
Medical
Communication
Biosci. Biotech. Res. Comm. 10(3): 455-462 (2017)
Comparison of stress distribution around implants with
three different attachments in overdenture supported by
four maxillary implants using nite element analysis method
Asadallah Ahmadzadeh
1
and Ahmad Teimouri
2
*
1
Assistant Professor, Department of Prosthodontics, School of Dental Medicine, Ahvaz Jundishapur
University of Medical Sciences Ahvaz Iran
2
Assistant Resident, Department of Prosthodontics, School of Dental Medicine, Ahvaz Jundishapur University
of Medical Sciences Ahvaz Iran
ABSTRACT
As a general rule, the purpose of treatment planning should be minimization and evenly distribution of mechanical stress in the
adjacent implant and bone system. Various experimental studies have examined the distribution of stress in the implant supporting
bones, thus avoiding the dangers involved. But there is still controversy about biomechanical effects and stress distribution in differ-
ent attachment designs. The purpose of this study was to compare the distribution of stress around the implant with three different
attachments in overdenture based on four maxillary implants using nite element analysis method (FEA). In this experimental study,
using the FEA method, a 3D model of maxilla, implant, attachment components and overdenture was rst prepared and then, using
the ANSYS nite element software, the components of the model were superimposed on each other so that it can act as a component
integrated with different materials. Implants are located in the anterior and posterior parts of the maxilla, with two implants placed in
the two sides of the canine, one in the left central position and the other in the right second premolar. These implants were attached
to the overdenture using three bar-clip, ball, and locator attachment designs. The 100N force used in this study and imposed verti-
cally to the tooth 6 unilaterally and bilaterally and the stress level was investigated in each design. Among the three different designs
examined, the highest stress was observed in the vertical force (22.87 MPa) imposed on the implant in the right second premolar
on the right overdenture supported by the locator implant. In the second place, the highest stress was observed on the Ball-retained
overdenture in the right side force, imposed on the implant in the right second premolar corresponding to 12.88 MPa. The least stress
among these three designs was observed in the bar-clip-retained overdenture design, the maximum stress on which is in the vertical
force imposed on the right side to the right second premolar implant at the size of 7.486MPa. Bar-clip-retained overdenture with the
lowest stress caused by the 100 N force is the most appropriate design in the present study.
KEY WORDS: FINITE ELEMENT METHOD; STRESS TEST; BAR-CLIP ATTACHMENT; BALL ATTACHMENT; LOCATOR ATTACHMENT; OVERDENTURE
455
ARTICLE INFORMATION:
*Corresponding Author: Dr.ahmad2013@yahoo.com
Received 12
th
July, 2017
Accepted after revision 22
nd
Sep, 2017
BBRC Print ISSN: 0974-6455
Online ISSN: 2321-4007 CODEN: USA BBRCBA
Thomson Reuters ISI ESC and Crossref Indexed Journal
NAAS Journal Score 2017: 4.31 Cosmos IF: 4.006
© A Society of Science and Nature Publication, 2017. All rights
reserved.
Online Contents Available at:
http//www.bbrc.in/
DOI: 10.21786/bbrc/10.3/19
456 COMPARISON OF STRESS DISTRIBUTION AROUND IMPLANTS BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS
Ahmadzadeh and Teimouri
INTRODUCTION
Considering the aging of people in communities and
consequently the increase in complete edentulousness,
today edentulousness has become a public health prob-
lem. Unfortunately, in Iran, edentulousness is not seen
only in the elderly and many young people also suf-
fer from complete edentulousness for a variety of rea-
sons, including systemic diseases, non-compliance with
oral and dental care, and absence of periodic visit to
the dentist. Edentulousness can reduce the quality of
life of patients both physically and psychologically.
Recent studies have shown that tooth loss can affect the
intake and absorption of nutrients due to reduced chew-
ing ability, and increase the risk of multiple diseases.
For this reason, dental implants are used to improve the
chewing ef cacy in complete edentulous patients and
have improved the quality of life of these patients to an
optimum level, (MacEntee etal 2003, Abnet etal., 2005,
Semba etal 2006, Goiato et al 2008, Pennington etal
2012, Cunha etal 2013 Cakir etal 2014, Dezhdar etal
2017 and Geerts 2017).
The treatment that is predominantly performed for
edentulous patients is the use of complete denture hands.
From a public health perspective, although this treat-
ment is a simple and inexpensive treatment, it cannot,
be a general remedy for all patients. One of the main
problems in edentulousness patients is their low satisfac-
tion in denture use. The main reason for this discontent
is poor compliance, inadequate collision, ulceration and
pain (Zarb etal 2004). Considering the problems men-
tioned for ordinary complete dentures, a rational solu-
tion must be sought to the problems. Two types of treat-
ment are widely used for these patients: there are xed
implant supported prostheses and implant-dependent
overdenture that are widely used for complete edentu-
lous patients (Dias et al 2013) and the use of any of
these treatments depends on the patient’s characteristics
and conditions, including the amount of bone remain-
ing, intervertebral space, oral hygiene, cost, and patient
satisfaction (Za ropoulos etal 2010).
Fixed implant-based prostheses may be one of the
best ways to treat edentulousness and are implemented
in case of suf cient bone and mandibular space (Chee
etal 2006). More implants are usually needed to support
a xed prosthesis than an overdenture (Payne etal 2009).
Since it is sometimes impossible to use a large number of
implants for the patient, this issue limits the use of xed
prostheses (Chee et al 2006). Other constraints on the
use of xed prostheses is the loss of facial beauty due to
the lack of lip support and soft tissue face, lack of access
to hygiene, multiple and high cost surgical procedures
(Vogel 2007). Using overdentures has greatly resolved
the problems associated with the use of xed prosthe-
sis. Implant-based overdenture is a moving prosthesis
that is placed on smaller number of implants per jaw,
and has excellent attachment and stability. Overdenture
is a simple, cost-effective, durable, less invasive treat-
ment and a successful treatment option for edentulous
patients and its use has recently become very common
(Assunção et al 2008). Implant-based overdenture has
improved the function of implant therapy (Awad et al
2003) due to the bene ts of physical and natural beauty,
and is superior to conventional dentures in many cases
(Sadowsky 2001). Different studies have shown that this
type of treatment has improved general health and qual-
ity of life of patients (Awad et al 2003). So, although
the patient wants a xed implant-based prosthesis, (s)
he tends to use overdenture. Implant-based overdentures
are connected to the implant by an interstitial part called
attachment, which allows the prosthesis to resist against
displacement forces (Locker 1998).
Many attachments such as rods, buttons, and mag-
nets, are used to support implant-dependent overden-
tures (Machado etal 2011). Clinical success and longev-
ity of dental implants are affected by the distribution of
stress transferred to the implant and surrounding bones
(Jacques et al 2009). Also, the lack of suf cient bio-
compatibility between the implant and the surrounding
bone can lead to implant failure (Berglundh etal 2002).
Different attachment systems used in overdentures show
different biomechanical characteristics and can be dan-
gerous to implant supporting bones (Sadowsky 2007).
Various experimental studies have examined the distri-
bution of stress in the implant supporting bones, thus
avoiding the dangers involved. But there is still contro-
versy about biomechanical effects of stress distribution
in different attachment designs (CHUN etal 2005) and
(Baumeister 1978). Paying attention to the principles of
biomechanics in implant-based prosthesis can provide
a suitable treatment design for each patient and reduce
the probability of functional problems or implant fail-
ure (Baumeister 1978). Different methods are used to
evaluate the stress and strain in the bone around the
implant, which can be used for photoelastic analysis,
strain gauge, and nite element analysis.
Fine Element Analysis (FEA) is a precise method for
evaluating the amount and pattern of stress distribu-
tion in dental structures which has many advantages
over other methods. Precise geometric reconstruction of
the structures involved in stresses acceptance and dis-
tribution, ability to accept and receive different simply,
showing the procedure of internal stresses and other
mechanical quantities, rapid and simple repeatability of
the tests are among the bene ts of this study method.
FEA is a numerical and quantitative method for analyz-
ing stress in complex structures. In this method, sepa-
rate structural elements are connected through points
BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS COMPARISON OF STRESS DISTRIBUTION AROUND IMPLANTS 457
Ahmadzadeh and Teimouri
or nodes. These components are created by dividing the
primary structure into units of the proper shape. For
each element, the physical properties are considered
proportional to the simulated material (Powers 2006).
This method is also used in dental studies as an ideal
method for preparing the correct tooth model and it’s
supporting structures in three dimensional form. This
method can provide measurement of partial mechanical
responses towards the difference in mechanical param-
eters and the evaluation of stress in dental materials and
tissues at different levels (Motta etal 2006). Various stud-
ies, using the FEA method, have shown that stress dis-
tribution in maxillary and mandibular implant systems
is signi cantly affected by various attachment designs
(CHUN et al 2005). The maxillary implant supported-
overdentures are less predictable than mandibular over-
dentures, and there is controversy over the use of dif-
ferent designs and the number of implants used (Dudley
2014). One of the overdenture treatments in maxilla is
the use of four implants, which has been studied in few
studies. There are also few studies on maxillary over-
denture than the mandibular one (Raghoebar etal 2014).
Some studies have shown that 4 or more than 4 max-
illary implant-dependent overdentures are more stable
and more durable than less than 4 implant-dependent
overdentures (Raghoebar etal 2014). These implants can
hold the overdenture with various attachments. Results
of studies on the acceptance and use of various attach-
ments showed that the bar and button attachments that
have a good stability as well as locators that are newer,
are at a higher level in terms of general acceptance and
enjoy more clinical use (Büttel etal 2009) and (Lonc˘ar
2015). For this reason, these attachments will be used in
a four-implant design to measure stress in the present
study. The present study uses a FEA method to simulate
the structure of various overdenture designs based on
four maxillary implants, to investigate the distribution
of Von Mises stress in the surface of all attachments and
implant supporting bones so that the most suitable solu-
tion for the treatment is identi ed.
MATERIAL AND METHODS
The present study is an experimental study in which the
distribution of stress is investigated and compared in
4 maxillary implant-dependent overdentures by FEA
method. In this study, the CBCT-Scan (NewTom VGi;
Finland) of a 30-year-old patient that was available in
the radiology department of Ahwaz Dental Faculty was
used to prepare the Maxilla model. Maxilla data were
imported to the Mimics ver. 8.1.1 for digitalization of
images. After transferring CBCT-Scan data to the Mim-
ics software, other changes were made to this data,
which included deleting the patient’s tooth data from
the initial data. The entire maxilla structure and root
site of the teeth was reconstructed with cortical bone
and 2 mm soft gum tissue was considered on it. The
maxillary bone structure was considered isotopic and
homogeneous, while the elasticity coef cient was lin-
early assumed. The overdenture was constructed on the
maxilla model that was obtained by a 3D printer of the
existing model. It is essential to accurately measuring
the implant for implant modeling. Hence, one specimen
of SPI implant (Thommen Medical, Element, Switzer-
land) with a diameter of 4x12.5 mm was measured by
the Coordinate Measuring Machine (CMM; Mitutoyo-
America Corporation) and the dimensions required for
modeling were used in solid works 2014. In this study,
Ball, Bar-clip, Locator (ThommenMedical, Switzerland)
attachments were used. Overdenture and attachments
were initially measured by CMM and turned into digi-
tal images. The output le of the Mimics software was
imported to the modeling software called Solid Works
(SolidWorks® Of ce Premium 2007 SP, Corporation,
Concord, MA, USA) to turn into a geometric model. Geo-
metric modeling in Solid Work software was performed
automatically based on the surface detail speci ed by
the user. In the above model, implants were placed in
the right second premolar, left and right canine and left
central regions. One 4-mm long locator with housing
with a diameter of 3.6 mm and a height of 2.3 mm was
modeled. Also, ball with a width of 2.2 and a height of
4.3 mm and bar-clip with width and height of 2.2 and
3 mm respectively were modeled. In the Bar design, the
abutment pattern was used and the outside part of the
implant had height of 5.5 mm.
The next step in FEA modeling is to apply appropriate
boundary conditions and loading. For this purpose, the
geometric model was imported to ABAQUS / Standard
software (Version 6.14/1, Pawtucket, IR) for nite analy-
sis. ANSYS software was used to implement FEA mode-
ling. The elements used in this study included SOLID187,
CONTA174 and TARGE170, the rst of which was used
to generate the grid in the geometric model components
and the latter two elements for the attachments. In the
loading stage, the 100N static forces were applied ver-
tically to the center of the rst molar center and the
stress distribution was demonstrated on the surface of
all implant supporting attachments and bones based on
computer graphic forms.
RESULTS AND DISCUSSION
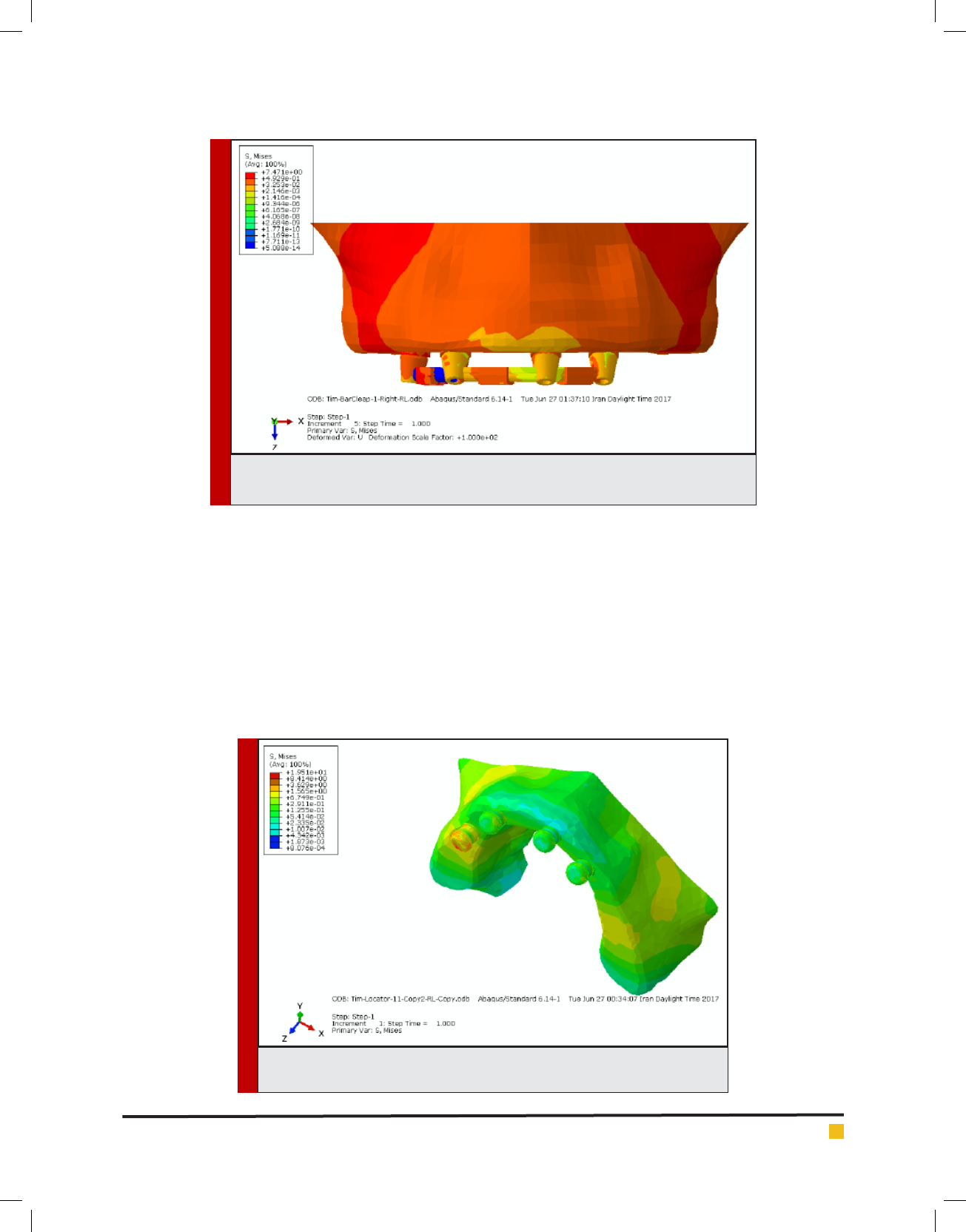
Among the three different designs examined, the high-
est stress was observed in the vertical force (22.87
MPa) imposed on the implant in the right second pre-
molar on the right overdenture supported by the loca-
tor implant. In the second place, the highest stress was
458 COMPARISON OF STRESS DISTRIBUTION AROUND IMPLANTS BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS
Ahmadzadeh and Teimouri
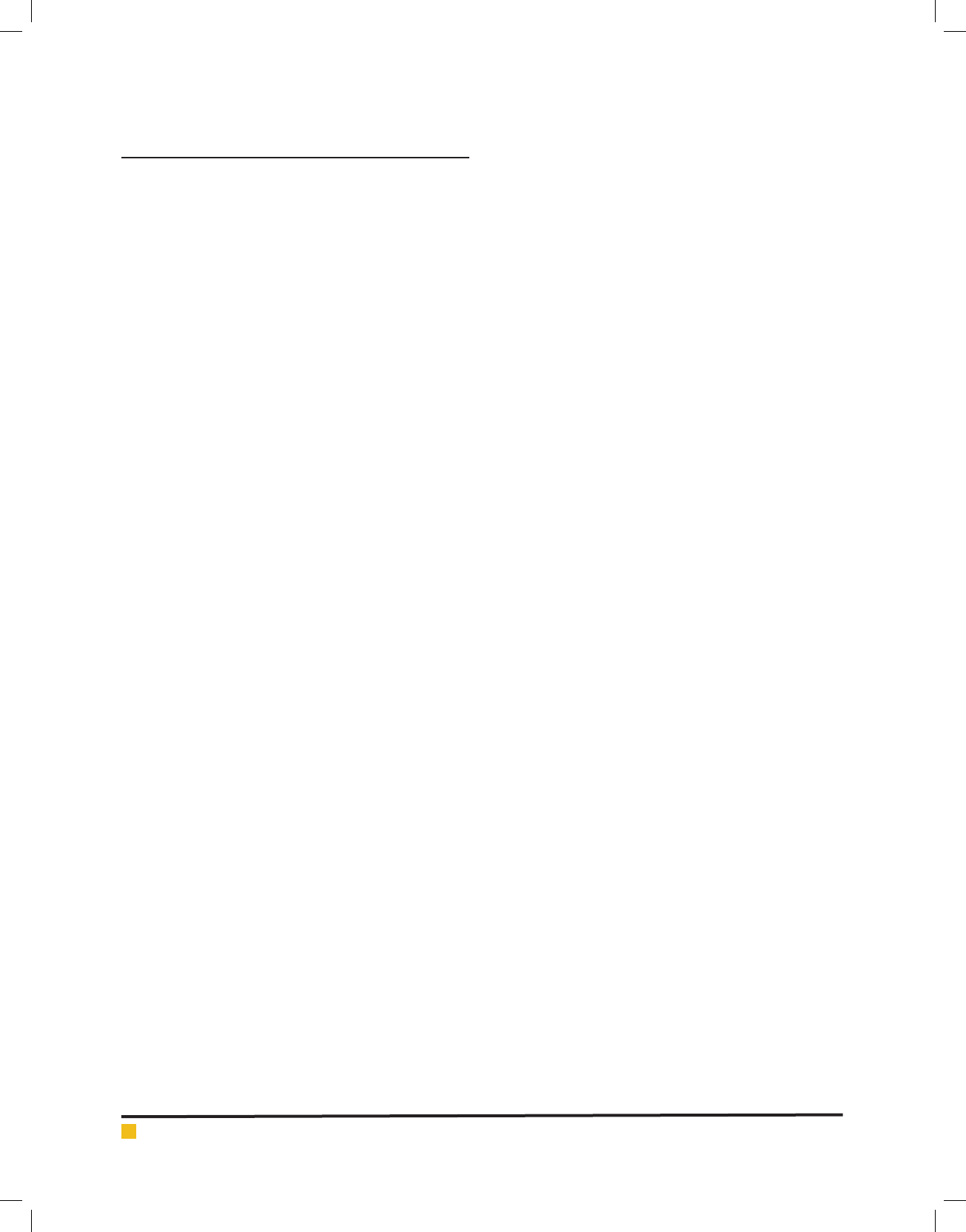
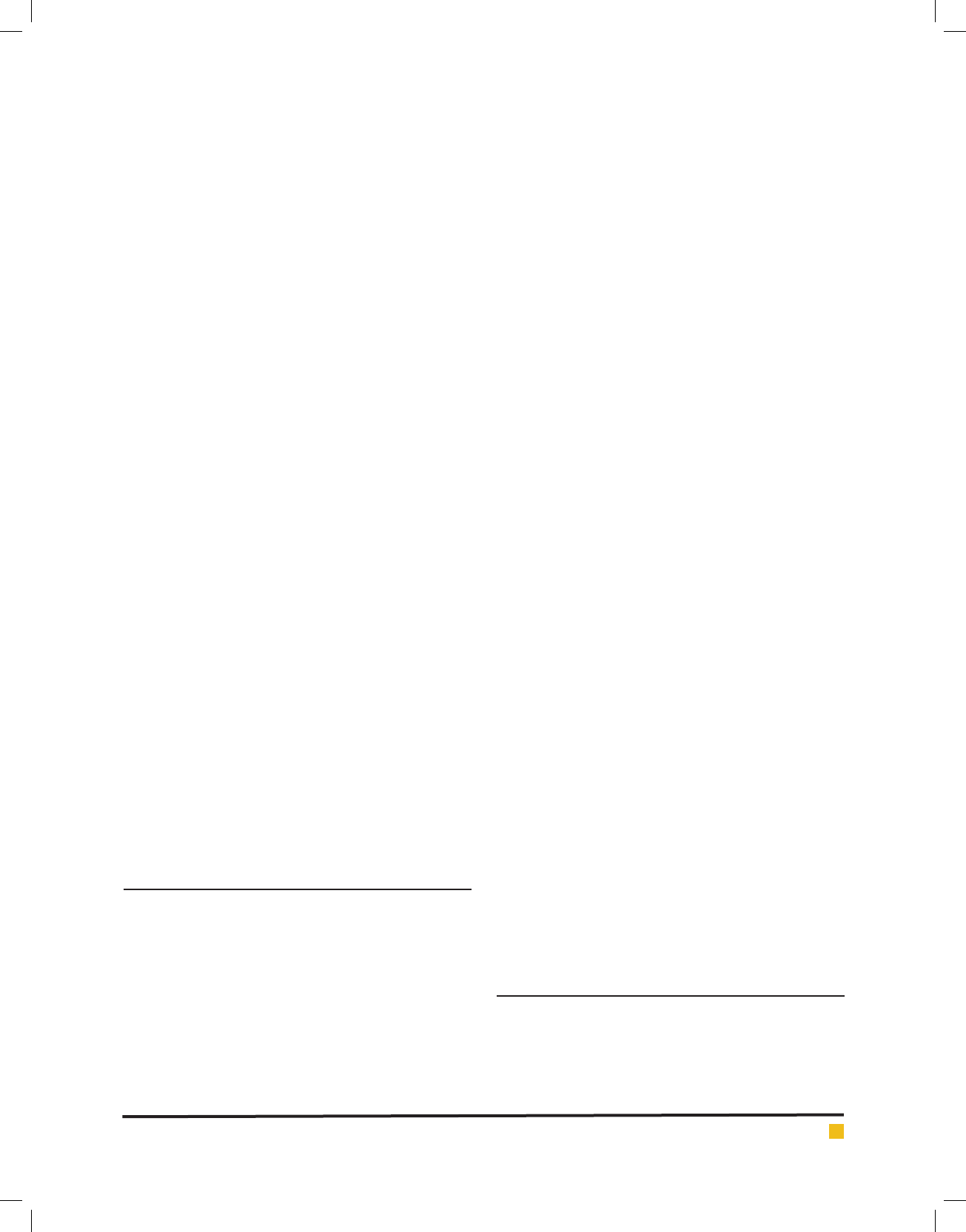
FIGURE 1. Distribution of stress caused by the bilateral force in ball attachment-based
overdenture
FIGURE 2. Distribution of stress caused by the bilateral force in ball attachment-based
overdenture
observed on the Ball-retained overdenture in the right
side force, imposed on the implant in the right second
premolar corresponding to 12.88 MPa. The least stress
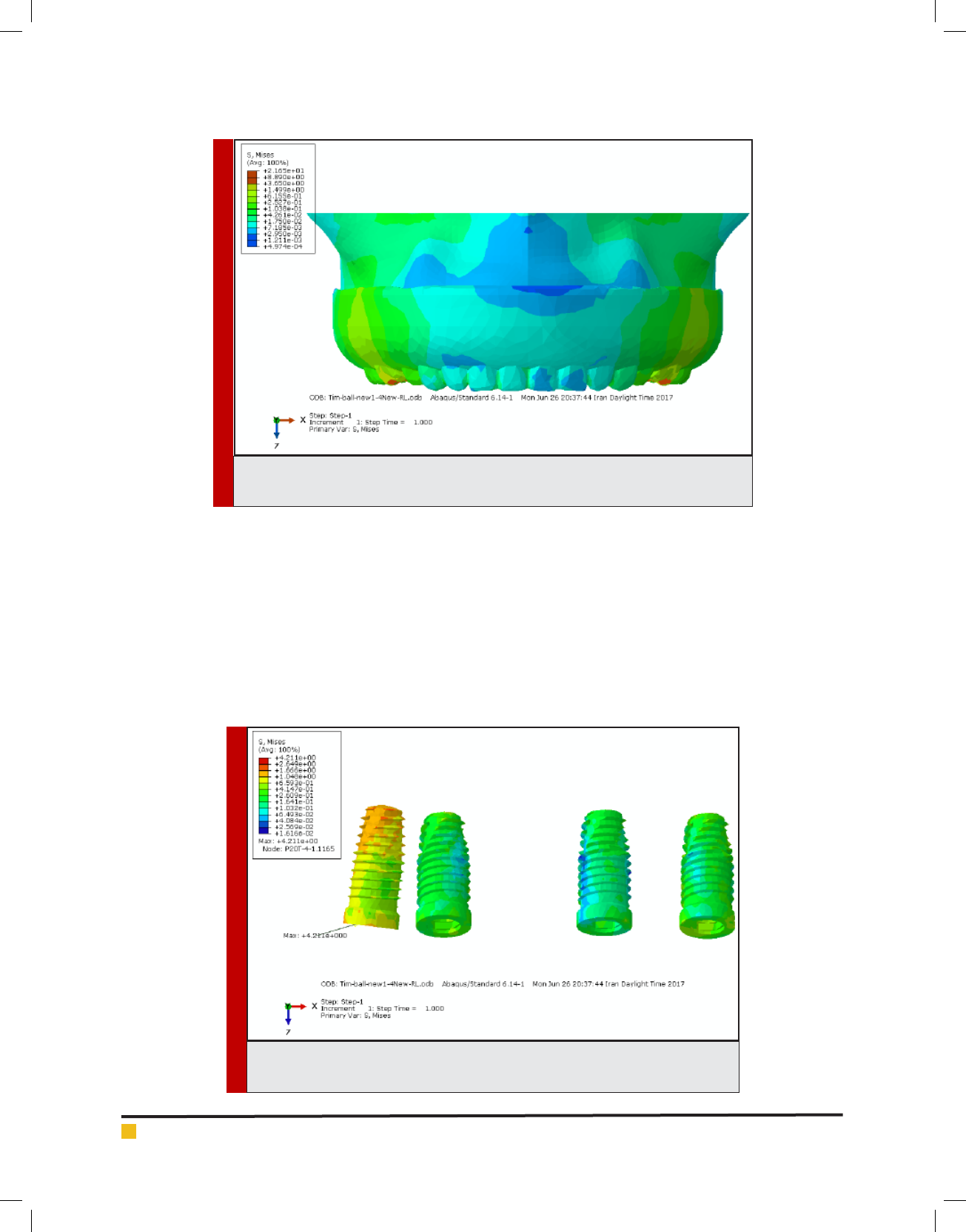
among these three designs was observed in the bar-
clip-retained overdenture design, the maximum stress
on which is in the vertical force imposed on the right
side to the right second premolar implant at the size of
7.486MPa. In the working side of the bone, the most
stress was induced to the nearest implant of the same
side. The results for the highest levels of stress in dense
and sponge bones did not reach the nal bone resorp-
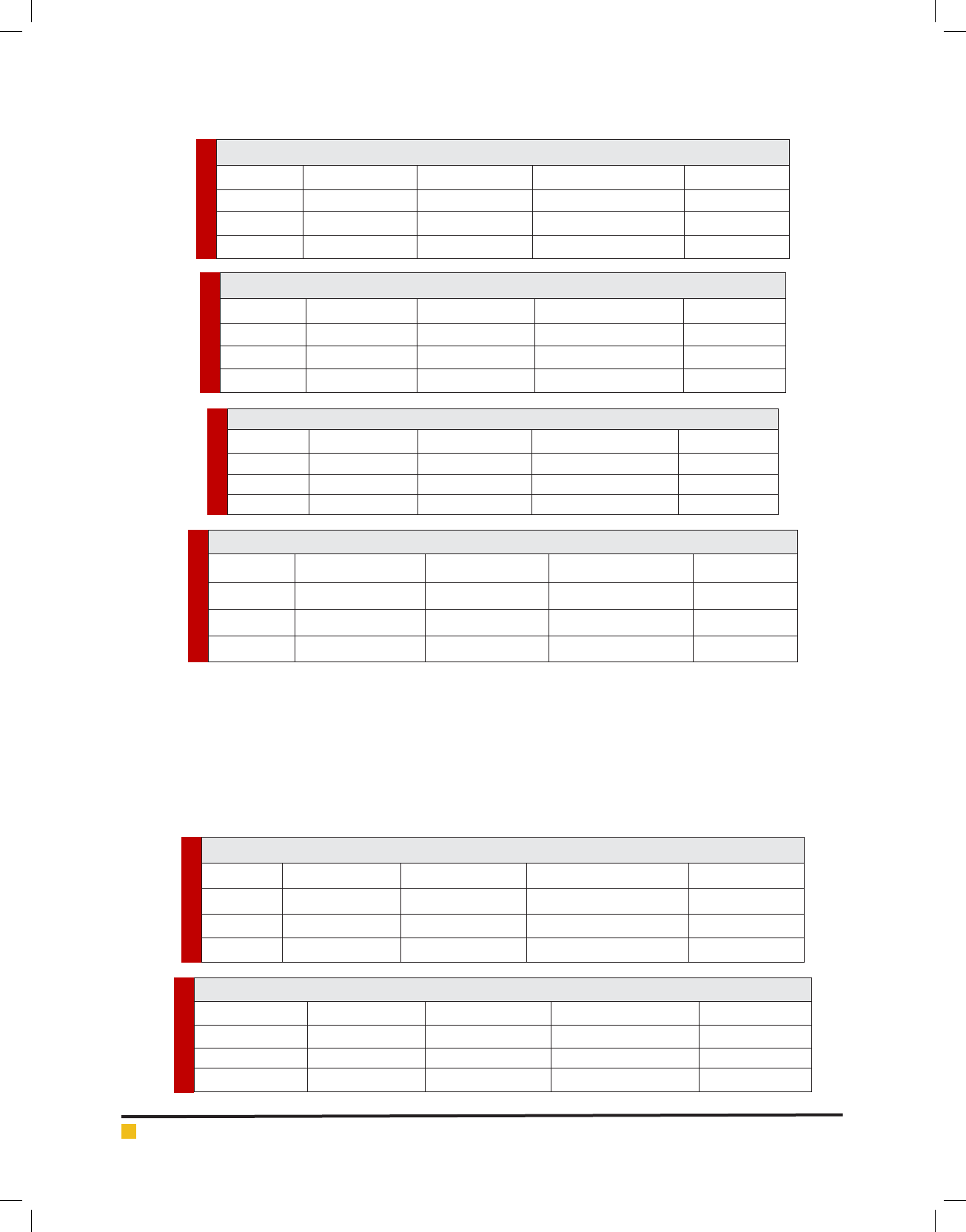
tion in any of the treatment plans (Figures 1 to 4).
Therefore, it can be concluded that overdenture based
on the bar-clip implant with the least stress produced
by the 100 N force, is the most suitable design, and the
ball design has the least stress and is suitable in the
second place (Tables 1 to 6).
In the working side of the bone, the most stress
was imposed to the nearest implant of the same side.
The results for the highest levels of stress in dense and
BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS COMPARISON OF STRESS DISTRIBUTION AROUND IMPLANTS 459
Ahmadzadeh and Teimouri
FIGURE 3. Distribution of stress caused by the bilateral force in bar-clip attachment-based
overdenture
FIGURE 4. Distribution of stress caused by the bilateral force in locator attach-
ment-based overdenture
sponge bones did not reach the ultimate bone resistance
in any of the treatment designs (Figures 1 to 4).
Among the three different attachment designs studied
in this study, the highest bone stress was observed around
the implant of the second right premolar area (working)
where locator attachment was used. In the present study,
the locator attachment was not evaluated using the FEA
method. After the locator attachment, the highest stress
was observed in the bone around the implant of the sec-
ond premolar area (working) using the ball attachment
and the result was consistent with the result of the study
by Chun etal. with the difference that the vertical input
force was 150 N was applied only bilaterally. In the pre-
sent study, vertical forces were applied unilaterally and
bilaterally with the highest concentration of stress in the
working side of the bone near the nearest implant to the
loading site in both cases.
According to the non-uniformity of force distribu-
tion obtained in the study of Mejer et al., the highest
the stress was seen in the working side of the bone and
Ahmadzadeh and Teimouri
460 COMPARISON OF STRESS DISTRIBUTION AROUND IMPLANTS BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS
Table 1. Maximum stress in implants in different treatment designs (Mpa) (bilateral force)
Treatment planRight second premolarTooth right caninTooth Left caninLeft central
Locator1/560/6740/6740/01
Ball0/6150/00710/00710/0071
Bar-clip1/30/0700/0700/070
Table 2. Maximum stress in implants in different treatment designs (MPa) (left force)
Treatment planRight second premolarTooth right caninTooth Left caninLeft central
Locator0/008010/008010/0170/017
Ball0/0400/0750/20330/075
Bar-clip0/0750/0140/32390/014
Table 3. Maximum stress in implants in different treatment designs (MPa) (right force)
Treatment planRight second premolarTooth right caninTooth Left caninLeft central
Locator0/48630/1680/0630/0012
Ball0/32180/1270/1270/0031
Bar-clip1/2020/48630/0310/031
Table 4. Maximum stress in bone around implants in different treatment designs (Mpa) (bilateral force)
Treatment planRight second premolarTooth right caninTooth Left caninLeft central
Locator22/870/0670/0670/067
Ball12/880/00710/00710/0071
Bar-clip7/4860/00780/00780/0078
Table 5. Maximum stress in the bone around the implants in different treatment designs (MPa) (left force)
Treatment planRight second premolarTooth right caninTooth Left caninLeft central
Locator0/36260/1701/4770/170
Ball0/0751/4770/36260/548
Bar-clip0/04037/3650/3230/114
Table 6. Maximum stress in the bone around the implants in different treatment designs (MPa) (right force)
Treatment planRight second premolarTooth right caninTooth Left caninLeft central
Locator22/870/4507/4860/168
Ball12/880/8090/8090/809
Bar-clip7/4860/4860/4500/0315
the nearest implant to the force insertion site, and the
results con rms the consistency of both studies. Accord-
ing to the results, the lowest concentration of stress in
the bone around the implant was observed when load-
clip-based overdenture was used, which is inconsistent
with the results obtained in the study of Menicucci etal.
on two types of ball and bar attachments. They used a
vertical 35N force on the mandibular overdenture, and
the results showed that ball attachment tends to trans-
mit less stress than the bar-clip attachment in the bone
around the implant.
In the present study, the vertical force input was
investigated in maxilla and the resulting difference
requires a review of similar studies in this area. In a

Ahmadzadeh and Teimouri
BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS COMPARISON OF STRESS DISTRIBUTION AROUND IMPLANTS 461
previous study, locator, ball and bar-clip attachments,
respectively, caused the highest amount of stress to the
bone around the implant in maxilla. Valentim et al.
obtained similar results by investigating Ball & Bar,
Ball and Bar attachments in the mandible by apply-
ing a vertical force of 100 N and found that the high-
est stress was fed through the Ball type attachment to
the bone around the implant. In the present study, the
highest level of stress in the bone around the implant
was concentrated in the implant neck region, which
was completely consistent with the results of the pre-
vious studies. In the study of stress in metal parts in
ball attachments, the stress concentration occurred in
the cervical area of the attachment in the 5th tooth
of the right implant area. The stress concentration for
the bar-clip attachment was observed between the 5th
and 3rd tooth right implants. In the locator attachment,
the greatest stress in the housing area of the locator
attachment was entered into the right side of the 5th
tooth. Compared to the different treatment designs, the
stress at the bar-clip attachments was higher than the
other two. It is recommended to use the bar-clip treat-
ment design in some cases where reducing stress in the
bone around the implant is more important than over-
denture stability and stress in the metal parts. If there
is no necessity in these cases, you can use the Ball and
Locator treatment designs as needed.
The greatest amount of bone stress in all treatment
designs was concentrated in the cervical implants in the
working side and a few upper threaded implants, and
the stress rate didn’t reach to the ultimate bone strength
in any of the treatment designs, thus, it seems that bone
resorption will not occur in any none of the treatment
designs. In clinical situations where overdenture is
expected to undergo lot of force, it is recommended to
use the Bar-Clip treatment design because less stress is
transmitted to the bone around the implant. The maxi-
mum stress induced in the implant-based overdenture
model was observed in the locator attachment, and the
implant overdenture supported by the Bar-clip attach-
ment with less stress was the most appropriate design
for the present study.
REFERENCES
Abnet, C.C., Qiao, Y.L., Dawsey, S.M., Dong, Z.W., Taylor, P.R.
and Mark, S.D., 2005. Tooth loss is associated with increased
risk of total death and death from upper gastrointestinal cancer,
heart disease, and stroke in a Chinese population-based cohort.
International journal of epidemiology, 34(2), pp.467-474.
Assunção, W.G., Tabata, L.F., Barao, V.A.R. and Rocha, E.P.,
2008. Comparison of stress distribution between complete den-
ture and implant‐retained overdenture‐2D FEA. Journal of oral
rehabilitation, 35(10), pp.766-774.
Awad, M.A., Lund, J.P., Shapiro, S.H., Locker, D., Klemetti, E.,
Chehade, A., Savard, A. and Feine, J.S., 2003. Oral health sta-
tus and treatment satisfaction with mandibular implant over-
dentures and conventional dentures: a randomized clinical
trial in a senior population. International Journal of Prostho-
dontics, 16(4).
Baumeister, T., 1978. Standard Handbook for Mechanical Engi-
neer. McGraw-Hill Interamericana.
Berglundh, T., Persson, L. and Klinge, B., 2002. A systematic
review of the incidence of biological and technical complica-
tions in implant dentistry reported in prospective longitudinal
studies of at least 5 years. Journal of clinical periodontology,
29(s3), pp.197-212.
Bilhan, H., Mumcu, E. and Arat, S., 2011. The comparison of
marginal bone loss around mandibular overdenture‐support-
ing implants with two different attachment types in a loading
period of 36 months. Gerodontology, 28(1), pp.49-57.
Büttel, A.E., Bühler, N.M. and Marinello, C.P., 2009. Locator
or ball attachment: a guide for clinical decision making. Sch-
weizer Monatsschrift fur Zahnmedizin= Revue mensuelle sui-
sse d’odonto-stomatologie= Rivista mensile svizzera di odon-
tologia e stomatologia, 119(9), pp.901-918.
Cakir, O., Kazancioglu, H.O., Celik, G., Deger, S. and Ak, G.,
2014. Evaluation of the ef cacy of mandibular conventional
and implant prostheses in a group of Turkish patients: A qual-
ity of life study. Journal of Prosthodontics, 23(5), pp.390-396.
Chee, W. and Jivraj, S., 2006. Treatment planning of the eden-
tulous mandible. British dental journal, 201(6), p.337.
Chun, H.J., Park, D.N., Han, C.H., Heo, S.J., Heo, M.S. And Koak,
J.Y., 2005. Stress distributions in maxillary bone surrounding
overdenture implants with different overdenture attachments.
Journal of oral rehabilitation, 32(3), pp.193-205
Cunha, T.R., Della Vecchia, M.P., Regis, R.R., Ribeiro, A.B.,
Muglia, V.A., Mestriner, W. and De Souza, R.F., 2013. A ran-
domised trial on simpli ed and conventional methods for
complete denture fabrication: masticatory performance and
ability. Journal of dentistry, 41(2), pp.133-142.
Dezhdar, S., Fereidoonpoor, N., Mostaghni, E., Jahanpour, F.
and Ravanipour, M., 2017. Transition from being OK to NOT
OK with tooth loss among a selection of older people in Iran: a
qualitative study. Gerodontology, 34(2), pp.215-226.
Dias, R., Moghadam, M., Kuyinu, E. and Jahangiri, L., 2013.
Patient satisfaction survey of mandibular two-implant–
retained overdentures in a predoctoral program. The Journal
of prosthetic dentistry, 110(2), pp.76-81.
Dudley, J., 2014. The 2-implant maxillary overdenture: A clini-
cal report. The Journal of prosthetic dentistry, 112(2), pp.104-
107.
Geerts, G.A., 2017. Neutral zone or conventional mandibular
complete dentures: a randomized cross‐over trial comparing
oral‐health related quality of life. Journal of Oral Rehabilita-
tion.
Goiato, M.C., Ribeiro, P.P., Garcia, A.R. and Dos Santos, D.M.,
2008. Complete denture masticatory ef ciency: a literature

Ahmadzadeh and Teimouri
462 COMPARISON OF STRESS DISTRIBUTION AROUND IMPLANTS BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS
review. Journal of the California Dental Association, 36(9),
pp.683-686.
Jacques, L.B., Moura, M.S., Suedam, V., Souza, E.A.C. and
Rubo, J.H., 2009. Effect of cantilever length and framework
alloy on the stress distribution of mandibular‐cantilevered
implant‐supported prostheses. Clinical oral implants research,
20(7), pp.737-741.
Locker, D., 1998. Patient-based assessment of the outcomes of
implant therapy: a review of the literature. International Jour-
nal of Prosthodontics, 11(5).
Lon
c
˘
ar, B., 2015. Konfekcijski pri
ˇ
c
vrsni sustavi pokrovnih pro-
teza nošenih implantatima (Doctoral dissertation, University of
Zagreb. School of Dental Medicine. Department of Removable
Prosthodontics.).
MacEntee, M.I., 2003. The impact of edentulism on function
and quality of life. Implant overdentures as the standard of
care for edentulous patients. Chicago: Quintessence Interna-
tional, pp.23-8.
Machado, A.C.M., Cardoso, L., Brandt, W.C., Henriques, G.E.P.
and de Arruda Nóbilo, M.A., 2011. Photoelastic analysis of the
distribution of stress in different systems of overdentures on
osseous-integrated implants. Journal of Craniofacial Surgery,
22(6), pp.2332-2336.
Motta, A.B., Pereira, L.C. and da Cunha, A.R., 2006. Finite ele-
ment analysis in 2D and 3D models for sound and restored
teeth. In 2006 ABAQUS conference. ABAQUS Inc (pp. 329-43).
Payne, A., Walton, J., Alsabeeha, N., Worthington, H.V. and
Esposito, M., 2009. Interventions for replacing missing teeth:
attachment systems for implant overdentures in edentulous
jaws. The Cochrane Library.
Pennington, J. and Parker, S., 2012. Improving quality of life
using removable and xed implant prostheses. Compendium
of continuing education in dentistry (Jamesburg, NJ: 1995),
33(4), pp.268-70.
Powers, J.M. and Sakaguchi, R.L., 2006. Impression materials.
Craig’s Restorative Dental Materials, 12, pp.269-312.
Raghoebar, G.M., Meijer, H.J., Slot, W., Slater, J.J. and Vissink,
A., 2014. A systematic review of implant-supported overden-
tures in the edentulous maxilla, compared to the mandible:
how many implants. Eur J Oral Implantol, 7(Suppl 2), pp.S191-
S201.
Sadowsky, S.J., 2001. Mandibular implant-retained overden-
tures: a literature review. The Journal of prosthetic dentistry,
86(5), pp.468-473.
Sadowsky, S.J., 2007. Treatment considerations for maxillary
implant overdentures: a systematic review. The Journal of
prosthetic dentistry, 97(6), pp.340-348.
Semba, R.D., Blaum, C.S., Bartali, B. and Xue, Q.L., 2006.
Denture use, malnutrition, frailty, and mortality among older
women living in the community. The journal of nutrition,
health & aging, 10(2), p.161.
Slot, W., Raghoebar, G.M., Vissink, A. and Meijer, H.J., 2013.
Maxillary overdentures supported by four or six implants in the
anterior region; 1‐year results from a randomized controlled
trial. Journal of clinical periodontology, 40(3), pp.303-310.
Vogel, R.C., 2007. Implant Overdentures: A New Standard of
Care for Edentulous Patients.
Za ropoulos, G.G. and Hoffman, O., 2010. Implant-retained
dentures for full-arch rehabilitation: a case report compar-
ing xed and removable restorations. General dentistry, 59(4),
pp.e137-43.
Zarb, G.A., Bolender, C.L., Eckert, S.E., Fenton, A.H., Jacob,
R.F. and Mericske-Stern, R., 2004. Prosthodontic treatment for
edentulous patients. Mosby.