
Medical
Communication
Biosci. Biotech. Res. Comm. 10(3): 341-345 (2017)
Assessment of short term prognosis in patients with
upper gastrointestinal bleeding
Saeid Hashemieh (MD)
1
, Ramtin Moradi (MD)
2
, Davood Karimi Hosseini (MD)
3
and
Habib Malek Pour (MD)
1
*
1
Department of Internal Medicine, Shahid Beheshti University of Medical Sciences
2
Mashhad Azad University School of Medicine
3
Stanford University School of Medicine, Palo Alto, CA, USA
ABSTRACT
Upper gastrointestinal bleeding (UGIB) is a medical emergency. There is no precise information of its prevalence
and prognosis in patients. The aim of present study was to investigate the prognostic factors of UGIB in patients. In
this prospective observational study 75 patients with UGIB referred to Hospital. Demographic and clinical data of
them were recorded and analyzed. Mortality rate in rst hospitalization was 16% and in one-month follow up was
4%. There was no signi cant association between age and gender with duration of hospitalization and one-month
prognosis (p>0.05). Mortality was associated with acute abdomen and orthostatic hypotension I admission time, pep-
tic ulcer in endoscopic evaluation, active bleeding, ICU admission and need to second endoscopy (p<0.05). Erosive
gastritis, need to emergent surgery and use of NSAIDs signi cant increase of mortality rate (p<0.05). It seems admis-
sion time signs and symptoms, hemodynamic and coagulation status, endoscopic results and need to re-endoscopic
evaluation are more prognostic factors in patients with UGIB.
KEY WORDS: SHORT TERM PROGNOSIS, UPPER GASTROINTESTINAL, BLEEDING
341
ARTICLE INFORMATION:
*Corresponding Author:
Received 27
th
June, 2017
Accepted after revision 27
th
Sep, 2017
BBRC Print ISSN: 0974-6455
Online ISSN: 2321-4007 CODEN: USA BBRCBA
Thomson Reuters ISI ESC and Crossref Indexed Journal
NAAS Journal Score 2017: 4.31 Cosmos IF: 4.006
© A Society of Science and Nature Publication, 2017. All rights
reserved.
Online Contents Available at:
http//www.bbrc.in/
DOI: 10.21786/bbrc/10.3/1
INTRODUCTION
The UGIB bleeding occurs frequently and is a common
cause of hospitalization or inpatient bleeding. Such
bleeding results in substantial patient morbidity, mor-
tality and healthcare expense. Ulcer disease is the most
common cause of severe UGIB, causing about 40-50%
of cases and UGIB is the most common complication of
peptic ulcer disease (Kovacs and Jensen, 2008). The ini-
tial management of the patient with UGIB should include
evaluation of severity of the hemorrhage, patient resusci-
tation, a brief medical history and physical examination,
342 ASSESSMENT OF SHORT TERM PROGNOSIS IN PATIENTS WITH UPPER GASTROINTESTINAL BLEEDING BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS
Saeid Hashemieh et al.
and consideration of possible interventions (Lin et al.
2005). This lack of evidence is re ected in the literature.
In databases and in product monographs for corticoster-
oids, peptic ulcer disease and GI bleeding may or may
not be described as possible adverse effects (de Abajo
etal. 2013).
GI bleeding, bleeding peptic ulcer and perforation
are feared complications of peptic ulcer disease, associ-
ated with considerable morbidity and mortality (Lanas
etal. 2011). In clinical recommendations, an association
between corticosteroid use and peptic ulcer has been
described as unlikely, and the value of antiulcer prophy-
laxis has been questioned due to a low bleeding risk
(Martinek etal. 2011). Non-steroidal anti-in ammatory
drugs (NSAID) use and Helicobacter pylori infection are
the most important risk factors for peptic ulcer disease.
Bleeding or perforation is also seen as complications to
stress ulcers among patients with critical illness in inten-
sive care units. GI bleeding and perforation are assumed
to occur when ulcers erode into underlying vessels (Hal-
liday etal. 2010). It is reported a high late as well as early
mortality for upper GI bleeding, with very poor longer
term prognosis following bleeding due to malignancies
and varices. Aetiologies with the worst prognosis were
often associated with high levels of social deprivation
(Roberts etal. 2012).
The aetiology of hemorrhage can be broadly con-
sidered to be non-variceal or variceal in origin. In the
upper gastrointestinal haemorrhage accounts for85%
of presentations, the major causative lesion being pep-
tic ulcer disease, followed by erosive diseases such as
oesophagitis, gastritis and duodenitis (Jairath & Barkun,
2012). Risk factors for developing upper gastrointesti-
nal hemorrhage include old age, socio-economic disad-
vantage, co-morbidities such as chronic renal disease,
Helicobacter pylori infection and several pharmaceuti-
cal agents including NSAIDS, aspirin, cyclo-oxygenase
(COX) 2 inhibitors and anticoagulants. The remaining
presentations (10–15%) are secondary to variceal hem-
orrhage in patients with liver cirrhosis (Holcomb etal.
2015).
Coagulopathy exacerbates bleeding and should be
corrected with blood products. Massive bleeding man-
dates emergency endoscopy. Emergency endoscopy
is performed as soon as the patient is stabilized after
initial resuscitation. In patients with exigent bleed-
ing, endoscopy can be performed during resuscitation
(Button et al. 2011). Local studies indicate that as the
incidence of upper GI bleeding has increased over time
(Hearnshaw et al. 2010). There is also current interest
in whether prognosis for emergency disorders varies
according to the day of admission, the size of hospi-
tal and the distance travelled to hospital although lit-
tle has been reported about these for upper GI bleed-
ing (Shaheen etal. 2009). So, the main objective of this
study was to establish short term prognosis in patients
with UGI bleeding in 1 month follow-up period.
MATERIAL AND METHODS
This prospective observational study was done to assess
short term prognosis in 75 patients with upper gastro-
intestinal bleeding referred to the Imam Husein Hospita,
(Tehran, Iran) during the 2015-16. The demographic
information was collected using check list based on
patient’s background, Para clinic information, hos-
pitalization and follow-up data. Correlation between
sex, gender, age, disease and medication background,
gastrointestinal disorder, smoking or alcohol drinking,
blood factors (hemoglobin, PT, PTT, INR and platelet)
and endoscopic ulceration are determined at the arrival
and after 1 month. Data is analyzed by repeated measure
one-way analysis of variance (ANOVA) using SPSS 16.0
for Windows (SPSS, Inc., Chicago, IL, USA). For treat-
ment showing a main effect by ANOVA, means com-
pared by Tukey–Kramer test. P<0.05 was considered as
signi cant differences between treatments.
RESULT AND DISCUSSION
As seen in the current study, among 75 patients, 54 male
(72%) and 21 women (28%) were include into the study.
The mean age of the patients was 61.2 ± 18.6 years old
(P=0.4).in this study, 37 (49.3%) had hematoma while 46
(61.3%) had melena, 11 (14.7%) Hematochezia and 27
(36%) with active bleeding were referred to the hospi-
tal. In the initial investigation the mean blood pressure
and diastolic pressures were 116.1±19.2 and 69.8±23.4
mmHg, respectively. Mean heart rate was 81.2±27.7/
min. the clinical results of the patients included into the
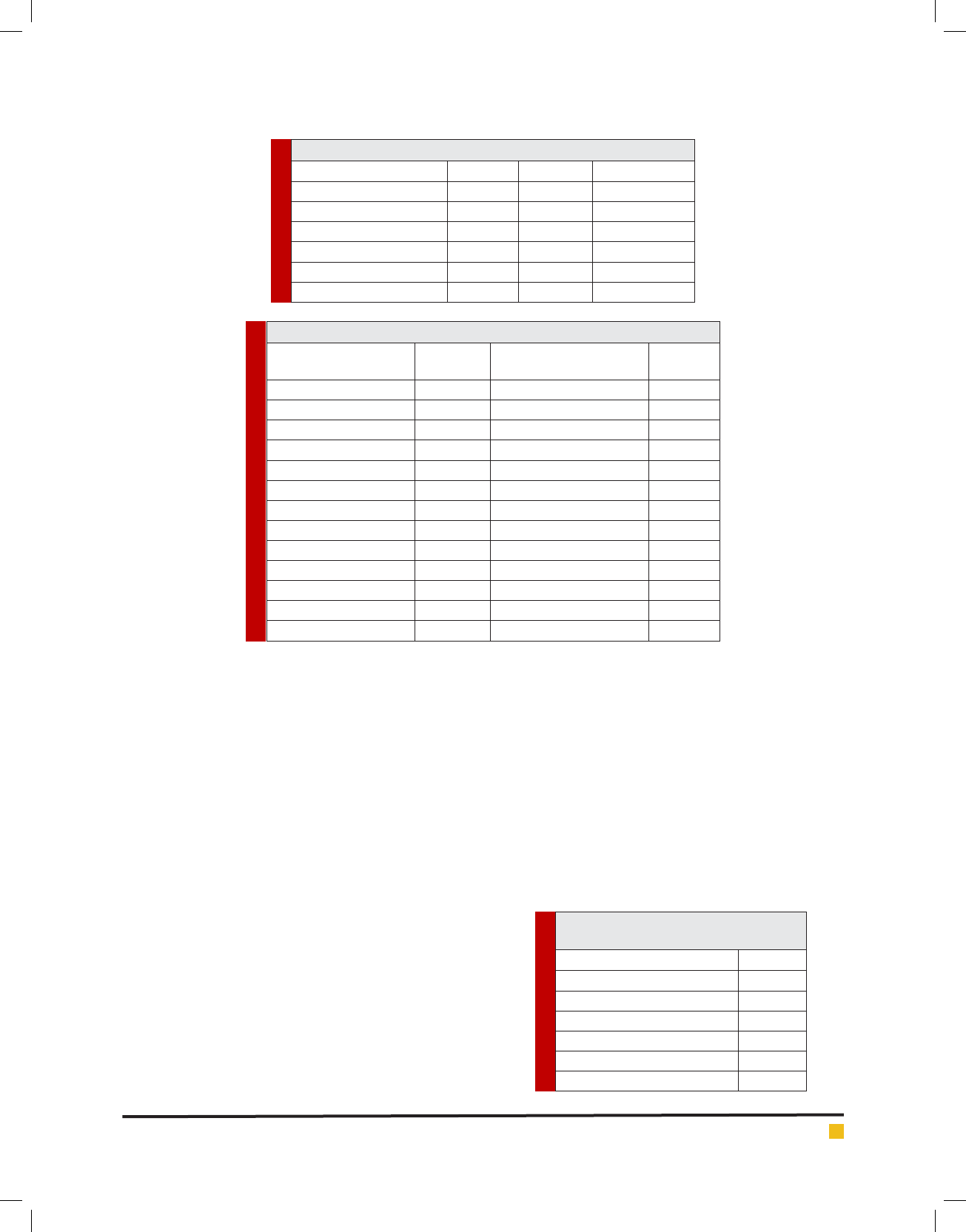
study is presented in table 1. According to the data, the
man HB at the beginning and end of the study were 9.3
± 2.9 and 9.8 ± 2.01 mg/dl, respectively. The mean PT,
PTT and INR were 14.7 ± 8.7, 31.9 ± 25.2 and 1.5 ± 1.4,
respectively.
The patient’s distribution based on disease back-
ground is presented in table 2. According to the data,
Hypertension and Cardiovascular disease were the most
frequent among them. Also, ulcer was the prominent
digestive disease 27 (36%). For family background for
gastrointestinal disease, GI cancer 4 (5.3%) was the most
report.
Based on the endoscopic observation, clean base
and gastritis were the more problem 23 (30.7%) and 22
(29.3%) in the patients.
In this study, 4 patients (5.3%) needed for urgency
surgery and 33 (44%) for packed cell. During the study,
BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS ASSESSMENT OF SHORT TERM PROGNOSIS IN PATIENTS WITH UPPER GASTROINTESTINAL BLEEDING 343
Saeid Hashemieh et al.
Table 1. The clinical results of the patients included into the study
Factor Minimum Maximum Mean ± Sd
Hb (at arrival) (mg/dl) 2.9 16 9.3 ± 2.9
Hb (after treatment) (mg/dl) 6.8 15.7 9.8 ± 2.01
PT 1.3 50 14.7 ± 8.7
PTT 1 120 31.9 ± 25.2
INR 1 9.3 1.5 ± 1.4
Platelet 31500 479000 213200 ± 111800
Table 2. The patients distribution based on disease background
Factor
N (%)
Family background for
Gastrointestinal disease
N (%)
Disease background Ulcer 2 (2.7)
Diabetes 31 (41.3) Gastrointestinal cancer 4 (5.3)
Hyperlipidemia 17 (22.7) Intestinal ulcers 2 (2.7)
Hypertension 41 (54.7) Medication Background
Cardiovascular disease 41 (54.7) NSAID 20 (26.7)
Cirrhosis 8 (10.7) SSRI 13 (17.3)
Hepatitis 5 (6.7) Warfarin 10 (13.3)
Digestive disorders Steroid 2 (2.7)
Ulcer 27 (36) Opioid therapy
Intestinal ulcers 8 (10.7) Alcohol 16 (21.3)
Gastrointestinal cancer 6 (8) Opiates 31 (41.3)
Gastrointestinal bleeding 8 (10.7) Smoking 5 (6.7)
Methadone 1 (1.3)
Table 3. The endoscopic observation in the
patients
Endoscopic results N (%)
Pigmented ulcer Pigmented ulcer 2 (5.3)
Clean base 23 (30.7)
Gastritis 22 (29.3)
Tearing 2 (2.7)
Gastric varices 7 (9.3)
Visiblessle ulcer 8 (10.7)
16 patients needed for hospitalization (21.3%) in the
ICU. 6 (8%) of them had bleeding and 11 (14.7%) sub-
sequent endoscopy. Hospitalization period was 5.5±2.5
days and 12 deaths during hospitalization and 3 deaths
in 1 month follow-up were reported. After a month fol-
low-up, digestive signs 32 (50.8%), bleeding 32 (50.8%),
sever moral 2(3.1%), re-endoscpoy 2(3.1%), re-hospital-
ization 2(3.1%), and death 3(3.4%) were recorded. No
signi cant difference detected between sex, age, family
background, medication, Hematochezia, hematoma and
melena before and after the study (P>0.05). No signif-
icant difference observed in group aged <60 and >60
years old in mentioned factors (P>0.05).
According to the results, a signi cant correla-
tion observed between blood pressure and bad moral
(P<0.001), GI bleeding (P=0.018), alcohol (P=0.04),
Opium administration (P=0.000), NSAIDs (P=0.036),
ulcer incidence in primary endoscopy (P=0.003), Gas-
tritis (P=0.008), emergency surgery (P=0.000), ICU care
(P=0.000), re-bleeding (P=0.010) and need for subse-
quent endoscopy (P=0.000). A correlation exist between
opium administration in 1 month follow-up and endo-
scopic ulcer (P=0.07). A signi cant correlation reported
between death and peritonitis (P=0.046), hypotension
(P=0.053), gastric ulcer in endoscopy (P=0.04), bleeding
(P=0.023), ICU care (P=008) and no differences found in
re-endoscopy (P=027), NSAIDs (P=056), gastritis (P=073)
and emergency surgery (P=053).
According to the results, mortality rate in rst hos-
pitalization was 16% and in one-month follow up was
4%. There was no signi cant association between age
and gender with duration of hospitalization and one-
month prognosis. Mortality was associated with acute
abdomen and orthostatic hypotension I admission time,
peptic ulcer in endoscopic evaluation, active bleeding,
ICU admission and need to second endoscopy. Erosive
gastritis, need to emergent surgery and use of NSAID
s

344 ASSESSMENT OF SHORT TERM PROGNOSIS IN PATIENTS WITH UPPER GASTROINTESTINAL BLEEDING BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS
Saeid Hashemieh et al.
signi cant increase of mortality rate. It seems admission
time signs and symptoms, hemodynamic and coagula-
tion status, endoscopic results and need to re-endoscopic
evaluation are more prognostic factors in patients with
UGIB.
In a study, Lanas etal. (2011) on 2660 patients (64.7%
men; mean age 67.7 years) signi cant differences reported
on across countries in bleeding continuation ⁄ re-bleed-
ing (range: 9–15.8%) or death (2.5–8%) at 30 days were
explained by clinical factors (number of comorbidities, age
> 65 years, history of bleeding ulcers, in-hospital bleed-
ing, type of lesion or type of concomitant medication).
Other factors (country, size of hospital, pro le of team
managing the event, endoscopic and/or pharmacological
therapy received) were not able to affect these outcomes
(Loper do etal. 2009). Risk factors that have been previ-
ously identi ed to be predictive of bleeding continuation
and re-bleeding include presence of comorbidities out-
comes (Loper do etal. 2009) endoscopy-observed high-
risk stigmata of bleeding; worse health status at admis-
sion; bleeding from a peptic ulcer ( Viviane and Alan,
2008) a nding of bright blood during rectal examination
and in nasogastric tube aspirate; smoking; failure to use
PPIs postendoscopy; postendoscopy use of intravenous
or low molecular-weight heparins and low endoscopist
experience (Travis etal. 2008).
A number of these previously identi ed predictive
factors were con rmed in UGIB (i.e. presence of comor-
bidities, bleeding from a duodenal ulcer), and a number
of new predictors of bleeding continuation⁄ re-bleeding
were characterized: older age (>65 years), presentation
with haematemesis and a history of UGIB at baseline
(Button etal. 2011). Previously characterized predictors
of mortality include older age; presence of, and increas-
ing number of, comorbidities; continued bleeding and
⁄ or re-bleeding and a nding of bright blood in the
nasogastric tube aspirate (Marmo etal. 2010). The pre-
dictive validity of older age and the presence of comor-
bidities were con rmed in UGIB; in fact, the presence of
comorbidities was by far the strongest predictor of mor-
tality in this patient population. Other factors identi ed
to be signi cantly predictive of mortality in this study
were presentation with clinical symptoms of acute upper
GI bleeding and alcohol abuse (Shaheen etal. 2009).
The overall rate of deaths due to GI complications
and the rate of deaths associated with NSAID/aspirin
use reported are lower than some frequently quoted
estimates from previous studies, despite the fact that
our gures include both upper and lower GI complica-
tions and also refer to low-dose aspirin use (Hawkey and
Langman, 2003).
There are a number of reasons that may account
for some of the discrepancies observed in the studies:
variation in prescribing practice by country; differences
in the extent of NSAID use and in the co-prescription
of gastroprotective drugs; decreasing GI complication
rates; and differences in study methodologies. Our data
would imply a lower NSAID consumption in Spain com-
pared with other countries. However, the annual NSAID
prescription rates in Spain are relatively high (35.4 mil-
lion) (Van Leerdam etal. 2003) and are proportionally
greater than rates reported in the United Kingdom and
50% of those reported in the United States (70 million),
despite Spain’s smaller population. In addition, the rate
of NSAID use among adults in Spain (20.6%) is simi-
lar than that determined in the United States (Estudio,
2000). Upper GI bleeding is one of the most important
emergency disorders with high rates of mortality during
the acute phase. Longer term increased risk of mortality
is partly due to very poor prognosis for malignancy and
variceal etiologies; although it also re ects an impact of
high levels of social deprivation and chronic co-morbid
disease among people with upper GI bleeding (Roberts
etal. 2012).
Survival over the three years was substantially poorer
than in the general population for most etiologies of
bleeding, with the possible exception of ‘complications
of analgesics, antipyretics and anti-in ammatory drugs’
and duodenal ulcers, which were both less prevalent
among deprived quintiles than most of the other eti-
ologies. Relative survival was worse for duodenal ulcer
than for gastric ulcer in the rst few months after admis-
sion, but it was better than for gastric ulcer bleeds in the
longer term. This nding is consistent with a large sin-
gle-center study of surgery for peptic ulcer which found
increased longer term mortality for gastric ulcer but not
for duodenal ulcer (Stae¨l von Holstein etal. 1997). In
conclusion it seems admission time signs and symp-
toms, hemodynamic and coagulation status, endoscopic
results and need to re-endoscopic evaluation are more
prognostic factors in patients with UGIB.
REFERENCES
Button LA, Roberts SE, Evans PA, et al. 2011 Hospitalized
incidence and case fatality for upper gastrointestinal bleeding
from1999 to 2007: a record linkage study. Aliment Pharmacol
Ther 2011; 33: 64–76.
Button LA, Roberts SE, Evans PA, Goldacre MJ, Akbari A,
Dsilva R, Macey S, Williams JG 2011. Hospitalized incidence
and case fatality for upper gastrointestinal bleeding from 1999
to 2007: a record linkage study. Aliment Pharmacol Ther 33:
64–76
Carmona L. Estudio 2000 EPISER. Madrid: Spanish Society of
Rheumatology; 141–54.
De Abajo FJ, Gil MJ, Bryant V, et al.2013 Upper gastrointesti-
nal bleeding associated with NSAIDs, other drugs and interac-
tions: a nested case-control study in a new general practice
database. Eur J Clin Pharmacol 69:691–701.

BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS ASSESSMENT OF SHORT TERM PROGNOSIS IN PATIENTS WITH UPPER GASTROINTESTINAL BLEEDING 345
Saeid Hashemieh et al.
Halliday HL, Ehrenkranz RA, Doyle LW.2010 Early (<8 days)
postnatal corticosteroids for preventing chronic lung disease
in preterm infants. Cochrane Database Syst Rev (1):CD001146.
Hawkey CJ, Langman MJ 2003 .Non-steroidal anti-in amma-
tory drugs: Overall risks and management. Complementary
roles for COX-2 inhibitors and proton pump inhibitors. Gut
52(4):600–8.
Hearnshaw SA, Logan RF, Lowe D, Travis SP, Murphy MF,
Palmer KR. 2010 Use of endoscopy for management of acute
upper gastrointestinal bleeding in the UK: results of a nation-
wide audit. Gut 59: 1022–9.
Holcomb, J.B., Tilley, B.C., Baraniuk, S. etal. (2015) Transfu-
sion of plasma, platelets, and red blood cells in a 1:1:1 vs a
1:1:2 ratio and mortality in patients with severe trauma: the
PROPPR randomized clinical trial. JAMA, 313, 471–82.
Kovacs TOG, Jensen DM. 2008 The short-term medical man-
agement of non-variceal upper gastrointestinal bleeding.
Drugs 68 (15): 2105-2111.
Lanas A, Garcia-Rodriguez LA, Polo-Tomas M, etal. 2011 The
changing face of hospitalisation due to gastrointestinal bleed-
ing and perforation. Aliment Pharmacol Ther 33:585–91.
Lin HJ, Lo WC, Cheng YC, etal. 2006 Role of intravenous ome-
prazole in patients with high- risk peptic ulcer bleeding after
successful endoscopic epinephrine injection: a prospective,
randomized, comparative trial. Am J Gastroenterol 101: 500-5.
Loper do S, Baldo V, Piovesana E, etal. 2009 Changing trends
in acute upper-GI bleeding: a population-based study. Gastro-
intest Endosc 70: 212–24.
Marmo R, Koch M, Cipolletta L, etal. 2010 Predicting mortality
in non-variceal upper gastrointestinal bleeders: validation of
the Italian PNED score and prospective comparison with the
Rockall score. Am J Gastroenterol 2010; 105: 1284–91.
Martinek J, Hlavova K, Zavada F, etal. 2010 A surviving myth—
corticosteroids are still considered ulcerogenic by a majority of
physicians. Scand J Gastroenterol 45:1156–61.
Roberts SE, Button LA, Williams JG (2012) Prognosis follow-
ing Upper Gastrointestinal Bleeding. PLoS ONE 7(12): e49507.
doi:10.1371/ journal.pone.0049507
Shaheen AA, Kaplan GG, Myers RP. 2009 Weekend versus
weekday admission and mortality from gastrointestinal hem-
orrhage caused by peptic ulcer disease. Clin Gastroenterol
Hepatol 7: 303–10.
Stae¨l von Holstein C, Anderson H, Ahsberg K, Huldt B (1997)
The signi cance of ulcer disease on late mortality after partial
gastric resection. Eur J Gastroenterol Hepatol 9: 33–40.
Travis AC, Wasan SK, Saltzman JR.2008 Model to predict
rebleeding following endoscopic therapy for non-variceal
upper gastrointestinal hemorrhage. J Gastroenterol Hepatol
23: 1505–10.
Van Leerdam ME, Vreeburg EM, Rauws EA, etal. 2003 Acute
upper GI bleeding: Did anything change? Time trend analysis
of incidence and outcome of acute upper GI bleeding between
1993/1994 and 2000. Am J Gastroenterol;98(7):1494–9.
Viviane A, Alan BN. 2008 Estimates of costs of hospital stay
for variceal and nonvariceal upper gastrointestinal bleeding in
the United States. Value Health 11: 1–3.