
Dental
Communication
Biosci. Biotech. Res. Comm. 10(4): 728-731 (2017)
Effect of vibration on pain during Injection of local
anesthesia: A split-mouth randomized clinical trial
Gholam Hossain Ramezani
1
, Mohammad Tajjedin
2
, Nasser Valaee
3
and Hooman Ebrahimi
4
*
1
Department of Pediatric Dentistry, Dental Branch, Islamic Azad University, Tehran, Iran
2
Specialist in Pediatric Dentistry
3
Epidemiologist, Dental Branch, Islamic Azad University, Tehran, Iran
4
Department of Oral Medicine, Dental Branch, Islamic Azad University, Tehran, Iran
ABSTRACT
Vibration can reduce pain. This study was conducted to use this effect while injecting dental anesthesia. This split-
mouth randomized clinical trial was performed on 40 injection sites from 20 patients. In the experimental sides, the
turned-on device would be positioned in contact with the injection area for 5 seconds; then the anesthesia would be
administered, while the device was in place; nally, the device would remain in place for 5 seconds after removing
the needle. In the control sides, the device would be placed on the mucosa in a similar fashion but turned off. Imme-
diately after removing the tip of Dental Vibe, patients were asked to rate their pain using Wong Baker method. Pain
scores were compared statistically. Average pain levels in the experimental and control sides were 1.95 ± 1.57 (95%
CI: 1.22 to 2.68) and 0.65 ± 0.81 (95% CI: 0.27 to 1.03), respectively. Their difference was signi cant according to
Wilcoxon test (P < 0.001). Age (P = 0.670), injection type (P = 0.175), and sex (P = 0.160) did not affect the response
to the Dental Vibe signi cantly, according to chi-square test. Dental Vibe is a useful and effective device in reducing
pain while injecting local anesthesia.
728
ARTICLE INFORMATION:
*Corresponding Author:
Received 10
th
Oct, 2017
Accepted after revision 29
th
Dec, 2017
BBRC Print ISSN: 0974-6455
Online ISSN: 2321-4007 CODEN: USA BBRCBA
Thomson Reuters ISI ESC and Crossref Indexed Journal
NAAS Journal Score 2017: 4.31 Cosmos IF: 4.006
© A Society of Science and Nature Publication, 2017. All rights
reserved.
Online Contents Available at:
http//www.bbrc.in/
DOI: 10.21786/bbrc/10.4/18
INTRODUCTION
Most common anxiety provoking and fearful experi-
ence for children in dental operatory is administration
of local anesthesia. Pain management when injecting
local anesthesia (LA) is one of the most critical stages in
performing dental treatments. Since painful dental treat-
ments typically begin with LA, pain control at this step
is essential. Pain is a deterrent of dental treatment and
many patients avoid or cancel their treatments because
of this factor because of being afraid of pain, which is
usually caused by previous painful experiences during
dental procedures. Therefore, reducing dental pain is
important and researchers have been seeking methods
Gholam Hossain Ramezani et al.
to reduce dental pain, including pain of injecting local
anesthesia Milgrom et al., 1997, Yenisey 2009 Bonjar
2011, Ungor et al 2014, Rakshan and Rakshan 2015,
Agarwal et al 2017).
Mechanisms for pain due to local anesthesia are
mainly quick expansion of the tissues and their tension,
followed by mechanical trauma by the needle puncture
to the region of the injection. Various methods have been
proposed to reduce or prevent pain while administer-
ing local anesthesia, including the application of topical
anesthetics, suggestion, slow injection , transcutaneous
electrical nerve stimulation (TENS) computer-assisted
local anesthesia (such as Wand), and vibration (Hersh et
al. 1996 Peretz et al., 2004 and Primosch 2003).
According to the “gate control” theory, providing
non-noxious stimuli might interrupt nociceptive signals
reduce the perceived pain . Thus, it is hypothesized that
stimulating larger-diameter A-beta bers with vibration
and pressure might reduce pain sensation (Saijo et al.,
2005 Nanitsos et al., 2009 and Rakshan and Rakshan
2015).
The Dental Vibe device (BING Innovations, Florida,
USA) is a new portable system that transmits pressure-
rotational pulses to the injection area, without any
need to changing the routine protocols of injection. We
hypothesized that vibration concurrent with injection
might decrease perceived pain in children.
MATERIALS AND METHODS
This split-mouth randomized clinical trial was per-
formed on 40 injection sites from 20 patients (13 boys
and 7 girls, with an average age of 5.7 years old) referred
to the Department of Pediatric Dentistry at Islamic Azad
University during 2014-2015. The protocol ethics were
approved by the Ethical Committee of the university,
and informed consents were taken from patients’ par-
ents. Inclusion criteria were being systemically healthy,
being aged between 5 and 7 years old, a cooperation
level of 3 or 4 (according to Frankel scale) determined
by a pediatric dentist, ability to determine pain levels
according to Wong Baker scale (8thesis), and clinical
need for bilateral local anesthetic injection in the man-
dible or maxilla.
Randomization, Local anesthesia administration, and
Pain evaluation
Randomization was performed by picking out a card
from a box, for each patient. Patients with “vibration
on” cards would receive the injection together with the
DentalVibe application while the device was on. They
would receive the second injection on the contralateral
side, with the vibration off. The patients with “vibra-
tion off” cards would rst receive the placebo (the device
touch without vibration) rst, and the treatment in the
second session.
In the experimental sides, the turned-on device would
be positioned in contact with the injection area for 5 sec-
onds; then the anesthesia would be administered, while
the device was in place; nally, the device would remain
in place for 5 seconds after removing the needle. In the
control sides, the device would be placed on the mucosa
in a similar fashion but turned off. The inferior alveo-
lar nerve (IAN) blocks were administered using a carpul
of 2% lidocaine and 1:80000 epinephrine (Darupakhsh,
Tehran, Iran). The in ltration blocks were administered
for the maxilla, using a carpul of the same anesthetic
solution. Of the 40 injections, 22 were IAN blocks while
18 were maxillary in ltration injections.
Immediately after removing the tip of Dental Vibe,
patients were asked to rate their pain using Wong Baker
method. All injections were performed by the same per-
son (a resident of pediatric dentistry).After data col-
lection, the treatment would be started in its routine
fashion; the patient would receive as many carpules as
needed/wanted after the data collection.
After summarizing the descriptive statistics and con-
dence intervals (CI), Wilcoxon test and chi-square tests
used to compare control and treatment groups.
RESULTS AND DISCUSSION
Of the 20 participants, 65% reported lower pain levels
when using the device; 25 % rated the pain on both sides
similarly; 10% reported greater pain levels on the con-
trol sides. Average pain levels in the experimental and
control sides were 1.95 ± 1.57 (95% CI: 1.22 to 2.68) and
0.65 ± 0.81 (95% CI: 0.27 to 1.03), respectively. Their
difference was signi cant according to Wilcoxon test (P
< 0.001).
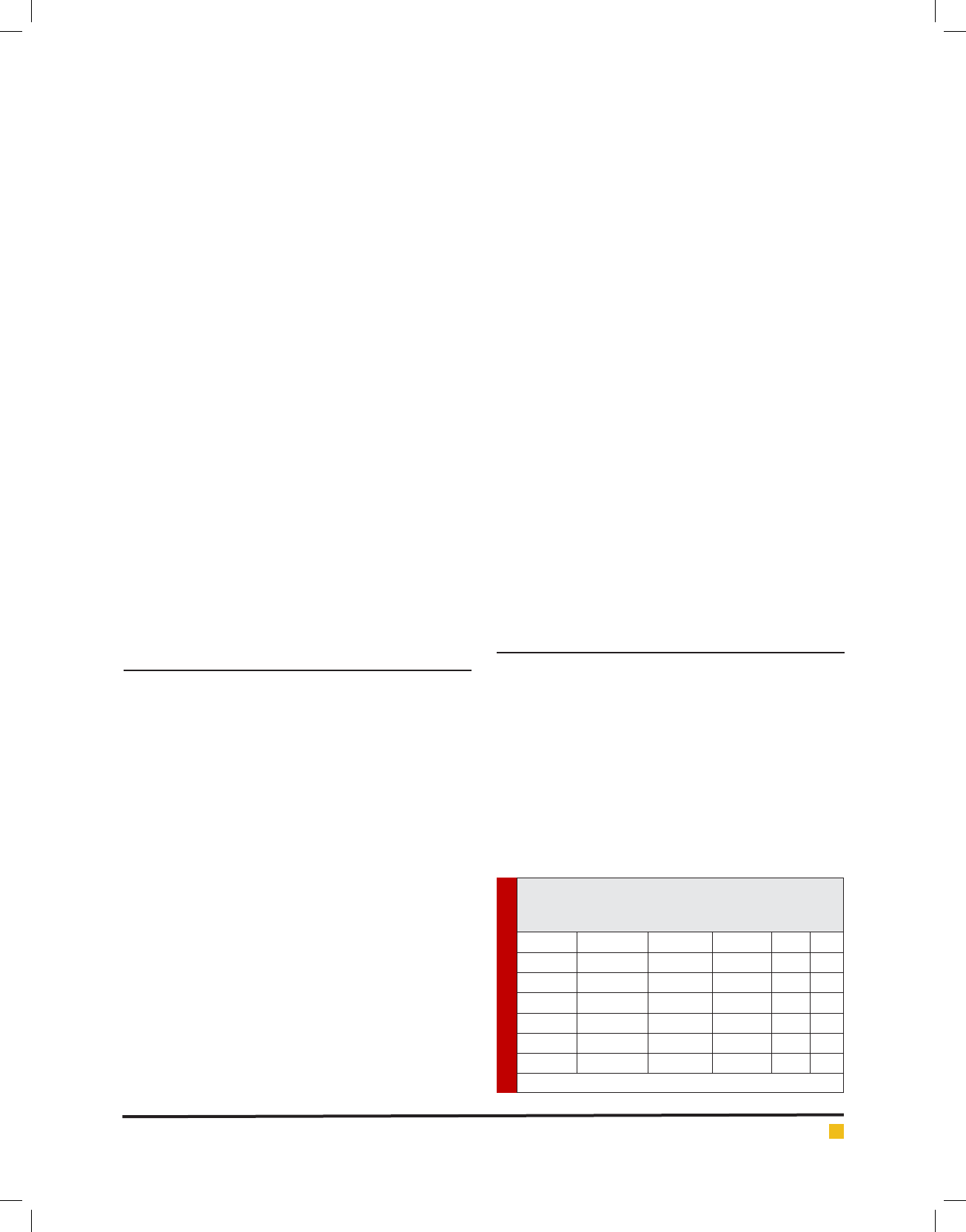
Age (P = 0.670), injection type (P = 0.175), and sex (P
= 0.160) did not affect the response to the Dental Vibe
signi cantly, according to chi-square test (Table 1).
Table 1. Results pertaining to experimental sides in
which the device was turned on (n = 20, control sides
are not used or shown).
Factor Painless Painful RR AR
Gender Boy 9 4 3.6 37
Girl 2 5
Age 5 yr old 5 6 2.4 21
> 5 yr old 3 6
Injection IAN block 8 3 3.5 30
In ltration 3 6
RR, relative risk; AR, attributable risk.
BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS EFFECT OF VIBRATION ON PAIN DURING INJECTION OF LOCAL ANESTHESIA 729
Gholam Hossain Ramezani et al.
Dental anxiety and fear are the most frequent reasons
preventing patients from dental visits, and are usually a
byproduct of local anesthesia injections. Hence, pain and
anxiety control during local anesthetic injections is of
signi cant clinical importance, (Ungor et al., 2014, Bon-
jar 2011 Berggren and Meynert 1984). Topical anesthet-
ics numb the injection surface and provide pain relief on
needle insertion, although there are other factors which
should be controlled (such as the clinician’s expertise
and amount, type, and dose of the injected medicine) for
a complete pain control. Although this method reduces
the pain during needle insertion, total elimination of
injection pain relies on causes like the amount, type,
and injection speed of anesthesia plus the experience
of clinician. In addition, local anesthetics have narrow
potential to enter deep into tissue. These might reduce
the discomfort during insertion of needle through the
surface however, they are not as effective when needle
passes through deeper layers, (Singh and Roberts 1994,
Meechan et al., 1998 Ungor et al 2014).
Hence, methods such as Wand and TENS are intro-
duced to solve this. TENS triggers large-diameter nerves
that are more sensitive to electrical stimuli than do
smaller-diameter nerves. The result is closure of central
gating mechanism to signals coming through nerves
with smaller diameters. The same mechanism of gate
control works for the vibration, which has impulses that
are transmitted very fast (75 meters per second) through
myelinated, thick, A-beta nerves. On the other hand,
sense of pain travels at a 2 meters per second speed
through unmyelinated and thin C bers, ( Ungor et al.,
2014, Nanitsos et al., 2009, Hall and Guyton 2015).
Simultaneous transmission of vibration signals
through thick A-beta bers versus pain signals through
C bers will make the sensory area of the brain release
inhibitory neurotransmitters these and inhibit the acti-
vation of projection neurons within dorsal horn of spi-
nal cord, leading to gate closure over pain stimuli. This
is the reason vibration is used to reduce pain during
many painful medical and dental procedures (Reed 2001,
Ungor et al., 2014). Another factor that contributes to
perception of pain is psychological status of person, par-
ticularly his or her fear or anxiety of pain. Dental fear
can prolong and intensify the pain (Peretz et al 2004).
Our results are similar to those of Ungor et al. (2014)
and Nanitsos et al. (2009) although in the latter study,
source of vibration was extra-oral, which might decrease
the ef cacy of expected gate control mechanism because
of pain and vibrated sites being distant. Another study
done by Saijo et al. (1995) examined injection pain
together with vibration of the site using VibraJect. They
could not nd signi cant differences between control
and treatment groups. Difference could be due to differ-
ent devices and methods.
CONCLUSION
This study has found DentalVibe as a useful and effec-
tive device in reducing pain while injecting local anes-
thesia.
REFERENCES
Agarwal N, Dhawan J, Kumar D, Anand A, Tangri K. 2017
Effectiveness of two aenesthetic agents used along with audio
visual aids in pediatric dental patients. Journal of clinical and
diagnostic research. 11(1):80
Berggren U, Meynert G. 1984 Dental fear and avoidance:
causes, symptoms, and consequences. The Journal of the
American Dental Association. 1984 08;109(2):247-51.
Bjerring P, Arendt-Nielsen L. 1990 Depth and duration of skin
analgesia to needle insertion after topical application of EMLA
cream. British Journal of Anaesthesia. 64(2):173-7.
Haas DA. 2002 An update on local anesthetics in dentistry.
Journal-Canadian Dental Association. 68(9):546-52.
Hall JE. Guyton JM 2015 A textbook of medical physiology:
Elsevier Health Sciences; 2015.
Hersh EV, Houpt MI, Cooper SA, Feldman RS, Wolff MS, Levin
LM. 1996 Analgesic Ef cacy And Safety Of An Intraoral Lido-
caine Patch. The Journal of the American Dental Association.
/11;127(11):1626-34.
Hutchins HS, Jr., Young FA, Lackland DT, Fishburne CP.
1997 The effectiveness of topical anesthesia and vibration
in alleviating the pain of oral injections. Anesth Prog. Sum-
mer;44(3):87-9.
Johnson J, Primosch RE.2003 In uence of site preparation
methods on the pain reported during palatal in ltration using
the Wand Local Anesthetic System. Am J Dent. 16(3):165-9.
Malamed SF. 2006 Local anesthetics: dentistry’s most impor-
tant drugs, clinical update CDA J. 2006;34(12):971-6.
Meechan JG, Gowans AJ, Welbury RR. 1998 The use of patient-
controlled transcutaneous electronic nerve stimulation (TENS)
to decrease the discomfort of regional anaesthesia in dentistry:
a randomised controlled clinical trial. Journal of Dentistry.
07;26(5-6):417-20.
Melzack R, Wall PD. 1965 Pain Mechanisms: A New Theory.
Science. 1965 11/19;150(3699):971-8.
Milgrom P, Coldwell SE, Getz T, Weinstein P, Ramsay DS. 1997
Four Dimensions Of Fear Of Dental Injections. The Journal of
the American Dental Association 06;128(6):756-62.
Nanitsos E, Vartuli R, Forte A, Dennison PJ, Peck CC. 2009 The
effect of vibration on pain during local anaesthesia injections.
Australian Dental Journal. 06;54(2):94-100.
Peretz B, Nazarian Y, Bimstein E. 2004 Dental anxiety in a stu-
dents’ paediatric dental clinic: children, parents and students.
International Journal of Paediatric Dentistry. /05;14(3):192-8.
Quarnstrom F, Libed EN. 1994 Electronic anesthesia versus
topical anesthesia for the control of injection pain. Quintes-
sence Int;25(10):713-6.
730 EFFECT OF VIBRATION ON PAIN DURING INJECTION OF LOCAL ANESTHESIA BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS

BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS EFFECT OF VIBRATION ON PAIN DURING INJECTION OF LOCAL ANESTHESIA 731
Gholam Hossain Ramezani et al.
Rakhshan H, Rakhshan V. 2015 Pain and discomfort perceived
during the initial stage of active xed orthodontic treatment.
The Saudi dental journal. 27(2):81-7.
Reed ML. 2001 Surgical Pearl: Mechanoanesthesia to reduce
the pain of local injections. Journal of the American Academy
of Dermatology. 2001 /04;44(4):671-2.
Saijo M, Ito E, Ichinohe T, Kaneko Y. 2005 Lack of Pain Reduc-
tion by a Vibrating Local Anesthetic Attachment: A Pilot
Study. Anesthesia Progress. 2005 06;52(2):62-4.
Shahidi Bonjar AH. 2011 Syringe micro vibrator (SMV) a new
device being introduced in dentistry to alleviate pain and anxi-
ety of intraoral injections, and a comparative study with a sim-
ilar device. Annals of Surgical Innovation and Research;5(1):1.
Sharma P, Czyz CN, Wulc AE. 2011 Investigating the Ef -
cacy of Vibration Anesthesia to Reduce Pain From Cos-
metic Botulinum Toxin Injections. Aesthetic Surgery Jour-
nal./10/14;31(8):966-71.
Singh P, Roberts M.1994 Skin permeability and local tissue
concentrations of nonsteroidal anti-in ammatory drugs after
topical application. Journal of Pharmacology and Experimen-
tal Therapeutics. 268(1):144-51.
Ungor C, Tosun E, Dayisoylu EH, Taskesen F, Senel FC. 2014
The effects of vibration on pain and anxiety during local anes-
thesia administration. JSM Dent. 2(1):1022.
Walton RE, Torabinejad M. Principles and practice of endo-
dontics. 1996.
Yenisey M. 2009 Comparison of the pain levels of com-
puter-controlled and conventional anesthesia techniques in
prosthodontic treatment. Journal of Applied Oral Science.
2009/10;17(5).