
Medical
Communication
Biosci. Biotech. Res. Comm. 10(4): 775-782 (2017)
Comparing the analgesic effect of intranasal fentanyl
and ketamine in children
Golikhatir Iraj
1
, Montazer Seyed Hossein
1
*, Aghilli Elham
2
, Aminiahidashti Hamed
1
, Bozorgi
Farzad
1
, Jahanian Fatemeh
1
and Hosseininejad Seyed Mohammad
1
1
Assistant Professor, Department of Emergency Medicine, Mazandaran University of Medical Science, Sari, Iran
2
Emergency Medicine Resident, Mazandaran University of Medical Science, Sari, Iran
ABSTRACT
Introduction: Pain control is one of the treatment priorities and the most important children’s rights because children
experience painful events since birth and during childhood due to common childhood illnesses or accidents. The aim
of this study was to compare the analgesic effect of intranasal ketamine and fentanyl in children. Method: The present
research is a double blind randomized clinical trial conducted on 80 children aged 3-13 years who were admitted to
the Emergency Department of Sari Imam Hospital. The patients who met the inclusion criteria were randomly divided
into two groups using random number generator and 40 patients were considered per group. Data were analyzed
using SPSS, Mann-Whitney-U test and wilcoxon paired test. Findings: The ndings showed that the analgesic effect
of ketamine and fentanyl are similar among the studied children and there is no signi cant difference. In ketamine
group there was signi cant difference between the mean of pain, systolic blood pressure, diastolic blood pressure,
heart rate and respiratory rate variables before and after taking ketamine, according to Willcoxon statistics and sig.
smaller than 0.05. In fentanyl Group, there was signi cant difference between the mean of pain, systolic blood pres-
sure, heart rate and respiratory rate variables before and after taking fentanyl, according to Willcoxon statistics and
sig. smaller than 0.05. There was no signi cant difference between ketamine and fentanyl analgesic effect in terms
of parental satisfaction and there was also no signi cant difference between medical team’s level of satisfaction with
ketamine and fentanyl analgesic effect. Conclusion: Considering that the analgesic effect of intranasal ketamine and
fentanyl on the pain control among the studied children is similar, their prescription is recommended. It is also rec-
ommended to simultaneously measure children’s level of anxiety and effect of these drugs on their anxiety because
children have different experiences of pain and anxiety affects measuring pain severity in future studies.
KEY WORDS: ANALGESIC, INTRANASAL, FENTANYL, KETAMINE, CHILDREN
775
ARTICLE INFORMATION:
*Corresponding Author: igk_47@yahoo.com
Received 1
st
Oct, 2017
Accepted after revision 21
st
Dec, 2017
BBRC Print ISSN: 0974-6455
Online ISSN: 2321-4007 CODEN: USA BBRCBA
Thomson Reuters ISI ESC and Crossref Indexed Journal
NAAS Journal Score 2017: 4.31 Cosmos IF: 4.006
© A Society of Science and Nature Publication, 2017. All rights
reserved.
Online Contents Available at:
http//www.bbrc.in/
DOI: 10.21786/bbrc/10.4/24
776 COMPARING THE ANALGESIC EFFECT OF INTRANASAL FENTANYL AND KETAMINE IN CHILDREN BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS
Golikhatir Iraj et al.
INTRODUCTION
Pain is one of the most common symptoms in patients
admitted to the emergency room. Achieving desired anal-
gesia and sedation before the procedures has become an
elusive goal in many cases (Murphy et al., (2014).Inter-
national Association of pain de ned it as an unpleasant
feeling and emotional experience associated with acute
or potential tissue damage (Hazinski 2013). Children
are usually brought to the emergency department due
to painful diseases and injuries. Other diagnostic and
painful or unpleasant therapeutic procedures may be
required during the visits (Atkinson et al., (2009). Pain
in children is more dif cult than adults either in the
evaluation or treatment process. This dif culty becomes
more obvious when Intravenous analgesic is considered
(Moore et al. (2010). Creating a practical approach to
sedation and analgesia may vary in different parts of the
world (Shahryariet al 2010 Majidi et al., 2017).
Many studies have been conducted on the analge-
sic effects of ketamine in the world. Many studies con-
ducted on intranasal, oral and rectal administration of
ketamine have shown that topical application of this
drug is also possible. Many empirical evidence suggest
that NMDA receptors exist in the central nervous sys-
tem and peripheral nerves. Moreover, empirical studies
have noted that the peripheral administration of NMDA
receptor antagonists show analgesic effects of this drug
(Hadayi M, Rezaeian M. (2011, Brian et al 2015).
Fentanyl is a potent opioid agonist that can be used
in different ways. Fentanyl is the oldest synthetic opioid
agonist and mainly exerts its effect on the hair receptor
(Brian et al., (2015). Intravenous administration is the
main method of medications to children but it is also
stressful and painful and we sometimes need to spend
a lot of time. Intramuscular injection is similar to the
intravenous injection with the exception that longer
period of time is required for the drug to exert its effect.
According to the foregoing, intranasal and buccal meth-
ods seem to be more appropriate methods (Banks, et al.
(2004). However, between these two methods, using buc-
cal method requires need more interaction between the
child and the therapist and even in voluntary cases of
drug use, 56% of the drug remains in the mouth. Nasal
cavity holds a rich vascular network and since this vas-
cular bed is easily accessible, it is easy to be managed.
Onset and peak effect usually occurs after 3-5 minutes
and within 10-15 minutes (Veldhorst, 2013).
Studies have shown that a wide range of intrana-
sal ketamine doses has been used in clinical practice
and further research is proposed to determine the opti-
mal dose of intranasal ketamine for analgesia (Marcia
et al. (2013). So far, various medications are presented
and provided for this purpose. But ketamine, which is a
receptor agonist has gained much popularity in this eld
(Majidi et al., 2017).
Fentanyl is a short-acting strong industrial drug and
is now widely used for pain relief. Few studies have com-
pared the effects of intranasal fentanyl and ketamine.
Graudins et al., (2015) conducted a study in American
Academy of Emergency Medicine (AAEM) and compared
the effect of intranasal fentanyl and ketamine in children
3 to 13 years who suffered from organ damage and had
pain severity of at least 6 out of 10. The 40 children were
assigned in each group in this comparison. As a result,
a reduced pain which was reported in both groups was
similar, but ketamine showed more side effects. Level of
satisfaction with and side effects of ketamine and fenta-
nyl was respectively 83%, 78% and 82%, 40%. Prior to
this study, there was no study on intranasal fentanyl and
ketamine for pain control in children.
In a study in 2013 in the Department of Emergency
Medicine of British Columbia Hospital, Andolfatto
investigated the intranasal ketamine effect in reducing
pain in patients admitted to the emergency department.
This study was performed in patients older than 6 years.
A total of 40 patients were enrolled in the study and the
mean change in pain was 34mm within 30 minutes and
the average time for this reduction in pain was about
9.5 minutes. There were no reports of serious side effects
during this time and all reported side effects were tran-
sient, requiring no intervention.
Murphy et al. (2014) conducted a study in the Depart-
ment of Emergency Medicine at University College Dub-
lin and studied intranasal fentanyl consumption for
the treatment of acute pain in children. Patients were
randomly selected and intranasal fentanyl was admin-
istrated for pain control and its ef cacy was compared
with intravenous medications. Side effects and level
of satisfaction were also investigated. This study was
carried out on children aged less than 21 years who
weighed more than 10 kg with severe pain . Severity of
pain was assessed every 5 minutes to 30 minutes and
then at 30.60 and 120 minutes. A total of 30 patients
were enrolled and the pain severity was dropped by
about 13mm after 120 minutes. There were no severe
side effects, for which intervention was needed. Also,
small sample size of some studies caused the results
not to be generalized to the entire population (Yeaman
et al., (2013). Also, different doses of these two drugs
were used in studies on the effects of intranasal keta-
mine or fentanyl in pain control among children (Saun-
ders et al., 2010).
In our country, no comparison has been made in this
way. Since there has been no similar study in this regard
so far in the country, similar studies conducted abroad
are few and the results of these few studies cannot gen-
eralized to all areas yet. On the other hand, taking into
BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS COMPARING THE ANALGESIC EFFECT OF INTRANASAL FENTANYL AND KETAMINE IN CHILDREN 777
Golikhatir Iraj et al.
account the speed and ease of use of the intranasal drug,
we decided to compare the effect of intranasal fentanyl
and ketamine as well as their effects and complications
in pain management. The present study also aimed to
achieve acceptable outcome with regard to recommend-
ing the use of these two drugs in the emergency depart-
ment by measuring satisfaction of parents and medical
team.
MATERIAL AND METHODS
This study is a double blind randomized clinical trial
that was conducted on 80 children aged 3-13 years’ old
who were taken to Sari Imam Hospital. Individuals who
were enrolled in the study were selected among all chil-
dren aged 3-13 years who were admitted to emergency
due to the trauma and needed remedial measures and
painful procedures such as healing wounds with moder-
ate to severe pain during procedure. The number of sam-
ples was considered 40 individuals for each group based
on statistical formulas. Patients who met the inclusion
criteria were randomly assigned in two groups using
random number generator so that the number of chil-
dren had relatively equal distribution at the end, allow-
ing evaluation of the results for both age groups. A total
of 40 patients were considered in each group. One group
received Ketamine and the other one was given fentanyl.
Among pain severity assessment scales, which are used
at early age, FPS-R scale is a scale that is translated into
30 languages and can be used for free (Julie 2013).
VAS scale is also a measure commonly used in the
age of 6 years, the patient shows the location of his/her
pain on a horizontal line. Left and right sides of the line
show point of no pain and unbearable pain, respectively.
Pain score range is between the pain score in the left side
and is expressed in millimeters. Based on the pain scales
pain severity of 6 and higher shows moderate to severe
pain. At the beginning of the project and during the pro-
cedure, FPS-R and VAS scales were respectively used to
assess pain in children aged 3-6 and over 6 years. Even-
tually, after summarizing the pain assessment results
and the effect of the drugs on it, qualitative evaluation
of the results was performed.
According to ASA physical status classi cation
standards, all ASA I and II class children were enrolled
in the study. Also according to method of drug use,
all children with severe colds, respiratory infections or
major nasal damage, and all those with taking painkill-
ers before referral, given the confounding effect on the
evaluation of results, and contraindications for drugs,
suspected cases of increased ICP, severe respiratory dis-
eases or a history of seizure disorders were excluded.
Also, after obtaining permission from the Medical Ethics
Committee, registering the present trial in the Iranian
database of clinical trials and providing adequate expla-
nations on how to do pain management technique as
well as obtaining consent letter from children’s parents,
patients were enrolled.
However, patients were not deprived of any treat-
ment due to participation in this research and it does
not cause any harm to them .Lidocaine was used for
local anesthesia during the procedure. Both drugs pro-
duced by Rotemxmedica-Germany company, Ketamine
and fentanyl were prepared by Saha Halal Pharmaceuti-
cal Company and Drug Administration of Mazandaran
University of Medical Sciences, respectively. After the
initial assessment and recording pain levels and vital
signs at admission in the rst questionnaire then in the
second questionnaire during the procedure, the follow-
ing standard recording and monitoring were performed:
pulse rate (PR), respiratory rate (RR), blood pressure (BP),
blood oxygen saturation (SpO2) and temperature body
temperature (T).
Drugs were already drawn into 1cc syringes, to have
equal volume of drugs, appropriate to 10 kg weight. The
syringe were named A and B and were given to the head
of the pharmaceutical ward who was unaware of their
contents. The drugs were later administrated to patients
in a double-blind, randomized manner during the pro-
ject. One group received 1 mg / kg intranasal ketamine
and 1mcg/kg intranasal fentanyl was administrated to
another group. The procedure was started 5 minutes
after administration is starting considering the time
required for onset of action. The pain severity and vital
signs were examined at 5, 15, 20, 30, 45 and 60 minutes
in the studied patients, if necessary, an additional 1.4
dose was prescribed for pain control to at 15 minutes.
In case of spo2 less than 92% for more than 10 seconds
or apnea more than 20 seconds, jaw thrust maneuver
and mask ventilation was started. Nausea and vomiting
was measured by observing and questioning the patient
and parents. Other side effects, including dizziness, and
derealization were recorded by observing and question-
ing and each of them underwent treatment and moni-
toring based on the severity and type. Information was
recorded by an individual (emergency resident or medi-
cine specialists) who was unaware of the groups. Data
analysis was carried out using SPSS v.16 and Mann-
Whitney-U test and Willcoxon paired test.
RESULTS AND DISCUSSION
The mean ± standard deviation of pain before tak-
ing Ketamine and fentanyl were respectively, 8.9, 8.93
and 0.93, 0.92 and there was no signi cant difference
between Ketamine and fentanyl groups in terms of pain
before taking these drugs based on Mann-Whitney U
z-statistic and sig. value of greater than 0.05. Thus, chil-
778 COMPARING THE ANALGESIC EFFECT OF INTRANASAL FENTANYL AND KETAMINE IN CHILDREN BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS
Golikhatir Iraj
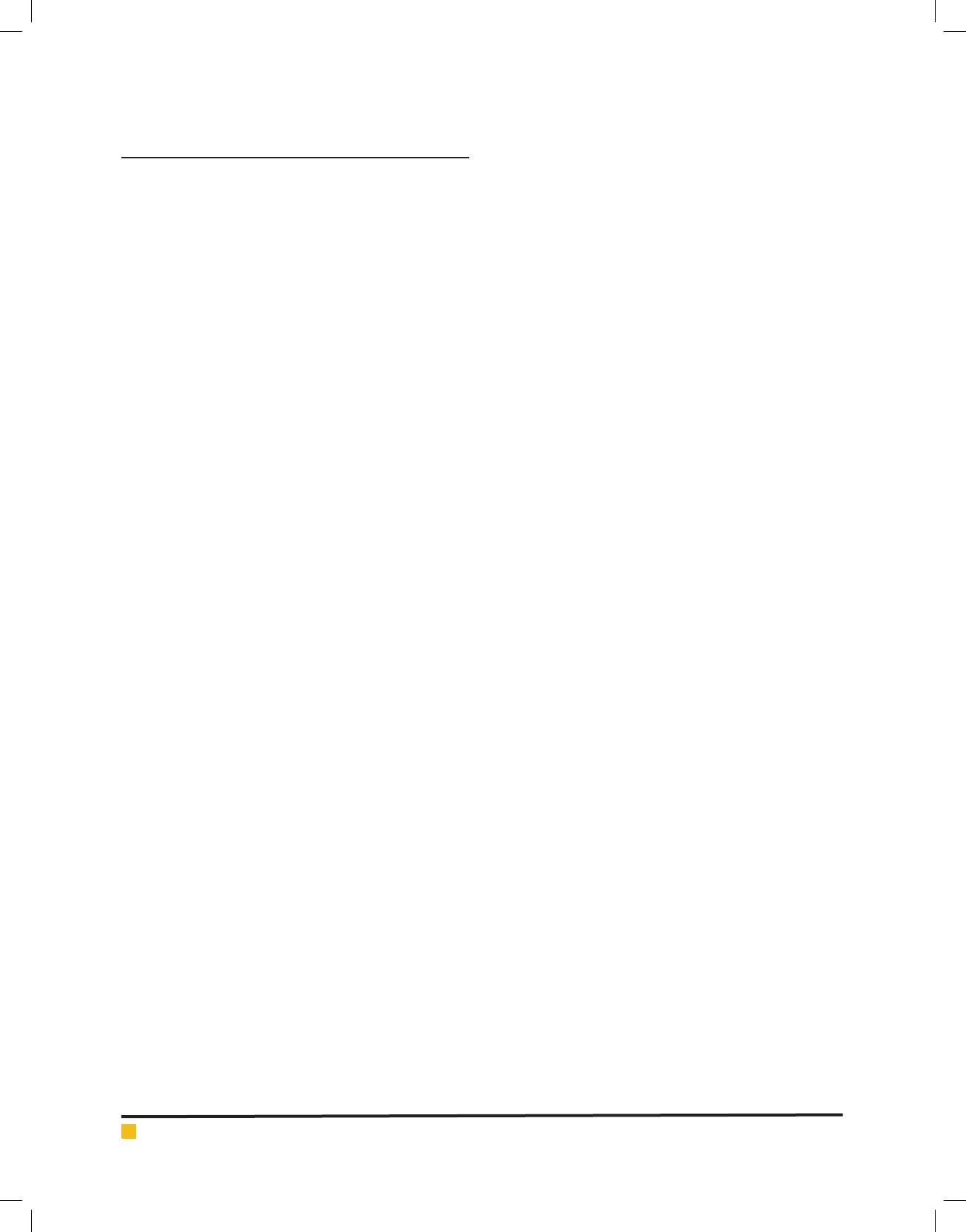
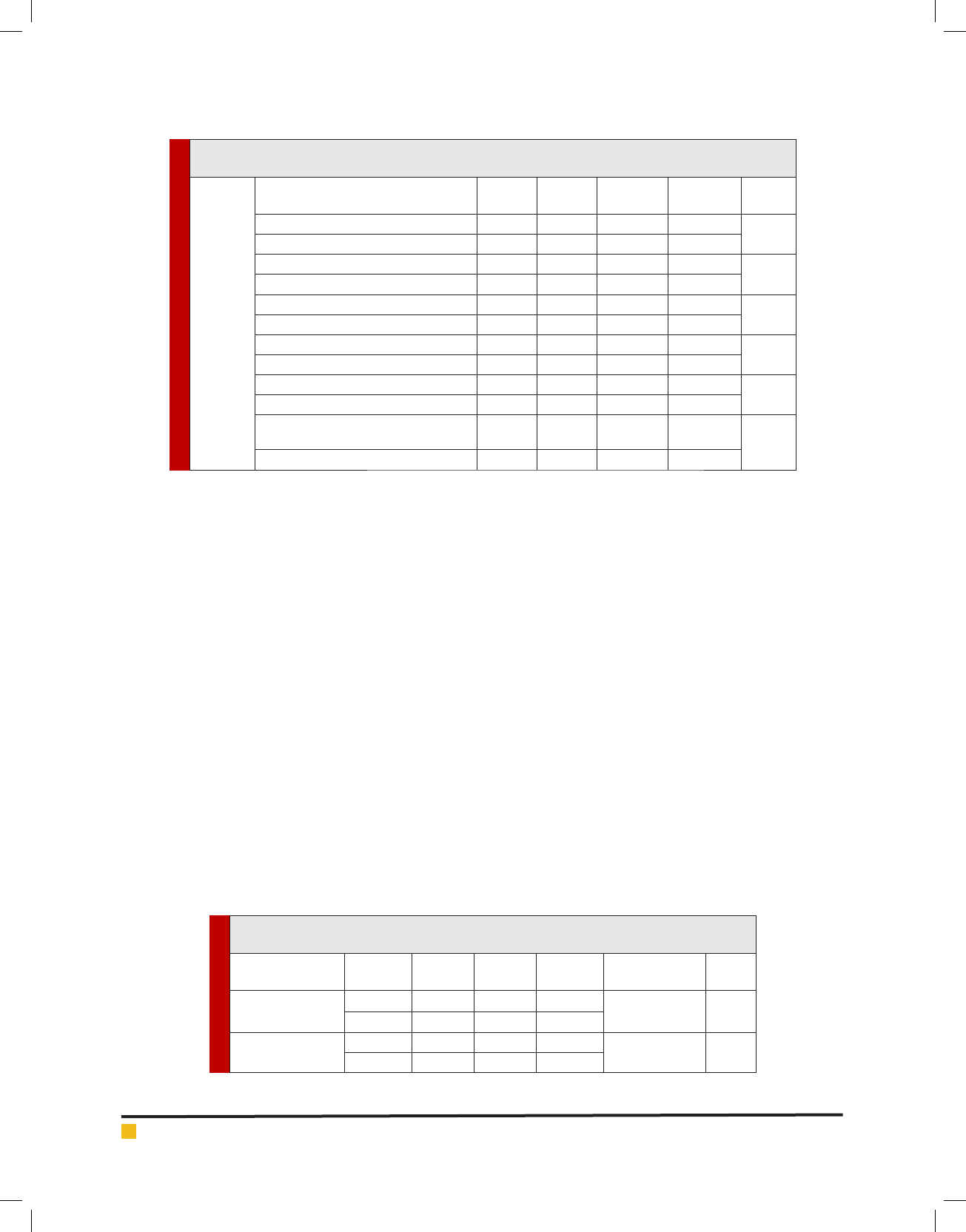
Table 1. Comparison of pre- to post-intervention change in pain intensity in both groups
based on Mann-Whitney-U test
Variable Group Average Number
Standard
Deviation
Mann- Whitney
Z statistics
Sig.
Pre medication
pain
Ketamine 40 8.90 0.93
0.14- 0.900
Fentanyl 40 8.93 0.92
Post medication
pain
Ketamine 40 2.68 0.86
0.00 0.001
Fentanyl 40 2.68 0.86
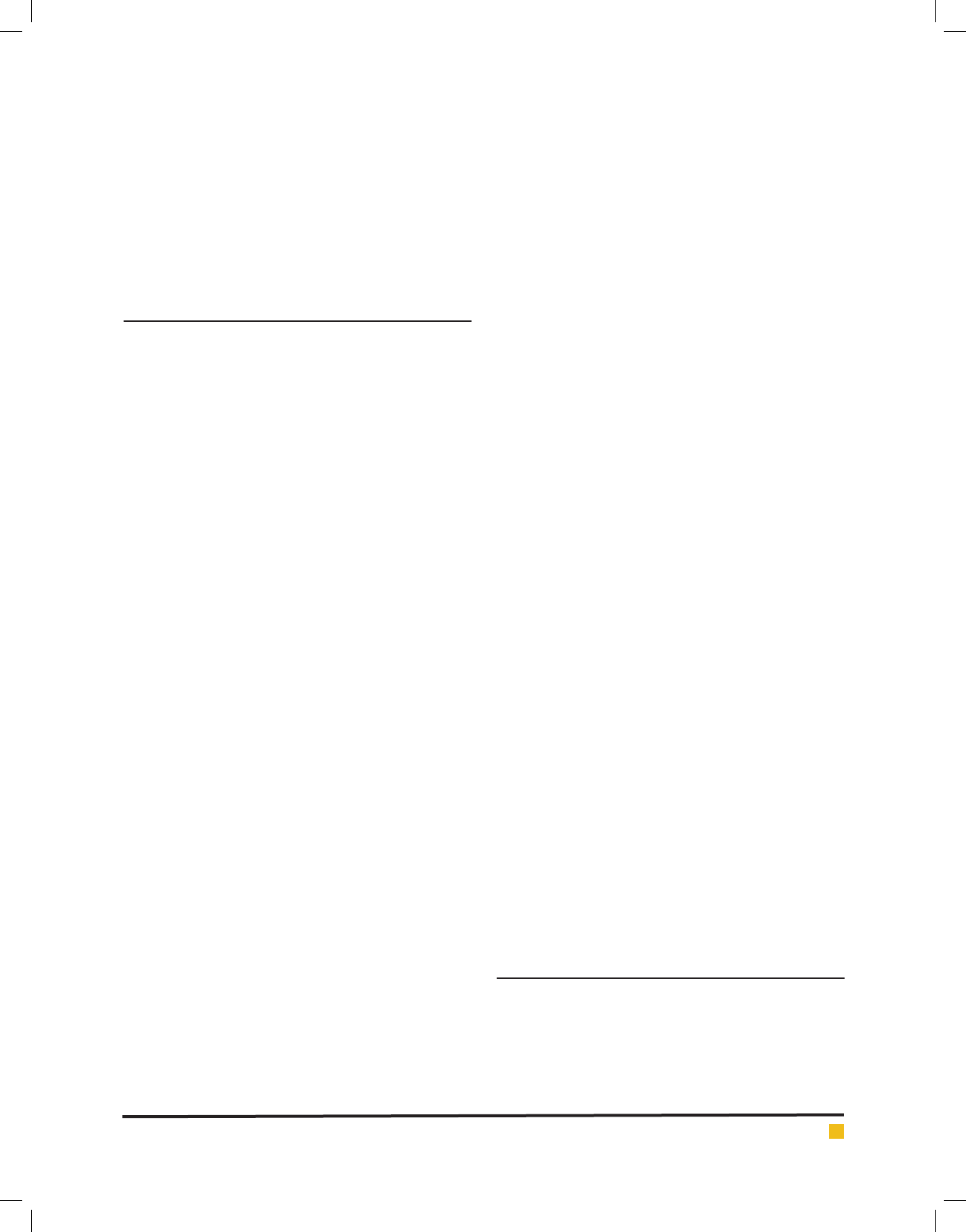
Table 2. Comparison of variable blood pressure, heart rate and oxygen saturation before
taking the drug among children in groups based on Mann-Whitney U test
Variable Group Number Average
Standard
deviation
Mann-Whitney
Z statistics
Sig.
Pre- systolic blood
pressure
Ketamine 40 107.63 5.43
1.86- 0.062
Fentanyl 40 107.38 4.86
Pre diastolic blood
pressure
Ketamine 40 66.38 5.06
0.64- 0.52
Fentanyl 40 65.63 4.83
Pre-heart rate
Ketamine 40 108.30 7.05
0.07 0.95
Fentanyl 40 108.35 7.49
Pre-RR
Ketamine 40 18.40 1.82
0.76- 0.45
Fentanyl 40 18.80 2.02
Pre- oxygen
saturation
Ketamine 40 99.50 0.96
0.05- 0.96
Fentanyl 40 99.55 0.85
dren in both groups were not statistically different in
terms of the premedication pain and are homogeneous.
The mean ± standard deviation of pain after taking Ket-
amine and fentanyl were respectively, 2.68, 2.68 and 0.86,
0.86 and there was no signi cant difference between Keta-
mine and fentanyl groups in terms of pain after taking
these drugs based on Mann-Whitney U z-statistic and sig.
value of greater than 0.05. Thus, children in both groups
were not statistically different in terms of the post-medi-
cation pain and are homogeneous. In other words, it can
be said that the analgesic effect of these drugs is similar in
children is not signi cantly different (Table 1).
According to U Mann Whitney Test, mean ± SD of
systolic blood pressure before taking ketamine and fen-
tanyl were 107.63, 107.38 and 5.43, 4.86, respectively.
Based on U Mann Whitney Test z-statistic and sig. value
of greater than 0.05, there is no difference between
the two groups of children in terms of blood pressure
before using the drug. According to U Mann Whitney
Test, mean ± SD of diastolic blood pressure before taking
ketamine and fentanyl were 66.38, 65.63 and 5.06, 4.83,
respectively. Based on U Mann Whitney Test z-statistic
and sig. value of greater than 0.05, there is no difference
between the two groups of children in terms of dias-
tolic blood pressure before using the drug. Mean ± SD
of heart rate before taking ketamine and fentanyl were
108.30, 108.35 and 7.05, 7.49, respectively. Based on U
Mann Whitney Test z-statistic and sig. value of greater
than 0.05, there is no difference between the two groups
of children in terms of heart rate before using the drug.
Mean ± SD of respiratory rate before taking ketamine
and fentanyl were 18.4,18.8 and 1.82,2.02, respectively
and based on U Mann Whitney Test z-statistic and sig.
value of greater than 0.05, there is no difference between
the two groups of children in terms of respiratory rate
before using the drug.
Mean ± SD of oxygen saturation before taking ket-
amine and fentanyl were 99.5, 99.55 and 0.96,0.85,
respectively and based on U Mann Whitney Test z-sta-
tistic and sig. value of greater than 0.05, there is no
difference between the two groups of children in terms
of oxygen saturation before using the drug. Thus, we
conclude that children in two groups are homogeneous
in terms of the above variables and there is no signi -
cant difference between them before treatment (Table 2).
Based on U Mann Whitney Test, mean ± SD of sys-
tolic blood pressure after taking ketamine and fenta-
nyl were 103.75,103.25 and 4.63,5.13, respectively and
based on U Mann Whitney Test z-statistic and sig. value
of greater than 0.05, there is no difference between the
two groups of children in terms of systolic blood pres-
sure after using the drug.
Mean ± SD of diastolic blood pressure after taking
ketamine and fentanyl were 64,65 and 4.56,4.24, respec-
BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS COMPARING THE ANALGESIC EFFECT OF INTRANASAL FENTANYL AND KETAMINE IN CHILDREN 779
Golikhatir Iraj
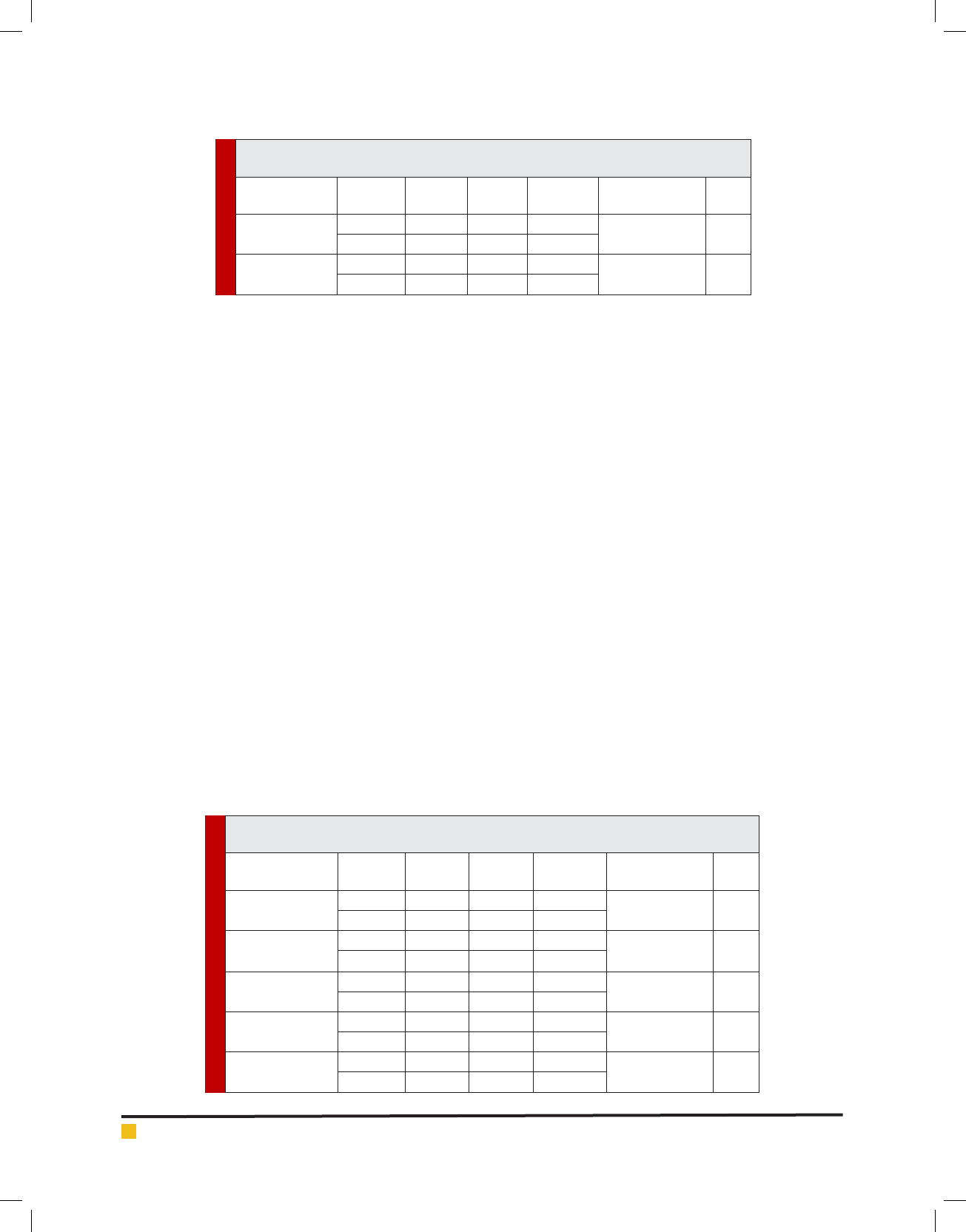
Table 3. Comparison of blood pressure, heart rate and oxygen saturation variables after drug
consumption among children in both groups based on Mann-Whitney-U test
Variable Group Number Average
Standard
deviation
Mann-Whitney
Z statistics
Sig.
Post- systolic blood
pressure
Ketamine 40 103.75 4.63
0.69- 0.4896
Fentanyl 40 103.25 5.13
Post diastolic blood
pressure
Ketamine 40 0.64 4.56
1.21- 0.2268
Fentanyl 40 0.65 4.24
Post –heart rate
Ketamine 40 102.15 5.57
1.54- 0.1242
Fentanyl 40 0.100 5.83
Post-RR
Ketamine 40 17.45 1.50
0.52- 0.6063
Fentanyl 40 17.60 1.45
Post –oxygen
saturation
Ketamine 40 99.70 0.72
1.11- 0.2666
Fentanyl 40 99.50 0.88
Table 4. Comparison of variables between children groups treated with ketamine based on Willcoxon
paired test
Ketamine
Drug type Average Number
Standard
deviation
Willcoxon
statistics
Sig.
Pre medication pain 8.90 40 0.93
5.630- 0.00009
Post-medicationpain 2.68 40 0.86
Pre medication systolicblood pressure 107.63 40 5.43
3.489- 0.0005
Post medication systolicbloodpressure 103.75 40 4.63
Pre-medicationdiastolicbloodpressure 66.38 40 5.06
2.747- 0.0060
Post-medicationdiastolicbloodpressure 0.64 40 4.56
Pre-medicationHeart ratePre 108.30 40 7.05
5.191- 0.00009
Post-medicationheart rate 102.15 40 5.57
Pre-medicationRR 18.40 40 1.82
4.359- 0.00009
Post-medicationRR 17.45 40 1.50
Pre- medication oxygen saturation 99.50 40 0.96 1.232-
0.2180
Post- medication oxygen saturation 99.70 40 0.72
tively and based on U Mann Whitney Test z-statistic and
sig. value of greater than 0.05, there is no difference
between the two groups of children in terms of diastolic
blood pressure after using the drug.
Mean ± SD of heart rate after taking ketamine and fen-
tanyl were 102.15,100 and 5.57,5.83, respectively and based
on U Mann Whitney Test z-statistic and sig. value of greater
than 0.05, there is no difference between the two groups of
children in terms of heart rate after using the drug.
Mean ± SD of respiratory rate after taking ketamine
and fentanyl were 17.45,17.60 and 1.5,1.45, respectively
and based on U Mann Whitney Test z-statistic and sig.
value of greater than 0.05, there is no difference between
the two groups of children in terms of respiratory rate
after using the drug.
Mean ± SD of oxygen saturation after taking ketamine
and fentanyl were 99.70,99.50 and 0.72,0.88, respectively
and based on U Mann Whitney Test z-statistic and sig.
value of greater than 0.05, there is no difference between
the two groups of children in terms of oxygen saturation
after using the drug. Thus, we conclude that there is no
statistically signi cant difference between children in the
two groups after taking the drugs and the effect of these
drugs on children is similar in this study (Table 3).
Now, after examining the mean differences between
studied variables in two groups of children, we inves-
tigate the differences between these variables in each
group before and after drug use in this section. Accord-
ing to Willcoxon statistics and sig. value of smaller than
0.05, there was statistically signi cant difference in
the ketamine group among mean values of pain, sys-
tolic blood pressure, diastolic blood pressure, heart rate
and respiratory rate before and after taking ketamine.
In other words, ketamine is effective in reducing blood
pressure (systolic and diastolic), heart rate and respira-
tory rate except for oxygen saturation variable (Table 4).
780 COMPARING THE ANALGESIC EFFECT OF INTRANASAL FENTANYL AND KETAMINE IN CHILDREN BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS
Golikhatir Iraj
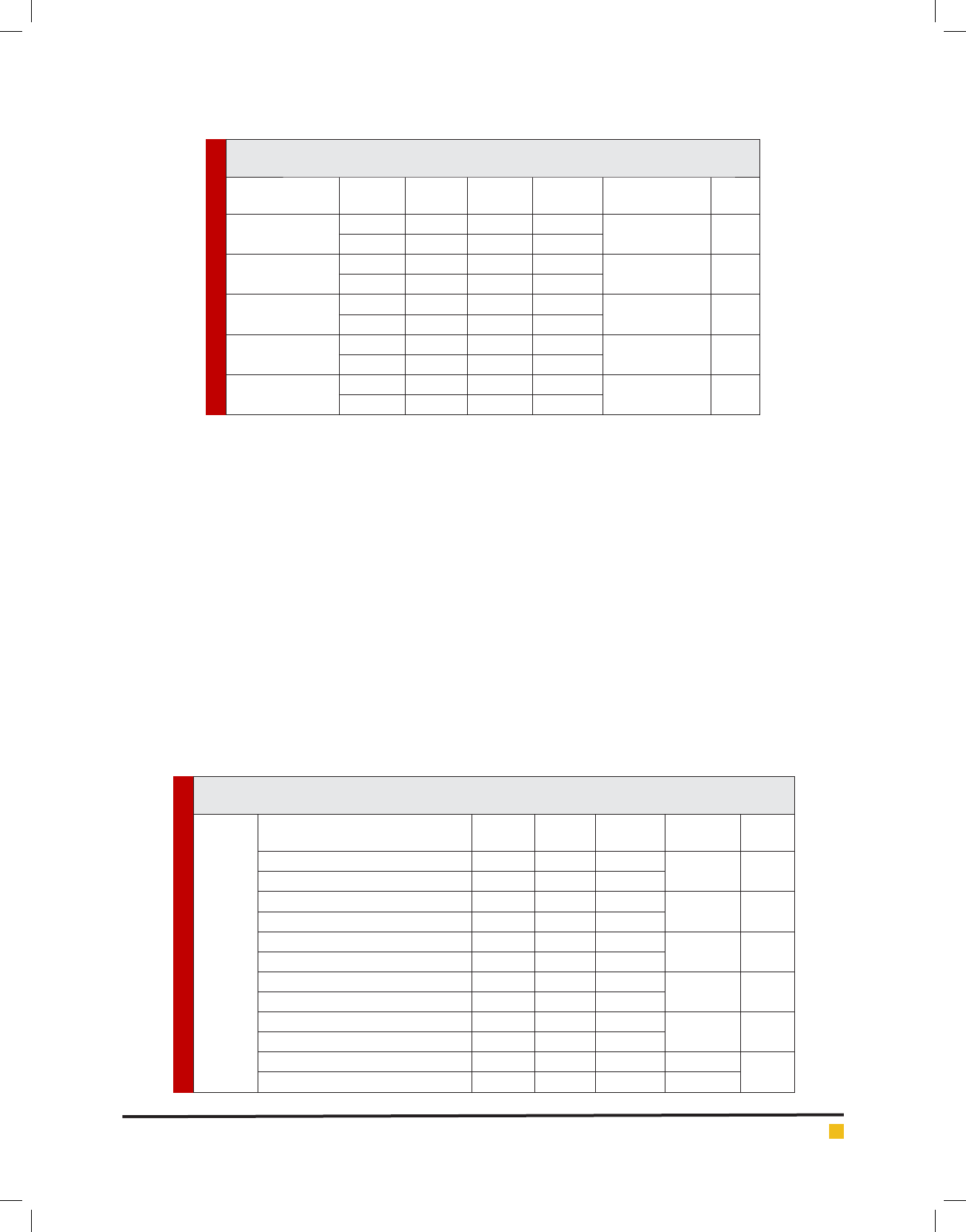
Table 5. Comparison of variables between children groups treated with fentanyl based on Willcoxon
paired test
Fentanyl
Drug type Average Number
Standard
deviation
Willcoxon
statistics
Sig.
Pre-medication pain 8.93 40 0.92 5.630-
0.00009
Post-medication pain 2.68 40 0.86
Pre-medication systolic blood pressure 109.88 40 4.87 3.489-
0.0005
Post-medication systolic blood pressure 103.25 40 5.13
Pre-medication diastolic blood pressure 65.63 40 4.83 2.747-
0.0060
Post-medication diastolic blood pressure 0.65 40 4.24
Pre-medication Heart Pre rate 108.35 40 7.49 5.191-
0.00009
Post- medication heart rate 0.100 40 5.83
Pre- medication RR 18.80 40 2.02 4.359 -
0.00009
Post-medication RR 17.60 40 1.45
Pre-medication oxygen saturation 99.55 40
0.85
1.232-
0.2180
Post-medication oxygen saturation 99.50 40 0.88
Table 6. Comparison of parents and the medical team satisfaction with analgesic effect of
Ketamine and fentanyl based on the Mann-Whitney U test
Variable Group Number Average
Standard
deviation
Mann Whitney
Z statistics
Sig.
Parental satisfaction
Ketamine 40 73.75 7.40
0.991 0.322
Fatanyl 40 75.25 6.79
Medical Team
Satisfaction
Ketamine 40 74.75 5.06
0.890- 0.374
Fantanyl 40 75.75 5.01
According to Willcoxon statistics and sig. value of
smaller than 0.05, there was statistically signi cant dif-
ference in the fentanyl group among mean values of
pain, systolic blood pressure, heart rate and respiratory
rate before and after taking fentanyl. In other words,
fentanyl is effective in reducing blood pressure (systolic
and diastolic), heart rate and respiratory rate except for
diastolic blood pressure and oxygen saturation variable
(Table 5)
Based on the Mann-Whitney test, mean ± SD of par-
ents’ satisfaction with analgesic effect of ketamine and
fentanyl were respectively 73.75, 75.25 and 7.40 6.79;
so based on the Mann-Whitney z-statistic and sig. value
of more than 0.05, there is no signi cant difference
between parental satisfaction with the ketamine and
fentanyl analgesic effect.
Mean ± SD of medical team satisfaction with anal-
gesic effect of ketamine and fentanyl were respectively
74.75, 75.75 and 5.06, 5.01; so based on the Mann-
Whitney z-statistic and sig. value of more than 0.05,
there is no signi cant difference between medical team
satisfaction with the ketamine and fentanyl analgesic
effect (Table 6).
The results showed that there is no signi cant dif-
ference between analgesic effects of these two drugs
in studied children. These results are consistent with
results obtained by Gradyns (2015) in America where
the level of pain reduction was similar in both groups.
The result of the current study are also consistent with
the results of the study conducted by Yeamen et al.,
(2013) who examined the effects of fentanyl and keta-
mine on pain and pain caused by intraoperative ulcer
and concluded that both fentanyl and ketamine are
effective in pain relief and analgesia compared with
placebo, but are not signi cantly different from each
other: but the results of this study are inconsistent with
results of the study conducted by (Julie 2013) in Iran,
in which the difference between ketamine and fenta-
nyl is relatively low and negligible and this effect has
been reported to be due to the analgesic properties of
ketamine.
The results of studies on the effects of fentanyl and
ketamine are different, which could be due to different
injury, choice of different patients, lack of blinding in the
studies and type of the study design. The results showed
that except for the oxygen saturation variable, ketamine

BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS COMPARING THE ANALGESIC EFFECT OF INTRANASAL FENTANYL AND KETAMINE IN CHILDREN 781
Golikhatir Iraj
was effective in reducing blood pressure (systolic and
diastolic), heart rate and respiratory rate and fentanyl
was also effective in reducing systolic blood pressure,
heart rate and respiratory rate except for diastolic blood
pressure and oxygen saturation variables. Very limited
side effects were observed that were not tested due to
being limited. Five derealization cases in the ketamine
Group and three vomiting and three nausea cases in the
fentanyl Group were reported. The results of the present
study are consistent with the results of the study con-
ducted by Gradyns (2015) who showed that ketamine
has more side effects.
In a study on changes in respiratory rate, Javaher-
forooshet al., (2006)showed that ketamine and fentanyl
lead to the highest and lowest respiratory rates, which
may be due to the respiratory stimulant and respiratory
depression effects of ketamine and fentanyl, respec-
tively. In a study, (Tsze et al., (2012) showed that keta-
mine was well tolerated in pediatric pain management
and one case led to vomiting. The results showed that
the difference between the satisfaction of parents and
the medical team of ketamine and fentanyl analgesic
effect is not signi cant. Parents’ average satisfaction
with the analgesic effect of ketamine in children is
73.75% and medical team’s average satisfaction with
the analgesic effect of fentanyl was equal to 74.75%.
The same amount for ketamine and fentanyl was 83%
and 82%, respectively in a study conducted by Gradyns
et al. (2015).
In a study on the effects of intranasal fentanyl for
pain relief in children with musculoskeletal trauma,
Saunders et al. (2010) reported satisfaction percentage
of 79% and 74% respectively for parents and the medi-
cal team. One of the limitations of this study include
that patients might have usednarcotic or any other
analgesic drug for pain relief prior to admission to the
emergency center. So, this issue could affect the out-
come of the research and that’s why this issue should
be considered in future studies and prevents the entry
of similar cases to the study. Considering the small
number of similar studies, further studies are needed
to prove the effectiveness and compare the intrana-
sal effect of these drugs. Another limitation was that
pain was different for children because they had dif-
ferent experiences of pain and assess pain in children
were not easy. Therefore, it is recommended to consider
larger sample size in next studies and level of anxi-
ety in children and the effect of these drugs on anxi-
ety be measured simultaneously because children have
different experiences of pain and anxiety is effective
in measuring the severity of pain. Also, ketamine and
fentanyl analgesic effects and side effects and different
methods of administration should be investigated in
future studies.
REFERENCES
Atkinson P, Chesters A, Heinz P. (2009). Pain management and
sedation for children in the emergency department. BMJ. 30;
339: 4234.
Banks, W. A., M. J. During, et al. (2004). Brain uptake of the
glucagon-like peptide-1 antagonist exendin (9 39) after intra-
nasal administration. J PharmacolExpTher. 309(2): 469-75.
Brian M. Radvansky, Khushbu Shah, Anant Parikh, Anthony
N. Sifonios, Vanny Le, and Jean D. (2015). Eloy Role of Keta-
mine in Acute Postoperative Pain Management, Department
of Anesthesiology and Peri-Operative Medicine. Rutgers-New
Jersey Medical School.
Graudins A, Meek R, Egerton-Warburton D, Oakley E, Seith R.
(2015). The PICHFORK (Pain in Children Fentanyl or Ketamine)
trial: a randomized controlled trial comparing intranasal keta-
mine and fentanyl for the relief of moderate to severe pain in
children with limb injuries. Ann Emerg Med. 65(3):248-254.
Hadayi M, Rezaeian M. (2011). The ef cacy of Ketamine gar-
gles on postoperative sore throat. Zahedan J Res Med Sci
(ZJRMS).13(5): 12-16.
Hazinski MF. Analgesia, sedation, and neuromuscular block-
ade. 3 rd ed. Chapter 5: Nursing care of the critically ill child.
Elsevier Mosby; 2013p.78.
Javaherforoosh F, Pipelzadeh M, Salary A, Zabihi A. (2006).
Comparison of Preanesthetic Sedation after Intranasal Admin-
istration of Fentanyle, Ketamin and Midazolam. Armaghane
Journal. 11(2): 19-27. (Persian)
Marcia L. Buck, Pharm.D. (2013). FCCP, FPPAG Options for
Intranasal Procedural Sedation and Analgesia in Children.
Pediatric Pharmacotherapy is available on the University of
Virginia School of Medicine .9(8).
Moore A, Straube S, Derry SH, McQuay HJ. (2010). Chronic low
back pain analgesic-A methodological mine eld. PAIN, 149:
431-434.
Murphy A, O’Sullivan R, Wakai A. (2014). Grant TS Intrana-
sal fentanyl for acute pain in children 1Paediatric Emergency
Research Unit (PERU), Department of Emergency Medicine,
National Children’s Research Centre.
MajidiNejad S, Goudarzi L, Esmaeilian M, Heidari F. (2017).
The Effect Ondansetron on Reducing Nausea Caused By Ket-
amine in Pediatric Patients Visiting Emergency Department;
a Clinical Trial. Journal of Emergency Medicine Iran. 4(1):
15-19. (Persian)
Saunders M, Adelgais K, Nelson D. (2010).Use of intranasal fen-
tanyl for the relief of pediatric orthopedic trauma pain. Depart-
ment of Pediatric Emergency Medicine, Medical College of Wis-
consin, Milwaukee, USA AcadEmerg Med. 17(11):1155-61.
Shahryari H, Alavi S.M, Ferasat Kish R, Motamed N, Karimi M.
(2010). Comparison of propofol effect with Ketamine for sedation
induction in pediatric patients who underwent cardiol catheteri-
zation. Iranian South Medical Journal .13(1): 16-23. (Persian).
Tsze D, Steele D, Machan J, Akhlaghi F, Linakis J. (2012). Intra-
nasal Ketamine for Procedural Sedation in Pediatric Laceration
Repair. Pediatric Emergency Care. 28(8):767-770.

782 COMPARING THE ANALGESIC EFFECT OF INTRANASAL FENTANYL AND KETAMINE IN CHILDREN BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS
Golikhatir Iraj
Veldhorst J. (2013). Intranasal delivery of rapid acting
drugs:Studies of pharmacokinetics, effect, tolerability and sat-
isfaction, UniversitairePers Maastricht. PhD Thesis: 141
Will Julie C. (2013). Preventable Hospitalizations and Emer-
gency Department Visits for Angina, United States, 1995–
2010. Preventing Chronic Disease. 10.
Yeaman F, Oakley E, Meek R, Graudins A. (2013). Sub-dissoci-
ative dose intranasal ketamine for limb injury pain in children
in the emergency department1Southern Health Emergency
Medicine Research Group, Southern Clinical School, Faculty
of Medicine, Nursing and Health Sciences, Monash Univer-
sity, Clayton, VIC 3168, Australia Emerg Med Australas. 25(2):
161-7.