
Health Science
Communication
Biosci. Biotech. Res. Comm. 10(2): 258-263 (2017)
Changes in the body weight and subsequent physical
activity of hypertensive patients using BASNEF model
Rahim Baghaee,
1
Neda Khalediyan
2
* and Alireza Didarloo
3
1
Associate Professor, Department of Nursing Medical Surgical, School of Nursing and Midwifery, Urmia
University of Medical Sciences, Urmia, Iran
2
Master Nursing Education, School of Nursing and Midwifery, Urmia University of Medical Sciences, Urmia, Iran
3
Associate Professor, Department of Health, School of Medicine, Urmia University of Medical Sciences, Urmia, Iran
ABSTRACT
Hypertension is a major public health issue. Lack of medication adherence in patients with hypertension can lead to
adverse outcomes. Therefore, patients need to be educated on how to control their blood pressure and increase their
behavioral preventive skills. Among the numerous models of health education, BASNEF model is the most com-
prehensive model used to study, identify and create new behaviors. This study aimed to determine the effect of an
educational intervention based on BASNEF model on the medication adherence in patients with hypertension. This
quasi-experimental study with pretest-posttest design conducted on 80 patients with hypertension referred to Health
Centers in Urmia, Iran, and met the eligibility criteria. They were selected using convenience sampling method and
then, randomly assigned to two groups as control and experimental. A 4-part questionnaire was used for collecting
the data. The collected data was analyzed by SPSS v.16 software using descriptive and inferential statistics (independ-
ent t-test, Mann-Whitney U test and Chi-square test). The results showed that the mean score of medication adher-
ence in patients with hypertension for a fundamental change in hypertension risk factors such as body weight and
subsequently physical activity in the experimental group was signi cantly more than the control group (P<0.001). It
seems that educational intervention based on BASNEF model has considerable advantages for a fundamental change
in hypertension risk factors such as body weight and subsequently physical activity and increases the medication
adherence in patients with hypertension signi cantly. Therefore, it is recommended to apply this educational model
as a key complementary factor to increases compliance of patients with hypertension.
KEY WORDS: HYPERTENSION, SMOKING, BODY WEIGHT, BASNEF, PHYSICAL ACTIVITY
258
ARTICLE INFORMATION:
*Corresponding Author: Urmia. neda.khaled22@gmail.com
Received 12
th
April, 2017
Accepted after revision 29
th
June, 2017
BBRC Print ISSN: 0974-6455
Online ISSN: 2321-4007 CODEN: USA BBRCBA
Thomson Reuters ISI ESC and Crossref Indexed Journal
NAAS Journal Score 2017: 4.31 Cosmos IF : 4.006
© A Society of Science and Nature Publication, 2017. All rights
reserved.
Online Contents Available at: http//www.bbrc.in/

Rahim, Neda and Alireza
INTRODUCTION
Hypertension is an increase in systolic blood pressure
over 140 mmHg systolic or 90 mm Hg diastolic (Kasper,
Braunwald, Fauci, Longo, & Jameson, 2005) and is
one of the factors to increase the incidence of mortal-
ity in developing countries and in developed countries.
According to WHO reports, in 2013, 12 % of all deaths
globally are attributed to hypertension and because of
the importance of this disease was the motto of 2013 in
the World Health Organization “be serious about hyper-
tension” (Organization, 2013). According to 2014 World
Health Organization, the prevalence of hypertension in
people over 18 years was 22% (Organization, 2014). In
2008, in Iran prevalence of hypertension in persons aged
64-25 was about 25 % (Esteghamati et al., 2008, Ghem-
baza et al., 2014).
The impact of non-pharmaceutical treatments include
reducing salt in the diet, get the weight loss, increase
the physical activity, lack of alcohol consumption for
reducing hypertension has been approved ) (Okwuonu,
Ojimadu, Okaka, & Akemokwe, 2014). In a study con-
ducted in Iran shown that only 40 % of patients gen-
erally obey the medicinal diet for controlling hyper-
tension (Hadi, Rostamigooran, & Jafari, 2005) and in
America also speci ed that 30-60% of the patients with
hypertension do not obey the prescribed medicinal regi-
men (Chobanian et al., 2003).Adherence of treatment is
de ned by the World Health Organization: the extent
which a person takes medicine and follows his diet or
exercise and changes its lifestyle (Ghembaza, Senous-
saoui, Kendouci Tani, & Meguenni, 2014). Non-adher-
ence of treatment also is de ned as “the failure to obey
the recommendations of health behavior or treat” (Mas-
ror Roudsari, Dabiri Golchin, & Haghani, 2013). Dif-
culty and complexity of the treatment regimen is a
factor related to treatment is considered as a possible
reason for low adherence to treatment. Repeat the dose,
the number of drugs that must be taken and the change
in antihypertensive medications are a number of fac-
tors that are involved in a dif cult regimen (Okwuonu,
Ojimadu, Okaka, & Akemokwe, 2014 and Ghajari,
Ghaderi, Valizadeh, Shakerinezhad, & Haghighizadeh,
2016).
In BASNEF model, unlike the behavior intention
model, the intention necessarily will not lead to behav-
ior, but enabling factors such as money, skill, precision
and facilities are between intention and behavior and in
the planning of this model should evaluate all enabling
factors on behavior (Didarloo A, 2013). Regarding the
mentioned issues, the authors decided to examine the
effect of education based on BASNEF to treatment in
patients with hypertension admitted to health centers of
Urmia University of Medical Sciences in 2015.
MATERIAL AND METHODS
In this experimental study, sample of study was obtained
among patients with hypertension referred to Health
Centers in Urmia, Iran. Using a list of patients referred
to the centers, based on quota random sampling and
lottery, 80 patients with hypertension were selected and
randomly divided into control and intervention groups.
The quota of health centers were included 40 patients
from the Tarzeloo health center, 20 patients from the 17
Shahryar health center and 20 patients from the Sho-
hada health center.
Informed consent was obtained from all participants.
Inclusion criteria included having a higher blood pres-
sure and equal to 140/90 mm Hg, 35-65 years of age,
the ability to read and write in the patient or one of his
family members and a willingness to participate in the
study and the exclusion criteria included three sessions
or more absence from training sessions, the patient’s
unwillingness to support the continuation of the study,
the patient’s hospitalization in the hospital and patient’s
death. The data collection instrument was a question-
naire that is designed according to the BASNEF model
and its reliability and validity were approved it. The
questionnaire included demographic information about
the opinion survey, questions related to the disease,
BASNEF model included four questions related to sec-
tion behavior, attitude, subjective norms and enabling
factors and Hill-Ben questionnaire for hypertensive
patients’ diet follow-up. Cronbach’s Alpha of discussed
structures was determined as follows:
Cronbach’s AlphaQuestionnaire Dimension
0.81Knowledge
0.96Attitude
0.93Subjective Norms
0.84Enabling factors
0.93Intention to behavior
0.90Adherence
Educational intervention based on BASNEF was done
only in the intervention group. Educational methods
were as lectures, distribution of educational package and
group discussion conducted on 6 session which each one
of them last 90 minutes. During the rst, second and
third session to in uence the attitude of the patients,
topics included: an overview of hypertension and its
complications, the effect of disease on the interpersonal
relationship, the cost of treating the complications, the
effects of healthy diet among hypertensive patients and
the effect of physical activity to decrease hypertension.
In the fourth session, the participation of patients in
team therapy and family were taught to impact on the
BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS CHANGES IN THE BODY WEIGHT AND SUBSEQUENTLY PHYSICAL ACTIVITY OF HYPERTENSIVE PATIENTS 259
Rahim, Neda and Alireza
dimensions of subjective norms. In the fth and sixth
sessions, the use of low facilities, increase the skill and
precision in the control of disease, adherence of treat-
ment and follow up in order to affect the enabling fac-
tors were taught. As well as, educational pamphlet about
control of diseases were distributed in order to affect the
intention to behavior aspect.
In the present study, three-month follow-up was
considered to examine the impact of the training based
on BASNEF model. Finally, after the completion of the
period of follow-up, the intervention group and the con-
trol answered the questionnaire again and the results of
the impact of educational based on BASNEF model was
analyzed.
Independent and paired t-test-test and Chi-square
statistics were used for the analysis of the data using
the software SPSS version 16. The limitations of the
study include the lack of cooperation of the relevant
authorities and personnel, the lack of educational ses-
sions and the existence of multilingual individuals in
the city of Urmia. The necessary permissions from the
research and ethics committees and the relevant authori-
ties was acquired from Urmia University of medical sci-
ences (Rec.IR.UMSU.1394.246). Researcher undertaken
that any con dential speci cations will not be inserted
in the article.
RESULTS AND DISCUSSION
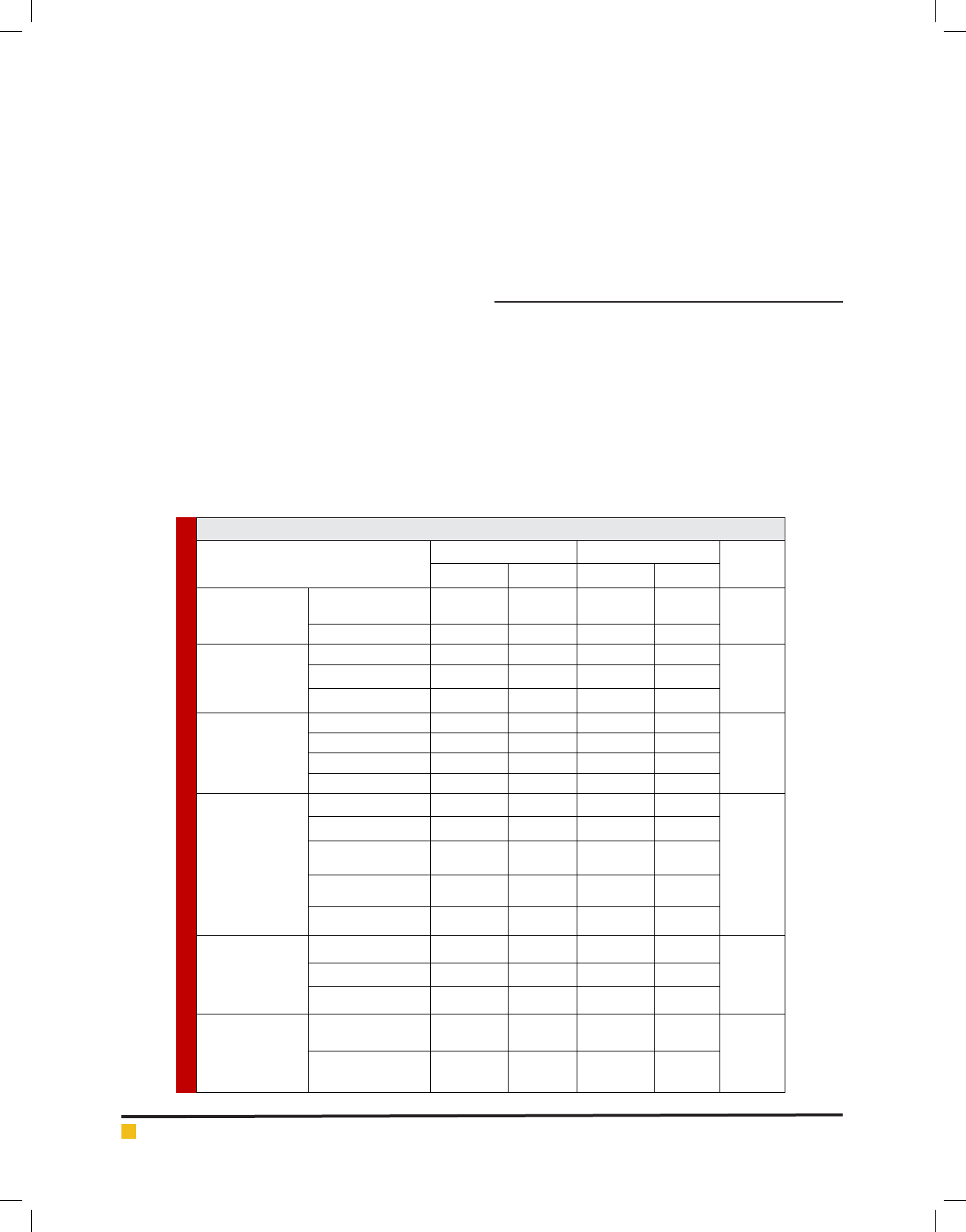
Gender, marital status, education level, employment sta-
tus, economic status, history of hypertension, history of
other diseases and sources of information between the two
groups had no signi cant difference (P>0.05) (Table 1).
There is a signi cant difference between the two
groups after the intervention in terms of the treatment of
hypertension and physical activity (P<0.05). Half of the
patients before the intervention had no physical activ-
ity, but after intervention, physical activity increased in
the intervention group than the control group. Also all
Table 1. The demographic information of patients in both intervention and control groups of subjects
P- Value
Intervention GroupControl GroupVariable
PercentFrequencyPercent
Frequency
P=0.999
208208Male
Gender
80328032Female
P=0.580
2.5100Single
Marital Status
85348534Married
5/125156Widow/Divorced
P=0.791
52.5216024Illiterate
Educational Level
22.5922.59Elementary
12.557.53Diploma
2.5100College
P=0.534
5200Employee
Occupation Status
52104Self-Employed
1047.53Unemployed
77.53177.531Household
5/2152Retired
P=0.784
1047.53Enough
Economic Status
52.5216024Somewhat Enough
37.51532.513Not Enough
P=0.066
72.5295020Yes
Hypertension
History
27.5115020No
260 CHANGES IN THE BODY WEIGHT AND SUBSEQUENTLY PHYSICAL ACTIVITY OF HYPERTENSIVE PATIENTS BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS

Rahim, Neda and Alireza
BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS CHANGES IN THE BODY WEIGHT AND SUBSEQUENTLY PHYSICAL ACTIVITY OF HYPERTENSIVE PATIENTS 261
aspects of the treatment of patients were observed after
treatment, including medication, nutrition and exercise
(Table 2).
Independent t-test showed that there was no signi -
cant statistical difference between the number of family
members and the body mass index before the interven-
tion (P = 0.225), but there was signi cant statistical dif-
ference after intervention between the body mass index
between the two groups, (P =0.019 (table 3).
High blood pressure is a major risk factor for devel-
opment of cardiovascular disease (Vrijens, Vincze,
Kristanto, Urquhart, & Burnier, 2008). The purpose of
this study was to determine the effect of education based
on BASNEF to treatment in patients with hypertension
admitted to health centers of Urmia University of Medi-
cal Sciences in 2015.In both groups, women formed the
majority of participants, that it’s more important for
women to refer the health centers. In the study of Rahaii
et al., in 2012, with the title “predictors of self-monitor-
ing of blood pressure based on the BASNEF in patients
with hypertension” (Rahaii et al., 2012) and in the study
of Naimii et al., in 2009 with the title “Knowledge and
Performance in Patients with high blood pressure “the
greatest of them were women (Naiimi, Malekzade, Had-
inia, Shari , & Mosavizade, 2008). The average age of
patients was 54.40 ± 10.85 years which is consistent with
the study of Izadirad et al., in 2012 (Izadirad, Masoodi,
& zareban, 2013).
Most subjects were married which is consistent with
the study of Hadi et al., in 2005 (Hadi, Rostamigooran,
& Jafari, 2005) .Most of the patients were illiterate and
only 2.5% were college educated people. In the study of
Naimii et al, more samples were illiterate (Naiimi, Male-
kzade, Hadinia, Shari , & Mosavizade, 2008). According
Table 2. Frequency distribution in terms of physical activity before and after the intervention in the subjects
P- Value
Intervention GroupControl GroupVariable
PercentFrequencyPercent
Frequency
P=0.278
27.51135141-3 times per week
Gender
Marital Status
1041563-5 times per week
7.53005-7 times per week
55225020None of them
P=0.009
351425101-3 times per week
Educational Level
2087.533-5 times per week
1562.515-7 times per week
30126526None of them
P=0.015
31.660015 minuteOccupation Status
63.212801630 minute
5.3120460 minute
000090 minute
P=0.007
3.617.7115 minute
Economic Status
39.31192.51230 minute
53.6150060 minute
3.610090 minute
Table 3. Comparison of average of BMI in two groups
P- value
intervention groupControl group
Variable
Mean± SDMean± SD
P=0.225
30.24±4.3731.27±5.14MBI after intervention
P=0.019
92.68±4.3723.15±5.44MBI before intervention

Rahim, Neda and Alireza
262 CHANGES IN THE BODY WEIGHT AND SUBSEQUENTLY PHYSICAL ACTIVITY OF HYPERTENSIVE PATIENTS BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS
to the results, most of the study subjects were house-
wives which is consistent with the study of Safai et al., in
2016 (M safaie sarnaghi, Hemmati Maslak Pak, Khadem-
vatan, & Alinejhad, 2016). Most patients had moderate
economic status which is consistent with the study of
Rahaii et al., in 2012 (Rahaii et al., 2012). According to
the results, the most of family had a history of hyperten-
sion. In the study of Jafarivarjoshani et al., with the title
‘impact of consultation = on the amount of blood pres-
sure in women with hypertension’, approximately half
of the participants had a history of hypertension (Jafari-
varjoshani, Anooshe, Ahmadi, & Namadian, 2004).
According to the obtained results of the intervention
and control groups in terms of the underlying variables,
there were no statistically signi cant differences and
were homogeneous. So the difference is meaningful in
the dependent variable after the intervention because of
the positive impact of the educational program based on
BASNEF model.
Regarding to the exercise, scores increased after the
intervention. Time of physical activity in the interven-
tion group signi cantly increased after intervention.
Chan et al., in 2009 found in their research that training
leads to more effective obedience in terms of activity
and exercise in patients (Chan, Lonsdale, Ho, Yung, &
Chan, 2009). The ndings of the study of Hung et al., in
2014, was consistent with our study (Hung et al., 2014).
CONCLUSION
Education is one of the most effective ways to treat highly
effective. It also requires training models for the correct
way of doing that. This study utilizes BASNEF to educate
patients and increase compliance with treatment and help
them improve their life. Hopefully, nurses and health pro-
viders apply the results of this study to improve the health
of patients and their treatment process.
REFERENCES
Chan, D. K., Lonsdale, C., Ho, P. Y., Yung, P., & Chan, K. (2009).
Patient motivation and adherence to postsurgery rehabilitation
exercise recommendations: the in uence of physiotherapists’
autonomy-supportive behaviors. Archives of physical medi-
cine and rehabilitation, 90(12), 1977-1982.
Chobanian, A., Bakris, G., Black, H., Cushman, W., Green, L.,
Izzo Jr, J.Wright Jr, J. (2003). The seventh report of the joint
national committee on prevention, detection, evaluation, and
treatment of high blood pressure: the JNC 7 report. Jama,
289(19), 2560-2571.
Didarloo A, S. D., Mohammadian H. (2013). Planning health
promotion, based on the models of behavior change. tehran:
asar sobhan.
Esmailizabihi, R., Ashktorab, T., Banaderakhshan, H., Zayeri,
F., & Zahrianbohi, S. (2011). Correlation between self-concept
according to Roy Adaptation model with adherence to thera-
peutic regimen in hypertensive outpatients who attended in
one of hospitals af liated to Urmia University Of Medical Sci-
ence. 21(73), 11-16.
Esteghamati, A., Abbasi, M., Alikhani, S., Gouya, M. M., Dela-
vari, A., Shishehbor, M. H., . . . Ramezani, R. D. (2008). Preva-
lence, awareness, treatment, and risk factors associated with
hypertension in the Iranian population: the national survey of
risk factors for noncommunicable diseases of Iran. American
journal of hypertension, 21(6), 620-626.
Ghajari, H., Ghaderi, N., Valizadeh, R., Shakerinezhad, G., &
Haghighizadeh, M. H. (2016). Knowledge, Attitude and Nutri-
tional Behavior of Female High School Students about Con-
sumption of Calcium-Rich Foods in Khorramshahr City, South
West of Iran. International Journal of Pediatrics, 4(11), 3837-
3846.
Ghembaza, M., Senoussaoui, Y., Kendouci Tani, M., &
Meguenni, K. (2014). Impact of patient knowledge of hyperten-
sion complications on adherence to antihypertensive therapy.
Current hypertension reviews, 10(1), 41-48.
Hadi, N., Rostamigooran, N., & Jafari, P. (2005). Assess the
determinants of adherence to medication regimen in patients
with high blood pressure. Elmi pezeshki, 4(3), 223-229.
Hung, Y., Bauer, J., Horsely, P., Coll, J., Bashford, J., & Isenring,
E. (2014). Telephone-delivered nutrition and exercise counsel-
ling after auto-SCT: a pilot, randomised controlled trial. Bone
marrow transplantation, 49(6), 786-792.
Izadirad, H., Masoodi, G., & zareban, I. (2013). Performance
review based of baznef model training program on self-care
behaviors of women with hypertension. Fasl name elmi pajho-
heshi zabol, 6(1), 42-51.
Jafarivarjoshani, N., Anooshe, M., Ahmadi, F., & Namadian,
M. (2004). Effect of Family Counseling on blood pressure in
patients with hypertension. Journal of Zanjan University of
Medical Sciences, 47(23-28).
Kasper, D., Braunwald, E., Fauci, S. H., Longo, D., & Jameson,
J. (2005). Harrison’s principles of internal medicine.
Masror Roudsari, D., Dabiri Golchin, M., & Haghani, H. (2013).
Relationship between Adherence to Therapeutic Regimen and
Health Related Quality of Life in Hypertensive Patients. Iran
Journal of Nursing, 26(85), 44-54.
Naiimi, E., Malekzade, J., Hadinia, A., Shari , B., & Mosavi-
zade, A. (2008). Knowledge and Performance in Patients with
Hypertension in The city’s top Boyer Ahmad in 2008. Arma-
ghan danesh, 16(5).
Okwuonu, C. G., Ojimadu, N. E., Okaka, E. I., & Akemokwe, F.
M. (2014). Patient-related barriers to hypertension control in
a Nigerian population. International journal of general medi-
cine, 7, 345.
Organization, W. H. (2013). http://www.emro.who.int/world-
health-days/2013/.

Rahim, Neda and Alireza
BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS CHANGES IN THE BODY WEIGHT AND SUBSEQUENTLY PHYSICAL ACTIVITY OF HYPERTENSIVE PATIENTS 263
Organization, W. H. (2014). http://www.who.int/mediacentre/
factsheets/fs317/en/.
Rahaii, Z., Baghianimoghadam, M., Morovatisharifabad, M.,
Zareian, M., Fallahzade, H., & Mahmoodabad, M. (2012). Pre-
dictors of self-monitoring based on BASNEF model of blood
pressure in patients with hypertension Payesh, 11(5), 621-627.
Sabaté, E. (2003). Adherence to long-term therapies: evidence
for action: World Health Organization.
Safaie sarnaghi, m., Hemmati Maslak Pak, M., khademvatan,
k., & Alinejhad, v. (2015). Comparison the effectiveness of
Short Massage Service and Remainder Cards on adherence to
treatment in patients with hypertension referred to Sayyed-Al
Shohada E ducational treatmental center in 2015.
Vrijens, B., Vincze, G., Kristanto, P., Urquhart, J., & Burnier, M.
(2008). Adherence to prescribed antihypertensive drug treat-
ments: longitudinal study of electronically compiled dosing
histories. BMJ, 336(7653), 1114-1117.