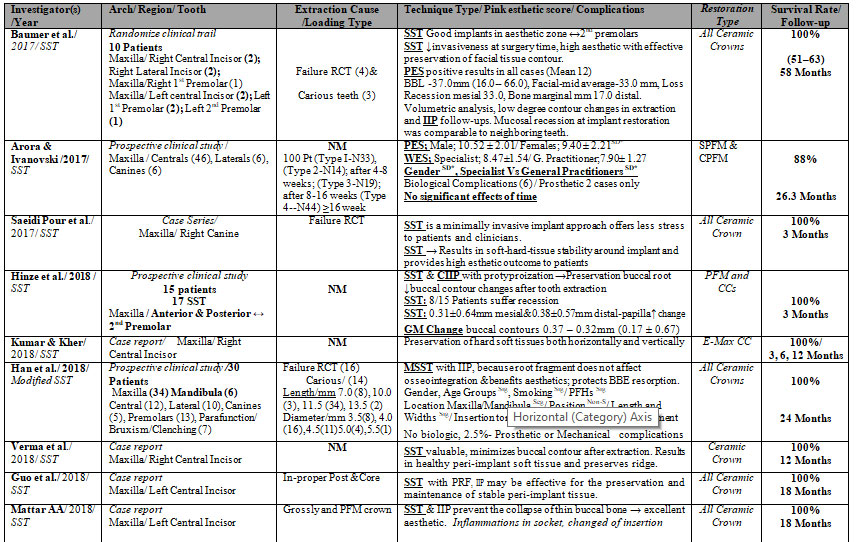
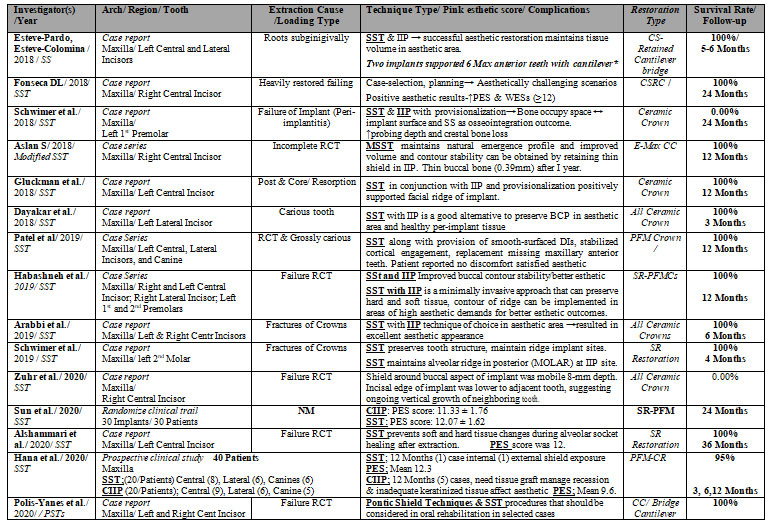
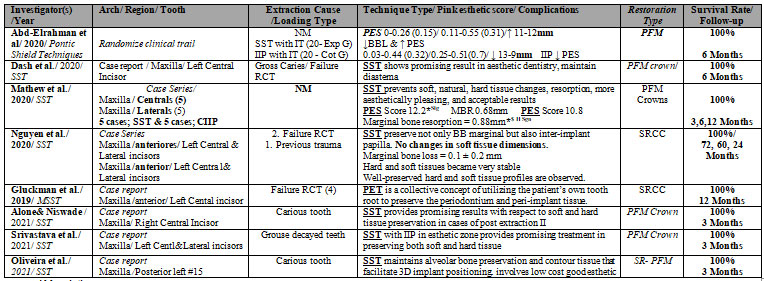 Abbreviations: Partial Extraction Therapy -PET; Root Submergence – RST; Socket Shield- SST; Proximal Socket Shield-PSST; Pontic-Shield -PST; Marginal Bone Loss- MBL; Crestal bone level -CBL; Crestal bone resorption- CBR; Buccal bone plate- BBP; BBL- buccal bone loss; Conventional immediate implant placement- CIIP; Modified socket shield technique – MSST; Immediate implant placement- IIP; Delayed – PRF ; Buccal cortical plate – BCP; Root fragment – RF; Alveolar bone loss – ABL; Pocket Probing Depth— PPD; implant surfaces- IS; Randomized clinical trial- RCT; Pink esthetic score- PES; ↑-Increase-; ↓-Decrease; ↔-Between; → Resulted in % – Percentage-; ↔-Between; NM-Not mentioned; Zirconia Abutment-ZA; Ceramic Crown-CC; Zirconia Crown- ZC; Screw-retained Ceramic Crowns- SRCC; All Ceramic Crown-ACC; Screw Retained All Ceramic-SRAL; Screw Retained Porcelain-Fused-Metal-SR-PFM; Porcelain-Fused-Metal-PFM
Abbreviations: Partial Extraction Therapy -PET; Root Submergence – RST; Socket Shield- SST; Proximal Socket Shield-PSST; Pontic-Shield -PST; Marginal Bone Loss- MBL; Crestal bone level -CBL; Crestal bone resorption- CBR; Buccal bone plate- BBP; BBL- buccal bone loss; Conventional immediate implant placement- CIIP; Modified socket shield technique – MSST; Immediate implant placement- IIP; Delayed – PRF ; Buccal cortical plate – BCP; Root fragment – RF; Alveolar bone loss – ABL; Pocket Probing Depth— PPD; implant surfaces- IS; Randomized clinical trial- RCT; Pink esthetic score- PES; ↑-Increase-; ↓-Decrease; ↔-Between; → Resulted in % – Percentage-; ↔-Between; NM-Not mentioned; Zirconia Abutment-ZA; Ceramic Crown-CC; Zirconia Crown- ZC; Screw-retained Ceramic Crowns- SRCC; All Ceramic Crown-ACC; Screw Retained All Ceramic-SRAL; Screw Retained Porcelain-Fused-Metal-SR-PFM; Porcelain-Fused-Metal-PFM
Figure 1: Flowchart of the study selection process (Moher et al. 2009; Siormpas et al. 2018;
Blaschke and Schwass 2020; Ogawaa et al. 2021; Magadmi. 2021).
Graph 1: Extracted data in relation to type of PET. Study type, arch
type, position, and restored tooth type.
Graph 2: Causes of tooth extraction, follow-up period, and survival
rate of studies included in this review.
Graph 3: Numbers of different types of prostheses (final restoration)
used in studies and cementation technique.
The advantage of RST is inexpensive preservation of alveolar bone dimensions to provide a good retentive surface area for RDP or to preserve alveolar bone for a future dental implant, or to preserve the tissues’ dimensions in the pontic’s area under a tooth supported FDP, with a chance of developing bone and new cementum and connective tissue coronal to submerged segment. It also preserves the tissues next to a dental implant and improves the predictability of interdental papillae height in DIT (Roe et al. 2017; Petsch et al. 2017; Baumer et al. 2017; Pour et al. 2017; Kumar and Kher 2018; Verma et al. 2018; Guo et al. 2018; Mattar 2018; Patel et al. 2018; Schwimer et al. 2019).
In the aesthetic area, the preservation of the interdental papilla among two implants is one of the major challenges of implant rehabilitation, and the PSST was first proposed and described by involving the similar values of the SST, but the distal root piece was used instead of the buccal one. Consequently, studies about this technique are lacking (Chen et al. 2018). The complications observed during follow-up of case series include a shield failure caused by infection, a case of deficiency of alveolar ridge, a patient who had complications with the three other socket shields exposed caused by failure of soft tissue closure (Lagas et al. 2015; Gluckman et al. 2016b; Schwimer et al. 2019).
The pontic ST was recognized as the modified SST, and it was introduced to preserve both hard and soft tissues in the pontic extents following the same technique as the SST. However, instead of inserting an IIP in the socket, a bone grafting material was used to seal the socket, and the socket was closed by a repositioned flap, gingival graft, or membrane. Moreover, under the presence of an apical pathology, the buccal pieces can be conserved, while all the other tooth structures and apical lesions are detached, which overcomes a matter that was identified with the use of RST (Nisar et al. 2020).
CONCLUSION
The findings of the present study suggests that although PET can be used for dental implant treatment, it remains difficult to predict long-term success of this technique until high-quality evidence becomes available. Studies published from 2010 to 202 were included. A total of 40 studies were included, as randomized controlled trial, cohort studies, clinical case reports, and case series. 123 patients were treated with PET, most of them underwent SST with IIP. The follow-up was conducted between 3–120 months after placement. Several complications were recorded, but it was manipulated. Most studies reported implant survival without complications (91%). Most of cases that were followed up for more than 12 months after implant placement achieved a good aesthetic appearance. The failure rate was low without the complications, although some failures occurred because of failed implant osseointegration, socket shield mobility and infection, socket shield exposure or migration, and apical root resorption.
Data Availability Statement: The database generated and /or analysed during the current study are not publicly available due to privacy, but are available from the corresponding author on reasonable request.
Conflict of Interest: Authors declare no conflicts of interests to disclose.
REFERENCES
Abadzhiev M, Nenkov P, Velcheva P (2014). Conventional immediate implant placement and Immediate placement with Socket shield technique—which is better. Int J Clin Med Res 1(5):176–180
Abd-Elrahman A, Shaheen M and Askar N (2020). Socket shield technique vs conventional immediate implant placement with immediate temporization. Randomized clinical trial. Clin. Implant Dent. Relat. Res; 22: 602–611.
Al Dary H and Al Hadidi A. (2015). The Socket Shield Technique using Bone Trephine: A Case Report. Int J Dentistry Oral Sci; S5:001: 1-5. doi: http://dx.doi.org/10.19070/2377-8075-SI05001.
Al-Dary H and Alsayed A (2017). The Socket Shield Technique: A Case Report with 5 Years Follow Up. EC Dental Science; 15.5: 168-18
Alone N and Niswade G (2021). Clinical Application of the Socket-Shield Concept for immediate implant placement- A Case Report. J Res Med Dent Sci; 9 (6): 36-40.
Alshammari NM, Alhawiti IA and Koshak H (2020). Socket shield technique for optimizing aesthetic results of immediate implants. IP International Journal of Periodontology and Implantology; 5(1): 29-32.
Arabbi KC, Sharanappa M, Priya Y, et al. (2019). Socket Shield: A Case Report. J Pharm Bioallied Sci; 11(1): S72–S75. doi: 10.4103/jpbs.JPBS_228_18.
Arora H and Ivanovski S (2018). Evaluation of the influence of implant placement timing on the esthetic outcomes of single tooth implant treatment in the anterior maxilla: A retrospective study. Journal of Esthetic and Restorative Dentistry; 30(4): 338-345. doi: 10.1111/jerd.12385.
Aslan S (2018). Improved volume and contour stability with thin socket-shield preparation in immediate implant placement and provisionalization in the esthetic zone.The International Journal Of Esthetic Dentistry; 172- 70L6M& 13 t /6MB&3 2t.
Baumer D, Zuhr O, Rebele S et al. (2018). Socket Shield Technique for immediate implant placement – clinical, radiographic and volumetric data after 5 years. Clin. Oral Impl. Res; 28: 1450–1458
Belser UC, Grutter L, Vailati F, et al. (2009). Outcome evaluation of early placed maxillary anterior single-tooth implants using objective esthetic criteria: a cross-sectional, retrospective study in 45 patients with a 2- to 4-year follow-up using pink and white esthetic scores. J Periodontol; 80(1): 140-51.
Blaschke C and Schwass DR (2020). The socket-shield technique: A critical literature review. Int. J. Implant Dent; 6: 52. doi: 10.1186/s40729-020-00246-2.
BUSER D, CHAPPUIS V, BELSER UC et al. (2017). Implant placement post extraction in aesthetic single tooth sites: when immediate, when early, when late? Periodontology 2000; 73: 84–102.
Buser D., Chappuis V., Bornstein MM. et al. (2013). Longterm stability of contour augmentation with early implant placement following single tooth extraction in the esthetic zone: a prospective, cross-sectional study in 41 patients with a 5- to 9-year follow-up. Journal of Periodontology; 84: 1517– 1527.
Chen J, Chiang C and Zhang Y (2018). Esthetic evaluation of natural teeth in anterior maxilla using the pink and white esthetic scores. Clinical Implant Dentistry and Related Research; 20(5): 770-777. 10.1111/cid.12631.
Dash S, Mohapatra A, Srivastava G et al. (2020). Retaining and regaining esthetics in the anterior maxillary region using the socket-shield technique. Contemp Clin Dent; 11: 158-61.
Dayakar MM, Waheed A, Bhat HS et al. (2018). The socket shield technique and immediate implant placement. J Indian Soc Periodontol; 22: 451-455.
Durrani F, Yadav DS, Galohda A et al. (2017). Dimensional Changes in Periodontium with Immediate Replacement of Tooth by Socket Shield Technique: Two-year Follow-up. Int J Oral Implantol Clin Res; 8(1): 17-21.
Esteve-Pardo G and Esteve-Colomina L (2018). Clinical Application of the Socket-Shield Concept in Multiple Anterior Teeth. Case Reports in Dentistry; Article ID 9014372, 7 pages https://doi.org/10.1155/2018/9014372.
Fonseca DL (2018). Incorporating the socket-shield technique in the esthetic treatment of a patient’s smile: A case report with 2-year follow-up. Int J Growth Factors Stem Cells Dent; 1: 38-41.
Germi AS, Barghi VG, Jafari K et al. (2020). Aesthetics outcome of immediately restored single implants placed in extraction sockets in the anterior maxilla: A case series study. J Dent Res Dent Clin Dent Prospect; 14(1): 48-53| doi: 10.34172/joddd.2020.007
Glocker M, Attin T and Schmidlin P (2014). Ridge preservation with modified Socket- Shield technique: a methodological case series. Dentistry J; 2(1): 11–21.
Gluckman H, Nagy K and Toit JD (2019). Prosthetic management of implants placed with the socket shield technique. J Prosthet Dent; 121(4): 581–585
Gluckman H, Salama M and Toit JD (2016). Partial extraction therapies (PET) Part 1: Maintaining alveolar ridge contour at pontic and immediate implant sites. Int J Periodontics Restorative Dent; 36: 681‑7.
Gluckman H, Salama M and Toit JD (2018). A retrospective evaluation of 128 socket-shield cases in the aesthetic zone and posterior sites: partial extraction therapy with up to 4 years follow-up. Clin Implant Dent Relat Res. 2018;20:122-129.
Gluckman H, Toit G, and Salama M (2016a). The pontic-shield: partial extraction therapy for ridge preservation and pontic site development. The International Journal of Periodontics & Restorative Dent; 36(3): 417–423.
Guo T, Nie R, Xin X, et al. (2018). Tissue preservation through socket-shield technique and platelet-rich fibrin in immediate implant placement: a case report. Medicine; 97: e1375.
Habashneh RA and Walid MA (2019). Socket-shield Technique and Immediate Implant Placement for Ridge Preservation: Case Report Series with 1-year Follow-up. J Contemp Dent Pract; 20(9): 1108–1117
Han CH, Park KB and Mangano FG (2018). The modified socket shield technique. J Craniofac Surg; 29: 224
HANA SA and OMAR OA (2020). SOCKET SHIELD TECHNIQUE FOR DENTAL IMPLANTS IN THE ESTHETIC ZONE, CLINICAL AND RADIOGRAPHICAL EVALUATION. Journal of University of Duhok; 32(1): 69-81. https://doi.org/10.26682/sjuod.2020.23.1.8
Hinze M, Janousch R, Goldhahn S et al. (2018). Volumetric alterations around single-tooth implants using the socket-shield technique: preliminary results prospective case series. Int J Esthet Dent;13: 146-170.
Hu C, Lin W, Gong T, et al. (2018). Early Healing of Immediate Implants Connected with Two Types of Healing Abutments. Implant Dent; 27(6): 646-52.
Huang H, Shu L, Liu Y et al. (2017). Immediate Implant Combined with Modified Socket-Shield Technique: A Case Letter. Journal of Oral Implantology; Vol. XLIII (2): 139-143.
Hurzeler MB, Zuhr O, Schupbach P et al. (2010). The socket-shield technique: a proof-of-principle report. J Clin Periodontol; 37: 855–862.
Kumar PR and Kher U (2018). Shield the socket: procedure, case report and classification. J Indian Soc Periodontol; 22: 266-272
Lagas LJ, Pepplinkhuizen JJFAA, Berge SJ et al. (2015). Implant placement in the aesthetic zone: the socket-shield-technique. Ned Tijdschr Tandheelkd; 122: 33–36.
Magadmi RM (2021). Assessing the Clinical Improvement in Patients with COVID-19 using Lopinavir-Ritonavir: A Systematic Review. Journal of Pharmaceutical Research International; 33(44A): 448-459; Article no.JPRI.74217.
Mangano C, Levrini L, Mangano A et al. (2014a). Esthetic evaluation of implants placed after orthodontic treatment in patients with congenitally missing lateral incisors. Journal of Esthetic and Restorative Dentistry 26: 61–71.
Mangano FG, Mastrangelo P, Luongo F et al. (2016). Aesthetic outcome of immediately restored single implants placed in extraction sockets and healed sites of the anterior maxilla: a retrospective study on 103 patients with 3 years of follow-up. Clin Oral Impl Res; 1–11 doi: 10.1111/clr.12795
Mathew L, Manjunath N, Anagha N P et al. (2020). Comparative Evaluation of Socket Sield and Immediate Implant Placement. International Journal of Innovative Science and Research Technology; 5(4): 1364-9
Mattar AA (2018). Socket Shield Technique with Immediate Implant Placement to Preserve thin Buccal bone: A Case Report. Int J Dent & Oral Heal; 4(8): 117-122.
Mitsias ME, Siormpas KD, Kotsakis GA et al. 2017). The root membrane technique: human histologic evidence after 5 years of function. Biomed Res Int; 20:1-8.
Moher D., Liberati A., Tetzlaff J. et al. (2009). PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med; 6: e1000097.
Mourya A, Mishra SK, Gaddale R et al. (2019). Socket‑shield technique for implant placement to stabilize the facial gingival and osseous architecture: A systematic review. J Investig Clin Den; 10: e12449.
Nguyen VG., Flanagan D., Syrbu J. et al. (2020). Socket Shield Technique Used in Conjunction with Immediate Implant Placement in the Anterior Maxilla: A Case Series. Clin. Adv. Periodontics; 10; 64–68.
Nisar N, Nilesh K, Parkar MI et al. (2020). Extraction socket preservation using a collagen plug combined with platelet-rich plasma (PRP): A comparative clinico-radiographic study. J Dent Res Dent Clin Dent Prospects.; 14(2): 139–145. Doi: 10.34172/joddd.2020.028
Ogawa T., Sitalaksmi RM., Miyashita M. et al. (2021). Effectiveness of the Socket Shield Technique in Dental Implant: A Systematic Review. J. Prosthodont. Res. doi: 10.2186/jpr.JPR_D_20_00054.
Oliveira GBD, Basilio MDA, Araujo NS et al. (2021). The socket-shield technique and early implant placement for tooth rehabilitation: A case report. J Clin Images Med Case Rep; 2(3): 1118.
Pagni G, Pellegrini G, Giannobile MV et al. (2012). Post extraction Alveolar Ridge Preservation: Biological Basis and Treatments. International Journal of Dentistry; Article ID 151030, 13 pages
Patel S, Parikh H, Kumar BB et al. (2019). Socket shield technique, a novel approach for the esthetic rehabilitation of edentulous maxillary anterior alveolar ridges: A special case file. J Dent Implant; 9:91-4.
Petsch M, Spies B and Kohal RJ (2021). Socket shield technique for implant placement in the esthetic zone: a case report. Int J Periodontics Restorative Dent; 37:853-860.
Polis-Yanes C, Cadenas-Sebastián C and Oliver-Puigdomenech C (2020). A Double Case: Socket Shield and Pontic Shield Techniques on Aesthetic Zone. Case Reports in Dentistry, Article ID 8891772, 6 pages
POUR RS, ZUHR O, HURZELER M et al. (2017). Clinical Benefits of the Immediate Implant Socket Shield Technique. Journal of Esthetic and Restorative Dent; 17: 1-8.
Roe P, Kan JYK and Rungcharassaeng K (2017). Residual root preparation for socket-shield procedures: a facial window approach. IJ Esthet Dent; 12: 324-35.
Saeidi Pour R, Zuhr O, Hürzeler M, et al. (2017). Clinical benefits of the immediate implant socket shield technique. J Esthet Restor Dent; 29:93-101.
Schwimer CW, Gluckman H, Salama M et al. (2019). The socket-shield technique at molar sites: a proof-of-principle technique report. J Prosthet Dent; 121:229-233.
Shaheen RS (2021). Partial extraction therapy: A review of the clinical and histological human studies. Int J Prev Clin Dent Res; 8:16-9.
Siormpas KD, Mitsias ME, Kotsakis GA et al. (2018). The root membrane technique: a retrospective clinical study with up to 10 years of follow-up. Implant Dent; 27:564-574.
Srivastava PA, Kusum CK, Aggarwal S et al. (2021). Immediate esthetic restoration of failed teeth in esthetic zone using socket shield technique: A case report. Inter J Applied Dent Sciences; 7(2): 374-376.
Sun C, Zhao J, Liu Z et al. (2020). Comparing conventional flap-less immediate implantation and socket-shield technique for esthetic and clinical outcomes: A randomized clinical study. Cli Ora Imp Res; 31: 181–191.
Troiano M, Benincasa M, Snchez P (2018). Bundle bone preservation with Root-T-Belt: Case study. Annals of Oral & Maxillofacial Surgery, Apr 12;2(1):7.
Verma N, Lata J and Kaur J (2018). Socket shield technique‐a new approach to immediate implant placement. Indian Journal of Comprehensive Dental Care; 8:1181-1183.
Zhao X, Qiao SC, Shi JY et al. (2016). Evaluation of the clinical and aesthetic outcomes of Straumann Standard Plus implants supported single crowns placed in nonaugmented healed sites in the anterior maxilla: a 5–8 years retrospective study. Clinical Oral Implants Research 27: 106–112.
Zhu YB, Qiu LX, Chen L et al. (2018). Clinical evaluation of socket shield technique in maxillary anterior region. Zhonghua Kou Qiang Yi Xue Za Zhi; 53: 665-668
Zuhr O, Staehler P and Hurzeler M (2020). Complication management of a socket shield case after 6 years of function. Int J Periodontics Restor Dent; 40: 409-15.


