
Microbiological
Communication
Biosci. Biotech. Res. Comm. 9(4): 615-620 (2016)
Frequency of
pvl
gene in methicillin resistant
Staphylococcus aureus
Isolates collected from
Northwest Iran
N. Javanshir Rezaei
1
, M R. Nahaei
2
*, J. Sadeghi
3
, A. Esmailkhani
4
1,4
M. Sc. Student, Immunology Research Center, and Department of Microbiology, Faculty of Medicine, Tabriz
University of Medical Sciences, Tabriz, Iran
2,3
Immunology Research Center, and Department of Microbiology, Faculty of Medicine, Tabriz University of
Medical Sciences, Tabriz, Iran
ABSTRACT
Staphylococcus aureus infections, particularly infections caused by methicillin-resistant S. aureus (MRSA) strains,
are emerging as a major public health problem. The aim of the present study was to determine the prevalence of
methicillin-resistant staphylococcus aureus (MRSA) by phenotypic and genotypic methods in clinical specimens and
detection of the Panton – Valentine leukocidin (PVL) gene in the MRSA strains. In an 11-month study, 710 clinical
specimens were collected from patients attending to several teaching hospitals of Urmia city, Northwest Iran. The
isolates were examined by conventional culture method for detecting S. aureus strains and further con rmation with
standard biochemical tests, including catalase, coagulase and DNase. MRSA isolates phenotypically were screened
by disk diffusion method. Then DNA was extracted from our MRSA isolates and mecA gene ampli ed by PCR.
Finally, pvl genes were identi ed among MRSA isolates which were positive for mecA gene. Among test isolates, 114
isolates (16%) were con rmed as S. aureus, from which 48 (42.1%) were recorded as MRSA. pvl gene was detected
in 13 (27%) MRSA isolates. Our study showed that the prevalence of PVL-positive MRSA isolates, justify further
detailed inspection to prevent possible future endemics in the studied hospitals and likewise other hospitals in the
region.
KEY WORDS: MRSA,STAPHYLOCOCCUS AUREUS,
PVL GENE
, MEC A GENE
615
ARTICLE INFORMATION:
*Corresponding Author: nahaeim@yahoo.com
Received 31
st
Oct, 2016
Accepted after revision 18
th
Dec, 2016
BBRC Print ISSN: 0974-6455
Online ISSN: 2321-4007
Thomson Reuters ISI ESC and Crossref Indexed Journal
NAAS Journal Score 2015: 3.48 Cosmos IF : 4.006
© A Society of Science and Nature Publication, 2016. All rights
reserved.
Online Contents Available at: http//www.bbrc.in/

616 FREQUENCY OF
PVL
GENE IN METHICILLIN RESISTANT
STAPHYLOCOCCUS AUREUS
ISOLATES BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS
Rezaei, Nahaei, Sadeghi and Esmailkhani
INTRODUCTION
Staphylococcus aureus is a Gram-positive opportunis-
tic bacterium of great clinical signi cance, expressing
diverse virulence factors that facilitate its adherence,
colonization, intercellular interaction, immune system
evasion, and tissue damage. Moreover, this microor-
ganism has developed resistance to -lactam antibiot-
ics by -lactamase expression or the presence of peni-
cillin binding protein 2a (PBP2a) directly related with
methicillin-resistant S. aureus (MRSA) strains.The mec
A gene codi es for PBP2a and is a structural part of a
mobile genetic element named Staphylococcal cassette
chromosome mec (SCCmec), which can insert itself into a
speci c region of its central genome. The different types
of SCCmec are classi ed according to the combina-
tion of the mec complex (mecA gene and its regulators)
and the cassette chromosomal recombinase (ccr), which
codi es for enzymes responsible for SCCmec mobility.
Mec A gene is not present in methicillin-sensitive S.
aureus (MSSA) strains and the presence of this gene is
regarded as a criterion of resistance (Merlino, Watson et
al. 2002 Llarrull, Fisher et al. 2009 Chambers and DeLeo
2009 Jensen and Lyon 2009, Borbón-Esquer, Villaseñor-
Sierra et al. 2014).
In 1961 the rst MRSA strain was identi ed in the
United Kingdom. Especially in the past two decades the
prevalence of these strains have increased in the world
(El-Din, El-Shafey et al. 2003). These strains are usually
associated with hospital-acquired infections (HA-MRSA)
that shows resistance to many antibiotics, including
-lactams, semi-synthetic penicillins, cephalosporins
and carbapenems. The prevalence of HA-MRSA is vari-
able in different parts of the world, ranging from 4.1%
in Panama up to 59% in Korea (Klevens, Edwards et al.
2006, Klein, Smith et al. 2007, Alvarez, Ramirez et al.
2008).
Genotyping of MRSA strains has been employed in
epidemiological studies to determine its prevalence, dis-
semination, risk factors, and association with antimicro-
bial resistance (Kondo, Ito et al. 2007). Production of the
Panton – Valentine leukocidin (PVL) in MRSA strains is
considered to be associated with disease severity (Lina,
Piémont et al. 1999). PVL is a Staphylococcal leukoci-
din which only attacks macrophages and polymorpho-
nuclears, and has two components “S (33kDa)” and “F
(34kDa)” which is controlled by luk S-PV and luk F-PV
genes, respectively (Narita, Kaneko et al. 2001). With
respect to the presence of certain chromosomal cas-
settes, the majority of the published studies have shown
an association of SCCmec type II strains with hospital
infections, whereas type IVa strains, with or without
the presence of the pvl gene, have been associated with
community-acquired infections (Borbón-Esquer, Vil-
laseñor-Sierra et al. 2014).The aim of the present study
was to determine the prevalence of pvl gene in MRSA
isolates by genotypic methods in clinical specimens.
MATERIAL AND METHODS
BACTERIAL ISOLATES
A total of 710 different clinical specimens, including
urine, wound, blood, broncho-alveolar lavage, skin
and soft tissue, cerebrospinal uid and body uids
were studied for isolation of S. aureus during January-
December 2015 from patients admitted to several hos-
pitals in Urmia city, West Azerbaijan, Iran. Initially, all
isolates were identi ed using standard microbiological
and laboratory methods, including growth on blood agar
and type of hemolysis, Gram stain, catalase test, growth
on mannitol salt agar, slide and tube coagulase tests,
and DNase test (Forbes et al. 2007). Later, all S. aureus
isolates were stored in nutrient broth supplemented with
15% glycerol at -20°C until use.
PHENOTYPIC DETECTION OF MRSA ISOLATES
Resistance to methicillin was determined by Kirby –
Bauer disk diffusion method on Muller Hinton agar
(MHA) using cefoxitin disk (Hi Media, India) as described
in the guidelines of Clinical and Laboratory Standards
Institute (CLSI) documents . As recommended in the CLSI
guidelines, direct colony suspension method was used
for testing of S. aureus isolates for potential methicillin
and or oxacillin resistance. The plates were incubated at
35°C for 18–24 hours aerobically, and growth inhibition
zones around the disk was measured. Inhibition zone
diameters ≤21 mm considered as resistant. Any visible
growth within the zone of inhibition was also consid-
ered as methicillin resistant.
DNA EXTRACTION
DNA extracti on was performed according to Sadeghi
et al. (Sadeghi and Mansouri 2014). Brie y, for mak-
ing a starter culture, a single colony of S. aureus was
inoculated on nutrient agar. Three or four colonies of
overnight growing bacteria from the starter culture were
suspended in 450 μl of TE (Tris-EDTA) buffer (10 mM
Tris, 1 mM EDTA, pH 8). Cell lysis was obtained by treat-
ment with 5 μl of proteinase K (20 mg/mL) for 20 min
at 50 °C followed by addition of 60 μl of 10% SDS for
10 min at 68 °C. In the next step, 80 μl of cetyltrimeth-
ylammonium bromide (CTAB)/NaCl and 100 μl of 5 M
NaCl were added and incubated at 65 °C for 10 min.
Then, chloroform/isoamyl alchohol (700 μl) was added
and centrifuged at 11000 × g for 8 min. Supernatant was
BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS FREQUENCY OF
PVL
GENE IN METHICILLIN RESISTANT
STAPHYLOCOCCUS AUREUS
ISOLATES 617
Rezaei, Nahaei, Sadeghi and Esmailkhani
transferred to another tube and the DNA was precipi-
tated with isopropanol, washed with 70% ethanol, dried,
and dissolved in 100 μl of deionized water.
MOLECULAR DETECTION OF MEC A GENE
All S. aureus isolates were evaluated by PCR ampli -
cation for detection of mecA gene by using mecA P4
(5’-TCCAGATTACAACTTCACCAGG-3’) and mecA P7
(5’- CCACTTCATATC TTGTAACG-3’) primers (McClure,
Conly et al. 2006). PCR performed in a 25μl volume
containing 10 pmol of each primers, 200 μM dNTP
(Roche, Germany), 2.5 μl (50 mM MgCl2), 0.5 μl Taq
polymerase (2.5 u) (Roche, Germany), 5 μl PCR buffer
10x (Roche,Germany) and 5 μl DNA-template. S.aureus
ATCC 33591 and ATCC 25923 were used as positive and
negative controls, respectively. The following PCR con-
dition was used: 94°C (4 min),30 cycles with 94°C (45 s)
,56°C (45 s), 72°C (1 min) and nally 72°C (7 min) ; 4°C
hold.
MOLECULAR DETECTION OF PVL GENE
PCR for detection of pvl gene was carried out by using
primers as below:
pvl-1:5’ATCATTAGGTAAAATGTCTGGACATGATCCA–3’
and pvl-2: 5’ GCATCAAGTGTATTGGATAGCAAAAGC –
3’ (McClure, Conly et al. 2006). PCR performed in a 50 μl
containing 20 pmol of each primer, 5 μl of 10x buffers,
1.5 μl of dNTP (10pmol), 3 μl of MgCl
2
and 32.5 μl of
distilled water and 4 μl of the template DNA. DNA dena-
tured for 5 minutes at 95 °C following with 35 cycles of
denaturing performed for 30 S at 92°C, with annealing
at 55 °C for 30 S, extension at 72 °C for 45 S and nally,
10 minutes of the nal extension performed at 72 °C.
AGAROSE GEL ELECTROPHORESIS FOR
DETECTION OF PCR PRODUCTS
PCR products were visualized following electrophoresis
in 1.7% agarose gels run at 70 V with ethidium bromide
staining (Sigma, USA). pvl gene and mecA gene posi-
tive isolates yielded an ampli cation product of shining
band in 433 and 162 base pair, respectively, with the
standard positive control under UV trans-illuminator
(UVP, USA) (SANTOS, TEIXEIRA et al. 1999).
STATICAL ANALYSIS
Data were analyzed using SPSS statistical software (ver-
sion 15, SPSS, Chicago, USA), Chi-square exact test was
used to test for signi cant association between cate-
gorical variables. P-value less than 0.05 was considered
signi cant.
RESULTS AND DISCUSSION
Distribution of methicillin resistant S. aureus:
Out of 710 clinical specimens, 114 isolates (16%) were
con rmed as S. aureus, of which 48 (42.1%) were
recorded as methicillin resistant, mostly isolated from
urine, wound discharge and blood (Table1).
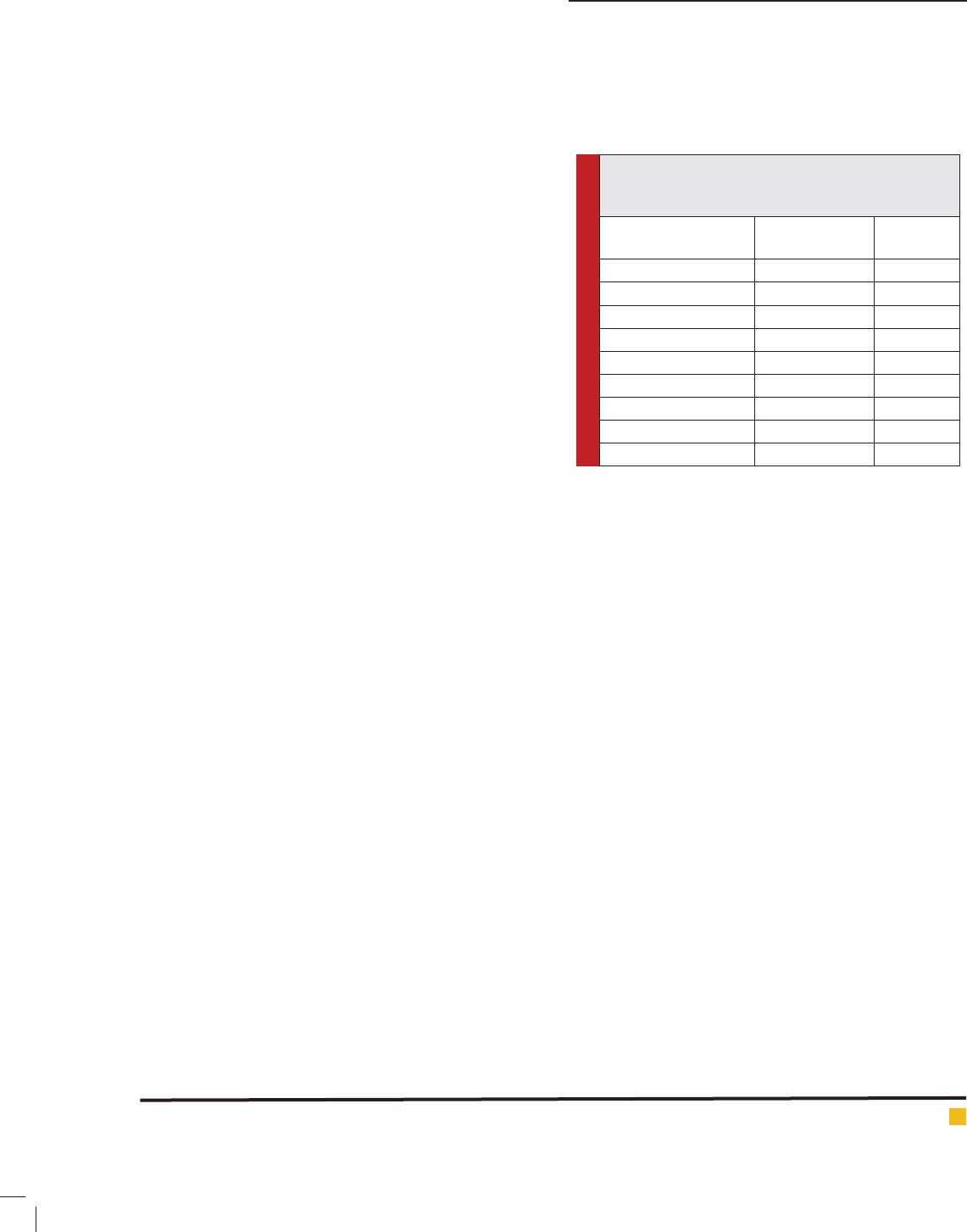
Table 1: Distribution of methicillin-resistant
Staphylococcus aureus (MRSA) isolates according to
clinical specimens.
Specimens No. of
S. aureus
isolates (%)
MRSA (%)
Urine 33(28.94) 16(14.03)
Wound 29(25.43) 15(13.15)
Blood 14(12.28) 8(7.01)
Broncho-alveolar lavage 11(9.64) 3(2.63)
Skin and soft tissue 8(7.01) 1(0.87)
Cerebrospinal uid 7(6.14) 3(2.63)
Body uids 5(4.38) 1(0.87)
Other specimens 7(6.14) 1(0.87)
Total 114(100) 48(42.1)
Phenotypic detection of methicillin resistant S. aureus
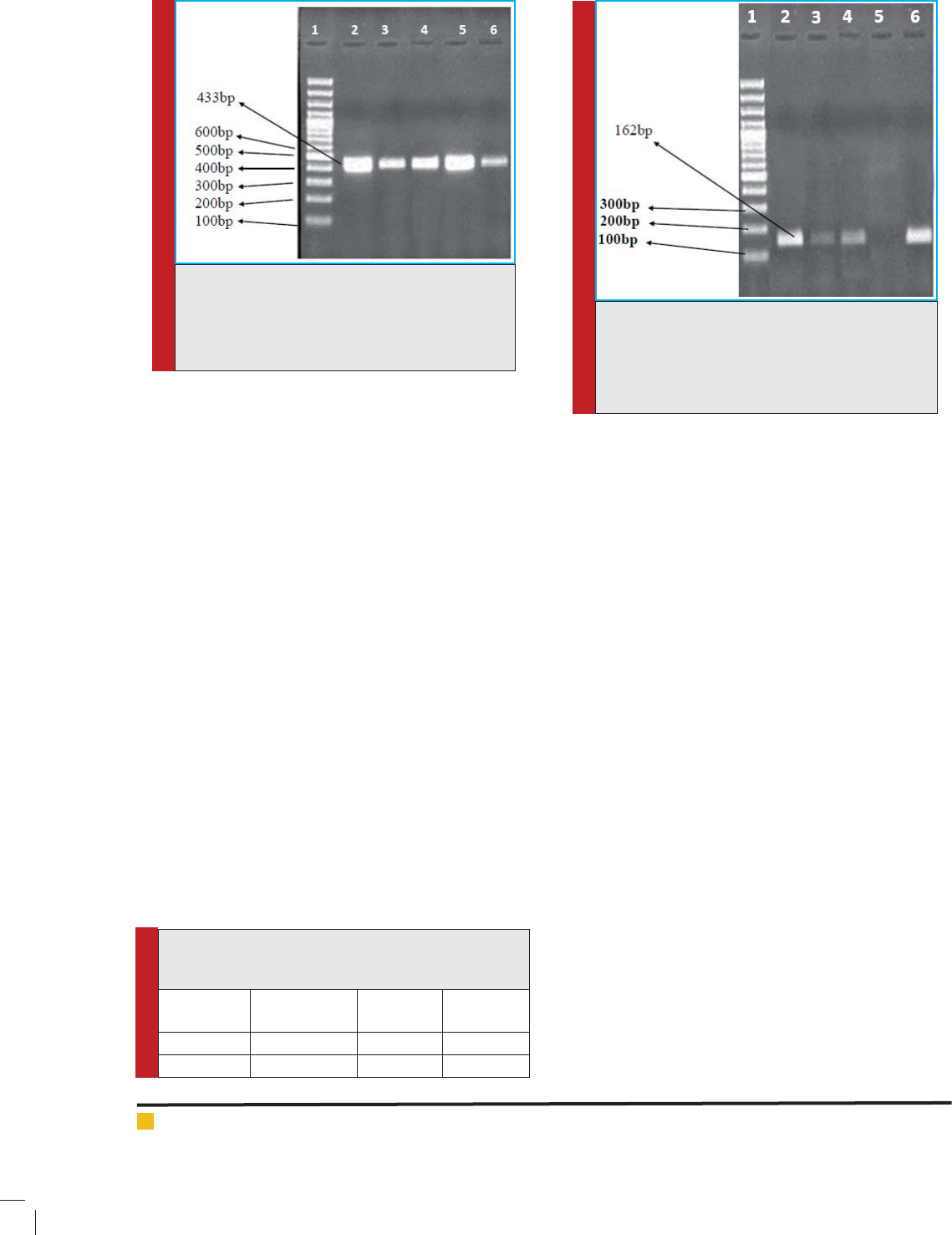
and molecular detection of mecA gene:
The presence of mecA gene using PCR considered as the
gold standard method for calculating the speci city and
sensitivity of the other tests in this study. Results from
conventional disk diffusion susceptibility tests correlated
very well with those from the PCR assay. The cefoxitin
disk detected MRSA isolates correctly in all cases com-
pared to the presence of mecA gene by PCR (42.1%)
(Figure 1). Entirely based on cefoxitin disc results there
was no substantial differences between conventional
susceptibility testing and PCR for calculating methicillin
resistant S. aureus (p>0.05). The overall results obtained
with different techniques are shown in Table 2.
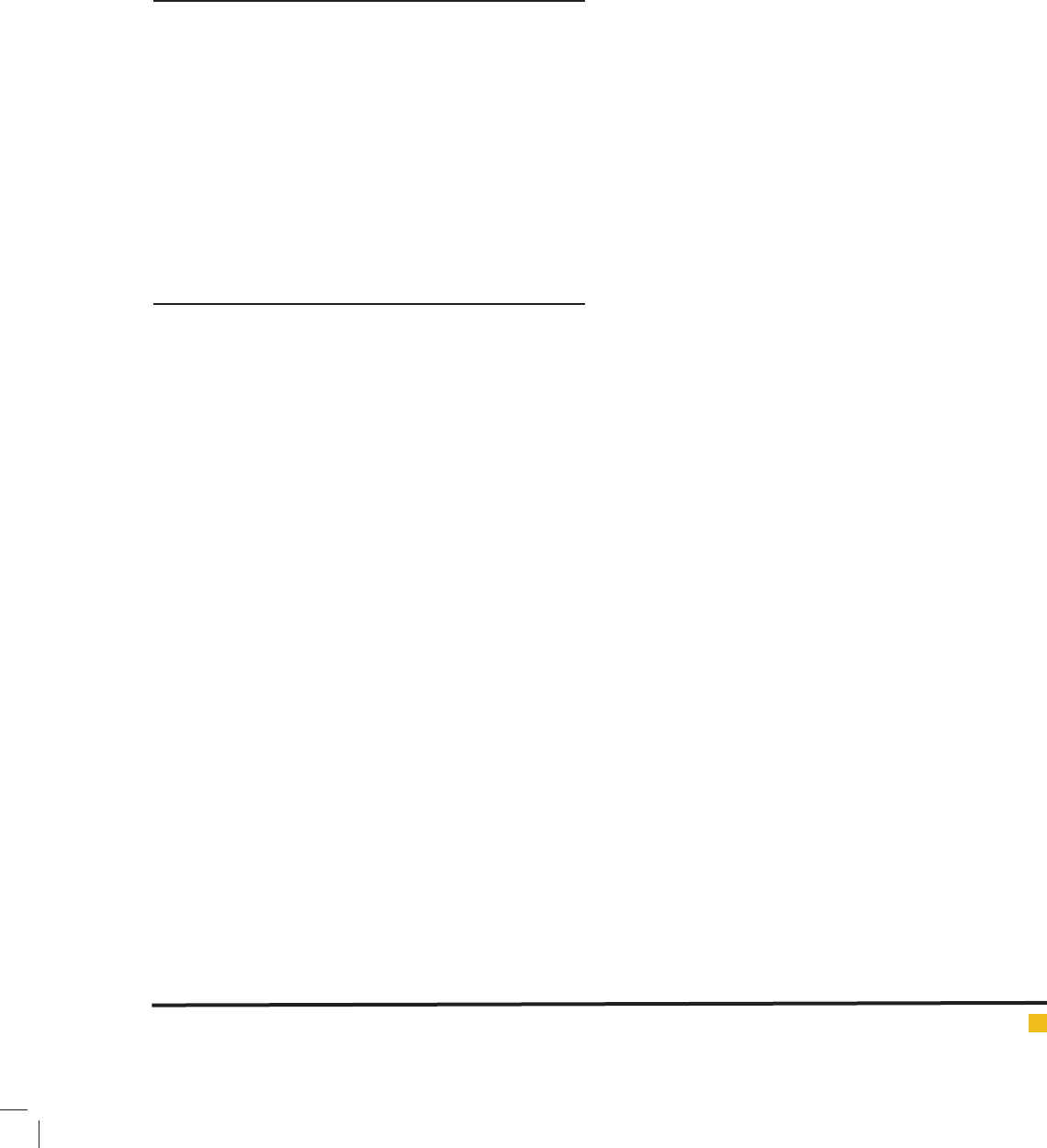
Detection of MRSA isolates carrying pvl gene:
Among MRSA isolates, 13 (27%) contained pvl genes
and the remaining isolates were recorded as pvl negative
(Figure 2).
S. aureus is one of the most common infectious
agents which has become a frequent cause of nosocomial
infection. This bacterium is simply gained and comprises
potential to become resistant to many common in-use
antibiotics and the prevalence of resistant strains pos-
ing serious therapeutic and infection control problems
within the hospital environment (Khosravi, Hoveizavi et
al. 2012). The infections caused by MRSA are important
and can even cause mortality, so increasing antibiotic
618 FREQUENCY OF
PVL
GENE IN METHICILLIN RESISTANT
STAPHYLOCOCCUS AUREUS
ISOLATES BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS
Rezaei, Nahaei, Sadeghi and Esmailkhani
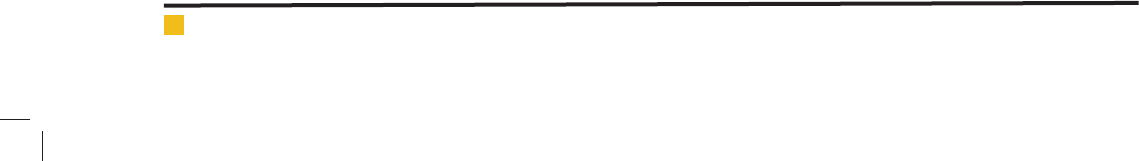
TABLE 2: Sensitivity and speci city of diagnostic
methods in identi cation of methicillin-resistant S.
aureus.
Test No. of MRSA
identi ed (%)
Sensitivity Speci city
Cefoxitin disk 48(40.67%) 100% 100
mecA 48(40.67%) 100% 100
resistance is a concern and should be monitored (Mer-
lino, Watson et al. 2002).
Approximately 89.4 million persons (32%) and 2.3
million persons (0.8%) of the US population are colo-
nized with S.aureus and MRSA, respectively (Kuehnert,
Hill et al. 2005). The rate of MRSA in all community-
associated S.aureus infections ranges from 2.5% to 39%
in Asian countries (Vandenesch, Naimi et al. 2003). In
our study, 42.1% of isolates were recorded as MRSA,
while other studies conducted in Iran have shown MRSA
prevalence is 55% in Tehran (Saderi, Habibi et al. 2008),
37% in Tabriz (NIKBAKHT, Nahaei et al. 2007) and 50%
in Hamedan (Zamani, Sadeghian et al. 2007).
Such strains can be spread by close contact with an
infected person, touching contaminated surfaces and
stuffs, unhealthy and crowded living conditions and
poor personal hygiene. In addition, MRSA is dif cult
to treat due to multi-drug resistance and cause confu-
sion in the usual sensitivity tests to detect the resist-
ance due to non-uniform expression of them. Therefore,
the detection of mecA and pvl genes represents a quick
and more speci c method for early identi cation of
CA-MRSA isolates (McClure, Conly et al. 2006). Also, a
combination of mecA and pvl genes is capable to pro-
duce super adaptable S. aureus strains (22-25). Most of
CA-MRSA strains have the virulence factor, PVL, which
is not often found in HA-MRSA or MSSA strains. But a
low occurrence of MSSA was reported, and has been led
to necrotizing pneumonia and death (Vandenesch, Naimi
et al. 2003).
In recent years, an impressive worldwide spread of
PVL-positive CA-MRSA clones have been observed
(Francis, Doherty et al. 2005). Out of the MRSA isolates
in our study, 27% carried PVL-encoding genes. Previ-
ous studies in Iran have reported the prevalence to be
19% in the capital of Iran; Tehran (Lari, Pourmand et
al. 2011), 7.23% in the Southwest; Ahvaz (Khosravi,
Hoveizavi et al. 2012), and 5.47% in the South; Shi-
raz (Alfatemi, Motamedifar et al. 2014). In contrast to
the present study, some previous reports have described
an extremely high prevalence of pvl genes in MRSA.
In Western Nepal, Tunisian and Texas, the prevalence
of PVL-positive MRSA isolates was 56.8%, 79%, 94.9%
respectively (Bocchini, Hulten et al. 2006, Mariem, Ito
et al. 2013, Bhatta, Cavaco et al. 2016). Some investiga-
tions revealed a low prevalence of PVL genes in MRSA.
In Turkey, UK and Austria PVL-positive MRSA occur-
rence were detected 1.3%, 1.6%, 3.7%, respectively (Hol-
mes, Ganner et al. 2005, Krziwanek, Luger et al. 2007,
Kilic, Guclu et al. 2008). These ndings may re ect
the difference in the prevalence of this gene in differ-
ent geographic regions and also kind of assay used for
detecting the genes.
Since there is a strong evidence of involvement of
pvl gene in pathogenesis of S. aureus strains, so diag-
nosis and treatment of infections caused by S. aureus
strains harboring these genes is very important. Detec-
FIGURE 1. PCR products for the
pvl
gene. Lane 1:
100 bp molecular weight marker. Lane 2: Staphy-
lococcus aureus pvl gene-positive control. lanes
3-6: pvl positive Staphylococcus aureus isolates
(433bp).
FIGURE 2. PCR products for the
mecA
gene. Lane
1: 100 bp molecular weight marker. Lane2: Posi-
tive control (MRSA). Lanes 3, 4 and 6: mecA posi-
tive Staphylococcus aureus isolates (162bp). Lane 5:
Negative control.
BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS FREQUENCY OF
PVL
GENE IN METHICILLIN RESISTANT
STAPHYLOCOCCUS AUREUS
ISOLATES 619
Rezaei, Nahaei, Sadeghi and Esmailkhani
tion of PVL is commonly carried out by using molecular
techniques (Khosravi, Hoveizavi et al. 2012). Accord-
ing to the results of this study, the phenotypic methods
with cefoxitin susceptibility testing and PCR assay for
MRSA gene can be useful for de nite diagnosis of MRSA
strains. Our study was limited because SCCmec typing
was not performed.
CONCLUSION
In conclusion, the prevalence of PVL-positive MRSA
isolates, found to be 27% in this study, justify further
detailed inspection to prevent possible future endemics
in the studied hospitals and likewise other hospitals in
the region.
Moreover, if these strains spread to parts of
hospital, including pediatrics, intensive care and cardiac
intensive care unit could be life threating. Therefore,
identi cation of these strains and treatment of relative
infections is important in prevention of colonization
and spread.
ACKNOWLEDGMENT
The authors are grateful to Immunology Research Center
of Tabriz University of Medical Sciences for supporting
this study to be undertaken.
REFERENCES
Clinical and Laboratory Standards Institute/NCCLS (2005). Per-
formance Standards for Antimicrobial Susceptibility Testing;
Fifteenth Informational Supplement. CLSI/ NCCLS documents
M100-S15. USA.
Alfatemi, S. M. H., M. Motamedifar, N. Hadi and H. S. E. Saraie
(2014). Analysis of virulence genes among methicillin resistant
Staphylococcus aureus (MRSA) strains. Jundishapur journal of
microbiology 7(6).
Alvarez, J., A. Ramirez, M. Mojica-Larrea, J. R. Huerta, J.
Guerrero, A. Rolon, H. Medina, J. Munoz, J. Mosqueda and A.
Macias (2008). [Methicillin-resistant Staphylococcus aureus at
a general hospital: epidemiological overview between 2000-
2007]. Revista de investigacion clinica; organo del Hospital de
Enfermedades de la Nutricion 61(2): 98-103.
Bhatta, D. R., L. M. Cavaco, G. Nath, K. Kumar, A. Gaur, S.
Gokhale and D. R. Bhatta (2016). Association of Panton Valen-
tine Leukocidin (PVL) genes with methicillin resistant Staphy-
lococcus aureus (MRSA) in Western Nepal: a matter of concern
for community infections (a hospital based prospective study).
BMC infectious diseases 16(1): 1.
Bocchini, C. E., K. G. Hulten, E. O. Mason, B. E. Gonzalez, W. A.
Hammerman and S. L. Kaplan (2006). Panton-Valentine leukoci-
din genes are associated with enhanced in ammatory response
and local disease in acute hematogenous Staphylococcus aureus
osteomyelitis in children. Pediatrics 117(2): 433-440.
Borbón-Esquer, E. M., A. Villaseñor-Sierra, E. Martínez-
López, J. J. Jáuregui-Lomeli, R. Villaseñor-Martínez and M.
d. R. Ruiz-Briseño (2014). SCC mec types and pvl gene in
methicillin-resistant Staphylococcus aureus strains from
children hospitalized in a tertiary care hospital in Mexico.
Scandinavian journal of infectious diseases 46(7): 523-
527.
Chambers , H. F. and F. R. DeLeo (2009). Waves of resistance:
Staphylococcus aureus in the antibiotic era.Nature Reviews
Microbiology 7(9): 629-641.
El-Din, S. A. S., E. El-Shafey, R. Mohamad, M. El-Hadidy, A.
El-Din, M. El-Hadidy and H. Zaghloul (2003). Methicillin-
resistant Staphylococcus aureus: a problem in the burns unit.”
Egyptian Journal of Plastic and Reconstructive Surgery 27:
1-10.
Forbes B A, Sahm DF and W. AS (2007). bailey&scotts Diagnos-
tic microbiology USA, Elsevier.
Francis, J. S., M. C. Doherty, U. Lopatin, C. P. Johnston, G.
Sinha, T. Ross, M. Cai, N. N. Hansel, T. Perl and J. R. Ticehurst
(2005). Severe community-onset pneumonia in healthy adults
caused by methicillin-resistant Staphylococcus aureus carry-
ing the Panton-Valentine leukocidin genes. Clinical Infectious
Diseases 40(1): 100-107.
Holmes, A., M. Ganner, S. McGuane, T. Pitt, B. Cookson and
A. Kearns (2005). Staphylococcus aureus isolates carrying
Panton-Valentine leucocidin genes in England and Wales: fre-
quency, characterization, and association with clinical disease.
Journal of clinical microbiology 43(5): 2384-2390.
Jensen, S. O. and B. R. Lyon (2009). Genetics of antimicrobial
resistance in Staphylococcus aureus. Future microbiology 4(5):
565-582.
Khosravi , A. D., H. Hoveizavi and Z. Farshadzadeh (2012). The
prevalence of genes encoding leukocidins in Staphylococcus
aureus strains resistant and sensitive to methicillin isolated
from burn patients in Taleghani hospital, Ahvaz, Iran. Burns
38(2): 247-251.
Kilic, A ., A. U. Guclu, Z. Senses, O. Bedir, H. Aydogan and
A. C. Basustaoglu (2008). Staphylococcal cassette chromosome
mec (SCCmec) characterization and panton-valentine leukoci-
din gene occurrence for methicillin-resistant Staphylococcus
aureus in Turkey, from 2003 to 2006. Antonie Van Leeuwen-
hoek 94(4): 607-614.
Klein, E ., D. L. Smith and R. Laxminarayan (2007). Hospitali-
zations and deaths caused by methicillin-resistant Staphylo-
coccus aureus, United States, 1999-2005.Emerging infectious
diseases 13(12): 1840.
Klevens, R. M., J. R. Edwards, F. C. Tenover, L. C. McDonald, T.
Horan, R. Gaynes and N. N. I. S. System (2006). Changes in the
epidemiology of methicillin-resistant Staphylococcus aureus
in intensive care units in US hospitals, 1992–2003. Clinical
infectious diseases 42(3): 389-391.
Kondo, Y ., T. Ito, X. X. Ma, S. Watanabe, B. N. Kreiswirth,
J. Etienne and K. Hiramatsu (2007). Combination of multi-
plex PCRs for staphylococcal cassette chromosome mec type
assignment: rapid identi cation system for mec, ccr, and major
Rezaei, Nahaei, Sadeghi and Esmailkhani
620 FREQUENCY OF
PVL
GENE IN METHICILLIN RESISTANT
STAPHYLOCOCCUS AUREUS
ISOLATES BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS
differences in junkyard regions.Antimicrobial Agents and
Chemotherapy 51(1): 264-274.
Krziwane k, K., C. Luger, B. Sammer, S. Stumvoll, M. Stammler,
S. Metz-Gercek and H. Mittermayer (2007). PVL-positive MRSA
in Austria. European Journal of Clinical Microbiology & Infec-
tious Diseases 26(12): 931-935
Kuehnert , M. J., H. A. Hill, B. A. Kupronis, J. I. Tokars, S. L.
Solomon and D. B. Jernigan (2005). Methicillin-resistant-
Staphylococcus aureus hospitalizations, United States. Emerg
Infect Dis 11(6): 868-872.
Lari, A. R., M. R. Pourmand, S. O. Moghadam, Z. Abdossa-
madi, A. E. Namvar and B. Asghari (2011). Prevalence of PVL-
containing MRSA isolates among hospital staff nasal carriers.
Laboratory Medicine 42(5): 283-286.
Lina, G. , Y. Piémont, F. Godail-Gamot, M. Bes, M.-O. Peter,
V. Gauduchon, F. Vandenesch and J. Etienne (1999). Involve-
ment of Panton-Valentine leukocidin—producing Staphylococ-
cus aureus in primary skin infections and pneumonia. Clinical
Infectious Diseases 29(5): 1128-1132.
Llarrull, L. I., J. F. Fisher and S. Mobashery (2009). “Molecular
basis and phenotype of methicillin resistance in Staphylococ-
cus aureus and insights into new -lactams that meet the chal-
lenge. Antimicrobial agents and chemotherapy 53(10): 4051-
4063.
Mariem, B. J.-J., T. Ito, M. Zhang, J. Jin, S. Li, B.-B. B. Ilhem,
H. Adnan, X. Han and K. Hiramatsu (2013). Molecular char-
acterization of methicillin-resistant Panton-valentine leuko-
cidin positive Staphylococcus aureus clones disseminating in
Tunisian hospitals and in the community. BMC microbiology
13(1): 1.
McClure, J .-A., J. M. Conly, V. Lau, S. Elsayed, T. Louie, W.
Hutchins and K. Zhang (2006). Novel multiplex PCR assay
for detection of the staphylococcal virulence marker Panton-
Valentine leukocidin genes and simultaneous discrimination of
methicillin-susceptible from-resistant staphylococci. Journal
of clinical microbiology 44(3): 1141-1144.
Merlino, J ., J. Watson, B. Rose, M. Beard-Pegler, T. Gottlieb,
R. Bradbury and C. Harbour (2002). “Detection and expres-
sion of methicillin/oxacillin resistance in multidrug-resistant
and non-multidrug-resistant Staphylococcus aureus in Central
Sydney, Australia.” Journal of Antimicrobial chemotherapy
49(5): 793-801.
Narita, S. , J. Kaneko, J.-i. Chiba, Y. Piémont, S. Jarraud, J.
Etienne and Y. Kamio (2001). Phage conversion of Panton-Val-
entine leukocidin in Staphylococcus aureus: molecular analy-
sis of a PVL-converting phage, SLT. Gene 268(1): 195-206.
NIKBAKHT, M. , M. Nahaei, M. Akhi, M. Asgharzadeh and S.
Nikvash (2007). Nasal carriage rate of Staphylococcus aureus
in hospital personnel and inpatients and antibiotic resistance
pattern of isolated strains from nasal and clinical specimens
in Tabriz.
Sadeghi, J. and S. Mansouri (2014). Molecular characteriza-
tion and antibiotic resistance of clinical isolates of methicil-
lin‐resistant Staphylococcus aureus obtained from Southeast
of Iran (Kerman).Apmis 122(5): 405-411.
Saderi, H., M . Habibi, P. Owlia and M. Asadi Karam (2008).
Detection of methicillin resistance in Staphylococcus aureus by
disk diffusion and PCR methods. Iranian Journal of Pathology
3(1): 11-14.
Santos, K. R. , L. M. Teixeira, G. Leal, L. S. Fonseca and P. Gon-
tijo Filho (1999). “DNA typing of methicillin-resistant Staphy-
lococcus aureus: isolates and factors associated with nosoco-
mial acquisition in two Brazilian university hospitals.” Journal
of medical microbiology 48(1): 17-23.
Vandenesch, F ., T. Naimi, M. C. Enright, G. Lina, G. R. Nimmo,
H. Heffernan, N. Liassine, M. Bes, T. Greenland and M.-E.
Reverdy (2003). Community-acquired methicillin-resistant
Staphylococcus aureus carrying Panton-Valentine leukocidin
genes: worldwide emergence.” Emerging infectious diseases
9(8): 978-984.
Zamani, A., S . Sadeghian, J. Ghaderkhani, M. Y. Alikhani, M.
Naja mosleh, M. T. Goodarzi, H. S. Farahani and R. Youse -
Mashouf (2007). Detection of methicillin-resistance (mec-A)
gene in Staphylococcus aureus strains by PCR and determina-
tion of antibiotic susceptibility.” Annals of Microbiology 57(2):
273-276.