
Medical
Communication
Biosci. Biotech. Res. Comm. 10(1): 167-171 (2017)
Evaluation of obsessive compulsive disorder and
depression symptoms in visitors of hair and skin clinic
of Shohadaye Ashayer Hospital of Khorramabad
Afarin Ahmadian
Medical Student, Shahid Beheshti University of Medical Sciences, Tehran, Iran
ABSTRACT
The main aim of this research is reports related to high prevalence of OCD and undiagnosed depression disorders
in visitors of skin clinics.164 visitors of skin clinics were chosen by the use of (simple random) sequential sampling
and by the use of Maudsley OCD scale and Beck’s revised depression questionnaire and a DSM-IV based clinical
interview; they were surveyed based on catching obsession along with depression disorders. The obsession severity
was determined based on Maudsley OC scale and depression severity was determined based on Beck’s revised depres-
sion questionnaire and also they were surveyed in terms of pattern of obsession and depression symptoms and skin
complaints.81 individuals were diagnosed with OCD; 76 were diagnosed with OCD along with depression symptoms.
From visitors suffering from obsession along with depression symptoms they were based on DSM-IV scales and none
of them had any pre-diagnosis. Type and dispersion of obsession symptoms along with depression symptoms had
no signi cant difference with normal clinical status. 5 individuals had no depression (6.2%) and 11 individuals had
minor depression (13.6%), 13 individuals had medium depression (16.1%) and 52 individuals had severe depression
(64.1%). Results indicated high prevalence of clinical symptoms of obsession along with depression symptoms in
visitors of hair clinics; thus it is better to pay more attention to diagnosis and treatment of individuals suffering from
obsession along with depression symptoms who do not refer to hair clinics.
KEY WORDS: DISORDER, COMPULSIVE OBSESSION, DEPRESSION, HAIR CLINICS
167
ARTICLE INFORMATION:
*Corresponding Author:
Received 1
st
Jan, 2017
Accepted after revision 22
nd
March, 2017
BBRC Print ISSN: 0974-6455
Online ISSN: 2321-4007 CODEN: USA BBRCBA
Thomson Reuters ISI ESC and Crossref Indexed Journal
NAAS Journal Score 2017: 4.31 Cosmos IF : 4.006
© A Society of Science and Nature Publication, 2017. All rights
reserved.
Online Contents Available at: http//www.bbrc.in/
168 EVALUATION OF OBSESSIVE COMPULSIVE DISORDER AND DEPRESSION SYMPTOMS BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS
Afarin Ahmadian
INTRODUCTION
Major depressive disorder is considered as the third most
common disorder and OCD is considered as the 4
th
com-
mon psychiatric disorder . Due to their characteristics
these disorders could have destructive effects on profes-
sional, educational and social performance of the indi-
vidual; for instance, OCD, due to characteristics such as
excessive washing, and excessive checking could cre-
ate disorders in family functions and quality of life.
Recently the researchers have found out that destruction
level of performance of this disorder could be compared
with psychotic disorders (Torres et al, 2006 Eisen et al,
2006, Sadock and Sadock 2007).
Based on most studies conducted on OCD, this dis-
order has a relationship with many other mental dis-
orders. Depression is one of its most common disorders
which overlap OCD (Keeley et al, 2008). Obsessive people
tend to depression more than other people and based on
conducted studies, depressive mode not only results in
increase and severity of undeliberate thoughts but also
results in increased discomfort caused by these thoughts
(Dadsetan 1999). Almost two third of individuals suffer-
ing from obsession also suffer from depression symp-
toms (Ghassemzadeh et al, 2006 Khairabadi et al 2011
and Ghosh et al 2013).
Most researchers believe that in terms of symptoms
there is an overlap between these two in terms of sense
of guilt, anxiety, self-doubts, and low self-esteem. Some
also discuss feeling of severe responsibility and ideal-
ism in obsession which are considered as features of
depression. Also, it has been shown that some admin-
istrative inef ciency is observed in obsessed patients
during implementation of tests which are the result of
concurrency of depression symptoms and OCD (Arntz
et al, 2007; Aycicegi et al, 2003). Some studies have
shown that high percentage of patients suffering from
OCD or its symptoms, refer to outpatient skin clinics due
to skin signs and symptoms (Demet et al, 2005; Hatch
et al, 1992). Gupta et al 2003 and Ghosh et al 2013 have
showed that 20 to 40 percent of individuals referring
to skin clinics also suffer from psychological problems.
(Ellis and Koblenzer 2005; Gupta and Gupta 2003 and
Ghosh et al 2013).
Companionship of OCD skin manifestations are called
Dermo-OCD in some studies and it is divided into two
groups of obsessive and compulsory manifestations.
According to this division, complaints such as hair fall,
ugliness and though of catching malignant sexual dis-
eases, fungal infections and aids are examples of obses-
sion and manifestations such as hair pulling, nervous
itching, nail pulling, lip licking, and skin irritations
and in ammations caused by excessive hand wash are
examples of Compulsive disorder (Aycicegi et al, 2003;
Koblenzer 1992; Stein and Hollander 1992). The current
study has been conducted with the aim of determin-
ing frequency and OCD severity along with depression
signs and determining the possible relationship between
obsession and a part of demographic variables in indi-
viduals referring to outpatient skin clinics of Shohadaye
Ashayer Khorramabad hospital.
MATERIAL AND METHODS
The current research methodology is descriptive-analyt-
ical and it is a cross sectional study. This study has been
conducted on 164 individuals referring to outpatient
hair and skin clinics of Shohadaye Ashayer Khorram
Abad. In this study demographic information such a age,
gender, marital status, education, disease duration and
clinical diagnosis of skin experts for diseases were col-
lected in an inventory. Maudsley Obsessive-Compulsive
Disorder Inventory (MOCI) was used in this study for
screening prevalence of obsession including 30 right and
wrong items (Hodgson RJ and Rachman S, 1977). and it
is designed for evaluating OCD symptoms. In addition to
an overall obsession score, this inventory also includes
4 sub-scores for reviewing, cleaning and washing, rep-
etition slowness, doubt-accuracy. Total Maudsley score
range is from 0 to 30. Validity and reliability of MOCD
has been con rmed in different countries. In Iran, Stakti
(1976) has achieved 0.85 for reliability through retest
and Dadfar (1997) has achieved 0.84 for total test reli-
ability coef cient and its convergent validity has been
0.87 through Yale-Brown OCD scale (Ghassemzadeh
et al, 2002). Beck revised depression questionnaire has
been used in this study in order to screen depression and
its severity (Beck AT. et al, 1961) This is a self-report
21-question tools used for evaluating depression sever-
ity and its total score is 0 to 63. 0 to 13 is normal, 14 to
19 is minor depression, 20 to 28 is medium depression,
29 to 63 is severe depression. Iranian researchers have
achieved 0.87 for test total reliability coef cient and
0.74 for its validity (Ghassemzadeh et al, 2005). In order
to diagnose OCD, patients with scores above 15 and for
diagnosing depression, patients with scores above 14
were participated in a clinical interview by the psychia-
trist according to DSM-IV scales and all of their diagno-
ses were con rmed. Information were collected by the
use of SPSS and analyzed by the use of statistical tests.
RESULTS AND DISCUSSION
Descriptive statistics for expression of demographic
speci cations of research units showed that 43.3% of
research units were females and 56.7% were males. In
terms of education the highest frequency was related to
BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS EVALUATION OF OBSESSIVE COMPULSIVE DISORDER AND DEPRESSION SYMPTOMS 169
Afarin Ahmadian
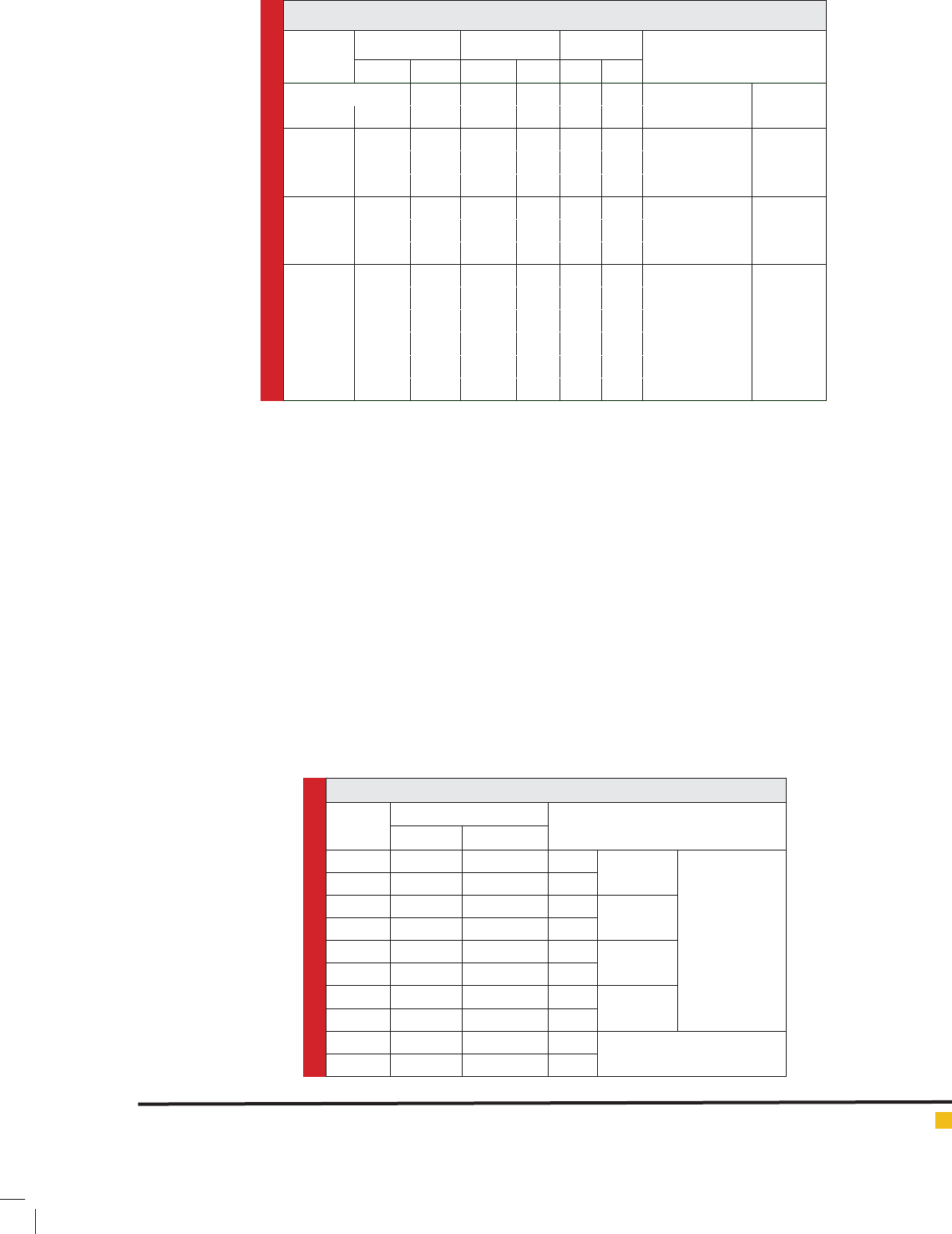
Table 2. Depression rate among patients with and without OCD.
Total obsession
Sum
UnhealthyHealthy
Depression level
Normal
No.358
%38%63%100%
Minor
depression
No.81119
%42%58%100%
Medium
depression
No.141327
%52%48%100%
Severe
depression
No.5852110
%53%47%100%
Total sum %
No.8381164
51%49%100%
high school level (53.7%) and the lowest was related to
primary level (6.7%). In terms of marital status (40.8%)
were single, (54.3%) were married and (4.9%) were
divorced. In terms of job, the highest frequency was
related to administrative level (29.9%) and the lowest
frequency was related to worker level (1.8%).
From 164 individuals, 81 individuals (49.4%) were
diagnosed with OCD; which means that their MOCD was
between 15 and 30 and their clinical interview was con-
rmed by the psychiatric and 83 individuals out of total
samples (51.6%) were free of OCD. This means that their
scale score was below the level. None of the samples
were previously diagnosed with OCD nor treated. In this
study the relative frequency of OCD had no signi cant
different between men and women (P>0.05) (table 1).
From 81 individuals with OCD, 76 individuals had
OCD along with depression symptoms; which meas
that their Beck scale score was between 14-63 and their
clinical interview has been con rmed by the psychiat-
ric. 5 individuals were depression free (6.2) which means
score of 0 to 13 and 11 individuals had minor depression
(13.6%) which means score 14 to 19 and 13 individuals
had medium depression (16.1%) which means score 20
to 28 and 52 individuals had severe depression (64.1)
which means score 29 to 63 (Table 2).
In the current study from 164 individuals, 81 indi-
viduals (49.4%) of individuals referring to skin clinics
were diagnosed with OCD according to Maudsley scale.
From 81 individuals, 76 individuals were diagnosed with
OCD along with depression and all of them surveyed by
the psychiatrist according to DSM-IV through structured
interview and their OCD diagnosis were con rmed. OCD
prevalence in individuals were reported to be (49.4%); in
study by Demet et al this score was 24.7%; Omrani et al
Table 1. some of the demographic features of total studied samples.
Variable name No.
Total No.OCD OCD Free
P value
%No.%No.%
Gender
Female713/43385/53335/46
49/0
Male937/56432/46508/53
Education
University656/39145/21515/78
54/0 High school887/5315177383
Primary school117/622/1898/81
Marital
status
Single6740.8352/52328/47
07/0 Married8954.3433/48467/51
Divorced84.935/3755/62
Job
Administrative499/29156/30344/69
40/0
Housewife426/25112/26318/73
Worker38/1003100
Student246/1447/16203/83
Freelancer325/1934/9296/90
Unemployed146/8
34/21116/78
Afarin Ahmadian
170 EVALUATION OF OBSESSIVE COMPULSIVE DISORDER AND DEPRESSION SYMPTOMS BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS
(22.1%) and KheirAbadi et al (52.3%) and Fineberg et al
reported 20%. In a study conducted in turkey this rate
was 24.7% which is consistent with our current research.
In our study, comparing to the public population there
was higher OCD prevalence; updated reported rate in
skin outpatient patients was more than other studies and
this indicates increased rate of OCD in population.
Regarding the high prevalence of OCD and depres-
sion among the individuals referring to skin clinics, two
hypotheses are discussed. The rst hypothesis is that the
same as other psychological disorders, clinical symptoms
of OCD along with depression are rstly manifested by
physical complaints and most people rstly refer to non-
psychological medical centers and the second hypothesis
is that obsessive individuals with depression symptoms
are usually more careful about their health and refer to
doctors more than others.
These results show that most of the individuals refer-
ring to skin disease medical centers simultaneously suf-
fer from OCD and depression and these psychological
disorders are signi cantly severe and need special care.
On the other hand, there was no signi cant difference
between relative frequency of OCD along with depres-
sion symptoms among men and women and healthy and
unhealthy people (P>0.05). this result is consistent with
results achieved from studies of several workers, ( Demet
et al., 2005., Omranifard et al., 2007, Kheir Abadi et al.
2011 and Fineberg et al. 2003)
Additionally, there was no signi cant difference
between relative frequency of OCD along with depres-
sion symptoms, and education in healthy and unhealthy
individuals (P>0.05). This result is inconsistent with
results of Omranifard et al., (2007) and this difference
may be due to elevating the educational level in Iran
in time. There was no signi cant difference between
relative frequency of OCD along with depression symp-
toms, marital status, and job of healthy and unhealthy
individuals (P>0.05) and this result in consistent with
research results of Demet et al., 2005 Omranifard
et al. 2007, Kheir Abadi et al.,2011., and Fineberg et al.
2003)
What could be achieved through surveying the cur-
rent research results is that there is a very complicated
relationship between skin diseases and OCD along with
depression symptoms; in a way that their skin problems
could overlap OCD and depression symptoms; some
researchers consider skin complaints as the secondary
effects of OCD with depression symptoms; and they have
stated that insuf cient touch of surrounding things due
to obsessive sensitivity could result in problem and
weakness of imagination in individual’s body and con-
sequently it may cause the individual to be mentally
occupied with one’s physical defects and refer to a der-
matologist with skin complaints; or excessive washing
caused by obsession may result in skin irritations and
create secondary effects (Kheirabadi et al, 2011).
CONCLUSION
Prevalence of OCD along with depression symptoms in
patients with skin disorders referring to skin clinics is
signi cantly higher than the reported amounts from
prevalence of this disorder in public. For curing skin
problems, it must be noted that in case of presence of
OCD along with undiagnosed depression symptoms and
not on-time treatment of these disorders could create
problems for skin conditions and decrease its successful
effect. Thus regarding the stated problems, the coopera-
tion and efforts of dermatologists and psychologists are
needed.
But regarding the prevalence of OCD along with
depression symptoms and unawareness of people
regarding its symptoms, causes and OCD/depression
treatments, it seems that it is necessary to educate pub-
lic through media, magazines and newspapers about
the relationship between OCD, depression symptoms
and curability of these disorders. Also it is necessary to
prioritize training of school health teachers and other
people in charge in medical centers in order to detect
patients suffering from these disorders and guide them
toward expert services.
REFERENCES
Arntz A, Voncken M, Goosen A. (2007). Responsibility and
obsessive- compulsive disorder: An experimental test. Behav
Res Ther; 45(3): 425-35.
Aycicegi A, Dinn WK, Harris CL, Erkmen H. (2003). Neuropsy-
chological function in obsessivecompulsive disorder: Effects
of comorbid conditions on task performance. Eur Psychiatry;
18(5): 241-8.
Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. (1961).
An inventory for measuring depression. Archives of general
psychiatry. 4 (6): 561-71.
Dadsetan P. (1999). [Developmental psychopathology, from
infancy to adulthood]. 7th ed. Tehran: Samt; 147-77.
Demet MM, Deveci A, Taskin EO, Ermertcan AT, Yurtsever F,
Deniz F, (2005). Obsessivecompulsive disorder in a dermatol-
ogy outpatient clinic. Gen Hosp Psychiatry; 27(6): 426-30.
Eisen JL, Mancebo MA, Pinto A, Coles ME, Pagano ME, Stout
R (2006). Impact of obsessive compulsive disorder on quality
of life. Comp Psychiatry. 47: 270-5.
Ellis CN, Koblenzer CS. (2005). Psychiatric evaluation of the
dermatology patient. Dermatol Clin; 23(4): 591-9.
Fineberg NA, O’Doherty C, Rajagopal S, Reddy K, Banks A,
Gale TM. (2003). How common is obsessive compulsive dis-
order in a dermatology outpatient clinic? J Clin Psychiatry;
64(2): 152.
BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS EVALUATION OF OBSESSIVE COMPULSIVE DISORDER AND DEPRESSION SYMPTOMS 171
Afarin Ahmadian
Ghassemzadeh H, Karamghadiri N, Shari V, Norouzian M,
Mojtabai R, Ebrahimkhani N. (2006). Cognitive, neuropsycho-
logic and neurological function in obsessive-compulsive disor-
der with and without depression symptoms. Cognitive sciences
novelties; 7(3): 1-13.
Ghassemzadeh H, Mojtabai R, Khamseh A, Ebrahimkhani N,
Issazadegan A-A, Saif-Nobakht Z. (2002). Symptoms of obses-
sive-compulsive disorder in a sample of Iranian patients. Inter-
national Journal of Social Psychiatry. 48 (1): 20-8
Ghassemzadeh H, Mojtabai R, Karamghadiri N, Ebrahimkhani
N. (2005). Psychometric properties of a Persian-language ver-
sion of the Beck Depression Inventory-Second edition: BDI-II-
PERSIAN. Depression and anxiety. 21 (4): 185-92.
Ghosh S. Sreyoshi Ghosh,Rishikesh V Behere,PSVN Sharma,K
Sreejayan (2013) Psychiatric evaluation in dermatology: An
overview Indian J of Dermatology Volume : 58 | Issue: 1 |
Page: 39-43
Gupta MA, Gupta AK. (2003). Psychiatric and psychological
co-morbidity in patients with dermatologic disorders: epidemi-
ology and management. Am J Clin Dermatol; 4(12): 833-42. 4
Hatch ML, Paradis C, Friedman S, Popkin M, Shalita AR.
(1992). Obsessive-compulsive disorder in patients with chronic
pruritic conditions: case studies and discussion. J Am Acad
Dermatol; 26(4): 549-51. 9
Hodgson RJ, Rachman S. (1977). Obsessional-compulsive com-
plaints. Behaviour research and therapy. 15 (5): 389-95.
Keeley ML, Storch EA, Merlo LJ, Geffken GR. (2008). Clini-
cal predictors of response to cognitive behavioral therapy for
obsessive-compulsive disorder. Clin Psychol Rev. 28: 118-30.
Kheirabadi GH, Dr. E. Salmasi, Dawn akbarpoor, Dr. Moon
Facies Naderian. (2011). Obsessive-compulsive disorder in
patients attending a public clinic eczematous skin Asfhanmjlh
School of Medicine in Asfhanhfth quarter / year Twenty-Nine
/ Number
Koblenzer CS. (1992). Dermatology and conditions related to
obsessive-compulsive disorder. J Am Acad Dermatol; 27(6 Pt
1): 1033-5.
Omranifard V, Kheirabadi GhR, Abtahi SMM, Kamali M. (2007).
Obsessive-compulsive disorder among outpatient referrals to
dermatologic clinics of Isfahan. Ofogh-e-Danesh Journal;
13(2): 52-7.
Sadock B, Sadock V. (2007). Synopsis of psychiatry: behavioral
sciences/clinical psychiatry. Philadelphia, PA: Lippincott, Wil-
liams & Wilkins.
Stein DJ, Hollander E. (1992). Dermatology and conditions
related to obsessive-compulsive disorder. J Am Acad Dermatol;
26(2 Pt 1): 237-42.
Torres AR, Prince MJ, Bebbington PE, Bhugra D, Brugha TS,
Farrell M. (2006). Obsessivecompulsive disorder: Prevalence,
comorbidity, impact, and help-seeking in the British National
Psychiatric Morbidity survey of 2000. Am J Psychiat. 163(11):
1978-85.