
Medical
Communication
Biosci. Biotech. Res. Comm. 10(4): 710-715 (2017)
Diabetic Predecessors: A factor leading to diabetes in
successors
Manju Dewan
Assistant Professor, Post Graduate Department of Zoology, DAV College, Sector 10, Chandigarh
ABSTRACT
Type 2 diabetes has several causes:genetics and lifestyle are the most important ones.A combination of these factors
can cause insulin resistance. Diabetes is a complex condition. Several factors must come together to develop type 2
diabetes. In the total population of 2048 subjects, 558 subjects had the positive family history of diabetes. Out of 558
subjects 12 (2.15%) subjects were found to have impaired glucose level, 12 (2.15%) subjects have already developed
diabetes and both have family history diabetes in rst degree relatives (Father, Mother, Father Mother both). In the
present study, 558 (27.3%) subjects have shown positive family history for diabetes.
KEY WORDS: TYPE 2 DIABETES, FAMILY HISTORY, FATHER, MOTHER
710
ARTICLE INFORMATION:
*Corresponding Author: manjudewan72@gmail.com
Received 12
th
Oct, 2017
Accepted after revision 19
th
Dec, 2017
BBRC Print ISSN: 0974-6455
Online ISSN: 2321-4007 CODEN: USA BBRCBA
Thomson Reuters ISI ESC and Crossref Indexed Journal
NAAS Journal Score 2017: 4.31 Cosmos IF: 4.006
© A Society of Science and Nature Publication, 2017. All rights
reserved.
Online Contents Available at:
http//www.bbrc.in/
DOI: 10.21786/bbrc/10.4/15
INTRODUCTION
Heredity plays an important role in determining the sus-
ceptibility to diabetes mellitus. Diabetes mellitus is mul-
tifactor in its etiology.A signi cantly greater frequency
of diabetes has been found in close blood relatives of
diabetic than in other population.Prevalence of over-
weight and obesityweremore in children with family his-
tory of diabetes and obesity.Environmental factors play
a major role in the development of diabetes. Environ-
mental risks factors known to in uence the development
of obesity and type 2 diabetes due to sedentary lifestyle,
wrong eating habits and stress. Other nutritional fac-
tors and toxins may also play a crucial role (Adeghate
et al, 2006). These environmental factors clearly play
a major role in the development of diabetes, but they
do not impact everyone in the same way (Omar 2013).
Family history of diabetes (FHD) and lifestyle are associ-
ated with type 2 diabetes (Yanyan et al, 2017). Nina et
al, 2016 also found that children had a strong family
history of cardiovascular disease and diabetes. The esti-
mated risk for the diagnosis of type 2 diabetes (T2DM)
increases approximately by 2-4 times, when father,
mother or both have this condition. Conversely, many
T2DM patients have family members with DM (Papaza-
ropoulou et al, 2017). The modern generalization of
Manju Dewan
Table 1. Prevalence of Family History of diabetes.
Father Mother
All Data 106 69.28 47 30.72 N.A.:1895 (92.53%)
FBG Categories
1. <110 102 70.83 42 29.17
2. 110-126 2 40.00 3 60.00
3. >=126 2 50.00 2 50.00 Chi^2=2.88(df:2)
C=0.14;
BMI Categories
1. <18.5 195 54.78 161 45.22
2. 18.5-22.9 69 52.67 62 47.33
3. 23.0-24.9 15 51.72 14 48.28
4. 25.0-29.9 15 45.45 18 54.55
5. >30.0 3 33.33 6 66.67 Chi^2=2.62(df:4)
C=0.07;
BMI Categories
1. <18.5 195 54.78 161 45.22
2. 18.5-22.9 69 52.67 62 47.33
3. 23.0-27.5 28 50.91 27 49.09
4. >27.5 5 31.25 11 68.75 Chi^2=3.58(df:3)
C=0.08;
Percentile Based
1.Under Wt. 76 55.88 60 44.12
2.Healthy
Wt.
186 53.14 164 46.86
3.At Risk 24 60.00 16 40.00
4.Over Wt. 11 34.38 21 65.62 Chi^2=5.69(df:3)
C=0.10;
W/H based (All)
1.Normal 255 52.80 228 47.20
2.Over Wt. 42 56.00 33 44.00 Chi^2=0.27(df:1)
C=0.02;
sedentary life and caloric abundance has created new
physiological conditions capable of changing the level
of expression of a number of genes involved in fuel
metabolism and body weight regulation.
MATERIALS AND METHODS
2048 children had undergone questionnaire and dietary
survey and health examination. Out of these, 1017 were
from urban population and 1031 from rural population
Children and adolescent aged 10-19 years were selected
randomly for questioning regarding the different aspects
of epidemiology and their health examination was done.
The permission from parents of the children, undergoing
examination and questionnaire survey was also taken
on the self designed consent form.The Centers for Dis-
ease Control and Prevention (CDC) suggests two levels
of concern for children based on the BMI-for-age charts.
At the 85th percentile and above, children are “at risk
for overweight”. At the 95th percentile or above, they
are “overweight”. The cutoff for underweight of less than
the 5th percentile is based on recommendations by the
World Health Organization Expert Committee on Physi-
cal Status 1998. The diagnostic criteria for diabetes mel-
litus have been modi ed from those previously recom-
mended by WHO (1985).Revised criteria from the report
of the expert committee on the diagnosis and classi ca-
tion of Diabetes Mellitus (2003) was used for the diag-
nosis of diabetes. Same criterion was used by Holly et al,
2003, Jung-Nan et al, 2003 and Reinehr (2013)
RESULTS AND DISCUSSION
Type 2 diabetes has several causes:genetics and lifestyle
are the most important ones. A combination of these
factors can cause insulin resistance. Diabetes is a com-
plex condition. Several factors must come together to
develop type 2 diabetes. For example, obesity and a sed-
entary lifestyle play a role. Genetics can also in uence
obesity and type 2 diabetes. Type 2 diabetes is caused
by both genetic and environmental factors. Obesity has
been attributed to various factors including genetics,
environment, metabolism, behavior, personal history of
obesity, culture, and socioeconomic status .In the total
population of 2048 subjects, 558 subjects had the posi-
tive family history of diabetes. Out of 558 subjects 12
(2.15%) subjects were found to have impaired glucose
level, 12 (2.15%) subjects have already developed diabe-
tes and both have family history diabetes in rst degree
relatives (Father, Mother, Father Mother both) Table 1
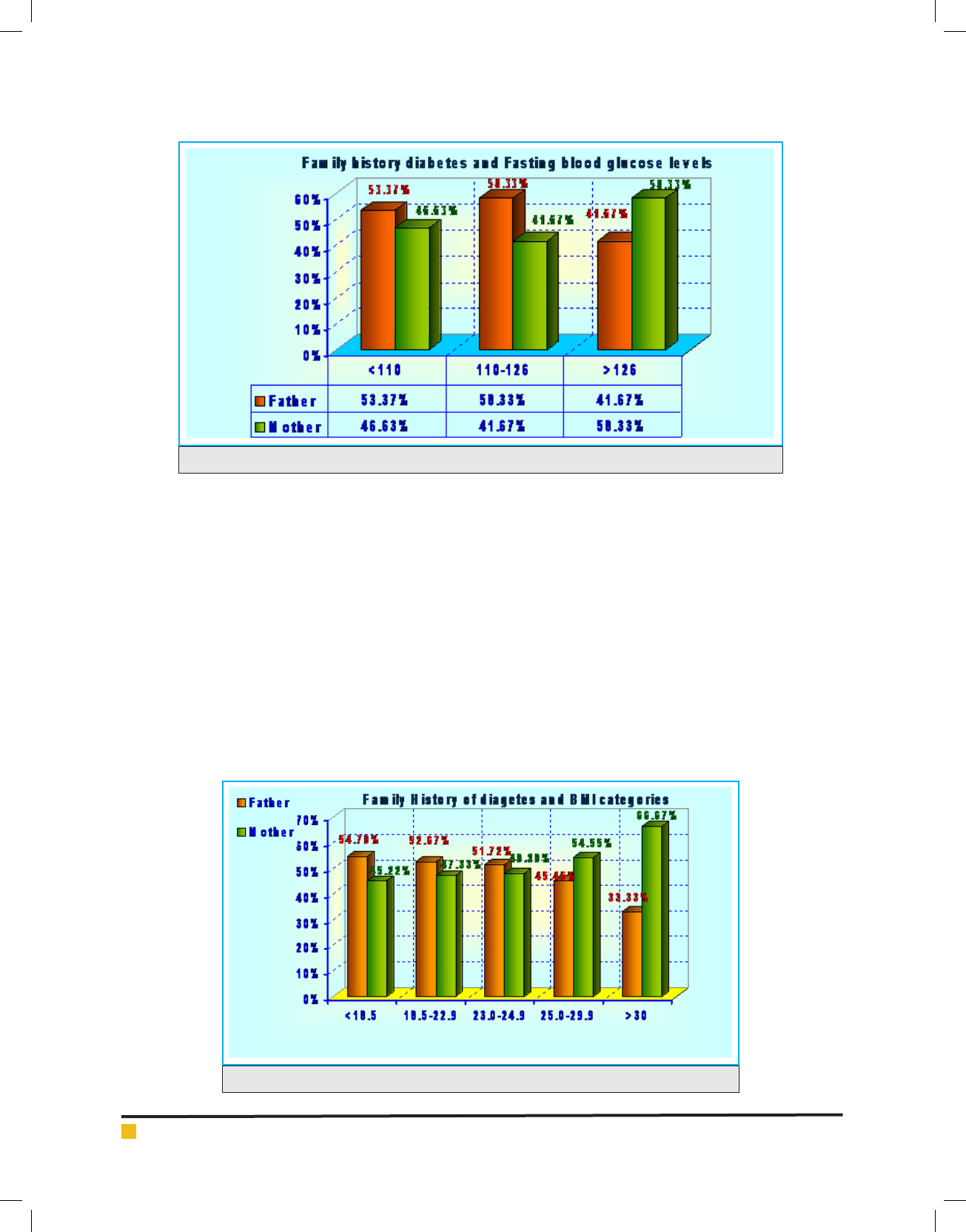
and graphs 1&2.
The lifetime risk of developing type 2 diabetes is 40%
for individuals who have one parent with type 2 diabetes
and 70% if both parents are affected. Type 2 diabetes are
about 3 times more likely to develop the disease than
individuals without a positive family history of the dis-
ease (Florez et al,2003). Type 2 diabetes itself is thought
to be a polygenic disorder that develops due to complex
interaction between multiple genes and environmental
factors.For type 2 diabetes, risk for developing the dis-
ease is increased if a close family member (parent, sib-
ling, or child) has type 2 diabetes or a medical condition
being overweight or obese, havinglipid abnormalities,
or high blood pressure (Gibson, 2011).
In the present study, 558 (27.3%) subjects have shown
positive family history for diabetes.The increased preva-
lence of type 2 diabetes in the relatives of affected sub-
jects is likely to re ect genetic predisposition to hypergl-
caemia with additional affects from shared environment
BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS DIABETIC PREDECESSORS: A FACTOR LEADING TO DIABETES IN SUCCESSORS 711
Manju Dewan
FIGURE 1.
FIGURE 2.
and life style (Shaw et al., 1999). Type 2 diabetes is rec-
ognized to arise from a combination of insulin resistance
and impaired beta cell function. There are several reasons
to consider that this could be particularly important in the
obesity-diabetes eld.(Ganada and Soeldner, 1987).
The rst reason is that evolutionary forces may have
shaped the human genome according to mechanisms
(fat storage and mobilization, insulin secretion and sen-
sitivity, leptin signaling, weight and body composition
regulation, availability of glucose to the brain, etc.) that
are now directly involved in the pathophysiology of
juvenile obesity and associated changes in insulin-fuel
homeostasis. These physiological functions and traits
were of major importance during the infancy, childhood,
and puberty of ancestors for metabolism, development,
and growth. It is likely that prehistoric metabolic genes
welcomed new mutations, provided that they favored
the storage of calories. The notion of the thrifty geno-
type (Neel, 1962) covers all kinds of genes that could
help early humans adapt to their hostile environment,
when food was scarce and rather unpredictable, but
nevertheless crucial for tness and reproduction. It is
likely that gene alleles favoring fat accumulation have
been selected by humans and are now turning their bad
effects to modern subjects because of an unexpected
caloric richness and sedentary environment. Similarly, it
is possible that insulin sensitivity underwent evolution-
ary changes toward increased channeling of glucose to
712 DIABETIC PREDECESSORS: A FACTOR LEADING TO DIABETES IN SUCCESSORS BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS

BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS DIABETIC PREDECESSORS: A FACTOR LEADING TO DIABETES IN SUCCESSORS 713
Manju Dewan
the large human brain rather than to the insulin-sensi-
tive muscle mass. Measuring these phenomena early in
life rather than in adulthood may more closely re ect
their evolutionary tendencies. In addition, the life span
of early humans was limited and evolution has there-
fore mostly worked on the physiology of young people
(Boyd-Eaton et al 1988and Ritenbaugh,1989)
The study of young individuals meets the goals of
predictive genetic epidemiology because it allows the
follow-up of genotyped patients through later pheno-
type evolution as well as clinical trials (Le Stunff et al,
2001). It has recently been put forward that several fat-
derived cytokines, including the anti-in ammatory adi-
ponectin, strongly modulate the risk of the metabolic
syndrome and T2D associated with obesity (diabesity)
(Lazar, 2006). Variation within the adiponectin gene is
reported to modulate plasma levels of adiponectin and
also to predict risk for diabesity and associated coronary
heart diseases (Vasseur et al, 2003). Paradoxically, the
adiponectin variant alleles that protect against the devel-
opment of diabesity by maintaining high adiponectin
concentrations also associate with obesity risk in both
adults and obese children (Bouatia-Naji et al, 2003).
Individuals with high adiponectin levels can be severely
obese but seem to enjoy metabolic protection (Vasseur
et al, 2005). In the general population, the same alleles,
together with the type 2 diabetes protective PPAR-g
12Ala allele associates with a coronary heart disease
protective risk factor pattern, elevated adiponectin and
insulin sensitivity but also with a dramatic increase of
3 units of body mass index (Tanko et al, 2005).
People having a close relative with type 2 diabetes
are at higher risk. There is also a strong inheritable
genetic connection in type 2 diabetes: having relatives
(especially rst degree) with type 2 increases risks of
developing this disease very substantially. In addition,
there is also a mutation to the Islet Amyloid Polypep-
tide gene that results in an earlier onset, more severe,
form of diabetes (Sakagashira, 1996). Developing type 2
diabetes is heavily in uenced by environmental factors.
Since our genetic code does not change signi cantly in
one or two generations, the recent secular trend in dia-
betes must be due mostly to changes in the environment.
Increased adiposity is the single most signi cant factor
in the development of type 2 diabetes and the epidem-
ics of obesity and type 2 diabetes largely parallel one
another. The increasing prevalence of obesity is thought
to be related primarily to changes in dietary habits and
our increasingly sedentary lifestyle, though other factors
(including toxins and infectious agents) may play a role.
Genes may in uence the risk of diabetes not only by
directly altering insulin action or secretion, but also by
altering how any given individual interacts with these
environmental factors (Cho et al 2003).
However, environmental factors (almost certainly diet
and weight) play a large part in the development of type
2 diabetes in addition to any genetic component. This
can be seen from the adoption of the type 2 diabetes
epidemiological pattern in those who have moved to a
different environment as compared to the same genetic
pool (Cotran and Collins, 1999).There is a stronger
inheritance pattern for type2 diabetes. Those with rst-
degree relatives with type2 diabetes have a much higher
risk of developing type2 diabetes, increasing with the
number of those relatives. Concordance among monozy-
gotic twins is close to 100%, and about 25% of those
with the disease have a family history of diabetes. Genes
signi cantly associated with developing type2 diabetes,
include TCF7L2, PPARG, FTO, KCNJ11, NOTCH2, WFS1,
CDKAL1, IGF2BP2, SLC30A8, JAZF1, and HHEX (Lys-
senkoet al, 2008). KCNJ11 (potassium inwardly rectify-
ing channel, subfamily J, member 11), encodes the islet
ATP-sensitive potassium channel Kir6.2, and TCF7L2
(transcription factor 7–like 2) regulates proglucagon
gene expression and thus the production of glucagon-
like peptide-1 (Rother et al, 2007). Moreover, obesity
(which is an independent risk factor for type2 diabetes)
is strongly inherited (National Diabetes Information-
Clearinghouse (NDIC), 2008).
Various hereditary conditions may feature diabe-
tes, for example myotonic dystrophy and Friedreich’s
Ataxia. Wolfram’s syndrome is an autosomal recessive
neurodegenerative disorder that rst becomes evident
in childhood. It consists of diabetes insipidus, diabetes
mellitus, optic atrophy and deafness, hence the acronym
DIDMOAD (Barrett 2001). A major risk factor of type 2
diabetes mellitus (T2DM) is a positive family history of
diabetes. In the present study it was found that family
historyofobesitywasmorelikelytohavemorepreva-
lence ofobesityandoverweightthanthosehavingfam-
ilyhistoryofdiabetes.Thisindicatesthatchildrenhav-
ing family history of obesity are more likely to
become obese or over weight and diabetes.In the pre-
sent study, subject having impaired glucose levels and
diabetes have the positive family history in rst degree
relatives 4.3% subjects have the 1st degree relatives in
having impaired glucose level and diabetes. Children
with type 2 diabetes usually have a family history of
this disease. Of the patients, 74–100% have a rst- or
second-degree relative with type 2 diabetes (American
Diabetes Association, 2000 and Arslanian, 2002). Of
note, diabetes in the parent or other relative may not
be recognized until the child is diagnosed. The high fre-
quency of relatives with type 2 diabetes demonstrate the
strong hereditary (likely multigenic) component to the
disease (Kiess et al, 2003).
Papaza ropoulou et al, (2017) suggested that the
likelihood of type 2 diabetes in the next generation is

714 DIABETIC PREDECESSORS: A FACTOR LEADING TO DIABETES IN SUCCESSORS BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS
Manju Dewan
higher in the event of a diabetic mother than father.
Both genetic factors, such as mitochondrial DNA muta-
tions, and environmental components such as intra-
uterine environment, have been implicated in the higher
maternal transmission of type 2 diabetes. Despite the
above ndings, some studies in populations with high
frequency of type 2 diabetes have not corroborated the
predominantly maternal transmission. Such works have
shown either an excess paternal or an equal transmis-
sion of type 2 diabetes.
Studies of (Patel et al 2013) and Srikanth(2015)
also showed that family history of diabetes was highly
prevalent among type 2 diabetic patients.First degree
relatives (FDR) of patients with type 2 diadetes were
more insulin resistant and are reported to had larger
abdominal subcutaneous adipocytes than adults with-
out a family history (Anthanont et al, 2017). Among
the type 2 patients in the study from Tamiln Naidu,
68.8% had a positive family history of type 2 diabetes
and 31.2% had a negative family history. Family history
of the study participants with type 2 diabetes was enu-
merated. Among the participants with positive family
history of diabetes, 25.1% of them had diabetic mother,
15.3% had diabetic father, 12.1% had both father and
mother with diabetes, 47.4% of them had siblings with
diabetes and 40% had family history of diabetes among
second degree relatives such as grandparents, aunts and
uncles (Geetha A et al. 2017)
ACKNOWLEDGEMENT
The author is highly thankful to UGC for providing grant
for undertaking the research award.
REFERENCES
Adeghate E, Schattner P, Dunn E.2006. An update on the eti-
ology and epidemiology of diabetes mellitus.Ann N Y Acad
Sci.;1084:1–29.
American Diabetes Association. 2000: Type 2 Diabetes in chil-
dren and adolescents. Pediatrics; 105:671–680.
Anthanont P,P Ramos,, Jensen M D& Hames K C.2017. Fam-
ily history of type 2 diabetes, abdominal adipocyte size and
markers of the metabolic syndrome International Journal of
Obesity;41,1621–1626(2017)
Arslanian S. 2002: Type 2 diabetes in children: clinical aspects
and risk factors. HormRes; 57:19–28.
Barrett TG.2001. “Mitochondrial diabetes, DIDMOAD and other
inherited diabetes syndromes”. Best Practice & Research. Clini-
cal Endocrinology & Metabolism; 15 (3): 325–43.
Bouatia-Naji N., MeyreD., Lobbens S., Seron K., Fumeron F.,
Balkau B., Heude B., Jouret B., Scherer P.E., Dina C.,et al. 2006.
ACDC/adiponectin polymorphisms are associated with severe
childhood and adult obesity, Diabetes,vol.55(pg.545-550)
Boyd-Eaton S, Konner M, Shostak M. 1988.: Stone-agers in
the fast lane: chronic degenerative diseases in evolutionary
perspective.Am J Med 84:739–749,
Center for Disease Control (CDC). Body mass Index: BMI for
children and teens.2000.apps.nccd.cdc.gov/dnpabmi.
Centers for Disease Control and Prevention.2003: National
Diabetes Fact Sheet: General Information and National Esti-
mates on Diabetes in the United States,.Rev.ed.
Cho YM, Kim M, Park KS, Kim SY, Lee HK . 2003 S20G muta-
tion of the amylin gene is associated with a lower body mass
index in Korean type 2 diabetic patients. Diabetes Res. Clin.
Pract.; 60 (2): 125–129.
Cotran, Kumar, Collins; Robbins .1999. Pathologic Basis of
Disease, Saunders Sixth Edition,; 913-926.
Elizabeth R. Pulgaron, PhD andAlan M. Delamater, PhD .2014.
Obesity and Type 2 Diabetes in Children.Epidemiology and
TreatmentCurrDiab Rep. Aug; 14(8): 508.
Florez JC, Hirschhorn J, Altshuler D.2003.The inherited basis
of diabetes mellitus: implications for the genetic analysis
of complex traits. Annu Rev Genomics Hum Genet; 4:257–
291.
Froguel P. 2005. ACDC/adiponectin and PPAR-gamma gene
polymorphisms: implications for features of obesity, Obes.
Res.,vol.13(pg.2113-2121)
Ganda,O. P. and Soeldner1987. Genetic, acquired and related
factors in the aetiology of diabetes mellitus. Arch Intern.
Med.,137: 461469.
G eetha A., Gopalakrishnan S., Umadevi R. 2017. Study on the
impact of family history of diabetes among type 2 diabetes
mellitus patients in an urban area of Kancheepuram district,
Tamil Nadu .Int J Community Med Public Health. 4(11):4151-
4156.
Gibson G. 2011. Rare and common variants: twenty argu-
ments.Nat Rev Genet.;13 :135–145.
Holly J. Kramer, MD, MPH; Quan Dong Nguyen, MD,
MSc; Gary Curhan, MD, ScD; et alChi-yuan Hsu, MD, MSc.
2003. Renal Insuf ciency in the Absence of Albuminuria and
Retinopathy Among Adults With Type 2 Diabetes Mellitus
JAMA.;289(24):3273-3277.
Jung-Nan Wei, PhD; Fung-Chang Sung, PhD; Chau-Ching
Lin, MD;et alRuey-Shiung Lin, MD, DrPH;Chuan-Chi Chiang,
PhD;Lee-Ming Chuang, MD, PhD. 2003. National Surveillance
for Type 2 Diabetes Mellitus in Taiwanese Children JAMA.;
290 (10):1345-1350.
Kiess W, BöttnerA, Raile K, Kapellen T, MüllerG, Galler A,
Paschke R &Wabitsch M. 2003. Type 2 diabetes mellitus in
children and adolescents: a review from a European perspec-
tive. Horm Res; 59 suppl1:77−84.
Lazar M.A. 2006.The humoral side of insulin resistance. Nat.
Med.,vol.12(pg.4344)
Le Stunff C, Fallin D, Bougnères P.2001. Paternal transmis-
sion of class I INS VNTR alleles predisposes to childhood obe-
sity.Nat Genet 29:96–99.

BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS DIABETIC PREDECESSORS: A FACTOR LEADING TO DIABETES IN SUCCESSORS 715
Manju Dewan
Lyssenko V, Jonsson A, Almgren P, et al. 2008. Clinical risk fac-
tors, DNA variants, and the development of type 2 diabete. The
New England Journal of Medicine; 359 (21): 2220–32.
National Diabetes Information Clearinghouse (NDIC) National
Institute of Diabetes and Digestive and Kidney Diseases,
NIH). 2008. http://www.diabetes.niddk.nih.gov/dm/pubs/mody/.
Retrieved.
Neel JV.1962. Diabetes mellitus: a‘thrifty genotype rendered
detrimental by ‘progress’?Am J Hum Genet14:353–362.
Nina E. Berentzen,Alet H. Wijga,Lenie van Rossem, Gerard H.
Koppelman,Bo van Nieuwenhuizen,Ulrike Gehring,Annemieke
M.W.Spijkerman, HenriëtteA.Smit Family history of myocar-
dial infarction, stroke and diabetes and cardiometabolic markers
in children Diabetologia August 2016, Volume 59, Issue 8,pp
1666–1674
Patel M, Patel IM, Patel YM, Rathi SK. 2013. A hospitalbased
observational study of type 2 diabetic subjects from India. Int
J Clin Pract.; 24(2):141-8.
Papaza ropoulou AK, Papanas N, Melidonis A, Maltezos E.
2017. Family History of Type 2 Diabetes: Does Having a Dia-
betic Parent Increase the Risk? Curr Diabetes Rev.;13(1):19-25
Omar, Ali. 2013. Genetics of type 2 diabetes World J Diabetes.
Aug 15; 4(4): 114–123.
Reinehr Thomas. 2013. Type 2 diabetes mellitus in children
and adolescents. World J Diabetes. Dec 15; 4(6): 270–281.
Ritenbaugh C, Goodby CS. 1989. Beyond the thrifty gene:
metabolic implications of prehistoric migration into the New
World.Med Anthropol 11:227–223.
Rother KI. 2007. Diabetes treatment—bridging the divide. The
New England Journal of Medicine 356: (15): 1499–501.
Sakagashira S, Sanke T, Hanabusa T, et al. 1996 . Missense
mutation of amylin gene (S20G) in Japanese NIDDM patients.
Diabetes; 45 (9): 1279–81.
Shaw, J.T.E., Purdie, D.M., Neil, H.A.W., Levy, J.C., Turner, R.C.
1999. The relative risk of hyperglycemia, obesity and dyslipi-
daemia in the relatives of patients with type-II diabetes mel-
litus. Diabetologia; 42: 27-37.
Srikanth E. 2015. Familial Aggregation of Type 2 Diabetes
Mellitus in Rural India. IJSR.:4(8):41-5. 17.
Tanko L.B., Siddiq A., Lecoeur C. Larsen P.J.Christiansen C.,
Walley A., Tillil H, Köbberling J. 1987. Age-corrected empiri-
cal genetic risk estimates for rst-degree relatives of IDDM
patients.Diabetes.; 36:93–99.
The Expert Committee on the Diagnosis and Classi ca-
tion of Diabetes Mellitus
.2003. From the American Diabe-
tes Association, Alexandria, Virginia Diabetes Care; 26:S5-
S20.
Vasseur F., Helbecque N., Lobbens S., Vasseur-Delannoy V., Dina
C., Clement K., Boutin P., Kadowaki T., Scherer P.E.,Froguel P.
2005. Hypoadiponectinaemia and high risk of type 2 diabetes
are associated with adiponectin-encoding (ACDC) gene pro-
moter variants in morbid obesity: evidence for a role of ACDC
in diabesity, Diabetologia,vol.48(pg.892-899)
Vasseur F. Lepretre F., Lacquemant C., Frogue lP. 2003. The
genetics of adiponectin,Curr. Diab. Rep.,vol.3(pg.151-158).
World Health Organization Study Group on Diabetes Mellitus.
1985. Technical Report Series, 727, WHO Geneva,
World Health Organization. 1998. Obesity: preventing and
managing the global epidemic. Report of a WHO consultation
on Obesity, Geneva, 3–5, June 1997. World Health Organiza-
tion: Geneva.
Yanyan Zhao,ChunhuaSong,XiaokunMa,XiaojunMa,Qing-
zhu Wang,HongfeiJi,FengGuo,andGuijunQin
Synergistic.
2017Effect of Family History of Diabetes and Dietary Habits
on the Risk of Type 2 Diabetes in Central China International
Journal of Endocrinology., 8 pages