Saveetha Dental College and Hospital, Saveetha Institute of Medical and
Technical Sciences, Chennai, Tamil Nadu, India.
Corresponding author email: dr.mathewthomasm@gmail.com
Article Publishing History
Received: 25/09/2021
Accepted After Revision: 26/12/2021
This study was designed with the aim to evaluate the effect of curing time on the shear-bond strength of orthodontic brackets bonded using light cure Resin-Modified Glass Ionomer Cements (RMGIC). This class of cement when used for luting orthodontic brackets offers certain advantages when compared to the more commonly used resin cements. Intact natural teeth (premolars) extracted for therapeutic purposes as part of orthodontic treatment was sourced for use in this study. The teeth were equally divided into four groups four testing, Group 1 – brackets bonded with RMGIC and cured for 3 seconds, Group 2 – brackets bonded RMGIC and cured for 6 seconds, Group 3 – brackets bonded with RMGIC and cured for 9 seconds and Control group – brackets bonded with composite and cured for 15 seconds.
A high intensity LED light source was used to cure the cements. The Shear-Bond strength of the brackets was evaluated using a universal testing machine. One-way ANOVA test and Tukey multiple comparison tests were done to compare the difference of Shear-Bond Strengths among the groups tested. The average Shear Bond Strength among study groups was 7.64±2.86 MPa. The ANOVA and Tukey multiple comparison tests could not identify a statistically significant difference in Shear-Bond Strengths among the groups. Curing time does not appear to have a statistically significant effect on the Shear Bond Strength of orthodontic brackets bonded using Resin-Modified Glass Ionomer Cements.
Bonding, Light-Cure, Light Intensity, Resin–Modified Glass
Ionomer Cement, Shear–Bond Strength.
Maliael M. T, Dinesh S. P. S. Effect of Curing Time on the Bond Strength of Orthodontic Brackets Bonded by Light Cure Resin-Modified Glass Ionomer Cement: An In Vitro Evaluation. Biosc.Biotech.Res.Comm. 2021;14(4).
Maliael M. T, Dinesh S. P. S. Effect of Curing Time on the Bond Strength of Orthodontic Brackets Bonded by Light Cure Resin-Modified Glass Ionomer Cement: An In Vitro Evaluation. Biosc.Biotech.Res.Comm. 2021;14(4). Available from: <a href=”https://bit.ly/3ryNBHE“>https://bit.ly/3ryNBHE</a>
Copyright © Maliael and Dinesh This is an open access article distributed under the terms of the Creative Commons Attribution License (CC-BY) https://creativecommns.org/licenses/by/4.0/, which permits unrestricted use distribution and reproduction in any medium, provide the original author and source are credited.
INTRODUCTION
Two important discoveries in orthodontics, Buonocore’s discovery of the acid-etch technique and Miura and Newman’s orthodontic bonding, transformed the field (Rossouw 2010; Graber et al. 2016). These steps simplified orthodontic practise while increasing clinical efficiency and effectiveness. It also aided in increasing orthodontic treatment acceptance and set the way for future improvements in the field. Light-cure orthodontic bonding materials were developed at the end of the 1970s (Eliades 2010).
These materials presented a number of advantages over self-cure materials, including the ability to control working time, enhanced bracket placement precision, ease of removal of excess material, reduced risk of field contamination, and the ability to engage the arch-wire right away (Sfondrini et al. 2002; Sfondrini et al. 2004; Graber et al. 2016; Shen et al. 2021).
Glass Ionomer Cements (GICs) were presented as an alternative to resin adhesives in orthodontics. They were less moisture sensitive, could attach to both enamel and metal, released fluoride, and reduced iatrogenic enamel damage caused by orthodontic treatment (Fukino and Komori 2015; Sidhu and Nicholson 2016). In comparison to resin composites, GICs showed low early mechanical strength and bond strength. Resin components were added to GICs to improve their properties. When compared to conventional GICs, this new material, Resin Modified Glass Ionomer Cement (RMGICs), showed better bond strengths (Owens and Miller 2000; Shen et al. 2021).
Despite being clinically significant, the bond strength was still lower than that of resin adhesives. For polymerization of adhesives, Light Emitting Diodes (LEDs) based on semiconductors produced from gallium nitride (GaN) are used. Compared to traditional curing lamps, LED lamps provide a number of advantages (Huang et al. 2017).
Increased lamp life, consistent light intensity, impact resistance, lack of heat generation avoiding pulpal damage, a coincidence of peak irradiance of light with camphorquinone, lightweight design and improved ergonomics, low power consumption translating to longer usage between charges and increased battery life, and monochromatic light output are just a few of the benefits (Nicholls 2000; Dunn and Taloumis 2002; Mills et al. 2002; Wiggins et al. 2004; Leprince et al. 2010; Shen et al. 2021).
Various studies utilized Shear-Bond Strength(SBS) as a method to evaluate and assess the strength of bracket bonding systems (Sfondrini et al. 2002; Uşümez et al. 2004; Gronberg et al. 2006; Sfondrini et al. 2006; Bishara et al. 2007; Turk et al. 2007; Yu et al. 2007; Cerekja and Cakirer 2011; Sağır et al. 2013; Graber et al. 2016; Shen et al. 2021). No previous research has employed high-intensity LED curing lamps to cure the luting cements to evaluate the SBS.
Furthermore, previous research has only looked at the SBS of resin cements used for luting orthodontic brackets, with no study of the SBS of RMGIC used for luting orthodontic brackets with a high intensity light source. As a result, the goal of this research is to see how curing time affects the shear-bond strength of orthodontic brackets bonded with light cure Resin Modified Glass Ionomer Cement that is cured with a high-intensity LED light source.
MATERIAL AND METHODS
To estimate the sample size, a similar study in the literature was identified. The sample size was calculated using the G*Power statistical power analysis software version 3.0.10 (Heinrich-Heine-Universität, Düsseldorf). A total sample size of 24 was calculated to have 95% power to detect a difference in means between the groups (Dall’Igna et al. 2011).
A total of 24 premolars were extracted as part of orthodontic treatment were sourced for the study. The teeth were preserved in a formalin solution for 24 hours following extraction, later these teeth were stored saline until they were to be used in the study (Lee et al. 2007; NawrockaA and ukomska-SzymaskaA 2019).
The teeth were then cleaned and mounted onto custom fabricated acrylic mounting jigs. Pumice paste was used to polish the bonding site, etched the teeth for 30 seconds with 37% phosphoric acid, washed for 10 seconds with distilled water, and air-dried for 10 seconds (Gaard and Fjeld 2010; Graber et al. 2016; Shen et al. 2021).
The teeth were randomly divided into 4 groups (n=6). In the Control group, Ortho Solo™ (Ormco Corporation, Orange, CA, USA) bonding agent was applied to the etched enamel and light-cured for 10 seconds. Enlight Light Cure adhesive (Ormco Corporation, Orange, CA, USA) was applied to the bracket base of a premolar bracket (Empower® 2 Self-ligating metal bracket; American Orthodontics, WI, USA).
A stainless-steel bracket holding tweezer was then used to place the bracket on the tooth, with enough pressure used to allow the extra resin to gather at the bracket’s edges. The brackets were cured for 15 seconds using the light cure equipment after the extra material was removed (Graber et al. 2016; Shen et al. 2021).
The RMGIC material (GC Fuji ORTHOTM LC, Resin-reinforced light cure orthodontic cement; GC America Inc, USA) was mixed and coated on the bracket base in the proportions prescribed by the manufacturer for the study groups. A bracket holding tweezer was used to place the brackets on the teeth, and enough pressure was applied to allow the excess cement to be collected from the bracket borders. The brackets were cured after the excess cement was removed.
Brackets in group 1 were cured for 3 seconds, brackets in group 2 for 6 seconds, and brackets in group 3 for 9 seconds. The manufacturer recommended a curing period of 10 seconds for the RMGIC used in the study. According to the manufacturer’s specs, the light cure unit employed (iLed Curing Light; Guilin Woodpecker Medical Instrument Co., Ltd, PRC) had an overall light output intensity of![]() and a wavelength range of (420nm – 480nm). The TURBO P1 high-intensity mode was used in our research, with an output light intensity of
and a wavelength range of (420nm – 480nm). The TURBO P1 high-intensity mode was used in our research, with an output light intensity of
 (Almeida et al. 2021).
(Almeida et al. 2021).
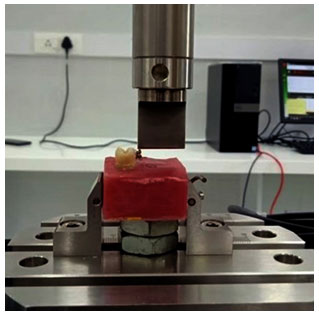
The teeth were then immersed for 24 hours in distilled water at 37°C. At a crosshead speed of 0.5mm/min, the teeth were then subjected to SBS testing on a universal testing machine (Instron® Corporation, MA, USA) (Figure 1). The peak load failure rate was divided by the specimen surface area to get SBS values in megapascals (MPa).
The SBS values were compared between the groups using analysis of variance (ANOVA) and Tukey multiple comparison tests. IBM® SPSS® Statistics software version 23 was used to tabulate and process the data (International Business Machines Corporation, NY, USA). The study’s protocol was approved by the institutional scientific review board.
Figure 1: The SBS of the bonded bracket being tested on the universal testing machine
(Photograph taken by the primary investigator taken during testing).
RESULTS AND DISCUSSION
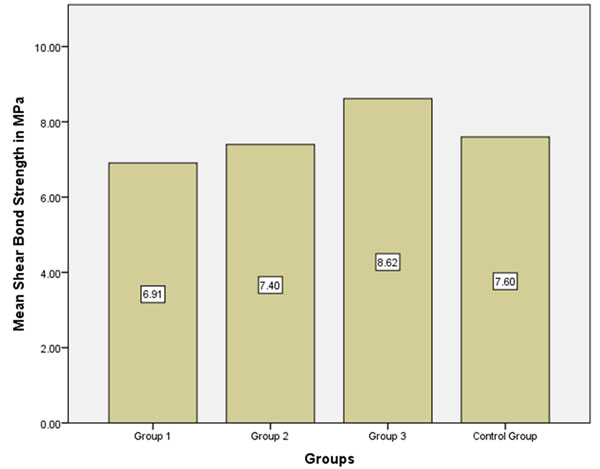
The overall average SBS among study groups was found to be 7.64±2.86 MPa. In Group 1, the average SBS was found to be 6.91±3.22 MPa. In Group 2, the average SBS was found to be 7.40±2.91 MPa. In Group 3, the average SBS was found to be 8.62±1.67 MPa. In the Control group, the average SBS was found to be 7.60±1.06 MPa (Figure 2). The ANOVA showed a that there wasn’t a statistically difference in SBS among the four groups evaluated in the study (Table 1). The Tukey multiple comparison tests did not identify any statistically significant difference in the SBS among the groups.
The results of the present study showed that there was a meagre increase in the SBS with the increase in curing time, however, the ANOVA and Tukey comparison tests weren’t able to determine statistical significance in the SBS among the groups. The increase in SBS with the increase in curing time could be probably due to the increased polymerization that occurs with the increased light-curing time. Such an observation was made by various authors in the case of light cured-resin cements (Uşümez et al. 2004; Mavropoulos et al. 2005; Peutzfeldt and Asmussen 2005; Staudt et al. 2005; Yu et al. 2007; Shen et al. 2021).
Table 1. ANOVA test to compare means SBS among the groups. The test shows that the
difference of SBS among the groups is not significant statistically.
| Sum of Squares | Df | Mean Square | F | Sig. | |
| Between Groups | 9.308 | 3 | 3.103 | 0.456 | 0.716 |
| Within Groups | 135.991 | 20 | 6.800 | ||
| Total | 145.300 | 23 |
Figure 2: Bar Graph representing the average SBS of the study groups
(Graph generated from SPSS post statistical analysis of the data obtained from testing).
The primary objective of this study was to identify whether curing brackets bonded with RMGICs with the use of high-intensity modes on LED curing lamps that have shorter curing cycles would affect the SBS of these brackets. The shorter curing cycles can increase clinical efficiency and reduce chairside time (Omidi et al. 2018).
In our study, we have an observation that the increase in SBS with the increase in curing time, although the difference wasn’t significant statistically. A 3 and 6 second curing times can offer a balance of both significant SBS for clinical usage and reduced clinical chairside bonding time. Our observation regarding intensity was similar to the results obtained by Cerekja and Cakirer, and Par et al. (Cerekja and Cakirer 2011; Par et al. 2020).
Although resin composite enjoys significant popularity, RMGICs still has its niche in orthodontics, especially in cases where the acid-etch technique isn’t effective such as enamel hypoplasia, dental fluorosis, and amelogenesis imperfecta (Choo et al. 2001; Wiltshire and Noble 2010). RMGICs are used in the indirect bonding techniques of lingual fixed appliances (Komori et al. 2010; Komori et al. 2013). Recently studies that were conducted to study the feasibility of using RMGICs to bond lingual attachments such as buttons, and also the bonding of fixed lingual retainers are showing promising results (Baysal and Uysal 2010; Alkhateeb and Al-Sheakli 2013).
The benefits of the use of RMGICs such as its advantages acting as a fluoride reservoir could help in the prevention of decalcification, reduced enamel damage during removal post debonding (Bishara and Ostby 2010). Improved accuracy being pursued through the techniques of indirect bonding and customized fixed appliances could utilize RMGICs for bonding (Miyashita et al. 2017; Shen et al. 2021).
Also, a study conducted by Mota et al. identified increased anti-microbial activity and reduced plaque accumulation adjacent to orthodontic brackets bonded with RMGICs during the initial stages of treatment (Mota et al. 2008). Although the average SBS of the study group seems low, according to Reynold’s, an SBS of 6 – 8 MPa is adequate for normal clinical use (Eliades and Brantley 2000; Brantley and Eliades 2001).
The lower SBS in the laboratory testing can be a misrepresentation as it does not translate into clinical performance and failure (Graber and Vanarsdall 2000). Silverman et al. reported a bond failure of 3.2% for brackets bonded with RMGICs in an 8-month long in-vivo study (Eliades and Brantley 2000; Brantley and Eliades 2001). Enamel preparation, oral environment, humidity, moisture control, and bracket design could also play a role in SBS (Cacciafesta et al. 2004; Graber et al. 2016; Proffit et al. 2018).
A Limitation of our investigation is its in-vitro nature which cannot reproduce the complex interaction occurring in the oral environment. Numerous authors have pointed out variabilities in laboratory results and clinical observations (Sifakakis and Eliades 2017). Another limitation is the crosshead speed of the universal testing machine set 0.5mm/min. This according to Eliades and Brantley although is generally used does not accurately correspond to the in-vivo scenario due to higher speeds in clinical conditions (Eliades and Brantley 2000).
With all these limitations we can surmise that RMGICs deliver the best of both worlds in terms of clinical performance and can be considered as a suitable alternative to resin composites. The shorter curing cycle with high-intensity LEDs can help reduce chairside time and improve efficiency. Although we have to always to take into account the enormous amounts of research and improvements occurring in the field biomaterials which could still advance and evolve our practice and delivery of care to our patients (Shen et al. 2021).
CONCLUSION
The findings of the present investigation indicate that curing time has no statistically significant effect on the shear bond strength of brackets bonded using resin modified glass ionomer cements. RMGICs can offer significant advantages and decent clinical performance when used for luting orthodontic brackets. The shorter curing cycle offered by the high-intensity LEDs can help in reducing clinical chairside time, improving clinical efficiency and aid in the delivery of better care to orthodontic patients.
Conflict of Interests: Authors declare no conflicts of interests to disclose.
REFERENCES
Alkhateeb, H. M. and Al-Sheakli, E. I. (2013). Shear Bond Strength of Different Lingual Buttons Bonded to Wet and Dry Enamel Surfaces with Resin Modified Glass Ionomer Cement: In Vitro Comparative Study, Journal of Baghdad College of Dentistry, pp. 146–152. doi: 10.12816/0014978.
Almeida, R., Manarte-Monteiro, P., Domingues, J., et al. (2021). High-Power LED Units Currently Available for Dental Resin-Based Materials—A Review. Polymers, 13(13), p.2165.
Baysal, A. and Uysal, T. (2010). Resin-modified glass ionomer cements for bonding orthodontic retainers, European journal of orthodontics, 32(3), pp. 254–258.
Bishara, S. E. (2007). The Effect of Modifying the Self-etchant Bonding Protocol on the Shear Bond Strength of Orthodontic Brackets, The Angle Orthodontist, pp. 504–508. doi: 10.2319/0003-3219(2007)077[0505:teomts]2.0.co;2.
Bishara, S.E. and Ostby, A.W., (2010). March. Bonding and debonding from metal to ceramic: research and its clinical application. In Seminars in orthodontics Vol. 16, No. 1, pp. 24-36.
Brantley, W.A. and Eliades, T., (2001). Orthodontic materials: scientific and clinical aspects. AMERICAN JOURNAL OF ORTHODONTICS AND DENTOFACIAL ORTHOPEDICS, 119(6), pp.672-673.
Cacciafesta, V. (2004). Effect of blood contamination on shear bond strength of brackets bonded with a self-etching primer combined with a resin-modified glass ionomer, American Journal of Orthodontics and Dentofacial Orthopedics, pp. 703–708. doi: 10.1016/j.ajodo.2003.10.041.
Cerekja, E. and Cakirer, B. (2011). Effect of short curing times with a high-intensity light-emitting diode or high-power halogen on shear bond strength of metal brackets before and after thermocycling, The Angle Orthodontist, pp. 510–516. doi: 10.2319/071810-412.1.
Choo, S. C., Ireland, A. J. and Sherriff, M. (2001). An in vitro investigation into the use of resin-modified glass poly(alkenoate) cements as orthodontic bonding agents, European journal of orthodontics, 23(3), pp. 243–252.
Dall’Igna, C. M. (2011). Effect of curing time on the bond strength of a bracket-bonding system cured with a light-emitting diode or plasma arc light, The European Journal of Orthodontics, pp. 55–59. doi: 10.1093/ejo/cjq027.
Dunn, W. J. and Taloumis, L. J. (2002). Polymerization of orthodontic resin cement with light-emitting diode curing units, American journal of orthodontics and dento-facial orthopaedics: official publication of the American Association of Orthodontists, its constituent societies, and the American Board of Orthodontics, 122(3), pp. 236–241.
Eliades, T. and Brantley, W. A. (2000). The inappropriateness of conventional orthodontic bond strength assessment protocols, European Journal of Orthodontics, pp. 13–23. doi: 10.1093/ejo/22.1.13.
Eliades, T. and Brantley, W.A., (2000). Orthodontic materials: scientific and clinical aspects. Georg Thieme Verlag.
Eliades, T., (2010). Polymerization lamps and photocuring in orthodontics. In Seminars in orthodontics Vol. 16, No. 1, pp. 83-90.
Fukino, Y. and Komori, A., (2015). Time-related bond strength of resin-reinforced glass ionomer cement under various light exposure conditions. Orthodontic Waves, 74(3), pp.76-82.
Graber, L.W., Vanarsdall, R.L., Vig, K.W. et al. (2016). Orthodontics-e-book: current principles and techniques. Elsevier Health Sciences.
Graber, T. M. and Vanarsdall, R. L. (2000). Orthodontics: Current Principles and Techniques. Year Book Medical Pub.
Gronberg, K. (2006). Distance and time effect on shear bond strength of brackets cured with a second-generation light-emitting diode unit, The Angle orthodontist, 76(4), pp. 682–688.
Huang, J.J., Kuo, H.C. and Shen, S.C., (2017). Nitride Semiconductor Light-Emitting Diodes (LEDs): Materials, Technologies, and Applications. Woodhead Publishing.
Komori, A. (2013). Precise direct lingual bonding with the KommonBase, Journal of clinical orthodontics: JCO, 47(1), pp. 42–9; quiz 63–4.
Komori, A., Fujisawa, M. and Iguchi, S. (2010). KommonBase for precise direct bonding of lingual orthodontic brackets, International orthodontics / College europeen d’orthodontie, 8(1), pp. 14–27.
Lee, J.J., Nettey-Marbell, A., Cook Jr, A., et al. (2007). Using extracted teeth for research: the effect of storage medium and sterilization on dentin bond strengths. The Journal of the American Dental Association, 138(12), pp.1599-1603.
Leprince, J. (2010). Pulpal-temperature rise and polymerization efficiency of LED curing lights, Operative dentistry, 35(2), pp. 220–230.
Mavropoulos, A. (2005). Light curing time reduction: in vitro evaluation of new intensive light-emitting diode curing units, European Journal of Orthodontics, pp. 408–412. doi: 10.1093/ejo/cji021.
Mills, R. W., Uhl, A. and Jandt, K. D. (2002). Optical power outputs, spectra and dental composite depths of cure, obtained with blue light emitting diode (LED) and halogen light curing units (LCUs), British Dental Journal, pp. 459–463. doi: 10.1038/sj.bdj.4801597.
Miyashita, W., Komori, A. and Takemoto, K. (2017). Kommon Base – A precise direct bonding system for labial fixed appliances, International orthodontics / College Europeen d’orthodontie, 15(3), pp. 452–466.
Mota, S. M. (2008). Streptococcus mutans counts in plaque adjacent to orthodontic brackets bonded with resin-modified glass ionomer cement or resin-based composite, Brazilian Oral Research, pp. 55–60. doi: 10.1590/s1806-83242008000100010.
NawrockaA, A. and Łukomska-SzymańskaA, M. (2019). Extracted human teeth and their utility in dental research. Recommendations on proper preservation: A literature review Zastosowanie usuniętych zębów ludzkich w badaniach naukowych. Wytyczne dotyczące przechowywania próbek–przegląd piśmiennictwa. Dent Med Probl, 56(2), pp.185-190.
Nicholls, J. I. (2000). Polymerization lights–light energy and wavelength, Quintessence international, 31(9), pp. 688–689.
Øgaard, B. and Fjeld, M. (2010). March. The enamel surface and bonding in orthodontics. In Seminars in orthodontics, Vol. 16, No. 1, pp. 37-48.
Omidi, B.R., Gosili, A., Jaber-Ansari, M. et al. (2018). Intensity output and effectiveness of light curing units in dental offices. Journal of clinical and experimental dentistry, 10(6), p.e555.
Owens, S. E. and Miller, B. H. (2000). A comparison of shear bond strengths of three visible light-cured orthodontic adhesives, The Angle orthodontist, 70(5), pp. 352–356.
Par, M., Marovic, D., Attin, T., et al. (2020). The effect of rapid high-intensity light-curing on micromechanical properties of bulk-fill and conventional resin composites. Scientific Reports, 10(1), pp.1-10.
Peutzfeldt, A. and Asmussen, E. (2005). Resin Composite Properties and Energy Density of Light Cure, Journal of Dental Research, pp. 659–662. doi: 10.1177/154405910508400715.
Proffit, W.R., Fields, H.W., Larson, B. et al. (2018). Contemporary orthodontics-e-book. Elsevier Health Sciences.
Rossouw, P.E., (2010). A historical overview of the development of the acid-etch bonding system in orthodontics. In Seminars in orthodontics Vol. 16, No. 1, pp. 2-23.
Sağır, S. (2013). Effect of enamel laser irradiation at different pulse settings on shear bond strength of orthodontic brackets, The Angle Orthodontist, pp. 973–980. doi: 10.2319/111412-872.1.
Sfondrini, M. F. (2004). Plasma arc versus halogen light curing of orthodontic brackets: a 12-month clinical study of bond failures, American Journal of Orthodontics and Dentofacial Orthopedics, pp. 342–347. doi: 10.1016/j.ajodo.2003.02.008.
Sfondrini, M. F. (2006). Effect of light-tip distance on the shear bond strengths of resin-modified glass ionomer cured with high-intensity halogen, light-emitting diode, and plasma arc lights, American Journal of Orthodontics and Dentofacial Orthopedics, pp. 541–546. doi: 10.1016/j.ajodo.2005.12.025.
Sfondrini, M. F., Cacciafesta, V. and Klersy, C. (2002). Halogen versus high-intensity light-curing of uncoated and pre-coated brackets: a shear bond strength study, Journal of Orthodontics, pp. 45–50. doi: 10.1093/ortho/29.1.45.
Shen, C., Rawls, H.R. and Esquivel-Upshaw, J.F. (2021). Phillips’ Science of Dental Materials E-Book. Elsevier Health Sciences.
Sidhu, S.K. and Nicholson, J.W. (2016). A review of glass-ionomer cements for clinical dentistry. Journal of functional biomaterials, 7(3), p.16.
Sifakakis, I. and Eliades, T., (2017). Laboratory evaluation of orthodontic biomechanics: The clinical applications revisited. In Seminars in Orthodontics Vol. 23, No. 4, pp. 382-389.
Silverman, E. (1995). A new light-cured glass ionomer cement that bonds brackets to teeth without etching in the presence of saliva, American journal of orthodontics and dentofacial orthopedics: official publication of the American Association of Orthodontists, its constituent societies, and the American Board of Orthodontics, 108(3), pp. 231–236.
Staudt, C. B. (2005). Light-curing time reduction with a new high-power halogen lamp, American Journal of Orthodontics and Dentofacial Orthopedics, pp. 749–754. doi: 10.1016/j.ajodo.2004.08.020.
Turk, T., Elekdag-Turk, S. and Isci, D. (2007). Effects of Self-Etching Primer on Shear Bond Strength of Orthodontic Brackets at Different Debond Times, The Angle Orthodontist, pp. 108–112. doi: 10.2319/011606-22r.1.
Uşümez, S., Büyükyilmaz, T. and Karaman, A. I. (2004). Effect of light-emitting diode on bond strength of orthodontic brackets, The Angle orthodontist, 74(2), pp. 259–263.
Wiggins, K. M. (2004). Curing performance of a new-generation light-emitting diode dental curing unit, The Journal of the American Dental Association, pp. 1471–1479. doi: 10.14219/jada.archive.2004.0059.
Wiltshire, W.A. and Noble, J., (2010). Clinical and laboratory perspectives of improved orthodontic bonding to normal, hypoplastic, and fluorosed enamel. In Seminars in orthodontics Vol. 16, No. 1, pp. 55-65.
Yu, H.S. (2007). Comparison of the shear bond strength of brackets using the led curing light and plasma arc curing light: polymerization time, World journal of orthodontics, 8(2), pp. 129–135.


