
Medical
Communication
Biosci. Biotech. Res. Comm. 10(1): 51-55 (2017)
A comparative analysis of the in uence of adding
morphine and tramadol to lidocaine in para cervical
block on the level of post-operation analgesia among
the patients applying for curettage
Alireza Kamali
1
, Rahele Rezaei Ashtiyani
2
, Maryam Shokrpour
2
and Shirin Pazoki
2
1
Department of Anesthesia, Arak University of Medical Sciences, Arak, Iran
2
Department of Gynecology, Arak University of Medical Sciences, Arak, Iran
ABSTRACT
Curettage is one of the most common operations among women. Several methods are used to reduce post-operation pain. The
present research seeks to study the effect of adding morphine and tramadol to lidocaine in para cervical block on post-operation
analgesia. This is a double-blind clinical trial conducted on 120 women applying for curettage. The participants were divided into
three completely random groups. The rst group received 5cc lidocaine 1.5% along with 1 mg (1cc) morphine (totally 6cc), the
second group received lidocaine 1.5% and 2 mg (1cc) tramadol, and the third group received 5cc lidocaine with 1cc distilled water
as placebo for para cervical block. The length and intensity of pain was registered based upon VAS table and time for requesting
painkiller after operation for all three groups. The pain score in the 0th, 30th, and 60th minute in those groups receiving morphine
and tramadol was less than what was observed in the group who had received lidocaine (P < 0.05), but the pain score in all times
in the group who had received tramadol was signi cantly less than other groups (P<0.05). The rst painkiller in morphine and
tramadol groups was asked much later than lidocaine group (P < 0.05) but no signi cant difference was observed between the
morphine and tramadol groups. The side effects were similar in all groups with lower levels of Bradycardia observed in placebo
group (P < 0.05). Morphine and tramadol were more effective than lidocaine creating para cervical block and analgesia and reduc-
tion of pain following the operation but tramadol exhibited a lower pain score throughout the research. The average length of
analgesia in placebo group was less than what was observed in other two groups. However, no signi cant difference was observed
between tramadol and morphine groups in terms of the length of analgesia after operation.
KEY WORDS: CURETTAGE, MORPHINE, TRAMADOL, ANALGESIA
51
ARTICLE INFORMATION:
*Corresponding Author: Maryam_shokrpour@yahoo.com
Received 27
th
Nov, 2016
Accepted after revision 20
th
March, 2017
BBRC Print ISSN: 0974-6455
Online ISSN: 2321-4007 CODEN: USA BBRCBA
Thomson Reuters ISI ESC and Crossref Indexed Journal
NAAS Journal Score 2017: 4.31 Cosmos IF : 4.006
© A Society of Science and Nature Publication, 2017. All rights
reserved.
Online Contents Available at: http//www.bbrc.in/
52 A COMPARATIVE ANALYSIS OF THE INFLUENCE OF ADDING MORPHINE AND TRAMADOL TO LIDOCAINE BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS
Alireza Kamali et al.
INTRODUCTION
Curettage is one of the most common types of gyneco-
logical operations in Iran and the whole world. As many
as 660 thousand curettages in the rst three months of
pregnancy were carried out in the US in 2003. General,
local or para cervical block anesthesia is used in this
type of operation. General anesthesia exhibits a higher
level of bleeding, womb trauma, and even death as a
result of hypoventilation and aspiration. As a result,
merely 10% of clinics in the US utilize general anesthe-
sia. Local anesthesia with/without oral treatment is used
in 58% of the patients and intravenous sleep drug mixed
with local anesthesia is used in 32% of cases (Mankowski
et al. 2014 and Poornima 2014).
Para cervical block is one of these available meth-
ods. Para cervical block prevents transmission of pain.
The sympathetic and parasympathetic sensory bers
are located in the internal surface of cervix before run-
ning through the womb. During cervix dilatation, pain
signals are transmitted through parasympathetic bers
and the process continues along the vaginal and liga-
ment vessels. As a result, para cervical block takes place
within the 3
rd
and 9
th
hours Kingston and Charles 2009).
The most common type of medicine used for local anes-
thesia is lidocaine. Lidocaine is economically affordable
and it had less side effects compared to other anesthet-
ics. Tramadol is an opioid pain medication used to tran-
quilize mild to severe pains. Morphine is a strong opioid
derived from opium and it is considered to be the most
important effective compound of opium Gourlay, (1988),
Ejlersen, et al. (1992) and Bray eld, (2013) and Yektag
Gümü (2016).
Considering the side effects of general anesthesia
and in order to prevent blood loss among emergency
patients, para cervical block can be really effective. Para
cervical block is an anesthetics method carried out by
gynecologists and it doesn’t require the constant pres-
ence of anesthesiologist. As a result, it is the best method
in emergency conditions. Various researches have uti-
lized different medical compounds in para cervical block
the most common of which is lidocaine 2%. Consider-
ing the little analgesic effects of lidocaine in post-oper-
ational analgesia after para cervical block, we decided to
enhance the intensity and length of analgesia by adding
morphine and tramadol to the common local anesthetics
(lidocaine).
MATERIAL AND METHODS
This double-blind, random. Clinical trial was carried out
on 120 women aging 20 to 45 years old who had resorted
to Taleghani Hospital of Arak for curettage. Using the
table of randomized numbers, the participants were
randomly divided into three groups: lidocaine and mor-
phine, lidocaine and tramadol, and lidocaine and dis-
tilled water. Each group consisted of 40 participants. The
quali ed patients took part in the research after obtain-
ing their consent. After each full monitoring of vital sig-
nals (ECG, BP, RP, BP, SPO2), the patients received as
much as 3 to 5 cc/kg crystalloid liquid as the alternative
liquid. The patients were then asked to lie on their back
and all of them received 2mg Midazolam and 2cc (10
mg) Sufentanil as sedative. The patients were then asked
to assume a lithotomical position. They underwent para
cervical block in a fully esterilized condition.
The rst group received 5cc lidocaine 1.5% along
with 1 mg (1cc) morphine (totally 6cc), the second group
received lidocaine 1.5% and 2 mg (1cc) tramadol, and
the third group received 5cc lidocaine with 1cc distilled
water as placebo for para cervical block. The length and
intensity of pain was registered based upon VAS table
and time for requesting painkiller after operation for
all three groups. 10 cc syringes containing the medi-
cine were prepared in advance by anesthesiologist and
marked with A, B, and C. The researchers were provided
with the syringes and para cervical block was carried
out. To make sure about accomplishment of full block
and analgesia, the level of patient’s cooperation at
the beginning of the operation was registered and the
patients were asked if the felt any pain.
Having made sure about the site of the above-said
blocks, curettage was conducted. Every 5 minutes dur-
ing the operation, the hemodynamic status of the patient
(including PR, BP) was registered in the questionnaire.
When the operation was over, the pain level of the
patients was measured 30 and 60 minutes later in the
recovery room using VAS (visual analog score) ruler.
The average length of patients analgesia was also meas-
ured by registering the time when the rst painkiller
was requested. Finally, SPSS 16 was used to analyze the
information obtained by questionnaires.
RESULTS AND DISCUSSION
This research was conducted on 120 women aging 20
to 45 resorting to Taleghani Hospital of Arak for curet-
tage. The participants were randomly divided into three
groups: lidocaine with morphine, lidocaine with tram-
adol, and lidocaine with distilled water. Each group
consisted of 40 people. No signi cant difference was
observed among the patients in terms of the average age
and age of pregnancy (P ≥ 0.05). As P ≥ 0.05, no signi -
cant difference was observed between the three groups
in terms of average blood pressure, heart rate and levels
of arterial oxygen saturation.
Considering P ≤ 0.05, the average length of analgesia
in placebo group was much less than what was observed
BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS A COMPARATIVE ANALYSIS OF THE INFLUENCE OF ADDING MORPHINE AND TRAMADOL TO LIDOCAINE 53
Alireza Kamali et al.
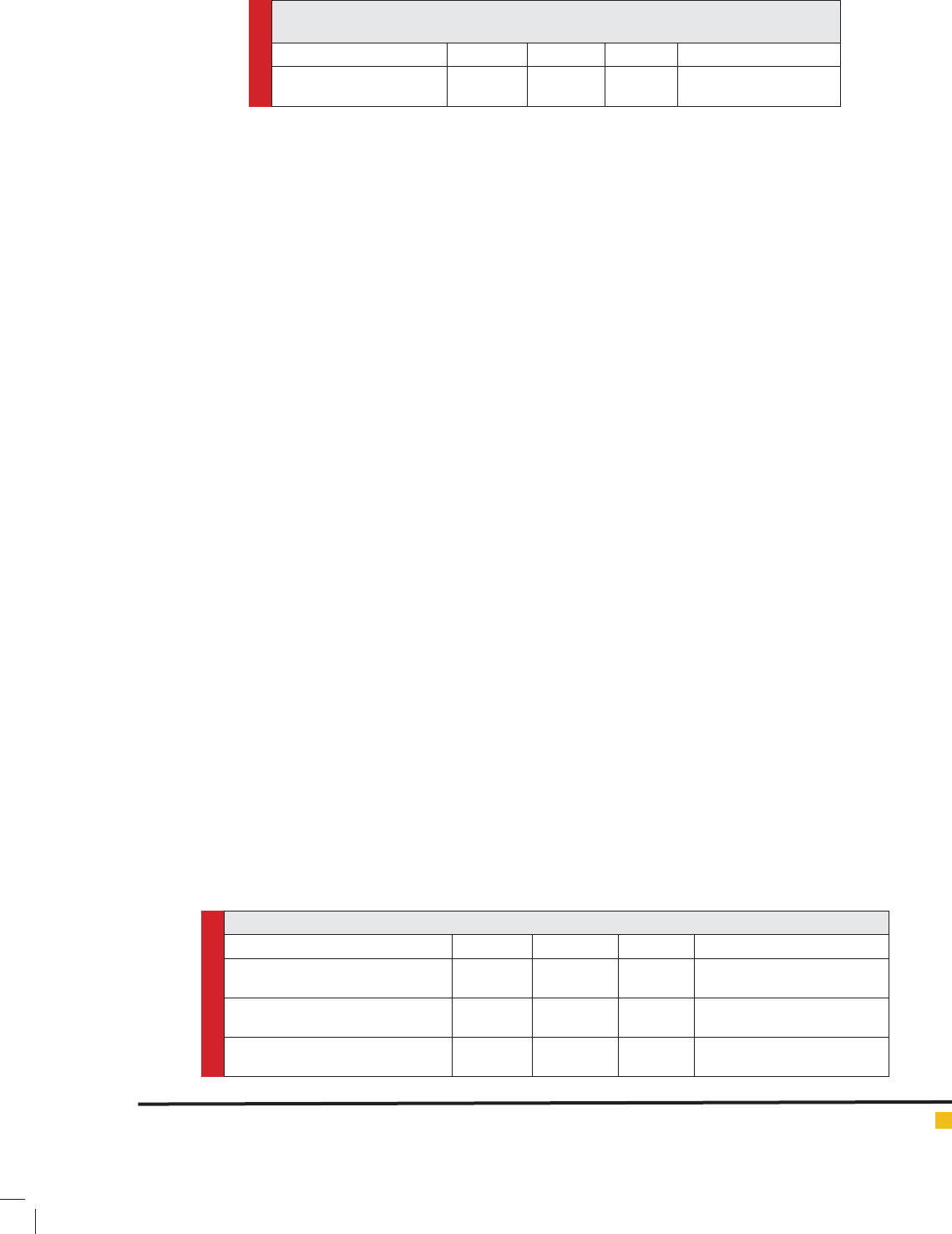
Table 1. Comparing the length of analgesia among patients applying for curettage in
three groups
Groups Tramadol Morphine Placebo P-value statistical test
Average length of analgesia
(Mean ± SD)
2.29 ± 3.1 2.25 ± 3.8 1.55 ± 4.1 Kruskal-Wallis P ≤ 0.05
Signi cant
Table 2. Comparing the average pain score among the patients applying for curettage in three groups
Group Tramadol Morphine Placebo P-value Statistical test
Pain score in recovery room
(Mean ± SD)
2.35 ± 4.8 3.3 ± 4.2 4.1 ± 5.1 Kruskal-Wallis P ≤ 0.05
Signi cant
Pain score 30 minutes after operation
(Mean ± SD)
2.8 ± 4.1 3.8 ± 4.4 4.45 ± 3.2 Kruskal-Wallis P ≤ 0.05
Signi cant
Pain score 1 hour after operation
(Mean ± SD)
3.6 ± 3.5 4.1 ± 4.2 4.9 ± 4.5 Kruskal-Wallis P ≤ 0.05
Signi cant
in the other two groups, but no statistically signi -
cant difference was observed between tramadol and
morphine groups in terms of post-operation analgesia
(table 1).
Considering P ≤ 0.05, pain score in the recovery room
in the recovery group was much less than what was
observed for the other two groups. On the other hand,
a less pain score was observed for morphine group in
recovery room compared to placebo group. Pain score in
tramadol group 30 minutes after the operation was less
than other groups (P ≤ 0.05). This pain score in morphine
group was also less than placebo group. 1 hour after
the operation, the pain score in tramadol group was less
than other groups (P ≤ 0.05). Again, a lower pain score
was reported in tramadol group compared to what was
observed in other groups. In other words, the pain score
in tramadol group was less than what was observed in
other groups throughout the research (table 2).
As P ≥ 0.05, no statistically signi cant difference was
observed between the three groups in recovery room in
terms of blood pressure, heart rate, and arterial oxygen
saturation levels among mothers applying for curet-
tage. No signi cant difference was observed between
the three groups in terms of post-operation nausea and
occurrence of hypotension after operation (P ≥ 0.05). A
signi cant difference was observed between the three
groups in terms of Bradycardia after operation (P ≤ 0.05)
and the occurrence of Bradycardia in placebo group was
less than what was observed in other two groups.
The present research seeks to study the analgesic
effects of lidocaine mixed with morphine or tramadol
and the cases when only lidocaine is used on creating
analgesia and killing pain after operation. According to
the results of this research, morphine and tramadol had
no in uence on hemodynamic parameters and arterial
oxygen, but they helped cause higher levels of analgesia
than placebo. The average length of analgesia in pla-
cebo group was shorter than other groups. However. No
statistically signi cant difference was observed between
the two groups of tramadol and morphine in terms of
post-operation analgesia.
The pain score in the recovery room in tramadol group
was less than the other two groups. On the other hand,
the pain score in the recovery room in morphine group
was less than placebo. 30 minutes after operation, a lower
pain score was reported in tramadol group compared to
other groups and this score in morphine group was less
than placebo. 1 hour after operation, a lower pain score
was reported in tramadol group compared to other groups
and this score in morphine group was less than placebo.
In other words, the pain score in tramadol group was less
than the other groups throughout the research.
No signi cant difference was observed between the
three groups in terms of the occurrence of post operation
nausea and vomiting and hypotension. However, a sig-
ni cant difference was observed in terms of the brady-
cardia and occurrence of bradycardia in placebo group
was less than the other two groups.
Various researches have pointed to the fact that
sensory signals sent by the injured organs during an
operation stimulate the central nervous system. The
present research focuses on controlling the central
nervous system. For a preventive treatment and con-
trolling environmental sensitivity, Nonsteroidal anti-
in ammatory drugs, local anesthetics and opioids are
utilized and an effective treatment for post operation
analgesia needs to focus on impeding both the central
and environmental sensitivity, Eide et al., (1995). Para
cervical block is accomplished by blocking the sympa-
thetic and parasympathetic sensory bers before then
enter the womb through internal whole. The most com-
mon medicine used for this purpose is lidocaine 1% used
in the 5
th
and 7
th
hour after cervix, Mankowski et al.
(2009).

Alireza Kamali et al.
54 A COMPARATIVE ANALYSIS OF THE INFLUENCE OF ADDING MORPHINE AND TRAMADOL TO LIDOCAINE BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS
The results of this research are in line with the
research conducted by Yektag and Gümüg (2016). They
arrived at the conclusion that prescribing tramadol for
local anesthesia has numerous clinical advantages such
as shorter commencement of sensory and mobile block
and reduction of pain and less need for painkillers and
better conditions during the operation. According to
the data achieved in our research, tramadol exhibited a
lower pain score throughout the research an increased
the analgesic length of patients. Another research con-
ducted by Byrne and Nolan (2016) failed to nd a sig-
ni cant difference between additional morphine and
tramadol. Similar levels of anti-emetics were used in
both groups. No signi cant difference was also observed
in our research in terms of analgesia between the mor-
phine and tramadol groups.
Our results were by no means in line with the research
conducted by Oral and Hanci (2015) in order to compare
the effect of Levobupivacaine tenoxicam tramadol with
Levobupivacaine tenoxicam morphine on post-opera-
tion pain of patients undergoing knee surgery. Vas in
the saline group while the knee was resting or in exion
position was signi cantly more than other groups. The
length of analgesia in groups T and N was signi cantly
longer than saline group. The difference between groups
T and M was signi cant. The number of painkillers
asked and used within 24 hours after operation in mor-
phine group was signi cantly less. Morphine resulted in
a more effective reduction of pain, longer analgesia and
less demand for painkiller compared to using tramadol.
These results are by no means in line with the results of
our research,( Oral and Hanci 2015).
In the research conducted by Thumwadee and Ussanee
(2013), no signi cant evidences were found to show that
para cervical block is better than local anesthesia and
systematic analgesia. The research conducted by Suvaya
et al (2013) failed to nd a signi cant difference in the
pain scores recorded for morphine and tramadol groups.
These results contradict the ndings of our research
where the pain score in tramadol group was shown to
be less. In another research conducted by Jazayeri et al
(2012), the pain score in tramadol and morphine group
was signi cantly less than when these medicines were
not used. Both of these local pain drugs can signi cantly
reduce pain during Arthroscopic knee surgery. Another
research conducted by Thongrong and Jarruwale (2011)
failed to nd a signi cant difference in the pain score
of those patients who had undergone para cervical block
and those receiving intravenous morphine. As a result,
para cervical block can be another alternative to reduce
pain in curettage. The results of our research also point
to the fact that para cervical block can be a good method
to get rid of pain in curettage .
Another research was also conducted by Aslan and
Izde (2009) which showed lidocaine block with mor-
phine or tramadol helps enhance analgesia and sensory
block. These results were in line with our research. A
research conducted by Unlugenc and Vardar (2008)
failed to nd a signi cant difference between morphine,
tramadol and Pethidine groups in terms of pain score
and side effects.
CONCLUSION
As previously mentioned, different studies have found
various results concerning the effects of tramadol and
morphine. These differences may be caused by different
types of surgery, various lengths of operations, selec-
tion of different patients, failing to achieve blindness
in researches and different designs of the research. The
participants studied in this researches were undergoing
the same type of operation and the type of operation
was not a heavy one where the abdominal organs are
exposed; in fact, we studied a light surgery where the
abdominal organs remain intact. The average length of
analgesia in placebo group was less than other groups
but no signi cant difference was observed between
the two groups of tramadol and morphine in terms of
the length of analgesia. Keeping in mind the fact that
patients had no background diseases and the operations
had a limited length, tramadol and morphine seem to
be effective medicines in causing anesthesia and anal-
gesia and reducing pain after operation. In all the times
studied in this research, tramadol exhibited a lower pain
score.
REFERENCES
Abdulkadir Yektag and Funda Gümüg ( 2016) Effects of Addi-
tion of Systemic Tramadol or AdjunctTramadol to Lidocaine
Used for Intravenous Regional Anesthesia in Patients Under-
going Hand Surgery Hindawi Publishing Corporation Anesthe-
siology Research and Practice, Article ID 9161264, 7 .
Aslan B. and Izde S (2009) Comparison of the effects of lido-
caine, lidocaine plus tramadol and lidocaine plus morphine
for intravenous regional anesthesia Agri. 2009 Jan;21(1):22-8.
Bray eld, A. (2013). Tramadol Hydrochloride Martindale: The
Complete Drug Reference. Pharmaceutical Press. Retrieved 5
April 2014.
Eide PK, Stubhaug A, Oye I. (1995) The NMDA-antagonist ket-
amine forprevention and treatment of acute and chronic post-
operative pain Baillie`re’s Clin Anaesthesiol 1995;9:539–54.
Ejlersen, Ellen, Andersen HB, Eliasen K, Mogensen T. A (1992)
A comparison between preincisional and postincisional lido-
caine in ltration and postoperative pain Anesthesia & Analge-
sia 74.4 (1992): 495-498.
¸
s
¸
s
Alireza Kamali et al.
BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS A COMPARATIVE ANALYSIS OF THE INFLUENCE OF ADDING MORPHINE AND TRAMADOL TO LIDOCAINE 55
Gourlay, Geoffrey K., Kwok Rebecca F., K Fentany (1988)
Blood concentration-analgesic response relationship in the
treatment of postoperative pain. Anesthesia & Analgesia 67.4
(1988): 329-337
Kelly Byrne and Aoife Nolan ( 2016) Managing Postoperative
Analgesic Failure: Tramadol Versus Morphine for Refractory
Pain in the Post-Operative Recovery Unit American Academy
of Pain Medicine.
Kingston, J, Charles W. N.(2009) Paracervical Compared With
Intracervical Lidocaine for Suction Curettage: A Randomized
Controlled Trial. Obstetrics & Gynecology 114.4
Mankowski, JL. Kingston J, Moran T, Nager CW, Lukacz ES.
(2009) Paracervical compared with intracervical lidocaine for
suction curettage: a randomized controlled trial. Obstetrics &
Gynecology 113.5 : 1052-1057.
Oral EG and A. Hanci ( 2015) The Analgesic Effects of Mor-
phine and Tramadol Added to Intra-articular Levobupivacaine-
Tenoxicam Combination for Arthroscopic Knee Surgery on
Postoperative Pain; a Randomized Clinical Trial Anesth Pain
Med. 2015 June.
Poornima, C.(2014) Intracervical block compared with intra-
muscular sedation for dilatation and curettage Int J Reprod
Contracept Obstet Gynecol. 3(1): 149-152
Suvaya C., Neves I, Juliana Andrea and Osório Balan (2012)
Comparison of extradural tramadol and extradural morphine
for postoperative analgesia in female dogs undergoing ovario-
hysterectomy Acta Cirúrgica Brasileira - Vol. 27 (4) 12 – 31
Thongrong P and Jarruwale P (2011) Effectiveness of paracer-
vical block versus intravenous morphine during uterine curet-
tage: a randomized controlled trial. J Med Assoc Thai. 2011
Apr.
Thumwadee T. and Ussanee S. (2013) Paracervical local anaes-
thesia for cervical dilatation and uterine intervention Cochrane
Database of Systematic Reviews 2013, Issue 9. Art. No.:
CD005056. DOI10.1002/14651858.CD005056.pub
Unlugenc H. and Mehmet Ali Vardar ( 2008) Comparative
Study of the Analgesic Effect of Patient-Controlled Morphine,
Pethidine, and Tramadol for Postoperative Pain Management
After Abdominal Hysterectomy. Article in Anesthesia and
Analgesia 20 8.