
Microbiological
Communication
Biosci. Biotech. Res. Comm. 10(4): 752-763 (2017)
Pharmacological activity of different solvent extracts
of
Tribulus terrestris
against multi drug resistant
Staphylococcus aureus
isolated from post-operative
wound patients
M.S. Uma Maheshwari, R. Rajendran and S. Vijayalakshmi
1
Associate Professor, Department of Microbiology, Tiruppur Kumaran College for Women, Tiruppur, India
2
Associate Professor, Department of Microbiology, PSG College of Arts and Science, Coimbatore, India
3
Research Scholar, PG and Research Department of Zoology, Division of Microbial Technology, Chikkanna
Govt. Arts College, Tirupur, India
ABSTRACT
Despite advances in infection control surgical site infections formerly called surgical wound infections, remain a substantial cause of
morbidity and mortality among hospitalized patients. The post-operative surgical site infection is the third most commonly reported
nosocomial infections, accounting for a quarter of all such infections. The early stages of invasive infection caused by Staphylococcus
aureus, also play major role in this process. In this present study a total of 50 pus samples were collected from patients having postop-
erative wound infections from the different surgical departments in the PSG Institute of Medical Sciences and Reasearch (PSG IMSR),
Coimbatore during Dec 2016 to July 2017. Identi cation of bacterial isolates was done by standard microbiological techniques. Further,
the antimicrobial susceptibilities were done against following antibiotics, Penicillin (10 units), Chloramphenicol (30mcg), Vancomycin
(30mcg), Streptomycin (10mcg), Neomycin (30mcg), Ampicillin (10mcg), Amoxicillin (10mcg), Amikacin (10mcg), Gentamycin (10mcg)
and Cipro oxacin (10mcg). Among these strains 100%, 30%, 90%, 50%, 40%, 100%, 50%, 20%, 30% and 60% were found to be exhibit-
ing a signi cant degree of resistance to antibiotics tested. Currently, the development of bacterial resistance has necessitated the search
for new antibacterial agents to combat the infectious disease using bio-medically active different solvent extract of Tribulus terrestris
for antimicrobial activity. In this present study the maximum inhibition was observed in Ethyl acetate, moderate inhibition in Ethanol,
minimum inhibition in Acetone, Chloroform, Methanol and no inhibition in aqueous and Petroleum ether. The results con rm that, the
plant appears to contain substances that exhibit broad antimicrobial activity against wound pathogens.
KEY WORDS:
STAPHYLOCOCCUS AUREUS, ANTIBIOTIC RESISTANCE, ANTIMICROBIAL ACTIVITY OF TRIBULUS TERRESTRIS
, POSTOPERATIVE
WOUND INFECTION
752
ARTICLE INFORMATION:
*Corresponding Author: maheswariuma938@gmail.com
Received 27
th
Oct, 2017
Accepted after revision 27
th
Dec, 2017
BBRC Print ISSN: 0974-6455
Online ISSN: 2321-4007 CODEN: USA BBRCBA
Thomson Reuters ISI ESC and Crossref Indexed Journal
NAAS Journal Score 2017: 4.31 Cosmos IF: 4.006
© A Society of Science and Nature Publication, 2017. All rights
reserved.
Online Contents Available at:
http//www.bbrc.in/
DOI: 10.21786/bbrc/10.4/22
Uma Maheshwari, Rajendran and Vijayalakshmi
INTRODUCTION
Recurrently, the post operative hospital acquired infec-
tions constitutes a major problem in surgical patients
contributing to morbidity, mortality and increased
resource utilization and health care costs. Patients in
whose surgical site infection develop have an increased
number of associated complications, the high risk of
requiring a stay in ICU have two to three times higher
risk of mortality. Their hospital stay is increased by 7 to
12 days and they are ve times more likely to require
readmission.The post-operative wound infections can
be caused by different groups of microorganisms like
bacteria, fungi and protozoa. However, different kind of
microorganisms can exist in polymicrobial communi-
ties, especially in the margins of wounds and in chronic
wounds (Percevil and Bowler, 2004, Anaya and Del-
linger, 2006 and Jain et al. 2014) .
The risk of invasive burn wound infection is in u-
enced by the extent and depth of the burn injury, vari-
ous host factors, and the quantity and virulence of the
microbial ora colonizing the wound (Church et al.
2006). The common burn wound pathogens are Staphy-
lococcus aureus, Pseudomonas aeruginosa, Escherichia
coli and Klebsiella spp., which produce a number of
virulence factors that are important in the pathogenesis
of invasive infection (Tredget et al. 2004) are frequently
associated with post-operative wound infection. One of
the major problems worldwide is the increase in anti-
biotic-resistant strains of bacteria, mainly in hospitals,
that poses constrain for their control without consider-
able resources and expenditure (Ayliffe et al. 2000). It
has been well documented that most of the clinical iso-
lates of Staphylococcus aureus are multiple-drug resist-
ant currently used antibiotics. The problem of microbial
resistance is increasingly alarming and the outlook for
the use of antimicrobial drugs in the future is still uncer-
tain (Nascimento et al. 2000 Naaz 2017).
Due to this treatment of postoperative wound infec-
tion with antibiotics is becoming a challenge for the sur-
geon as multidrug resistance is reported to be high. It is
therefore, important to have knowledge regarding the
prevalent microorganism in the surgical units and their
susceptibility patterns to antibiotics so that proper treat-
ment can be started earlier. It is essential to take appro-
priate steps to curtail the spread of infection within
the unit (Tahir, 1995). One of the measures to combat
this increasing rate of resistance is to have continuous
investigations into new, safe and effective antimicrobi-
als as alternative agents to substitute with less effective
ones. Plants have been traditionally proved to be a rich
source of novel drug compounds, as the herbal mix-
tures have made large contributions to human health
and well-being (Ergin and Mutlu, 1999). A wide vari-
ety of secondary metabolites, such as tannins, terpe-
noids, alkaloids, quinones and avonoids are endowed
with antimicrobial properties (Lewis and Ausubel, 2006
Mohammad et al 2015).
Currently, the research is being carried out to inves-
tigate ethno-botanical uses of plants prevailing among
native people (Sibanda and Okoh, 2007). There are
numerous reports evidencing the antibacterial activity
of plants against microorganisms (Sundharameshwari
and Radhika, 2007). Thus, it is very much necessary
to analyze the potential of the plants in combating the
antibiotic resistant organisms, (Al Maofari 2013).
Recurrently, the Tribulus terrestris is a strong herbal
remedy which is used for various purposes in folk and
modern medicine and sport, as well. It has been used
as a tonic, aphrodisiac, astringent, analgesic, stomachic,
anti-hypertensive, antibacterial, antifungal, skin infec-
tion and urinary anti-septic (Al-Bayati and Al-Mola,
2008). T. terrestris has been commonly used as a diuretic
as well as treatment for hypertension, hypercholester-
olemia and colic pains. (Wang et al., 1990).The leaves
of Tribulus terrestris are used traditionally for the treat-
ment of various kinds of wound. T. terrestris is found to
be a rich source of calcium (Bourke et al., 1992). Extract
from T. terrestris has immune stimulatory and antimi-
crobial effect (Sengul et al., 2009, Al Maofari 2013 )
against pathogens. Recently Naz et al., (2017) stated that
the leaf extracts of plants with a history of traditional
use should be tested using modern methods for activi-
ties against multidrug resistant human pathogens, with
the aim of discovering potential new drugs. So, hence
the present study has made an attempt to point out the
different solvent extraction of Tribulus terrestris against
multidrug resistant Staphylococcus aureus isolated from
wound of post-operative patients.
MATERIALS AND METHODS
A total of 50 pus samples was collected from patients
aseptically with a sterile cotton swab suffering from post
operative wound infection at the PSG Institute of Medi-
cal Sciences and Reasearch (PSG IMSR), Coimbatore
for the period of Dec 2016 – July 2017. For collection,
the wound sample was washed thoroughly with normal
saline and it was placed in the ice box. After reaching to
the laboratory of PG and Research Department of Micro-
biology, PSG College of Arts and Science, Coimbatore.
Finally the samples were incubated at 37ºC for 24 hours
in isolation of wound pathogens.
All the strains isolated from wound samples were seri-
ally diluted, plated onto Mannitol Salt Agar, it was incu-
bated at 37°C for 48hours. The colonies with characteristic
growth were subjected to routine biochemical test accord-
ing to the Bergey’s manual of systematic bacteriology.
BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS PHARMACOLOGICAL ACTIVITY OF DIFFERENT SOLVENT EXTRACTS OF
TRIBULUS TERRESTRIS
753

Uma Maheshwari, Rajendran and Vijayalakshmi
The standard Kirby Bauer disk diffusion method was
used to determine the antimicrobial pro le of wound
isolates against 10 antimicrobial agents such as Peni-
cillin (10 units), Chloramphenicol (30mcg), Vancomy-
cin (30mcg), Streptomycin (10mcg), Neomycin (30mcg),
Ampicillin (10mcg), Amoxycillin (10mcg), Amika-
cin (10mcg), Gentamycin (10mcg) and Cipro oxacin
(10mcg). The diameters of the inhibition zone were
measured using a ruler under a colony counter appara-
tus. The results were expressed as sensitive (S), margin-
ally susceptible (I), and resistant (R).
The plants of Tribulus terrestris were collected from
the dry lands of Coimbatore and Tirupur regions and
identi ed. The identi cation was authenticated by the
Botanical Survey of India ,Tamilnadu Agricultural Uni-
versity Campus (TNAU),Coimbatore. The plant extracts
were prepared as per standard procedures. The leaf of T.
Terrestris plant (Fig. 1) were washed with sterile distilled
water to remove dirt, dried under shade and were ground
to powder using household electric blender. The 20g of
dry powdered Terrestris was weighed and transferred to
a conical ask containing 100 ml of 80% of Ethanol,
methanol, Chloroform, acetone, Ethyl acetate and Petro-
leum ether (Fig. 2) respectively and allowed to soak at
ambient temperature for 72 hours. The extract was than
ltered using Whatman no 1 lter paper and the ltrates
were concentrated in vaccum at 40°C using a rotary
evaporator. Residues of the extracts made into suspen-
sions using sterile distilled water and sterile dimethyl
sulphoxide at a concentration of 500 mg/ml of Tribulus
extracts respectively.
The leaf of the puri ed Tribulus extract was tested
for antibacterial activity by standard agar well diffusion
method against pathogenic bacteria S.aureus. The pure
culture of bacterial pathogen was sub cultured on nutri-
ent agar. 20ml of nutrient agar were poured into petri-
plates. The well of 6mm diameter were made on nutrient
agar using gel puncture 100μl of fresh over night grown
culture of the respective bacteria were spread on nutri-
ent agar medium containing petriplates. The culture was
FIGURE 1. Tribulus terrestris
FIGURE 2. Extraction of Solvent from bioactive leaf
of Tribulus terrestris a) Petroleum ether, b) Acetone, c)
Ethanol, d) Aqueous, e) Ethyl acetate, f) Methanol, g)
Chloroform
FIGURE 3. Colony of Staphylo-
coccus aureus on Mannitol Salt
agar
754 PHARMACOLOGICAL ACTIVITY OF DIFFERENT SOLVENT EXTRACTS OF
TRIBULUS TERRESTRIS
BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS
Uma Maheshwari, Rajendran and Vijayalakshmi
BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS PHARMACOLOGICAL ACTIVITY OF DIFFERENT SOLVENT EXTRACTS OF
TRIBULUS TERRESTRIS
755
swabbed uniformly using a sterile cotton swab and then
50μl of the plant extract solution was loaded into the
well. After incubation at 37ºc for 24 hours the different
zone of inhibition was measured.
Minimum inhibition concentration was made by the
lowest cost of the extract of T. Terrestris leaves where
it can show the bactericidal and bacteriostatic effect.
The test was performed in 96 well micro titer plates.
Microtiter plate wells from each column in row 1 were
marked and 100μl (500mg/ml) of stock (aqueous and
solvent extract) was added. 50μl of sterile distilled water
was added to rows 2-12. Two fold serial dilutions were
performed by transferring 50μl of solution from row 1
to 2, using a multichannel pipette. This was repeated
down the row 2 to 12. 40μl of double strength nutri-
ent broth and 10μl of bacterial culture was added to all
the wells in a separate column, so the nal concentra-
tion of the inoculum in all the wells. Finally, to prevent
dehydration, the plates were covered with a plastic cover
and then incubated at 37ºC for overnight. The bacterial
growth was determined after adding of 40μl of 2, 3, 5
Tri Phenyl Tetrazolium Chloride Red (0.02mg/ml). The
Minimum inhibitory concentration (MIC) of the isolates
was taken as the lowest concentration of the antibiotic
of which the bacteria tested did not show visible growth
(Table: 1).
RESULTS AND DISCUSSION
Totally 50 clinical wound samples, 10 positive Staphylo-
coccus aureus were isolated from different wound sites
of patients admitted in surgical ward in the PSG Insti-
tute of Medical Sciences and Research (PSG IMSR) (Fig.
2), Coimbatore. All the wound samples were tested on
Mannitol Salt Agar (MSA) for the isolation of S.aureus.
On MSA, S.aureus colonies were appeared yellow colour
which is containing mannitol to detect mannitol fermen-
tation. In the routine microbiological laboratory, prompt
identi cation of the S. aureus was done by grams stain-
ing, catalase, oxidase, coagulase, IMViC, nitrate reduc-
tion test, triple sugar iron agar test. After performing, all
these tests was con rmed as S.aureus.
All the 10 S.aureus isolates were tested invitro to
determine their antibiotic susceptibility patterns by
antibiotic disc diffusion method and the following anti-
biotic discs were used for this assay are Penicillin (10
units), Chloramphenicol (30mcg), Vancomycin (30mcg),
Streptomycin (10mcg), Neomycin (30mcg), Ampicillin
(10mcg), Amoxycillin (10mcg), Amikacin (10mcg), Gen-
tamycin (10mcg) and Cipro oxacin (10mcg).. Totally 10
antibiotic discs were used to identify vancomycin resist-
ant Staphylococcus aureus. All the isolates were shown
multiple antibiotic resistances to the antibiotic tested
none of the isolates showed 100% resistant to antibi-
otics tested. The maximum resistant pattern percentage
(80%) was recorded in strain no MBUM02, MBUM06 and
MBUM07 followed by minimum resistant pattern per-
centage (30%) was recorded in strain no MBUM01 and
MBUM08.
Among 10 strains, 2 isolates were shown 30% resist-
ant against all the antibiotics tested with strain No.
MBUM01 and MBUM08 both were showed equally with
the following antibiogram: VAN- AMP-P followed by
the strain no. MBUM10, MTUM04 were showed 40%
with antibiogram of STR-CHL-AMP-P, STR-CHL-AMP-
CIP. Two strains MBUM03 and MTUM05 were showed
50% against the antibiotics tested with antibiogram
of VAN-AMX-NEO-AMP-P followed by one strain
no. MBUM09 was exhibit 70% resistant to antibiotics
tested: VAN-AMX-AMP-P-GEN-AK-CIP, these antibio-
gram was recorded in the isolate. Finally, three strains
MBUM02, MBUM06 and MBUM07 was showed the
highest resistant percentage of 80% with the antibio-
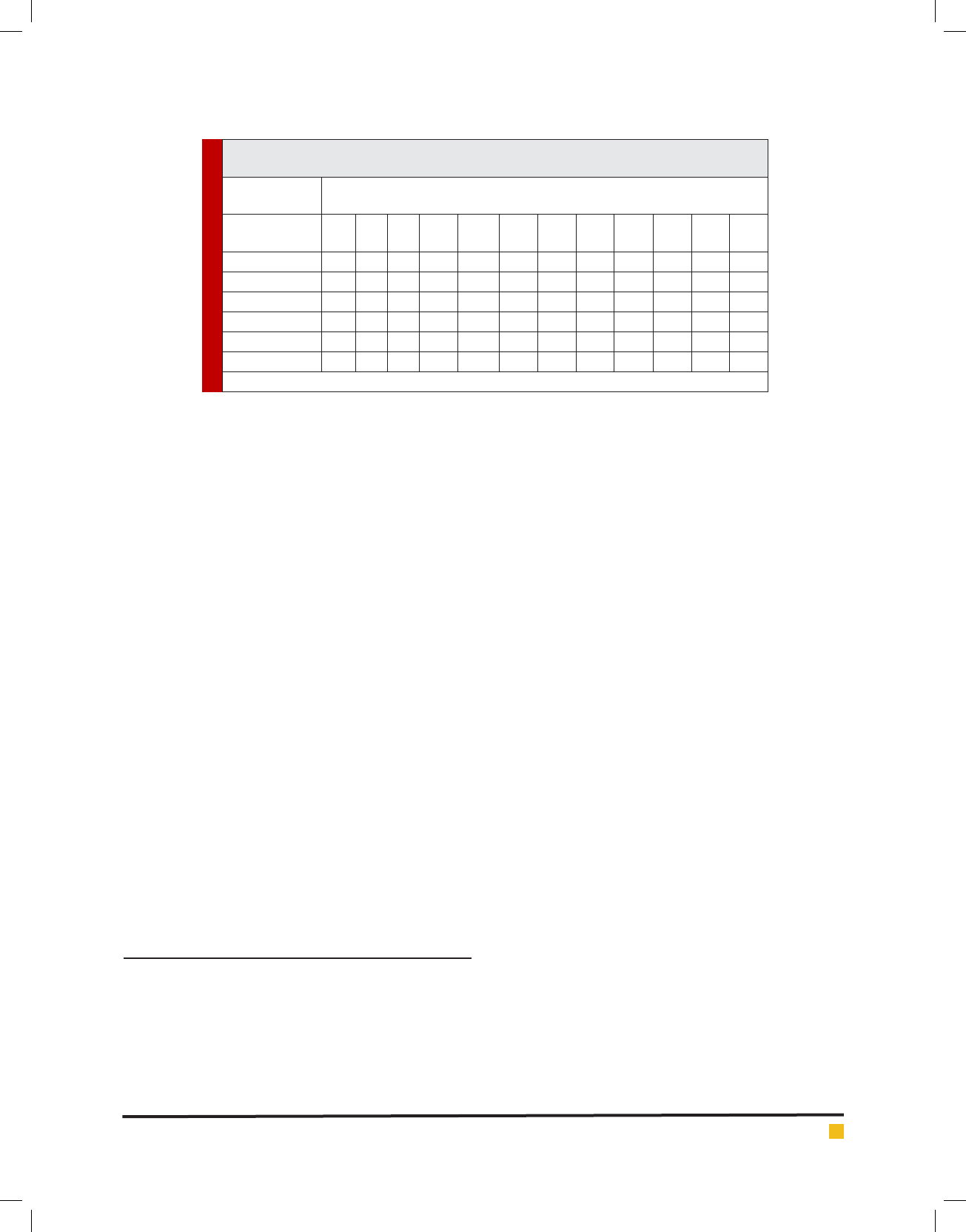
Table 1. MIC of different strains of Petroleum ether extract of Tribulus terrestris by broth
dilution method
Test
microorganism
Plant Extract (Petroleum ether)
Concentration (500mg/ml)
100
(μl)
50
(μl)
25
(μl)
12.5
(μl)
6.25
(μl)
3.12
(μl)
1.56
(μl)
0.78
(μl)
0.39
(μl)
0.19
(μl)
0.09
(μl)
0.04
(μl)
MTUM02 - - + + + + + + + + + +
MTUM03 - - + + + + + + + + + +
MTUM05 - - + + + + + + + + + +
MTUM06 - - + + + + + + + + + +
MTUM07 - - + + + + + + + + + +
MTUM09 - - + + + + + + + + + +
(-) indicates absence of growth and (+) indicates presence of growth of microorganisms.
Uma Maheshwari, Rajendran and Vijayalakshmi
756 PHARMACOLOGICAL ACTIVITY OF DIFFERENT SOLVENT EXTRACTS OF
TRIBULUS TERRESTRIS
BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS
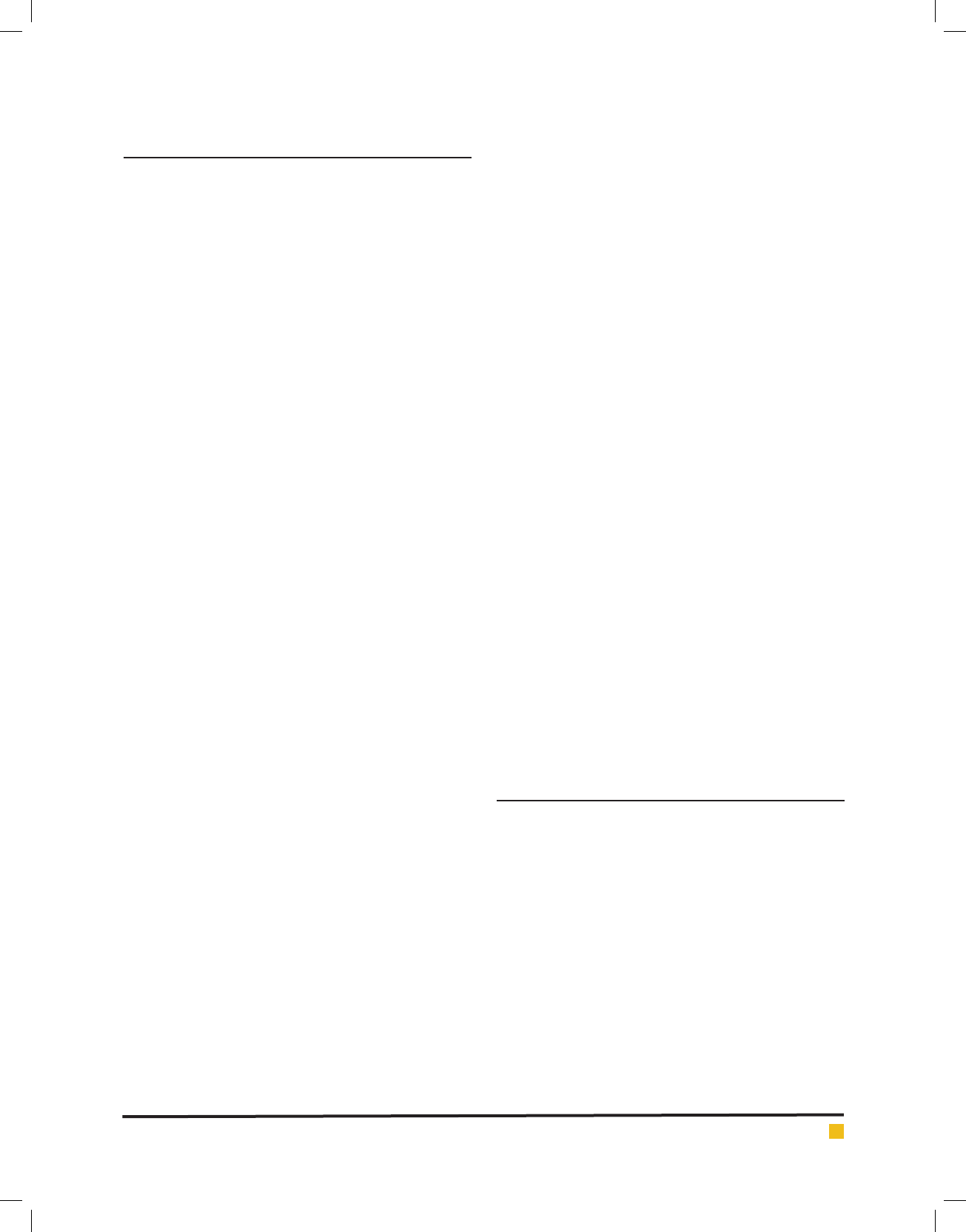
FIGURE 4. Antimicrobial activity of different solvent extract of Tribulus terrestris against
Staphylococcus aureus shows that the maximum inhibition was seen in Ethyl acetate extract of
Tribulus terrestris. The moderate inhibition was seen in Ethanol extract of Tribulus terrestris.
The minimum inhibition was seen in the Acetone, Chloroform extract Tribulus terrestris. No
inhibition of Tribulus terrestris was seen in the Aqueous and Petroleum ether extract of Tribu-
lus terrestris. a) P.E-Petroleum ether, (b) AQ-Aqueous, (c) E.A-Ethyl acetate, (d) M-Methanol,
(e) E-Ethanol , (f) CHL-Chloroform, (g) AC-Acetone.
FIGURE 5. MIC of different strains of Petroleum ether extracts of Tribulus terrestris
by broth dilution method
Uma Maheshwari, Rajendran and Vijayalakshmi
BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS PHARMACOLOGICAL ACTIVITY OF DIFFERENT SOLVENT EXTRACTS OF
TRIBULUS TERRESTRIS
757
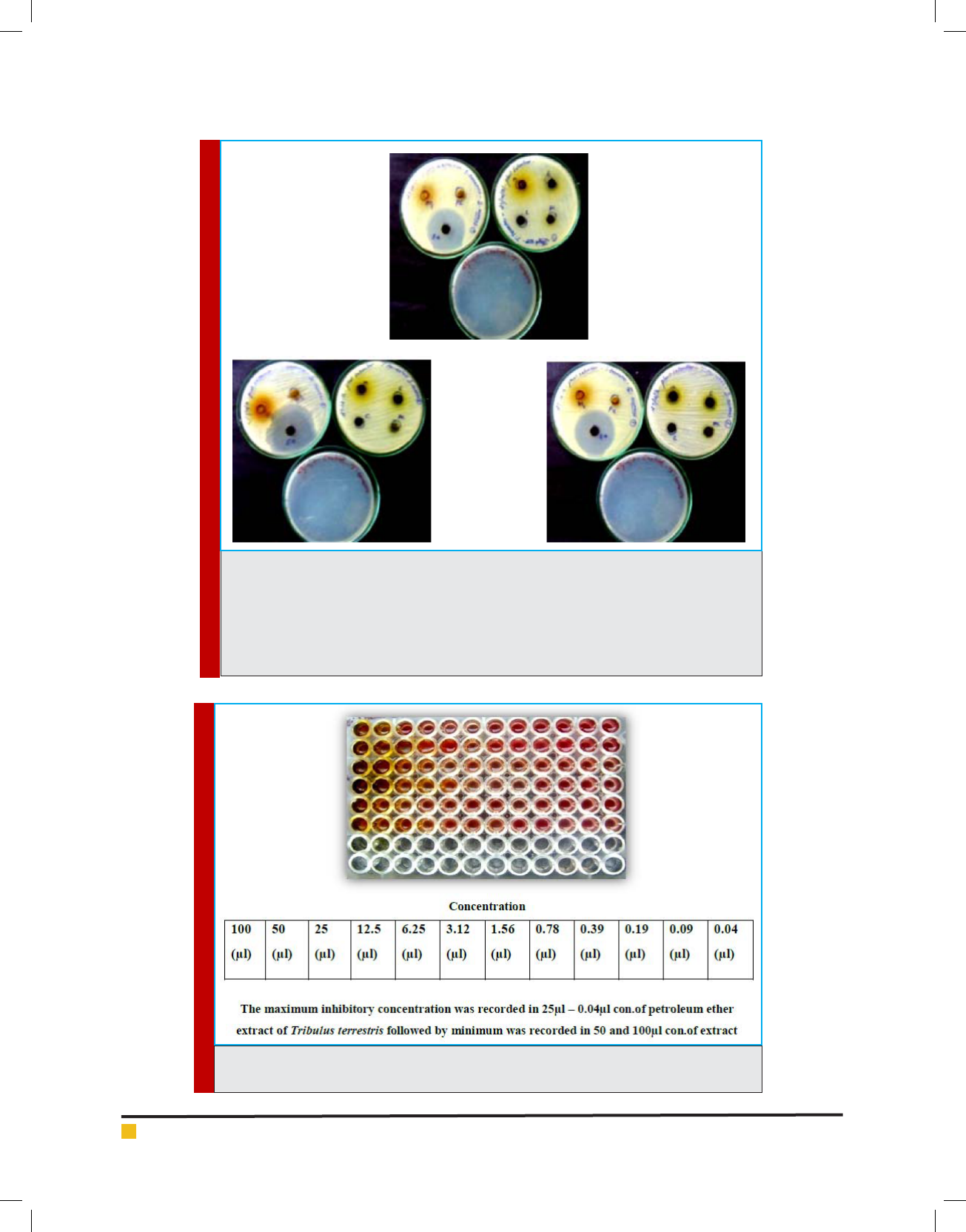
FIGURE 6. MIC of different strains of Aqueous extracts of Tribulus terrestris by broth dilution
method
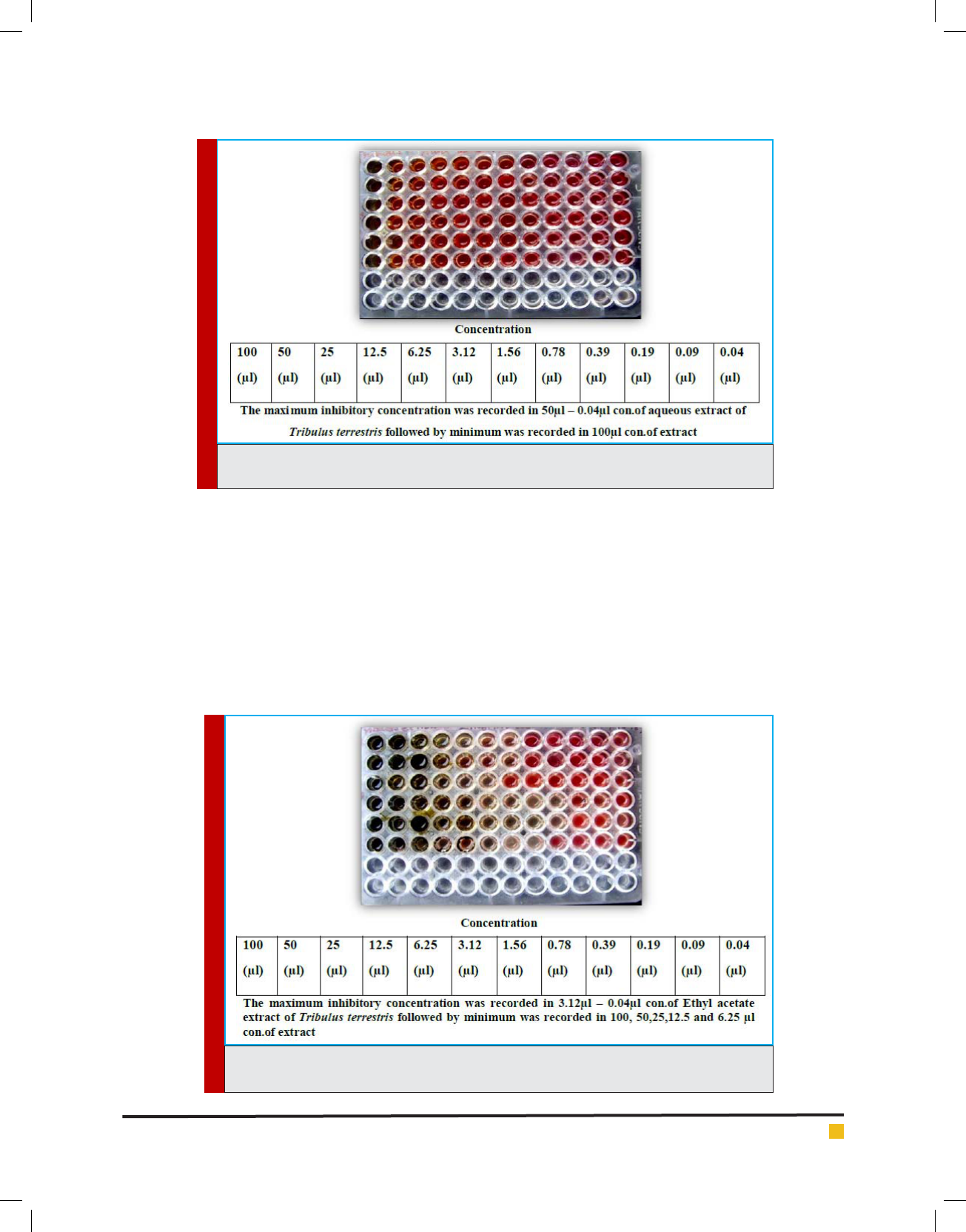
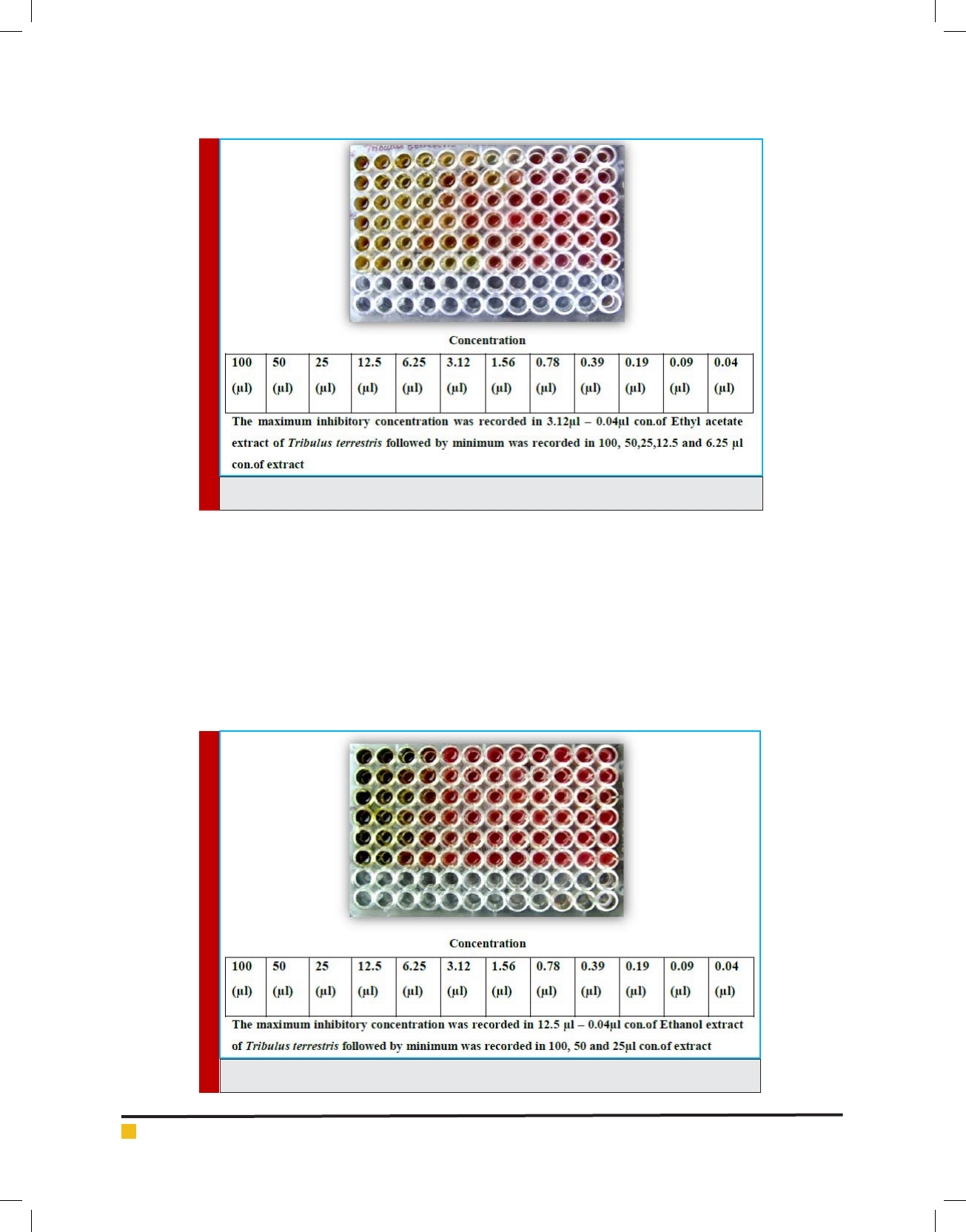
FIGURE 7. MIC of different strains of Ethyl acetate of Tribulus terrestris by broth dilution
method
gram of STR-VAN-AMX-NEO-CHL-AMP-P-CIP; STR-
VAN-AMX-NEO-AMP-P-GEN-CIP and STR-VAN-CHL-
AMP-P-GEN-AK-CIP.
Totally 10 antibiotics were used to know the resist-
ant pattern, among, 10 antibiogram were recorded. Ten
antibiotics were showing more than 20% resistant to the
isolates. All isolates (100%) were resistant of Ampici-
lin and Penicillin, while Vancomycin showed resistance
(90%), Cipro oxacin (60%), Streptomycin and Amoxyil-
lin (50%), Neomycin (40%), Chlorompenical and Gen-
tamycin (30%) followed by Amikacin (20%). All the
Staphylococcus aureus isolates showed multiple antibi-
otic resistances. Such that one isolate resisted four, six
and seven types of antibiotics, two isolates resisted 3
types of antibiotics, three isolates resisted eight antibi-
otics. The multiple antibiotic resistances (MAR) index
was calculated according to the MAR index formula.
The Maximum MAR index 0.8 was shown by MTUM08,
MTUM06, MTUM07 and minimum MAR index 0.3 was
shown by MBUM01 and MBUM08
Uma Maheshwari, Rajendran and Vijayalakshmi
758 PHARMACOLOGICAL ACTIVITY OF DIFFERENT SOLVENT EXTRACTS OF
TRIBULUS TERRESTRIS
BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS
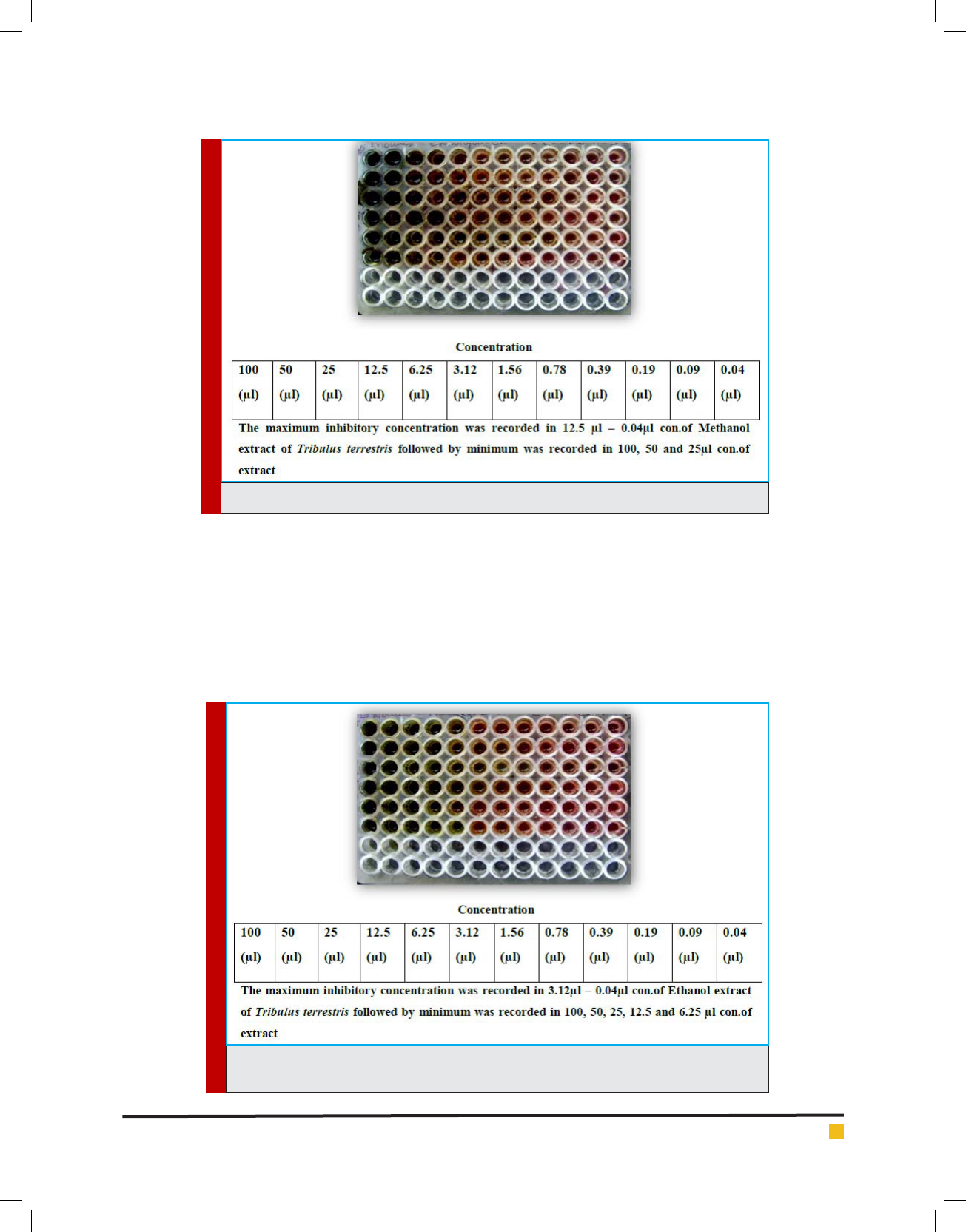
FIGURE 8. MIC of different strains of Methanol of Tribulus terrestris by broth dilution method
FIGURE 9. MIC of different strains of Ethanol of Tribulus terrestris by broth dilution method
Based upon the MDR (Multiple Drug Resistance),
seven strains of Staphylococcus aureus were selected
for further studies. Finally, the strains were tested with
puri ed leaf extract of various solvents using Tribulus
for antimicrobial activity and showed maximum inhi-
bition in Ethyl acetate, moderate inhibition in Ethanol,
minimum inhibition was recorded in Acetone, Chloro-
form, Methanol and no inhibition observed in Aqueous
and Petroleum ether solvents. Minimum inhibitory con-
centrations were performed to determine the minimum
concentration of antibiotics, which is effective on the
wound pathogens were also recorded and compared to
currently used antibiotics, the plant extract of Tribulus
terrestris shows effective results (Fig. 5 to g. 11).
Post-operative wound infection still remains one of
the most important causes of morbidity and is one of
the most common nosocomial infection (Suljagic et al.,
2010) in surgically treated patients. In the present study,
an attempt has been made to know the predominant
pathogen Staphylococcus aureus is the major respon-
Uma Maheshwari, Rajendran and Vijayalakshmi
BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS PHARMACOLOGICAL ACTIVITY OF DIFFERENT SOLVENT EXTRACTS OF
TRIBULUS TERRESTRIS
759
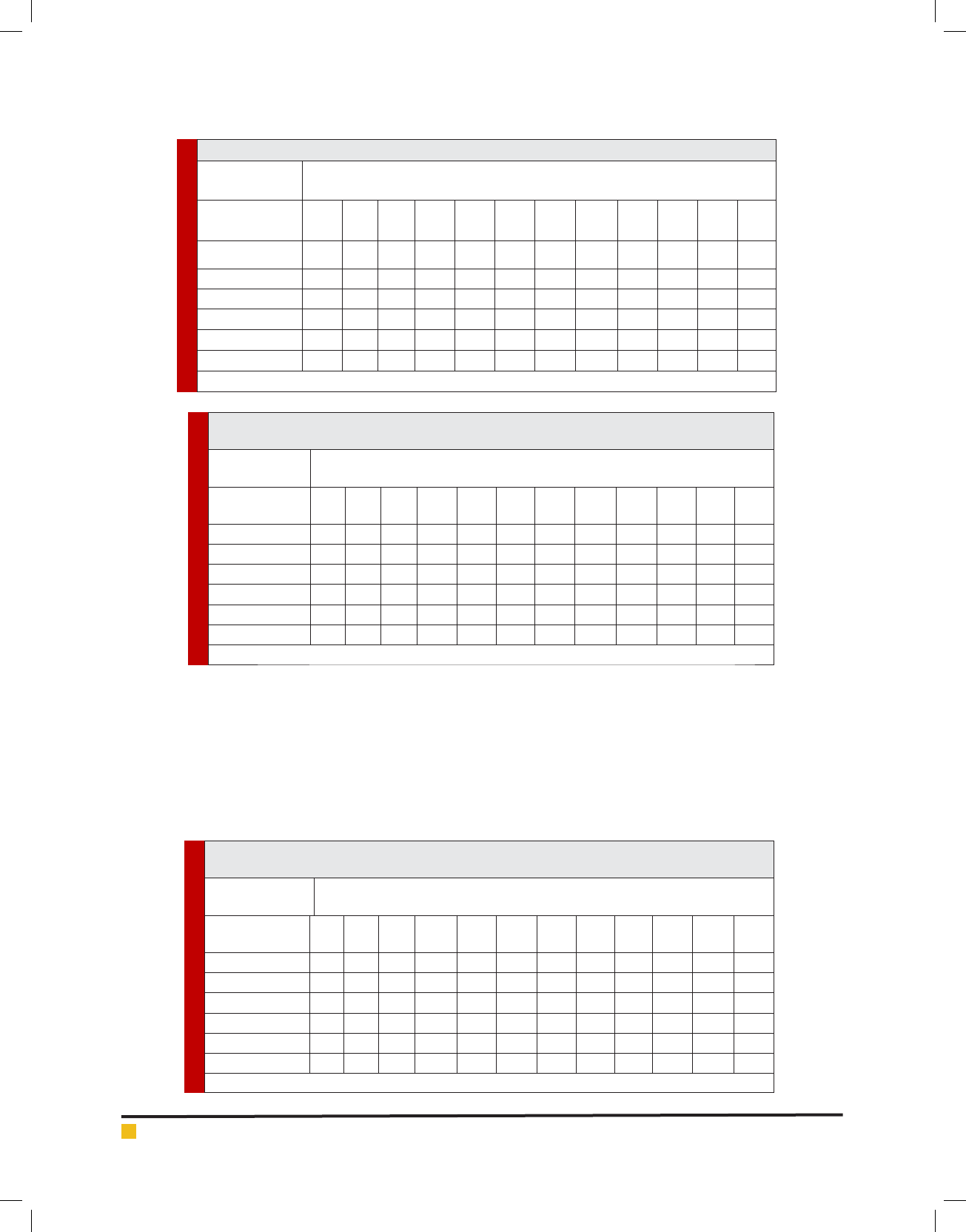
FIGURE 10. MIC of different strains of Methonol of Tribulus terrestris by broth dilution method
FIGURE 11. MIC of different strains of Chloroform of Tribulus terrestris by broth dilution
method
sible for surgical site infections and their antibacterial
susceptibility pattern. The rate of surgical site infection
varies greatly worldwide and from hospital to hospital.
The rate of SSI varies from 2.5% to 41.9% as per differ-
ent studies. The incidence of SSI in the present study is
2.69% even though high, is in agreement with the vari-
ous studies (Reichman and Greenberg, 2009).
Wound infections in ict clinical and societal conse-
quences on the patients, but its bacteriological charac-
teristic varies with different factors. Therefore, effective
treatment and management of wound infections in hos-
pital and community setting will require detailed epide-
miological knowledge of the infecting bacterial patho-
gens and their antibiogram peculiar to the environment.
Uma Maheshwari, Rajendran and Vijayalakshmi
760 PHARMACOLOGICAL ACTIVITY OF DIFFERENT SOLVENT EXTRACTS OF
TRIBULUS TERRESTRIS
BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS
Table 2. MIC of different strains of Aqueous extract of Tribulus terrestris by broth dilution method
Test
microorganism
Plant Extract (Aqueous)
Concentration (500mg/ml)
100
(μl)
50
(μl)
25
(μl)
12.5
(μl)
6.25
(μl)
3.12
(μl)
1.56
(μl)
0.78
(μl)
0.39
(μl)
0.19
(μl)
0.09
(μl)
0.04
(μl)
MTUM02 - + + +++++ ++++
MTUM03 - + + +++++ ++++
MTUM05 - + + +++++ ++++
MTUM06 - + + +++++ ++++
MTUM07 - + + +++++ ++++
MTUM09 - + + +++++ ++++
(-) indicates absence of growth and (+) indicates presence of growth of microorganisms
Table 3. MIC of different strains of Ethyl acetate extract of Tribulus terrestris by broth dilution
method
Test
microorganism
Plant Extract (Ethyl acetate)
Concentration (500mg/ml)
100
(μl)
50
(μI)
25
(μI)
12.5
(μI)
6.25
(μI)
3.12
(μI)
1.56
(μI)
0.78
(μI)
0.39
(μI)
0.19
(μI)
0.09
(μI)
0.04
(μI)
MTUM02 - - - - - - - + + + + +
MTUM03 - - - - - - - + + + + +
MTUM05 - - - - - - + + + + + +
MTUM06 - - - - - - - - - + + +
MTUM07 - - - - - - - - - + + +
MTUM09 - - - - - - - - + + + +
(-) indicates absence of growth and (+) indicates presence of growth of microorganisms
Table 4. MIC of different strains of Methanol extract of Tribulus terrestris by broth dilution
method
Test
microorganism
Plant Extract (Methanol)
Concentration (500mg/ml)
100
(μl)
50
(μI)
25
(μI)
12.5
(μI)
6.25
(μI)
3.12
(μI)
1.56
(μI)
0.78
(μI)
0.39
(μI)
0.19
(μI)
0.09
(μI)
0.04
(μI)
MTUM02 - - - - + + + + + + + +
MTUM03 - - - - - - - + + + + +
MTUM05 - - - - + + + + + + + +
MTUM06 - - - + + + + + + + + +
MTUM07 - - - - - + + + + + + +
MTUM09 - - - - - - + + + + + +
(-) indicates absence of growth and (+) indicates presence of growth Microorganisms
Based on this information, the author (Bularafa Moham-
med Yasidi et al., 2015) examined the prevalence and
antibiogram of bacterial pathogens isolated from wound
infection cases seen at the hospital over the study period.
A total of 392 wound swabs/ and pus of different types
of wound infections from different anatomical sites and
associated clinical conditions were analyzed by standard
bacteriological methods. Of the 392 clinical specimens
analyzed, 301(76.8%) yielded the majority of pathogens
were recovered from septic wound infections. Overall, 7
different bacterial pathogens were identi ed.
The authors state that among different kind of micro-
organisms the major pathogen Staphylococcus aureus
was isolated and used for antimicrobial testing. The
Uma Maheshwari, Rajendran and Vijayalakshmi
BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS PHARMACOLOGICAL ACTIVITY OF DIFFERENT SOLVENT EXTRACTS OF
TRIBULUS TERRESTRIS
761
Table 5. MIC of different strains of Ethanol extract of Tribulus terrestris by broth dilution method
Test
microorganism
Plant Extract (Ethanol)
Concentration (500mg/ml)
100
(μl)
50
(μI)
25
(μI)
12.5
(μI)
6.25
(μI)
3.12
(μI)
1.56
(μI)
0.78
(μI)
0.39
(μI)
0.19
(μI)
0.09
(μI)
0.04
(μI)
MTUM02 - - - + + + + + + + + +
MTUM03 - - + + + + + + + + + +
MTUM05 - - - + + + + + + + + +
MTUM06 - - + + + + + + + + + +
MTUM07 - - - + + + + + + + + +
MTUM09 - - + + + + + + + + + +
(-) indicates absence of growth and (+) indicates presence of growth of microorganisms
Table 6. MIC of different strains of Chloroform extract of Tribulus terrestris by broth dilution
method
Test
microorganism
Plant Extract (Chloroform)
Concentration (500mg/ml)
100
(μl)
50
(μI)
25
(μI)
12.5
(μI)
6.25
(μI)
3.12
(μI)
1.56
(μI)
0.78
(μI)
0.39
(μI)
0.19
(μI)
0.09
(μI)
0.04
(μI)
MTUM02 - - + + + + + + + + + +
MTUM03 - - + + + + + + + + + +
MTUM05 - - + + + + + + + + + +
MTUM06 - + + + + + + + + + + +
MTUM07 - - - + + + + + + + + +
MTUM09 - - - - + + + + + + + +
(-) indicates absence of growth and (+) indicates presence of growth of microorganisms
Table 7. MIC of different strains of Acetone extract of Tribulus terrestris by broth dilution
method
Test
Microorganim
Plant Extract (Acetone)
Concentration (500mg/ml)
100
(μl)
50
(μI)
25
(μI)
12.5
(μI)
6.25
(μI)
3.12
(μI)
1.56
(μI)
0.78
(μI)
0.39
(μI)
0.19
(μI)
0.09
(μI)
0.04
(μI)
MTUM02 - - - - - + + + ++++
MTUM03 - - - - + + + + ++++
MTUM05 - - - - - - - - ++++
MTUM06 - - - - - + + + ++++
MTUM07 - - - - + + + + ++++
MTUM09 - - - - - + + + ++++
(-) indicates absence of growth and (+) indicates presence of growth of microorganisms
bacterial pathogens demonstrated high resistance to
Ampicillin (78%), Amoxicillin (66%), and Cotrimoxa-
zole (78%), in contrast to the high sensitivity pattern
observed with O oxacin 83%, Nor oxacin 71%, Cip-
ro oxacin 78%, Erythromycin 72%, Chloramphenicol
62%, Gentamicin 58% and Ceftazidime 60%. But in
this present study demonstrates that all Staphylococcus
aureus isolated from pus samples of infectious patients.
The high resistance was observed in Cipro oxacin (60%),
Amoxicillin (50%) in contrast to high sensitivity pat-
tern observed with Chloramphenicol (30%), Gentamicin
(30%), Nor oxacin (40%).
Jain et al. (2014) states that in their study all Staphy-
lococci were susceptible to Vancomycin and Teicoplanin.
Uma Maheshwari, Rajendran and Vijayalakshmi
762 PHARMACOLOGICAL ACTIVITY OF DIFFERENT SOLVENT EXTRACTS OF
TRIBULUS TERRESTRIS
BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS
In contrast, the Vancomycin remains the rst choice of
treatment for MRSA and to preserve its value, its use
should be limited to those cases where there are clear
indications. But in this present study dissimilar results
were obtained by predominant pathogen Staphylococ-
cus aureus indicates resistant to Vancomycin, it proofs
that the emerging of drug resistant ability of Staph to be
currently initiated.
The result of this present study indicated that bacte-
rial isolates demonstrated high sensitivity to Chloram-
phenicol being about 70% sensitive, whereas resistant
to -lactam antibiotic namely Penicillin (100%) was
very high. These results are contrary to that obtained for
anaerobes isolated from oro-facial infections in earlier
study which reported good activities of the later agents
against the anaerobes (Nicholes, 2004).
Recurrently, the medicinal plants are the oldest form
of healthcare known to mankind. From the ancient time
people are using different herbs or plants as the rem-
edy forvarious diseases. But now a day’s people have
become dependent on synthetic medicines which have
many side effects. So to reduce the side effects we can
use medicinal plants for the treatment of common dis-
eases rather than using drugs.
Phan et al. (2001) nd out the secondary metabolites
are synthesized by the plant as part of the defence sys-
tem of the plant. The plant contains chebulinc acid, tan-
nic acid, gallic acid, resin, anthroquinone and sennoside.
It also contains glycosides, sugar, terpenoids, steroids,
phosphoric acid and these compounds were proven to
exhibit antibacterial, antifungal, antiviral and anticar-
cinogenic (Neamsuvan et al., 2012). Hence, the present
study to logically select a leaf part of bio-medically
active Tribulus plant to exhibit a broad antimicrobial
activity against wound pathogen Staphylococcus aureus.
Ali et al., (2001) con rmed that their study the Tribulus
terrestris had no detectable antibacterial activity against
any of the infectious disease causing reference bacte-
ria. For this reason, in this present study choose a plant
material of Tribulus to check the vital activity against
infectious disease that proved the Indian leaf of T. ter-
restris were active against clinically dominant pathogen
S.aureus isolated from post-operative wound infection.
Recurrently, the plant extract is highly sensitive when
compared to the standard antibiotic. These data indi-
cate that Gram-positive bacteria are the most sensitive
strains for the different extracts, which exhibited their
main antibacterial activity on Gram-negative bacte-
ria (Bakri and Douglas 2005). Our results are in good
agreement with previous works (Al Maofari et al., 2013)
showing a weaker activity of essential oil of Anis and
Salvia tomentosa and also Nair and Chanda, a (2008)
also reported Gram positive were more sensitive. Etha-
nol extract showed more effect than aqueous extract in
inhibiting the growth of the bacterial strains (Nair and
Chanda, b 2007; Firas et al., 2008). The growth of the
Gram positive strains was found more inhibition than
Gram negative. In this present study, similar results was
observed the antimicrobial activity of 7 different solvent
plant extract was tested against S.aureus. The maximum
antibacterial activity was seen in Ethyl acetate extract
(100μl) of Tribulus terrestris. Intermediate antibacterial
activity was seen in Ethanol extract (100μl) of Tribulus
terrestris (Fig. 3).
CONCLUSION
The present study revealed that the post operative wound
infection is one of the most common chronic infectious
diseases of human is also a serious problem among wound
of post-operative patients caused by predominant patho-
gen Staphylococcus aureus. Therefore, effective treatment
and management of wound infections in hospital and
community setting will require detailed knowledge of the
infecting bacterial pathogens and their antibiogram pecu-
liar to the environment for drug selection. Resistant bac-
teria which are human pathogens may cause the disease,
they may still be dangerous because they can transfer
their antibiotic resistance genes to other organism. Anti-
microbial resistances of bacterial pathogens are a major
problem for the treatment of animal and human patients
with bacterial diseases. There is an alarming increase
of infections caused by antibiotic resistant bacteria to
urgently need of antimicrobial compound to treat a path-
ogenic organism. Recurrently the plants have been one of
the important sources of medicine since the beginning of
human civilization. There is a growing demand for plant
based medicines to activity against several infectious
pathogens. Hence the current study concluded that the
different solvent extract of Tribulus plant has different
mode of action to eradicate the wound pathogen around
the surgical site. The plant extracts can also be exploited
in designing the wound care products.
REFERENCES
Al Maofari A, S. EL Hajjaji, A. Debbab, S.Zaydoun, B. Ouaki, R.
Charof, Z. Mennane, Hakiki A and Mosaddak M (2013). Chemi-
cal composition and antibacterial properties of essential oils
of Pimpinella anisum L. growing in morocco and yemen. Sci-
enti c Study & Research Chemistry & Chemical Engineering,
Biotechnology, Food Industry. Vol. 14, Issuev1, 011 – 016.
Al-Bayati F.A, and Al-Mola H.F. (2008) Antibacterial and anti-
fungal activities of different parts of Tribulus terrestris grow-
ing in Iraq. J. Zhej.Univ Sci. Vol. 9, Issue 2, 154– 159.
Anaya D.A and Dellinger E.P (2006).Challenges in the preven-
tion of surgical site infections.Infections in Medicine. Vol 23,
Issue 3, 120-126.
Uma Maheshwari, Rajendran and Vijayalakshmi
BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS PHARMACOLOGICAL ACTIVITY OF DIFFERENT SOLVENT EXTRACTS OF
TRIBULUS TERRESTRIS
763
Awadh-Ali NA, W.D. Julich, Kusnick C and Lindequist U
(2001). Screening of Yemeni medicinal plants for antibacterial
and cytotoxic activities. J Ethno pharmacol. Vol. 74, Issue 2,
173–179.
Ayliffe G.A.J, A.P. Fraise, Geddes A.M. and Mitchell K (2000).
Control of Hospital Infection: A Practical Handbook; 4th edn.
London: Arnold.
Bakri IM and Douglas CWI (2005). Inhibitory effect of garlic
extract on oral bacteria. Arch Oral Biol. Vol. 50, 645–651.
Bourke CA, G.R Stevens, et al. (1992). Locomotor effects in
sheep of alkaloids identi ed in Australian Tribulus terrestris.
Aust. Vet. J. Vol. 69, 163-165.
Church D, S. Elsayed, O. Reid, Winston B and Lindsay R (2006).
Burn Wound Infections. Clin. Microbiol. Rev. Vol. 19, Issue 2,
403–434.
Ergin C and Mutlu G (1999). Clinical Distribution and Antibi-
otic Resistance of Pseudomonas species. Eastern J. Med. Vol. 4,
Issue 2, 65-69.
Firas A, Al-Bayati and Hassan F. Al-Mola (2008). Antibacterial
and antifungal activities of different parts of Tribulus terrestris
L. growing in Iraq. J. Zhejiang. Univ. Sci., B. Vol. 9, Issue 2,
154-159.
Jain A., S. Bhatawadekar and M. Modak (2014). Bacteriologi-
cal pro le of surgical site infection from a tertiary care hos-
pital, from western India. Indian Journal of Applied Research.
Vol. 4, Issue (1), 397-400.
Lewis K and Ausubel F.M (2006). Prospects for plant-derived
anti-bacterials. Nat. Biotechnol. Vol. 24, Issue 12, 1504-1507.
Mohammed B., Yasidi H, Denue Ballah Akawu (2015). Retro-
spective analysis of bacterial pathogens isolated from wound
infections at a Tertiary Hospital in Nguru, Yobe State Nigeria
. American Journal of Biomedical and Life Sciences. Vol. 3,
Issue 1, 1-6.
Nair, Ratish and Chanda Sumitra, V. (2007a). Antibacterial
activities of some medicinal plants of the Western Region of
India. Turk. J. Bot. Vol. 31, 231-236.
Nair, Ratish and Chanda Sumitra, V. (2007b). In vitro antimi-
crobial activiy of Psidium guajava leaf extracts against clini-
cally important pathogenic microbial strains. Braz. J. Micro-
biol. Vol. 38, 452-458.
Nascimento G.G.F, J. Locatelli, Freitas P.C and Silva G.L (2000).
Antibacterial activity of plant extracts and phytochemicals on
anbiotic resistant bacteria. Braz. J. Microbiol. Vol. 31, 247-256.
Naz R, Hafsa Ayub, Sajid Nawaz , Zia U Islam , Tayyaba Yasmin,
Asghari Bano, Abdul Wakee , Saqib Zia and Thomas H Roberts
(2017). Antimicrobial activity, toxicity and anti in ammatory
potential of methanolic extracts of four ethno medicinal plant
species from Punjab, Pakistan. BMC Complementary and Alter-
native Medicine. Vol. 17, Issue 302, 1-13.
Neamsuvan O, P. Singdam, Yingcharoen K and Sengnon N
(2012). A survey of medicinal plants in mangrove and beach
forests from sating Phra Peninsula, Songkhla Province, Thai-
land. J. Med. Plants Res. Vol. 6, Issue (12), 2421-2437.
Nichols RL, (2004). Current Strategies for Prevention of Surgi-
cal Site Infections.Curr Infect Dis Rep. Vol. 6, Issue 6, 426–434.
Percevil S and Bowler P (2004). Understanding the effects of
bacterial communities and bio lms on wound healing. Avail-
able from: URL: ttp://www.worldwidewounds.com
Phan TT, L. Wang, P. See, R.J. Grayer, Chan SY and Lee ST (2001).
Phenolic compounds of Chromolaena odorata protect cultured
skin cells from oxidative damage: implication for cutaneous
wound healing. Biol. Pharm. Bull. Vol. 24, Issue 12, 1373-1379.
Reichman DE and Greenberg JA (2009). Reducing Surgical Site
Infections: A Review. Rev Obstet Gynecol. Vol. 2, 212-221.
Sengul M, H. Yildiz, et al. (2009). Total phenolic content, anti-
oxidant and antimicrobial activities of some medicinal plants.
Pak. J. Pharm. Sci. Vol. 22, Issue 1, 102-106.
Sibanda T and Okoh A.I (2007). The Challenges of overcom-
ing antibiotic resistance: plant extracts as potential sources of
antimicrobial and resistance modifying agents. Afr. J. Biotech-
nol. Vol. 6, Issue 25, 2886-2896.
Sudharameshwari K and Radhika J (2007). Antibacterial
Screening of Aegle marmelos, Lawsonia inermis and Albizzia
libbeck. AJTCAM. Vol. 4, Issue 2, 199-204.
Suljagic V, M. Jevtic, Djordjevic B and Jovelic A (2010). Surgi-
cal site infections in a tertiary health care center: Prospective
cohort study. Surg Today. Vol. 40, 763-71.
Tahir MS, (1995). Surgical wounds and prevention of
infection in the hospital. The Professional. Vol. 2, 173-81.
Tredget E. E, H. A. Shankowsky, R. Rennie, Burrell R. E and
Logsetty S (2004). Pseudomonas infections in the thermally
injured patient. Burns, Vol. 30, 3–26.
Wang B., Ma L and Liu T (1990) 406 cases of angina pectoris
in coronary heart disease treated with saponin of Tribulus ter-
restris. Chung Hsi. J. Chieh Ho Tsa Chih. Vol. 10, Issue 2, 85–87
(in Chinese).