Buraydah Colleges, College of Dentistry and Pharmacy, Qassim, Saudi Arabia
Corresponding author email: Nasser.aloqayil@outlook.sa
Article Publishing History
Received: 19/08/2021
Accepted After Revision: 15/12/2021
More than 570,000 new oral cancer cases are diagnosed, and around 300,000 deaths of this dreadful disease take place annually. The most widely recognized reason for morbidity and mortality globally is cancer. Early detection and regular follow up of high-risk patients can curb the mortality and morbidity rate. Dentists play a vital role in the early detection of oral cancer; therefore, assessing their knowledge and practice for early detection of oral cancer is crucial. A cross-sectional study was designed to assess the dentists’ knowledge and practice for the early detection of oral cancer. The study was conducted in the Qassim region among dental interns, general dental practitioners (GPs), specialists, and consultants. The questionnaire consisted of 14 closed-ended questions that contain socio-demographic characters of participants, information regarding the participants’ knowledge, and practice related questions. Data collected and analysed in SPSS software v. 21 and descriptive analysis was done.
A total of 159 participants in the study. Regarding the potential risks for oral cancer, 48.4% and 34.6% believed viruses and hereditary. Regarding the high-risk sites for oral cancer, 38.4% of the participants choose soft palate complex, lateral border of the tongue, and floor of the mouth as high-risk sites. The majority of the participants, i.e., 70.4% did not use any adjunctive screening tools. 57.2% feel they do not have sufficient knowledge concerning the early detection of oral cancer. The vast majority, i.e., 87.4% agreed that they need more information and continuing education for the same. Dentists’ comprehension must be reinforced and constantly updated by continuing education programs.
Continuing Education, Diagnostic Aids, Early Detection, Oral Cancer, Qassim.
Aloqayi N. M, Puttalingaiah V. D. Early Diagnosis of Oral Cancer: Knowledge and Perception of Oral Health Care Providers in Qassim, Saudi Arabia. Biosc.Biotech.Res.Comm. 2021;14(4).
Aloqayi N. M, Puttalingaiah V. D. Early Diagnosis of Oral Cancer: Knowledge and Perception of Oral Health Care Providers in Qassim, Saudi Arabia. Biosc.Biotech.Res.Comm. 2021;14(4). Available from: <a href=”https://bit.ly/3ccpZQ9“>https://bit.ly/3ccpZQ9</a>
Copyright © This is an Open Access Article distributed under the Terms of the Creative Commons Attribution License (CC-BY) https://creativecommons.org/licenses/by/4.0/, which permits unrestricted use distribution and reproduction in any medium, sources the original author and sources are credited.
INTRODUCTION:
The most widely recognized reason for morbidity and mortality globally is cancer. More than 570,000 new oral cancer cases are diagnosed, and around 300,000 deaths of the disease annually (Hung et al. 2020). Majority of oral cancer diagnosed at late stages that will lead to disfiguration and results in severe loss of oral function and chronic discomfort, including difficulty in chewing, swallowing and speaking (Shanmugavel and Shive, 2010). Also, in these patients with advanced disease along with surgical intervention results in distortion, social/psychological problems, increased morbidity level, and uncommonly death (Decuseara et al. 2011).
The comparatively low survival rate is attributed to late diagnosis, which occurs in more than half of all cases (Clovis et al. 2002). Varela et al. (2017) investigating the relationship between late diagnosis, stage, and death rate would 80% increase if the disease was detected and treated earlier. Early detection is the single most critical intervention influencing survival (Awan et al. 2014; Varela et al. 2017). Several dynamic factors were involved in the early detection of oral cancer from a primary care viewpoint, including general dental practitioners (GPs) and dentists’ professional knowledge of oral cancer, saving services of the primary care, and the impact of the doctor-patient relationship (Gomez et al. 2010; Rawal et al. 2018; Alqutaibi et al. 2020; Morikawa et al. 2021).
The access of oral cavity is easy and can be examined with little discomfort. Dentists, as primary care providers, can easily incorporate the screening protocol into their routine examinations (Clovis et al. 2002). Dentists have precise knowledge about oral cancer to diagnose individuals at risk, which is vital. Examining the whole oral cavity and running for appropriate treatments can contribute to reducing the oral cancer occurrence, morbidity, and mortality (Rawal et al. 2018; Alqutaibi et al. 2020; Morikawa et al. 2021).
National Institute for Health and Care Excellence (NICE, 2017) guidance recommends that GPs refer to an oncologist if the patient has an unexplained persistent neck lump or an unexplained persistent mouth ulcer for three weeks. Oral cancer is influenced by numerous factors, such as alcohol, tobacco, familial and genetic predisposition, shisha, viruses, and more. Viruses have been positively associated with the development of oral malignancy. HPV, especially HPV 16 type, are the common viruses implicated in oral cancer (Rawal et al. 2018; Alqutaibi et al. 2020; Morikawa et al. 2021).
Genetic susceptibility has been known to be an important risk factor in the occurrence of oral squamous cell carcinoma. Sharp teeth that occurred by a fracture due to caries or trauma and long-standing irritation has been proposed to promote neoplasm in the presence of other risk factors. Shisha smoking has been associated with oral cancer in many studies (Kumar et al. 2016; Patil et al. 2019). Statistically, the smokeless tobacco habit is considered a significant risk factor associated with oral cancer among the Saudi population.
Numerous studies show an absence of dentists’ knowledge and a negative approach toward oral cancer investigation and routine oral examination (Kumar et al. 2016; Gupta et al. 2016; Alqhtani et al. 2019; Jafer et al. 2020). Greenwood and Lowry (2001) showed that the majority of the dentists focus their examination on teeth and the procedure‑related instead of high‑risk sites like the floor of the mouth. Our study aims to assess the knowledge and practice in early detection of oral cancer among the practising dentists in Qassim region of Saudi Arabia.
MATERIAL AND METHODS
The Ethical Committee in Buraydah Colleges approved the current study. The questionnaire consisted of 14 closed-ended questions that contain socio-demographic characters of participants such as gender, designation, and region. Furthermore, information regarding the participants’ knowledge, such as the causes/risks for oral cancer, signs, and symptoms of oral cancer, high-risk sites of the disease, and knowledge regarding the obstacles of the early detection of oral cancer. Practice related questions were framed in the last part of the questionnaire such as the use of any adjunctive screening tools in their clinics with specifying the type of tool if used, how to examine a patient for signs and symptoms of oral cancer and if we should do a periodic oral cancer examination for the high-risk patients.
Also, we asked about the referral point if suspected oral malignancy. Two self-reported questions about if the participants feel they have sufficient knowledge concerning the early detection of oral cancer and if they need more information or training on oral cancer. This cross-sectional survey was conducted in the Qassim region among dental interns, general dental practitioners (GPs), specialists, and consultants in both private and public sectors. The goal of the questionnaire was explained to participants, and all necessary information was provided to them. Data collected and analysed in SPSS software version 21 and descriptive analysis was done.
RESULTS AND DISCUSSION
The demographic characteristics of the participants, 51.6% were females and 48.4% males. The study comprised 44.7% GP dentists, 32.1% dental interns, 21.4% specialist dentists and 1.9% consultants (Table 1).
Table 1. Socio-Demographic Characteristics of the Participants
| Variables | n | (%) |
| Gender | ||
| Male | 77 | 48.4% |
| Female | 82 | 51.6% |
| Designation | ||
| Intern | 51 | 32.1% |
| GP Dentists | 71 | 44.7% |
| Specialist | 34 | 21.4% |
| Consultant | 3 | 1.9% |
| Region | ||
| Qassim | 159 | 100% |
The potential risks/causes for oral cancer were smoking and smokeless tobacco, respectively 96.2% & 92.5%, which viruses and hereditary are considered to be the least risk factors, i.e., 48.4% & 34.6% respectively. Regarding the high-risk sites for oral cancer, 38.4% of the participants choose soft palate complex, lateral border of tongue, floor of mouth as high-risk sites. 32.1% of the participants believed that early oral cancer is generally asymptomatic and may be difficult to see (Table 2).
Table 2. Dentist’s Knowledge about Oral Cancer
| Variables | n | % |
| Knowledge regarding causes of oral cancer | ||
| Smoking | 153 | 96.2% |
| Alcohol | 143 | 89.9% |
| Viruses (HPV) | 77 | 48.4% |
| Hereditary | 55 | 34.6% |
| Smokeless tobacco (Chewing) | 147 | 92.5% |
| Shisha | 120 | 75.5% |
| Sharp cusp/Long standing irritations | 131 | 82.4% |
| Knowledge regarding signs and symptoms | ||
| A lump / non-healing ulcer that develops in the mouth or in the neck | 50 | 31.4% |
| TMJ fusion | 0 | 0.0% |
| Dysphagia | 4 | 2.5% |
| Options 1 & 3 | 104 | 65.4% |
| None of these | 1 | 0.6% |
| Knowledge regarding high risk sites for oral cancer | ||
| The soft palate complex | 24 | 15.1% |
| The lateral tongue | 9 | 5.7% |
| Floor of the mouth | 10 | 6.3% |
| Options 1 & 2 | 55 | 34.6% |
| All of the above | 61 | 38.4% |
| Knowledge regarding obstacles early detection of oral cancer | ||
| Warning signs are actually manifestations of more advanced disease | 7 | 4.4% |
| Early oral cancer is generally asymptomatic and may be difficult to see | 51 | 32.1% |
| The oral cancer exam may not be done by enough clinicians on their patients at risk | 16 | 10.1% |
| All of the above | 85 | 53.5% |
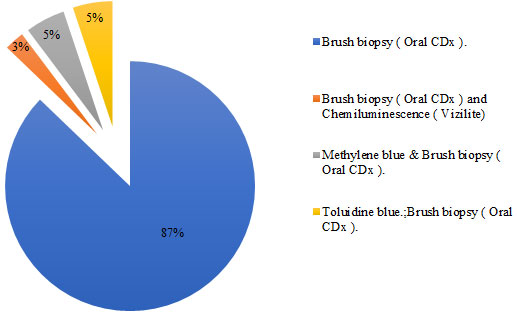
Regarding the usage of screening tools and their relations with designation among participants, consultants and specialists used adjunctive screening tools more compared to GPs and dental interns (P<0.05) (Table 3). Regarding types of screening tools, brush biopsy (Oral CDx) was the most commonly used (Figure 1).
Table 3: Prevalence of usage of screening tool and its relations with designation among participants
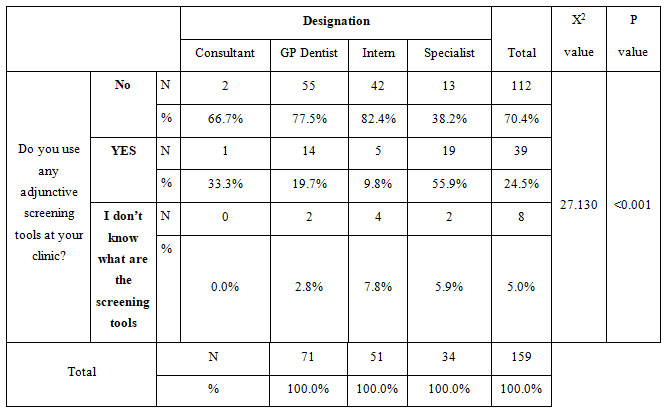
Figure 1: Type of screening tools used by participants (n=39)
About examining the patient for signs and symptoms of oral cancer, 56.6% opined unusual lumps, sensitivity and non-healing ulcers in and around the head & neck were considered vital. But 40.9% choose to palpate the lumps in and around the head & neck region while examining. Regarding the referral point, if suspected oral malignancy, 58.5% considered oral medicine/oral pathology, 30.8% considered oral & maxillofacial surgery, and 10.7% considered tertiary care hospital, respectively (Table 4).
Table 4. Practice Related Questions
| Variables | n | (%) |
| Do you use any adjunctive screening tools at your clinic? | ||
| Yes | 39 | 24.5% |
| No | 112 | 70.4% |
| I don’t know what are the screening tools | 8 | 5.0% |
| How you will examine a patient for signs and symptoms of oral cancer? | ||
| By palpating areas of the patient face, neck and mouth for unusual lumps or sensitivity | 65 | 40.9% |
| By talking with the patient about any unusual sores or non-healing ulcers | 2 | 1.3% |
| Options 1 & 2 | 90 | 56.6% |
| None of these | 2 | 1.3% |
| Practice regarding providing periodic oral cancer screening to the high-risk patients |
|
|
| Yes | 151 | 95.0% |
| No | 8 | 5.0% |
| Practice regarding the referral point if suspected oral malignancy | ||
| Oral & Maxillofacial Surgery | 49 | 30.8% |
| Oral Medicine / Oral Pathology | 93 | 58.5% |
| Tertiary Care Hospital | 17 | 10.7% |
Self-reported questions regarding the knowledge for the early detection of oral cancer, 57.2% of the participants lack the same. The majority of the dentists, 87.4%, agreed that they need more information and continuing education programs for the early detection of oral cancer (Table 5).
Table 5. Self-Reported Questions
| Variables | n | (%) |
| Do you feel that you have sufficient knowledge concerning early detection of oral cancer? | ||
| Yes | 68 | 42.8% |
| No | 91 | 57.2% |
| Do you need more information or training on oral cancer? | ||
| Yes | 139 | 87.4% |
| No | 20 | 12.6% |
Regarding the signs and symptoms of oral cancer, a study done by Rethman et al. (2010) showed that the non-healing ulcer is a clinical presentation of the early stage of disease. 96.8% of our participants agreed with the same. The knowledge findings regarding the clinical presentation of oral cancer in our study population are similar to a study done in the past in United Arab Emirates (Hashim et al. 2018). The familiarity of anatomy and health of different structures of the oral cavity will help the dentists in easily identifying the signs and symptoms of oral cancer than any other health professionals (Lingen et al. 2008; Galvão-Moreira and da Cruz 2017; Nagao et al. 2020).
38.4% of the participants choose soft palate complex, lateral border of the tongue, and mouth floor as high-risk sites. 6.3% of the participants opined floor of the mouth as a high-risk site. Whatever, the lateral side of the tongue and floor of the mouth are the high predilection sites for cancer in most parts of the world except for South and Southeast Asia, where buccal mucosa is commonly involved (Lingen et al. 2008; Galvão-Moreira and da Cruz 2017; Nagao et al. 2020). The overall usage of an adjunctive screening tool for oral cancer among the participants was low, and specialist dentists reported more usage than others. In our study, among those who used screening tools, 87% of the dentists used brush biopsy alone.
Many screening tools have been used to help in the early detection of oral cancer (Masthan et al. 2012; Walsh et al. 2013). According to Cochrane Systematic Review done by Macey et al. (2015) and a study done by Morikawa et al. (2020), scalpel biopsy is considered as the gold standard in oral cancer screening and diagnosis. Dentists also can utilize other less invasive techniques such as vital stains like Toluidine blue, exfoliative cytology, fluorescent imaging, etc. for this purpose (Wan and Savage 2010; Murgod et al. 2011; Awan et al. 2014; Vinuth et al. 2015; Morikawa et al. 2021; Jafer et al. 2021).
The lesser usage of a screening tool for early detection of oral cancer could be attributed to inadequate exposure or importance given to the practical teaching of these techniques during their undergraduate training (Wan and Savage 2010; Murgod et al. 2011; Jafer et al. 2021). The study findings showed that almost all participants believed that periodic oral screening should be done for individuals above 40 years of age and also for high-risk patients like tobacco, alcohol users, etc. According to Sankaranarayanan et al. (2015), oral visual screening can reduce oral cancer-related mortality in high-risk individuals. In Oral visual screening, a visual and physical examination of intraoral mucosa is done using a mouth mirror and gauze under bright lights.
They are used for signs of oral potentially malignant disorders (OPMDs), which is then followed by extra-oral examination using gloved hands and good lighting to examine the skin and palpate muscles, TMJ and lymph nodes for any abnormality (Sankaranarayanan et al. 2015). Despite good knowledge of the oral anatomy and risk factors of oral cancer, the lack of confidence in our study population is obvious. Studies conducted by Diamanti et al. (2002) and Anandani et al. (2015) also reported that dentists were reluctant to perform oral screening and biopsy techniques for detecting oral cancer (Diamanti et al. 2002; Anandani et al. 2015; Morikawa et al. 2021; Jafer et al. 2021).
Some of the limitations should be considered before generalizing the findings for our study. As this is a questionnaire study, the reported responses may vary from the actual clinical practices and knowledge regarding oral cancer. Thus, there could be a presence of social desirability bias in reported responses, resulting in underestimation. It is apparent in our study that there are inconsistencies between dentists, which necessitates further study to understand the barriers and concerns in oral screening and associated procedures for oral cancer.
CONCLUSION
The findings of the present study indicates that the current dental education curriculum still lacks the training of graduates in early detection and in conducting biopsy procedures. The majority of the study participants wanted to have more information and training through workshops and continuing education programs on oral cancer detection and related procedures. Training on use of chairside invasive and non-invasive diagnostic procedures especially for interns and GPs, screening of high-risk population at community level can reduce the mortality rate.
Conflict of Interests: Authors declare no conflicts of interests to disclose.
Data Availability Statement: The database generated and /or analysed during the current study are not publicly available due to privacy, but are available from the corresponding author on reasonable request.
REFERENCES
Alqhtani N, Alenazi A, Nasyam FA, et al. (2019). Role of the dentist in early detection of oral cancer. J IntOral Health, 11, 66-9.
Alqutaibi AY, Borzangy S, Al-Maweri SA, et al. (2020). Early detection of oral cancer and potentially malignant disorders: experiences, practices, and beliefs of prosthodontists practicing in Saudi Arabia. J Prosthet Dent S0022-3913(20):30434
Anandani C, Metgud R, Ramesh G, et al. (2015). Awareness of General Dental Practitioners about Oral Screening and Biopsy Procedures in Udaipur, India. Oral Health Prev Dent, 6, 523-530.
Awan KH, Khang TW, Yee TK, et al. (2014). Assessing oral cancer knowledge and awareness among Malaysian dental and medical students. J Cancer Res Ther, 10(4), 903-7.
Clovis JB, Horowitz AM and Poel DH (2002). Oral and pharyngeal cancer: knowledge and opinions of dentists in British Columbia and Nova Scotia. Journal of Canadian Dental Association, 68(7), 415-420.
Decuseara G, MacCarthy D, and Menezes G (2011). Oral cancer: knowledge, practices and opinions of dentists in Ireland. Journal of the Irish Dental Association, 57(4), 209–214.
Diamanti N, Duxbury AJ, Ariyaratnam S, et al. (2002). Attitudes to biopsy procedures in general dental practice. Br Dent J, 10, 588-592.
Galvão-Moreira L. V, and da Cruz M (2017). Screening and early detection of oral cancer: current controversies. Acta odontologica Scandinavica, 75(5), 361–365.
Gomez I, Warnakulasuriya S, Varela-Centelles PI, et al. (2010). Is early diagnosis of oral cancer a feasible objective? Who is to blame for diagnostic delay? Oral Dis, 16(4), 333–342.
Greenwood M., and Lowry R. J. (2001). Primary care clinicians’ knowledge of oral cancer: a study of dentists and doctors in the North East of England. British dental journal, 191(9), 510–512.
Gupta N, Gupta R, Acharya AK, et al. (2016). Changing trends in oral cancer – A global scenario. Nepal J Epidemiol, 6, 613‑9.
Hashim R, Abo-Fanas A, Al-Tak A, et al. (2018). Early Detection of Oral Cancer- Dentists’ Knowledge and Practices in the United Arab Emirates. Asian Pac J Cancer Prev, 8, 2351-2355.
Hung LC, Kung PT, Lung CH, et al. (2020). Assessment of the Risk of Oral Cancer Incidence in A High-Risk Population and Establishment of A Predictive Model for Oral Cancer Incidence Using A Population-Based Cohort in Taiwan. Int J Environ Res Public Health, 17(2):665.
Jafer M, Crutzen R, Halboub E, et al. (2020). Dentists Behavioral Factors Influencing Early Detection of Oral Cancer: Direct Clinical Observational Study. J Cancer Educ,10.1007/s13187-020-01903-1.
Jafer, M., Crutzen, R., Moafa, I. et al. (2021). What Do Dentists and Dental Students Think of Oral Cancer and Its Control and Prevention Strategies? A Qualitative Study in Jazan Dental School. J Canc Educ, 36, 134–142.
Keser, G., Yılmaz, G. and Pekiner, F.N. (2021). Assessment of Knowledge Level and Awareness About Human Papillomavirus Among Dental Students. J Canc Educ 36, 664–669.
Kumar M, Nanavati R, Modi TG, et al. (2016). Oral cancer: Etiology and risk factors: A review. J Can Res Ther, 12, 458-63.
Lingen MW, Kalmar JR, Karrison T, et al. (2008). Critical evaluation of diagnostic aids for the detection of oral cancer. Oral Oncol, 1, 10–22.
Macey R, Walsh T, Brocklehurst P, et al. (2015). Diagnostic tests for oral cancer and potentially malignant disorders in patients presenting with clinically evident lesions. Cochrane Database Syst Rev, 5, CD010276.
Masthan KM, Babu NA, Dash KC, et al. (2012). Advanced diagnostic aids in oral cancer. Asian Pac J Cancer prev, 13(8), 3573–6.
Morikawa T, Shibahara T, Takano M, et al. (2021). Countermeasure and opportunistic screening systems for oral cancer. Oral Oncol, 112:105047.
Morikawa T., Shibahara T., Nomura T., et al. (2020). Non-Invasive Early Detection of Oral Cancers Using Fluorescence Visualization with Optical Instruments. Cancers, 12(10), 2771.
Murgod V, Angadi PV, Hallikerimath S, et al. (2011). Attitudes of general dental practitioners towards biopsy procedures. J Clin Exp Dent, 3, 418–23.
Nagao T and Warnakulasuriya S. (2020). Screening for oral cancer: Future prospects, research and policy development for Asia. Oral Oncol,105(104632).
National Institute for Health and Care Excellence (2015). Suspected cancer: recognition and referral. NG12. London: NICE, Accessed 15 April 2020. https://www.nice.org.uk/guidance/NG12
Patil S, Rajagopalan P, Patel K, et al. (2019). Chronic shisha exposure alters phosphoproteome of oral keratinocytes. J Cell Commun Signal, 13(3), 281-289.
Poelman MR, Brand HS, Forouzanfar T, et al. (2018). Prevention of HPV-Related Oral Cancer by Dentists: Assessing the Opinion of Dutch Dental Students. J Cancer Educ, 6, 1347-1354.
Rawal M, Malusare PC and Patil BS (2018). Awareness and Knowledge of Oral Cancer among Dental Practitioners of Bhopal, India – A Cross-Sectional Study. Int J Oral Dent Health 4:056.
Rethman MP, Carpenter W, Cohen EE, et al. (2010). Evidence-based clinical recommendations regarding screening for oral squamous cell carcinomas. J Am Dent Assoc, 5, 509-520.
Sankaranarayanan R, Ramadas K, Amarasinghe H, et al. (2015). Cancer: Disease Control Priorities, Oral Cancer: Prevention, Early Detection, and Treatment, Washington (DC): The International Bank for Reconstruction and Development / The World Bank, 85-99.
Shanmugavel A and Shive SE (2010). Oral Health Practices and Oral Cancer Knowledge Attitudes and Behaviors among College Students. World J Dent, 1(3), 141-148.
Varela-Centelles P, López-Cedrún JL, Fernández-Sanromán J, et al. (2017). Key points and time intervals for early diagnosis in symptomatic oral cancer: a systematic review. International journal of oral and maxillofacial surgery, 46(1), 1–10.
Vinuth DP, Agarwal P, Kale AD, et al. (2015). Acetic acid as an adjunct vital stain in diagnosis of tobacco-associated oral lesions: A pilot study. J Oral Maxillofac Pathol, 19(2), 134-138.
Walsh T, Liu JL, Brocklehurst P, et al. (2013). Clinical assessment to screen for the detection of oral cavity cancer and potentially malignant disorders in apparently healthy adults. The Cochrane database of systematic reviews, 11, CD010173.
Wan A, and Savage NW (2010). Biopsy and diagnostic histopathology in dental practice in Brisbane: usage patterns and perceptions of usefulness. Australian dental journal, 55(2), 162–169.


