
Dental
Communication
Biosci. Biotech. Res. Comm. 10(3): 518-524 (2017)
Prevalence of osseous changes of the temporomandibular
joint in CBCT images of patients with and without
temporomandibular disorders
Shahriar Shahab
1
, Zeynab Azizi
2
, Farnaz Taghavi Damghani
3
*and Farnoosh Taghavi Damghani
4
1
Assistant Professor, Department of Oral & Maxillofacial Radiology, Shahed Dental School, Tehran, Iran
2
Assistant Professor, Department of Oral & Maxillofacial Radiology, Shahed Dental School, Tehran, Iran
3
Dentist, Shahed Dental School, Tehran, Iran
4
Assistant Professor, Department of Prosthodontics, Shahid Beheshti University of Medical Sciences, Dental
School, Tehran, Iran
ABSTRACT
Radiographic examinations are a part of routine clinical examination of temporomandibular disorders (TMD) to verify degenerative bone
changes in the joint structures. Assessment of the prevalence of osseous changes of the temporomandibular joint (TMJ) in CBCT images
of the patients with and without temporomandibular disorders.CBCT images of temporomandibular joint were taken in 62 patients with
temporomandibular disorders and 62 patients without TMD. The presence of bone changes including attening, erosion, subcortical
sclerosis, osteophyte, subcortical cyst, condylar hyperplasia and condylar hypoplasia of temporomandibular joint were studied at left
and right sides on CBCT images. Furthermore, clinical ndings in relation to temporomandibular disorders in patients were obtained
from their records. The prevalence of bone changes and clinical ndings in the 2 group of patients were analyzed. Radiographic nd-
ings in the right TMJ of TMD patients, included erosion (27.4%), osteophyte (17.7%), subcortical sclerosis (16.1%), condyle hyperplasia
(6.5%) and attening (40.3%). The prevalence of these bone changes in the right TMJ of non-TMD patients were 35.5, 6.5, 3.2, 0 and
37.1%, respectively. In the left side of TMD group; erosion was found in 29.0%, osteophyte 12.9%, subcortical sclerosis 12.9%, condyle
hyperplasia 6.5% and attening in 37.1% of the patients. The incidence of these changes in the same side of non- TMD group was
22.6, 3.2, 1.6, 0 and 32.3%, respectively. Signi cant differences were found for osteophyte incidence in the left TMJ(P=0.04), subcortical
sclerosis in the right TMJ(P=0.02), subcortical sclerosis in the left TMJ(P=0.02) and condylar hyperplasia in both joints (P=0.04) between
TMD and non-TMD patients.The most prevalent bone changes related to temporomandibular disorders included attening, erosion and
osteophyte. The changes were highly reported for temporomandibular disorders than healthy individuals and no signi cant correlation
was found between TMJ bone changes and the patients’ age and gender.
KEY WORDS: BONY CHANGES, CONDYLE, CONE BEAM COMPUTED TOMOGRAPHY, TEMPOROMANDIBULAR JOINT, TEMPOROMANDIBULAR
JOINT DISORDERS
518
ARTICLE INFORMATION:
*Corresponding Author: ftaghavi6@yahoo.com
Received 12
th
June, 2017
Accepted after revision 18
th
Sep, 2017
BBRC Print ISSN: 0974-6455
Online ISSN: 2321-4007 CODEN: USA BBRCBA
Thomson Reuters ISI ESC and Crossref Indexed Journal
NAAS Journal Score 2017: 4.31 Cosmos IF: 4.006
© A Society of Science and Nature Publication, 2017. All rights
reserved.
Online Contents Available at:
http//www.bbrc.in/
DOI: 10.21786/bbrc/10.3/27
Shahriar Shahab et al.
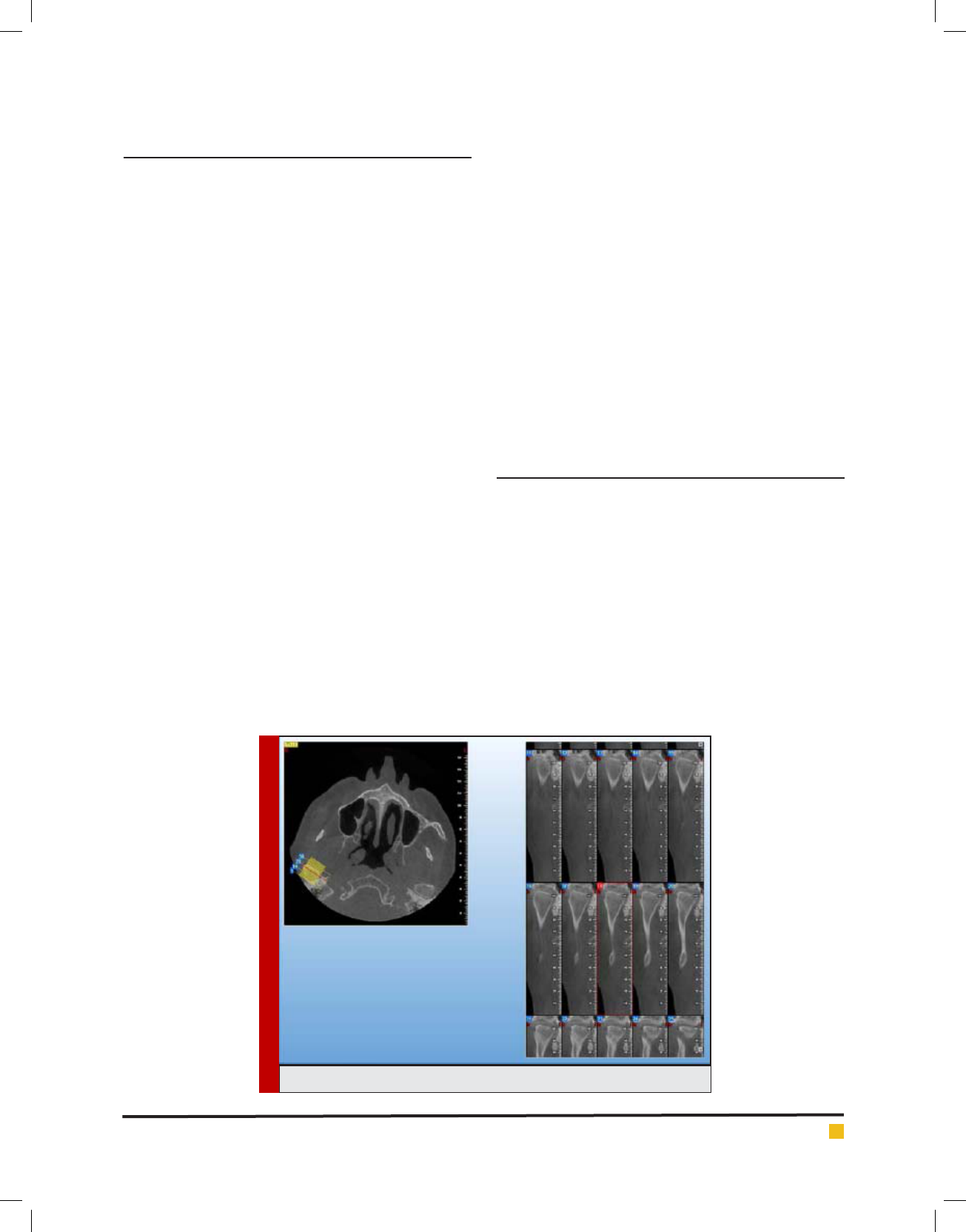
FIGURE 1. CBCT images of the changes in attening
INTRODUCTION
Temporomandibular disorders (TMD) are well de ned
as classi cation of abnormality including masticatory
muscles, osseous and ligamentous components of the
temporomandibular joints (TMJ) and neurological dis-
ease of this complex. The most common clinical signs
of the TMDs are joint and muscle pain, mouth-opening
limitation, crepitation and clicking. TMDs are frequently
associated with degenerative bone changes involving
the bone structures of the temporomandibular joint
(TMJ) including attening, osteophyte, erosion, subcor-
tical sclerosis and pseudocysts, (Dos Anjos Pontual et al.
2012 De Melo et al. 2014, Ladeira et al. 2015 and Kho-
jastepour et al. 2017).
Knowledge about these bone changes is fundamen-
tal for correctly diagnosing the dysfunctions associated
with the disease and for appropriate treatment planning
(Alexiou et al. 2009). Diagnostic procedure in patients
with TMJ disorders includes the background, physical
examination and other diagnostic processes such as
imaging of the TMJ (Ludlow et al. 2008). A panoramic
radiograph is often taken to assess the general condi-
tion of the teeth and structures of the maxilla and the
mandible. To obtain more detailed information about the
bony structures of the TMJ, other radiographs including
computed tomography (CT) scans, and magnetic reso-
nance images (MRI) can be taken which the latter gives
information about the articular disc and the surrounding
soft tissues (Honey et al. 2007). A relatively new imaging
technique is cone-beam computed tomography (CBCT)
and enables 3D imaging of bony structures of the skull,
including the mandible and the TMJ (De Boer et al. 2014
Khojastepour et al. 2017).
The diagnostic accuracy of CBCT in detecting con-
dylar osseous abnormalities was similar to CT images,
while the sensitivity of CBCT in the detection of these
abnormalities was higher (Wiese et al. 2011). The CBCT
is more accurate than panoramic radiographs for the
assessment of bone components of the TMJ (Ladeira et
al. 2015). It is reported that the diagnostic properties of
the CBCT in assessing bony conditions, is better than
other existing imaging techniques. However, to date
limited information exists on the role of CBCT in clinical
decision-making in diagnosis or management of disor-
ders of the TMJ (Krishnamoorthy et al. 2013). So, the
aim of the current study was to determine the prevalence
of osseous changes of the TMJ in CBCT images of the
patients with and without TMD.
MATERIALS AND METHODS
In a descriptive cross-sectional trial, CBCT images of
TMJ in 62 TMD-patients and 62 non-TMD patients
(older than 17 years old) were obtained from 2 radiol-
ogy centers and 3 dental clinics in Tehran, Iran during
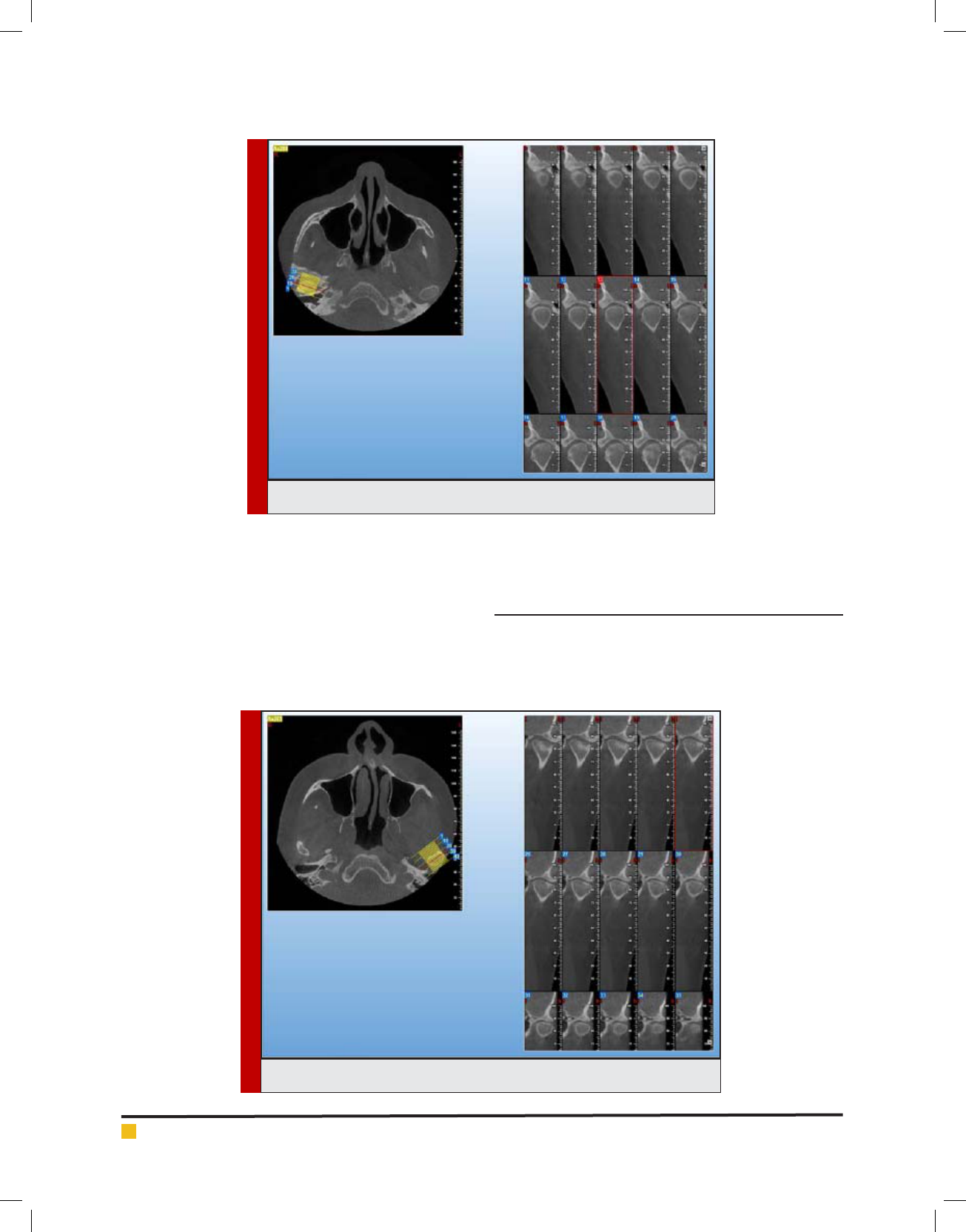
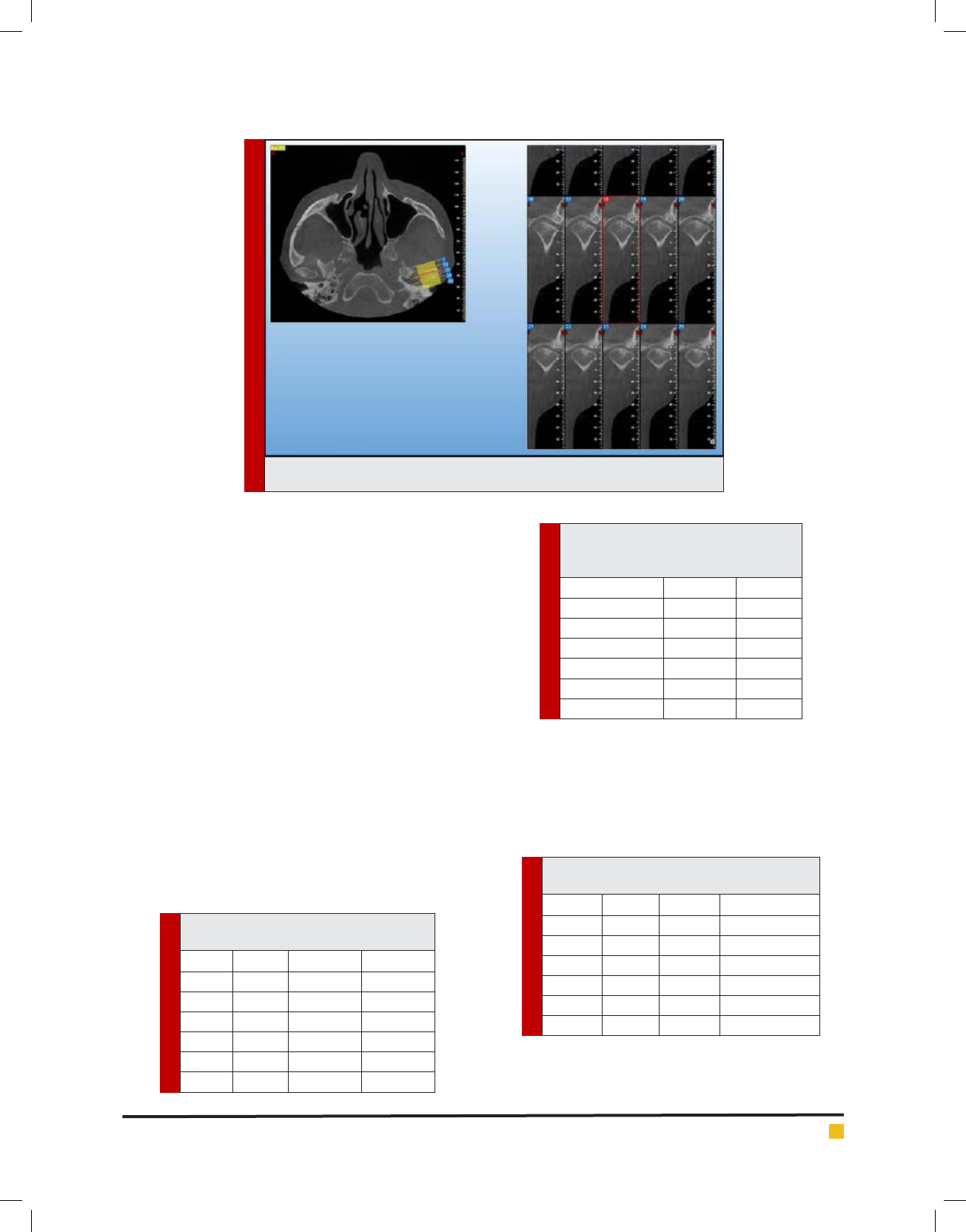
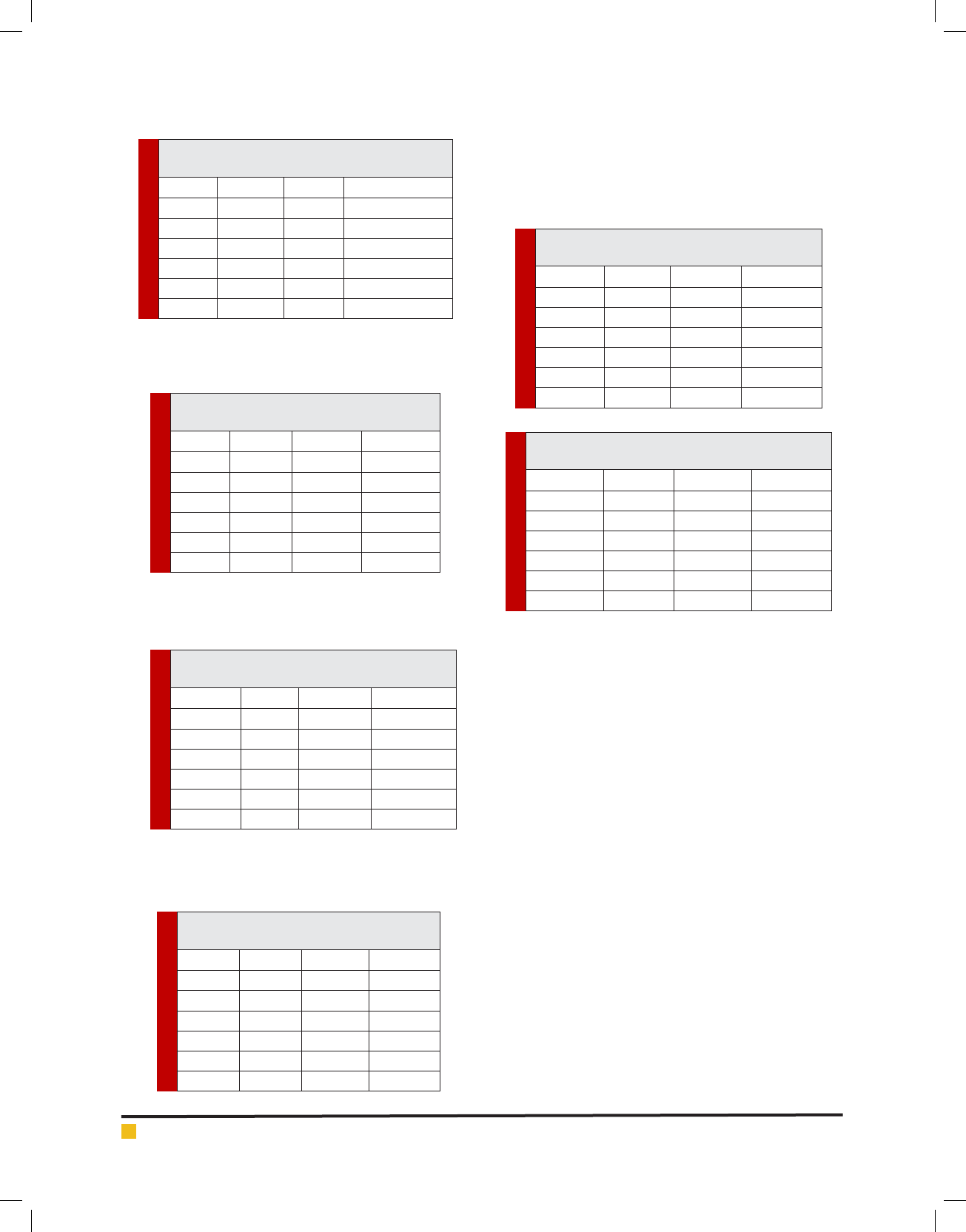
2016-2017. The presence of bone changes of attening,
erosion, subcortical sclerosis, osteophyte, subcortical
cyst, condylar hyperplasia and hypoplasia of TMJ were
studied at left and right sides on CBCT images. In the
TMD group the clinical evidences, and their correlation
with sex and age were determined. The CBCT images
of changes in attening, osteophyte, erosion and sub-
cortical cyst is presented in gures 1-4. Furthermore,
BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS PREVALENCE OF OSSEOUS CHANGES OF THE TEMPOROMANDIBULAR JOINT IN CBCT IMAGES OF PATIENTS 519
Shahriar Shahab et al.
FIGURE 2. CBCT images of the changes in osteophyte
FIGURE 3. CBCT images of the changes in erosion
clinical ndings in relation to TMD in TMD-patients
were obtained from their records. The prevalence of
bone changes and clinical ndings in 2 TMD and non-
TMD patients were analyzed using SPSS statistical soft-
ware ver. 22 by Mann-Whitney U test. The correlation
between bone changes and factors of age and gender
were also determined by Spearman correlation ratio.
P<0.05 was considered as signi cant difference.
The CBCT images of changes in attening, osteophyte,
erosion and subcortical cyst is presented in gures 1-4.
RESULTS AND DISCUSSION
In this study in the right TMJ of TMD-patients; erosion
has been found in 27.4% (17 patients), osteophyte in
17.7% (11 patients), subcortical sclerosis in 16.1% (10
520 PREVALENCE OF OSSEOUS CHANGES OF THE TEMPOROMANDIBULAR JOINT IN CBCT IMAGES OF PATIENTS BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS
BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS PREVALENCE OF OSSEOUS CHANGES OF THE TEMPOROMANDIBULAR JOINT IN CBCT IMAGES OF PATIENTS 521
Shahriar Shahab et al.
FIGURE 4. CBCT images of the changes in subcortical cyst
Table 1. the frequency and percentage of
pain in TMD cases and control patients
Group Sex right left
Male 7 (50%) 5 (35.7%)
Case Female 23 (47.9%) 22 (45.8%)
Total 30 (48.4%) 27 (43.5%)
Male 0 (0%) 0 (0%)
Control Female 0 (0%) 0 (0%)
Total 0 (0%) 0 (0%)
Table 2. the frequency and percentage
of joint tenderness in TMD cases and
control patients
Group Sex right
Male 1 (7.1%)
Case Female 1 (2.1%)
Total 2 (3.2%)
Male 0 (0%)
Control Female 0 (0%)
Total 0 (0%)
Table 3. the frequency and percentage of
muscle tenderness in TMD and control patients
Group Sex right left
Male 1 (7.1%) 1 (7.1%)
Case Female 3 (6.3%) 1 (2.1%)
Total 4 (6.5%) 2 (3.2%)
Male 0 (0%) 0 (0%)
Control Female 0 (0%) 0 (0%)
Total 0 (0%) 0 (0%)
patients), condylar hyperplasia in 6.5% (4 patients) and
attening in 40.3% (25 patients). The prevalence of these
bone changes in the right TMJ of non-TMD patients was
35.5% (22 patients), 6.5% (4 patients), 3.2% (2 patients),
0 and 37.1% (23 patients) respectively.
In the left TMJ of TMD-patients; erosion was reported
in 29.0% (18 patients), osteophyte in 12.9% (8 patients),
subcortical sclerosis in 12.9% (8 patients), condyle
hyperplasia in 6.5% (4 patients) and attening in 37.1%
(23 patients). The incidence of these changes in the left
TMJ of non-TMD patients were also 22.6% (14 patients),
3.2% (2 patients), 1.6% (1 patients), 0 and 32.3% (20
patients), respectively.
Signi cant differences were found regarding osteo-
phyte incidence in the left TMJ (P=0.04), subcortical scle-
rosis in the right TMJ (P=0.02), subcortical sclerosis in the
left TMJ (P=0.02) and condyle hyperplasia in both left and
right TMJs (both: p=0.04) in TMD and non-TMD patients.
As seen in tables 1and 2, in left TMJ pain was reported
in 30 (48.4%) patient and in the right TMJ in 27 (43.5%),
joint tenderness was also observed in 2 (3.2%) patients.
According to table 3, muscle tenderness was observed
in 4 (6.5%) patients at the right side and in 2cases (3.2%)
at left.
The deviation in opening in right and left sides were
detected in 1 (1.6%) and 1 (1.6%) patients, respectively.
522 PREVALENCE OF OSSEOUS CHANGES OF THE TEMPOROMANDIBULAR JOINT IN CBCT IMAGES OF PATIENTS BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS
Shahriar Shahab et al.
Table 4. the frequency and percentage of
deviation in opening in case and control patients
Group Sex right left
Male 0 (0%) 1 (7.1%)
Case Female 1 (2.1%) 0 (0%)
Total 1 (1.6%) 1 (1.6%)
Male 0 (0%) 0 (0%)
Control Female 0 (0%) 0 (0%)
Total 0 (0%) 0 (0%)
Table 5. the frequency and percentage of
limitation in case and control patients
Group Sex right left
Male 4 (28.6%) 4 (28.6%)
Case Female 9 (18.8%) 9 (18.8%)
Total 13 (21%) 13 (21%)
Male 0 (0%) 0 (0%)
Control Female 0 (0%) 0 (0%)
Total 0 (0%) 0 (0%)
Table 6. the frequency and percentage of
clicking in case and control patients
Group Sex right left
Male 5 (35.7%) 5 (35.7%)
Case Female 21 (43.8%) 25 (52.1%)
Total 26 (41.9%) 30 (48.4%)
Male 0 (0%) 0 (0%)
Control Female 0 (0%) 0 (0%)
Total 0 (0%) 0 (0%)
Table 7. the frequency and percentage of
crepitus in case and control patients
Group Sex right left
Male 0 (0%) 0 (0%)
Case Female 1 (2.1%) 3 (6.3%)
Total 1 (1.6%) 3 (4.8%)
Male 0 (0%) 0 (0%)
Control Female 0 (0%) 0 (0%)
Total 0 (0%) 0 (0%)
Table 8. the frequency and percentage of locking
in case and control patients
Group Sex right left
Male 1 (7.1%) 1 (7.1%)
Case Female 2 (4.2%) 2 (4.2%)
Total 3 (4.8%) 3 (4.8%)
Male 0 (0%) 0 (0%)
Control Female 0 (0%) 0 (0%)
Total 0 (0%) 0 (0%)
Table 9. the frequency and percentage of the
subluxation in case and control patients
Group Sex right left
Male 1 (7.1%) 1 (7.1%)
Case Female 13 (27.1%) 14 (29.2%)
Total 14 (22.6%) 15 (24.2%)
Male 0 (0%) 0 (0%)
Control Female 0 (0%) 0 (0%)
Total 0 (0%) 0 (0%)
Limitation in right and left sides was observed in 13
(21%) patients (table 5).
Clicking in right and left sides was detected in 26
(41.9%) and 30 (48.4%) patients, respectively (table 6).
The crepitus occurrence in left and right sides in
patients were 3 (4.8%) and 1 (1.6%), respectively.
The frequency and percentage of locking in both sides
and subluxation in the right side were 3 (4.8%) and 14
(22.6%), respectively. The frequency of the subluxation
in the left side was 15 (24.2%) patients.
The TMJ, which comprises the mandibular condyle,
the inferior component, and the temporal bone form-
ing the superior component, is one of the most complex
joints in the body (Wu et al. 2012). TMDs are clinically
manifested by craniofacial pain in masticatory muscles
and other relevant structures, limited mouth opening,
and click occurring in the TMJ. (Su et al. 2014). Approx-
imately in 60% of the population some type of TMD
including myofascial dysfunction, internal derangement
or degenerative joint disease has been observed. TMD
is epidemic in women between 20 and 40 years old (He
et al., 2010). In the current study, in the right TMJ of
TMD patients, erosion was (27.4%), osteophyte (17.7%),
subcortical sclerosis (16.1%), condylar hyperplasia
(6.5%) and attening (40.3%). The prevalence of these
bone changes in the right TMJ of non-TMD patients
was 35.5, 6.5, 3.2, 0 and 37.1%, respectively. In the left
TMJ of the TMD group; erosion was 29.0%, osteophyte
12.9%, subcortical sclerosis 12.9%, condylar hyperplasia
6.5% and attening was 37.1%. The incidence of these
bone changes in the left TMJ of non-TMD patients was
22.6, 3.2, 1.6, 0 and 32.3%, respectively. Signi cant
differences were found for osteophyte incidence in left
TMJ, subcortical sclerosis in right TMJ, subcortical scle-
rosis in left TMJ and condylar hyperplasia in both joints
between TMD and non-TMD patients. CBCT provides

BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS PREVALENCE OF OSSEOUS CHANGES OF THE TEMPOROMANDIBULAR JOINT IN CBCT IMAGES OF PATIENTS 523
Shahriar Shahab et al.
accurate and reliable linear measurements of the dimen-
sions of the mandible and the TMJ because of its nearly
1:1 reconstruction (Honda et al. 2006).
The diagnostic accuracy of CBCT in detecting corti-
cal erosion of the mandibular condyle is greater than
that of either linear tomography or panoramic radiog-
raphy. Its diagnostic properties in assessing bony con-
ditions, therefore, seem to be similar to, or better than
other imaging techniques (Hilgers et al. 2005). Until now
limited information exists on the role of the CBCT in
clinical decision-making in diagnosis or management of
disorders of the TMJ (Krishnamoorthy et al. 2013). CBCT
has several advantages over CT, such as lower cost, bet-
ter access to equipment, lower radiation, and diagnostic
ef cacy as high as CT(but superior than panoramic radi-
ography and linear tomography) (Barghan et al. 2012).
CBCT better visualizes bony changes than CT in TMD
patients, analyzing lateral slices in isolation and com-
bining coronal and lateral slices (Honey et al. 2007). So,
using CBCT imaging technique to assess condylar bone
changes was considered for this study.
In a research on association between condylar bone
changes revealed in CBCT and clinical dysfunction index
in patients with or without TMD, Khojastepour et al.
(2017) signi cant difference reported for the prevalence
of all types of bone changes between TMD and non-
TMD groups. As well as their report, evaluation of CBCT
images in the present study revealed signi cant differ-
ences between TMD and non-TMD condyles (Khojaste-
pour et al. 2017). In a study by Moshfeghi et al. (2012)
it was reported that Flattening was the most observed
abnormal nding with 16.3% prevalence. Erosion, con-
dylar hyperplasia, concavity, bi d condyle, condylar
hypoplasia and sclerosis were respectively the most
common abnormal ndings in this study. There were
no signi cant differences in the prevalence of abnormal
radiographic ndings regarding to the patient’s gender,
dental status and occlusion, which was in agreement
with our report.
Li et al. (2015) studied the characteristics of TMJ in
patients with TMD complaints and reported that in the
patients with unilateral TMJ pain or joint sounds, the
vertical 60° joint space of the symptomatic side was sig-
ni cantly increased comparing with the asymptomatic
side. It is important to note symptoms of TMJ disorders
may be observed with normal TMJ and vice versa, which
is possibly due to measuring method, age, gender, chew-
ing habits and etc. The condyle and mandibular fossa
might differ in shape in subjects with numerous TMD
complaints, since shape and function are closely related
(Li et al. 2015).
In a similar study, Honey et al. (2007) reported intra
observer reliability was moderate (0.57±0.22; range,
0.34-0.78). Pan-N (0.72±0.15), CBCT (0.65±0.21) and
CBCT reliability was greater than corrected angle linear
tomography. The diagnostic accuracy of CBCT inter-
actively (0.95±0.05) and CBCT statically (0.77±0.17)
was signi cantly greater than all other modalities.
CBCT interactively was also more accurate than CBCT
statically, and Pan-N was more accurate than Pan-TM
and corrected angle linear tomography. CBCT images
provide superior reliability and greater accuracy than
other modalities in the detection of condylar cortical
erosion. The CBCT and spiral CT methods were highly
reliable for evaluation of the bony mandibular con-
dyle. In the several cases, the bone abnormalities of
the autopsy specimens were found with both meth-
ods by carefully analyzing all of the images (Honda et
al. 2006). Being less expensive and with considerably
lower radiation dose in patient examinations, CBCT is
both a cost and a dose-effective alternative diagnostic
method for examination of the bony components of the
TMJ (Honda et al. 2006).
In this regard, Madani et al. (2015) in a recent study
using 34 cases for evaluation of degenerative changes,
condylar position and joint effusion in patients with
TMD via MRI revealed about the condylar position in
the fossa that 32 of the examined joints (47.1%) were in
central position, 30 (44.1%) were in posterior position,
and 6 joints (8.8%) were in the upper position. Moreover,
34 joints (70.8%) had clicks, and 14 joints (70%) didn’t
show clicks or symptoms of osteoarthritis. Following
that, grade-zero and grade-one effusions accounted for
the highest number of examined joints, and there was
no signi cant relationship between effusion volume
and type of clicking. 10 cases (14.7%) had premature
clicks, 20 (29.4%) had intermediate clicks, and 18 joints
(26.5%) had delayed clicks.
Several radiographic methods are used to assess the
TMJ, a eld dif cult to be imaged due to factors like
superimposition of adjacent structures and morpho-
logical variations. The complexity of the TMD however,
demands a clear and precise image of the region for
effective management of the patient. CBCT provides a
de nite advantage over other techniques due to its low
radiation dose to patient, smaller equipment and ability
to provide multi-planar reformation and 3D images and
there are promising researches in the eld of CBCT in
TMJ imaging (Krishnamoorthy et al. 2013).
In conclusion, the most prevalent bone changes
related to TMD included attening, erosion and osteo-
phyte. The changes were highly reported for TMD than
healthy individuals and no signi cant correlation was
found between TMJ bone changes and the patients’ age
and gender. Similar comparative studies are needed to
demonstrate the full spectrum of TMJ articular dysmor-
phology and determine whether the accuracy of CBCT
remains high.

524 PREVALENCE OF OSSEOUS CHANGES OF THE TEMPOROMANDIBULAR JOINT IN CBCT IMAGES OF PATIENTS BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS
Shahriar Shahab et al.
REFERENCES
Alexiou KE, Stamatakis HC, Tsiklakis K.2009 Evaluation of
the severity of temporomandibular joint osteoarthritic changes
related to age using cone beam computed tomography. Den-
tomaxillofacial Radiology 38: 141–147.
Barghan S, Tetradis S, Mallya SM: 2012 Application of cone
beam computed tomography for assessment of the temporo-
mandibular joints. Aust Dent J 57: 109 118
De Boer EWJ, et al. 2014 Value of cone-beam computed
tomography in the process of diagnosis and management of
disorders of the temporomandibular joint. Br J Oral Maxillofac
Surg , http://dx.doi.org/10.1016/j.bjoms.2014.12.007
De Melo DP, Sousa Melo SL, de Andrade Freitas Oliveira LS, de
Moraes Ramos-Perez FM, Flores Campos PS. 2014 Evaluation
of temporo-mandibular joint disk displacement and its cor-
relation with pain and osseous abnormalities in symptomatic
young patients with magnetic resonance imaging. Oral Surg
Oral Med Oral Pathol Oral Radiol :1-6
dos Anjos Pontual ML, Freire JSL, Barbosa JMN, Fraza˜o MAG,
dos Anjos Pontual A, Fonseca da Silveira MM. 2012 Evaluation
of bone changes in the temporomandibular joint using cone
beam CT. Dentomaxillofacial Radiology 41, 24–29.
He SS, Deng X, Wamalwa P, Chen S: 2010 Correlation between
centric relation-maximum intercuspation discrepancy and
temporomandibular joint dysfunction. Acta Odontol Scand 68:
368 376
Hilgers ML, Scarfe WC, Scheetz JP, et al. 2005 Accuracy of lin-
ear temporo-mandibular joint measurements with cone beam
computed tomographyand digital cephalometric radiography.
Am J Orthod Dentofacial Orthop128:803–11.10.
Honda K, Larheim TA, Maruhashi K, et al. 2006 Osseous abnor-
mali-ties of the mandibular condyle: diagnostic reliability of
cone beamcomputed tomography compared with helical com-
puted tomogra-phy based on an autopsy material. Dentomax-
illofac Radiol 35:152–7.9.
Honey OB, Scarfe WC, Hilgers MJ, et al.2007 Accuracy of cone-
beam com-puted tomography imaging of the temporomandib-
ular joint: comparisonswith panoramic radiology and linear
tomography. Am J Orthod Dentofa-cial Orthop 132:429–38.
Khojastepour L, Vojdani M, Forghani M. 2017 The association
between condylar bone changes revealed in cone beam com-
puted tomography and clinical dysfunction index in patients
with or without temporomandibular joint disorders. Oral Surg
Oral Med Oral Pathol Oral Radiol 123:600-605.
Krishnamoorthy B, Mamatha N, Kumar VA. 2013 TMJ imaging
by CBCT:current scenario. Ann Maxillofac Surg 3:80–3.
Ladeira DBS, da Cruz AD, de Almeida SM. 2015 Digital pan-
oramic radiography for diagnosis of the temporomandibu-
lar joint: CBCT as the gold standard. Braz Oral Res [online].
29(1):1-7
Li Y, Guo X, Sun X, Wang N, Xie M, Zhang J, Lv Y, Han W,
Hu M, Liu H. 2015 Characteristics of temporomandibular joint
in patients with temporomandibular joint complaint. Int J Clin
Exp Med 8(9):16057-16063
Ludlow JB, Ivanovic M. 2008 Comparative dosimetry of den-
tal CBCT devicesand 64-slice CT for oral and maxillofacial
radiology. Oral Surg Oral MedOral Pathol Oral Radiol Endod
106:106–14.
Madani A.S., Taheri Heravi M., Imani Moghadam
M., Chamani A., Javan A., Mirmortazavi A.2015 Evalua-
tion of degenerative changes, condyle position and joint effu-
sion in patients with temporomandibular joint disorder via
MRI. Journal of Babol University of Medical Sciences(JBUMS)
17(11):13-20
Moshfeghi M, Amin Tavakoli M, Razaghi Kashani Z, Ra eian
N.2012 Abnormal Temporomandibular Joint radiographic
ndings in patients referred to Department of Oral and Maxil-
lofacial Radiology, Dental School, Shahid Beheshti University
of Medical Sciences. J Dent Sch. 29 (5) :381-389.
Su N, Liu Y, Yang X, Luo Z, Shi Z, 2014 Correlation between
bony changes measured with cone beam computed tomogra-
phy and clinical dysfunction index in patients with temporo-
mandibular joint osteoarthritis, Journal of Cranio-Maxillofa-
cial Surgery doi: 10.1016/ j.jcms.2014.04.001.
Wiese M, Wenzel A, Hintze H 2011 In uence of cross-sectional
temporo-mandibular joint tomography on diagnosis and man-
agement decisionsof patients with temporomandibular joint
disorders. J Orofac Pain 25:223–31.
Wu CK, Hsu JT, Shen YW, Chen JH, Shen WC, Fuh LJ: 2012
Assessments of inclinations of the mandibular fossa by com-
puted tomography in an Asian population. Clin Oral Investig
16: 443 450,