1Department of Pathology, College of Medicine, Majmaah University, Majmaah 11952, Saudi Arabia,
2Department of Community Medicine, College of Medicine, Majmaah University, Majmaah 11952, Saudi Arabia,
3Department of Basic Science, College of Medicine, Majmaah University, Majmaah 11952, Saudi Arabia
4Department of Mechanical Engineering, College of Engineering, Majmaah University, Majmaah 11952, Saudi Arabia
Corresponding author Email: ubghaffar@gmail.com
Article Publishing History
Received: 17/07/2019
Accepted After Revision: 18/09/2019
Medical education aims to provide valuable knowledge through effective learning and teaching strategies to students so that they can become competent caregivers. This study seeks to determine students’ perception regarding those strategies and preferences for different available teaching methodologies. This is an observational, cross-sectional, and institution-based study conducted using a pre-structured, pre-validated, close-ended questionnaire. Three hundred fifty students participated in the study. Most of the students (78.3%) preferred interactive lecture through multimedia which was perceived to be the most effective method of delivery. More than 45% respondents considered the use of PowerPoint presentations as an efficient tool and 58% considered the multiple-choice question format in examination as the best evaluation method as compared to essay questions. Student’s perceptions should be evaluated further through longitudinal and follow up studies which could help in corroborating their effectiveness. This would help in bridging the gap between the knowledge taught and gained by the students, thus improving academic excellence and reducing average outcomes.
Lecture, Medical Education, Multimedia, Medical Students, Seminars
Ghaffar U. B, Ahmed S. M, Faraz A, Salar B. M. K. M, Hussain S, Khan M. N. Students Perception of Teaching Methodologies Practiced in an Academic Institution in Majmaah, Saudi Arabia: A Unified Perspective. Biosc.Biotech.Res.Comm. 2019;12(3).
Ghaffar U. B, Ahmed S. M, Faraz A, Salar B. M. K. M, Hussain S, Khan M. N. Students Perception of Teaching Methodologies Practiced in an Academic Institution in Majmaah, Saudi Arabia: A Unified Perspective. Biosc.Biotech.Res.Comm. 2019;12(3). Available from: https://bit.ly/2lBlmIG
Copyright © This is an Open Access Article distributed under the Terms of the Creative Commons Attribution License (CC-BY). https://creativecommons.org/licenses/by/4.0/, which permits unrestricted use distribution and reproduction in any medium, provided the original author and sources are credited.
Introduction
The arena of medicine is a very competitive field, and medical students encounter various teaching strategies over the course of their studies.. Medical institutions worldwide face the challenge of catering to a growing student population while maintaining the quality of education. Teacher-centered and student-centered approaches are broad categories of approaches to education. Lecture is a conventional teacher-focused strategy, though in a student-focused approach, students play a functional role in learning and concentrate on deep thinking (Lida and Mona, 2013). The introduction of technology in education has changed the way that ideas are delivered and conveyed. Electronic media like PowerPoint is becoming more and more popular in medical institutions (Muttappallymyalil et al, 2016). Research about efficient teaching techniques is a pressing issue, and the implications of this research can shape the nature of education (Jafri and Keramati, 2012, Withers et al 2016, ,AyeMon et al 2014, Raj and Kanagasabapathy, 2019).
Student evaluations of teaching methodologies contribute significantly to improving teaching standards. Students are the end beneficiaries of education, and their opinions regarding teaching methods are indicators of their satisfaction with a particular learning experience (Withers et al, 2016; Theall and Franklin, 2001). Papanna et al (2013) conducted a study involving 286 students and found that problem-based learning (PBL) was most favored (71.4%), while didactic lectures were the least preferred (32.8%). Blackboard was observed to be another favored teaching aid, preferred by 46.9% of students (Papanna et al, 2013). Salwani et al (2014) conducted a study involving 50 students. In his study, 72% of students chose lecture as the most-preferred teaching and learning method, tutorials were preferred by 10% of students, while 6% of students preferred PBL and practical respectively (Salwani et al, 2014). Atif et al (2011) conducted a study involving 200 students and found that 40% of the students favored PowerPoint presentations as a reliable mode of teaching as it was interesting and interactive as compared to PBL (28.8%), audio-visual aids (18.6%), and Whiteboard (12%). Shreemanta et al (2013) conducted a study among 337 students and found that 77.02% selected standard lectures as the most efficient mode of teaching, followed by group discussion (68.02%), tutorials (58.94%), and seminars (49.05%) (Shreemanta et al, 2013).
Therefore, this study aims to evaluate the perceptions and preferences of students regarding various learning methodologies used in medical colleges. Evaluating students’ opinions can help address student learning issues, identify students’ preferred learning methods, and help teachers improve the efficiency of their teaching. The findings of this study will help overcome deficiencies in medical education and improve the credibility of medical graduates as future caregivers.
Material and Methods
This is an observational, cross-sectional, and institution-based study employing a pre-validated, close-ended questionnaire. A total of 350 students participated in the study. The participants were all MBBS students at various stages of their studies. Approval for the study was granted by the ethical and research committee, allowing the participants to be approached for the study. Informed consent was obtained from every student and confidentiality was assured. A carefully designed questionnaire comprised of four sections was distributed among the students. In the first section, they were instructed to indicate their unbiased opinion regarding various teaching methods on a Likert scale ranging from 1–5 (1 = strongly disagree to 5 = strongly agree). The respondents were asked to select the option that they believed was most appropriate. In the second section, they were encouraged to propose the reason they preferred a particular teaching method. The third section consisted of questions regarding students’ preferences for various teaching aids, including PowerPoint, Blackboard, various other audio-visual aids, and problem-based discussions. Finally, the fourth part was framed to elicit responses regarding student preferences for various evaluation methods used in examinations on a Likert scale ranging from 1–5 (1 = strongly disagree to 5 = strongly agree). There were clear instructions to participants not to disclose their identity nor to write any individualized remarks about staff members. Responses were collected from students within a time-bound period. On the basis of analysis and observation, results were extrapolated and were compared with other relevant literature.
Results and Discussion
Undergraduate medical education is undergoing major changes, and efforts are being made to make it more interesting (Desy et al, 2017). In our study, the majority of the medical students strongly agreed or agreed that teacher-centered approaches were better than student-centered approaches. Teacher-centered activities were defined as conventional lectures, whereas student-centered activities were teaching methodologies that promoted active student participation, such as small-group discussions, tutorials, and seminars prepared and delivered by students (Kim and Hwang, 2017). The student-centered approach has challenged the traditional role of teachers as experts in their field who thus determine how and what a student needs to learn (Vizeshfar and Torabizadeh, 2018).
Regarding the results of the first section of the questionnaire, which addressed students’ preferred teaching methods, 78.3% of students favored lecture, followed by small-group discussion (60%) and tutorials (46.9%). Seminar was the least popular teaching method (44.9%).
Table 1: Preference for Teaching Methods
| Teaching method | Strongly Agree
(5) |
Agree
(4) |
Neutral
(3) |
Disagree
(2) |
Strongly disagree
(1) |
Mean Likert- scale score |
| Lecture | 83 (23.7%) | 191 (54.6%) | 50 (14.3%) | 16 (4.5%) | 10 (2.9%) | 3.9 |
| Seminars | 46 (13.2%) | 111 (31.7%) | 99 (28.3%) | 54 (15.4%) | 40 (11.4%) | 3.1 |
| Small-group discussion | 78 (22.3%) | 132 (37.7%) | 60 (17.2%) | 54 (15.4%) | 26 (7.4%) | 3.5 |
| Tutorial | 50 (14.3%) | 114 (32.6%) | 88 (25.1%) | 68 (19.4%) | 30 (8.6%) | 3.2 |
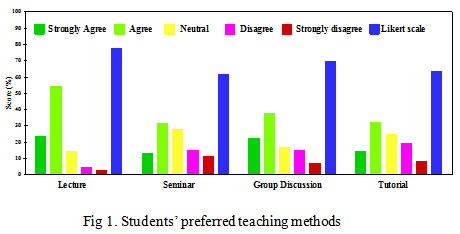 |
Figure 1: Students’ preferred teaching methods |
The participants in our study favored lectures because they felt that they are more informative, their delivery by content experts with good communication skills and grasp of the subject matter made them interesting and beneficial, and students received more attention in these. This result is similar to those of the studies conducted by Zinski et al (2017); El-Belbasy et al (2018); and Stirling (2017). In contrast, the studies conducted by Schwartzstein and Roberts (2017); Ramnanan and Pound (2017); Abdul et al (2015); and Vimal et al (2015) showed that e – learning, flip method teaching and also small group discussion (as shown in fig. 2) were the preferred teaching mode. This is because they feel that it could enhance students’ reasoning, gives them the opportunity to provide their opinion, a good stage for student-teacher cooperation and develops confidence.
Table 2: Comparative overview of findings on student teaching-method preferences
| Teaching Method | This
study |
Shreemanta
et al |
Salwani
et al. |
Vimal
et al |
Abdul
et al |
Papanna
et al. |
| Lecture | 78.3% | 77% | 72% | 67% | 59.1% | 32.8% |
| Seminar | 44.9% | 49% | – | 48% | 54.3% | – |
| Small group discussion | 60% | 68% | 6% | 89% | 80% | 71.4% |
| Tutorial | 46.9% | 58.9% | 10% | 57% | – | – |
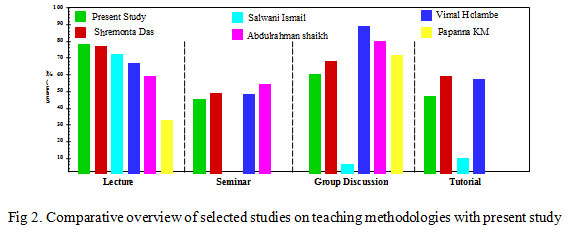 |
Figure 2: Comparative overview of selected studies on teaching methodologies with present study. |
Figure 3 shows that small-group discussions were the selected as the best for interactive participation (36%). Tutorials scored highly for being informative (25.7%), and seminars scored highly for confidence-building (36.6%).
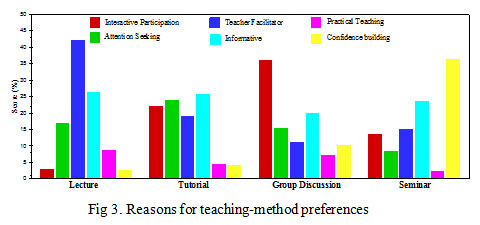 |
Figure 3: Reasons for teaching-method preferences |
Figure 4 shows a graphical representation of the teaching tools included in our study. Many students, 48% and 46.6% of the participants, responded that PowerPoint was the best tool for learning and teaching, as it provides a better learning experience. A study conducted by Shigli et al (2016) concluded that PowerPoint presentations deliver a multisensory experience, foster better understanding of charts, diagrams, tables, and various other concepts and helps improve memory. McBride and Drake (2017) in their research, found an increase of 24% to 29% in classroom attendance as compared to a similar study done Aye Mon et al (2014).
PBL was the second most-favored teaching tool, with 26.3% respondents stating it to be their preferred learning method. A study conducted by Merritt et al (2017) showed that PBL increased students’ enthusiasm as it upgraded their reasoning skills, academic achievement, knowledge retention, conceptual development and attitude.
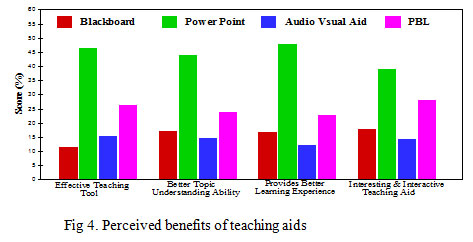 |
Figure 4: Perceived benefits of teaching aids |
Figure 5 describes students’ preferred evaluation methods. The majority chose multiple-choice questions (MCQs) (58.6%), followed by short essay questions (52.3%). Long essay questions were rated the worst evaluation method, as only 6.2% of students strongly agreed with this method of evaluation. The finding is similar to a finding in a study (Ibrahim et al, 2015) conducted at King Abdul Aziz University in Jeddah, wherein the majority preferred MCQs as their assessment procedure of choice. Contrary to our findings, Lalvarmawi et al (2015) found that majority of the students preferred revision cum self-study, tutorials, and terminal exams These students, for whom English is their first language, do not experience the language problem faced by Saudi students. Our participants’ mother tongue is Arabic, and they find it difficult to express themselves. Therefore, assessment approaches in Saudi Arabia need to be designed according to regional preferences.
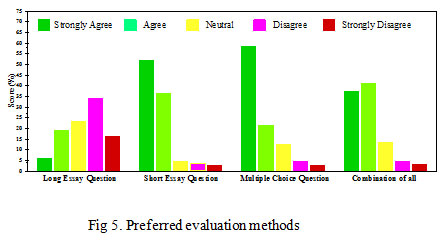 |
Figure 5: Preferred evaluation methods |
Conclusion and Recommendation
This study revealed that lecture-style teaching accompanied by the use of additional aids such as multimedia software presentations was the method most preferred by the participants. Participants emphasized that its benefits include increasing the clarity of teaching materials and offering a more engaging presentation style. They also welcomed the opportunity to have more interactive sections or student involvement during lectures. Therefore, we recommend that several similar studies be conducted among the wider community of medical students to discover innovative and effective educational interventions that will benefit medical students through identifying their concerns and preferences and formulating an action plan suited to their needs.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflicts of interest
The authors declare that there is no conflict of interests regarding the publication of this paper.
Acknowledgements
The authors gratefully acknowledge the kind suport from the Research Committee, College of medicine, Majmaah University, Majmaah, Saudi Arabia without which this project would not have been possible.
References
Abdul, R.S., Abida, S., Muhammad, Y.A.(2015). Student’s Preferences for Modes of Teaching in Basic Medical Sciences. Journal of Rawalpindi Medical College,19(1),93-95.
Atif, M., Fahmida, K., Mukarram A., Saima E., Kamran A., Masood, A. Q.(2011). Perception and Preferences of Undergraduate Medical Students Regarding the Use of Contemporary Teaching Aids at Dow International Medical College, Karachi. J Dow Univ Health Sci,; Vol. 5(1),34-36.
Aye Mon, Amirah, F., Chang,W.Y, Mohamad, A.B, Paw, L.J., Tai, K.L.(2014). Learning style preferences among pre-clinical medical students. J Med Allied Sci.,4(1):22-27.
Barman, A., Jaafar, R., Naing.(2006). Perception of students about the problem- based learning sessions conducted for medical and dental schools’ students of University Sains Malaysia. Educ Health; 19(3),363-366.
Desy, J.R., Reed, D.A. & Wolanskyj, A.P.(2017). Milestones and millennials: a perfect pairing—competency-based medical education and the learning preferences of generation. In Mayo Clinic Proceedings, Vol. 92,(2), 243-250.
El-Belbasy, R., Abo-Elmagd, E.K., & Abd-Rabo, M.(2018). Medical Students’ Attitude and Perception towards Basic Medical Sciences in the Faculty of Medicine for Girls, Al-Azhar University: A Study Prior to the Integrated Program. Egyptian Journal of Hospital Medicine; 70(12),24-31.
Haidet, P., Stein H.F.(2006). The role of the student-teacher relationship in the formation of physicians-The hidden curriculum as process. J Gen Intern Med21, Suppl:16-20.
Ibrahim, N.K., Al-Sharabi, B.M., Al-Asiri, R.A., Alotaibi, N.A., Al-Husaini, W.I., Al-Khajah, H. A., Rakkah, R.M., Turkistani, A. M.(2015). Perceptions of clinical years’ medical students and interns towards assessment methods used in King Abdulaziz University, Jeddah. Pakistan Journal of Medical Sciences,1(4),757-762.
Jafari, H., Keramati, E.(2012). Attitudes of faculty about relationship between educational and research activities. Quarterly journal of research and planing in higher education, 64, 1-17.
Kim, K.J., Hwang, J.Y.(2017). Characteristics of medical teachers using student-centered teaching methods. Korean J Med Educ,29(3),187-191.
Lalvarmawi, F., Banik, U., & Devi, M.A. (2015). Feedback of medical students on teaching and evaluation methodology in physiology. National Journal of Physiology, Pharmacy and Pharmacology, 5(1),36-42.
Lida, J., Mona, N.(2013). Evaluation of teaching through lecture with new methods of student-centered teaching in medical students. Future of Medical Education Journal, Vol 3(4), 6-9.
Mattick, K., Bligh, J.(2006). Teaching and assessing medical ethics: where are we now?. J Med Ethics, 32(3),181–185.
McBride, J.M., and Drake, R.L.(2018). National survey on anatomical sciences in medical education. Anatomical sciences education, 11(1),7-14.
Merritt, J., Lee, M.Y., Rillero, P. & Kinach, B.M. (2017). Problem-based learning in K–8 mathematics and science education: A Literature review. Interdisciplinary Journal of Problem-Based Learning, 11(2),3-15.
Muttappallymyalil, J., Mendis, S., John, L.J., Shanthakumari, N., Sreedharan, J., Shaikh, R.B., (2016). Evolution of technology in teaching: Blackboard and beyond in Medical Education. Nepal J Epidemiol.,6(3),588-592.
Papanna, K.M., Kulkarni, V., Tanvi, D., Lakshmi, V., Kriti, L. B., Unnikrishnan, A.S., Tejesh, S., Sumit, K.S.(2013). Perceptions and preferences of medical students regarding teaching methods in a Medical College, Mangalore India. African Health Sciences, vol 13(3),808-813.
Qamar, M.R., Ahmad, A., Niaz, K.(2015). Small Group Discussion Vs Didactic Lectures. Pak Armed Forces Med J, 65(3),386-90.
Raj, S., & Kanagasabapathy, S.(2019). Relationship between gender and learning style preferences- A study among undergraduate medical students in South India. Journal of Evolution of Medical and Dental sciences, 8(19), 1550-1554.
Ramnanan, C.J., & Pound, L.D., (2017). Advances in medical education and practice: student perceptions of the flipped classroom. Advances in Medical Education and Practice, 8, 63-73.
Salwani, I., Nor Iza, A. R., Nasir, M., Norhasiza, M. J., Aminatul, I. B. H. (2014). Preference of teaching and learning methods in a new medical school of Malaysia. Journal of Applied Pharmaceutical Science,4(2), 48-55.
Schwartzstein, R.M., & Roberts, D.H.,(2017). Saying goodbye to lectures in medical school—Paradigm Shift or Passing Fad?. New England Journal of Medicine, 377(7),605-607.
Shigli, K., Agrawal, N., Nair, C., Sajjan, S., Kakodkar, P., Hebbal, M.(2016). Use of PowerPoint presentation as a teaching tool for undergraduate students in the subject of gerodontology.
J Indian Prosthodont Soc,16,187-192.
Shreemanta, K. D., Shubhransu P., Basant, K. B.(2013). Teaching Methods and Its Efficacy: An Evaluation by the Students. J Indian Acad Forensic Med, vol. 35(4),321-324.
Stirling, B.V. (2017). Results of a study assessing teaching methods of faculty after measuring student learning style preference. Nurse education today, 55,107-111.
Theall, M., & Franklin, J.(2001). Using technology to facilitate evaluation. New Directions for Teaching and Learning, 88, 41-50.
Vimal, M. H., Namrata, A.T., Purushottam, A G.(2015). Student’s preferences for learning in medical education. International Journal of Community Medicine and Public Health, 2(3),328-330.
Vizeshfar, F. & Torabizadeh, C., (2018). The effect of teaching based on dominant learning style on nursing students’ academic achievement. Nurse education in practice, 28,103-108.
Warriner, D.R., Bayley, M., Shi, Y., Lawford, P.V., Narracott, A. & Fenner, J.( 2017). Computer model for the cardiovascular system: development of an e-learning tool for teaching of medical students. BMC Medical Education, 17(1), 220.
Withers, M., Press, D., Wipfli, H., McCool, J., Chan, C., Jimba, M., Tremewan, C., Samet, J. (2016). Training the next generation of global health experts: experiences and recommendations from Pacific Rim universities. Global Health.,12(1),34.
Zinski, A., Blackwell, K.T.P.W., Belue, F.M. & Brooks, W.S.(2017). Is lecture dead? A preliminary study of medical students’ evaluation of teaching methods in the preclinical curriculum. International Journal of Medical Education, 8,326-333.


