
Health Science
Communication
Biosci. Biotech. Res. Comm. 10(2): 192-196 (2017)
Insulin resistance beliefs in patients with type II
diabetes according to the health belief model
Milad Borji,
1
Ali Shari ,
2
Razieh Molavi,
3
* Mohammad Amin Mohseni
4
and Asma Tarjoman
4
1
Department of Nursing, Faculty of Nursing and Midwifery, Ilam University of Medical Science, Ilam, Iran
2
Assistant Professor, Department of Internal Medicine, School of Medicine, Ilam University of Medical Sciences,
Ilam, Iran
3
MSc Elderly Nursing, AL-Zahra Hospital, Isfahan University of Medical Sciences, Isfahan, Iran
4
Student Research Committee, Ilam University of Medical Sciences, Ilam, Iran
ABSTRACT
Regular administration of insulin injections with correct dosing results in well-controlled blood glucose levels and
decreased diabetic complications. This study aimed to investigate beliefs associated with insulin resistance in patients
with type II diabetes, according to the Health Belief Model. In this descriptive cross-sectional study, 300 patients with
type II diabetes from the hospitals of Ilam were included. Data were collected using the Insulin Resistance Beliefs in
Patients with Type II Questionnaire, which was designed using the components of the Health Belief Model from previ-
ous studies. The Kruskal-Wallis test, Mann-Whitney test, and Pearson correlation coef cient were adopted at a signif-
icance level of less than 0.05.The mean age of the study participants was 9.62 ± 47.77 years. Of them participants, 95
(31.7%) were illiterate, 156 (52%) were married, and 151 (50.3%) had an income level less than 500,000 Tomans per
month. The scores for components of perceived sensitivity, perceived severity, perceived barriers, perceived bene ts,
self-ef ciency, operation guideline, and general awareness were 5.37 (2.36), 16.79 (5.07), 27.53 (7.06), 30.83 (5.11),
19.51 (5.44), 27.51 (5.63), and 127.20 (13.91), respectively. Training packages and appropriate nursing interventions
are recommended to reduce the negative beliefs associated with insulin injection.
KEY WORDS: HEALTH BELIEF MODEL, DIABETES, INSULIN
192
ARTICLE INFORMATION:
*Corresponding Author: Raziehmolavi@yahoo.com
Received 1
st
Feb, 2017
Accepted after revision 22
nd
May, 2017
BBRC Print ISSN: 0974-6455
Online ISSN: 2321-4007 CODEN: USA BBRCBA
Thomson Reuters ISI ESC and Crossref Indexed Journal
NAAS Journal Score 2017: 4.31 Cosmos IF : 4.006
© A Society of Science and Nature Publication, 2017. All rights
reserved.
Online Contents Available at: http//www.bbrc.in/
DOI: 10.21786/bbrc/10.2/33

Milad Borji et al.
INTRODUCTION
Chronic diseases persist for a long time. Therefore, if
chronic conditions are not well-controlled, the demand
for health care services increases, leading to a reduced
quality of life in these,(Esmaeili Shahmirzadi et al.,
2012). Diabetes is a chronic disease of the endocrine
glands, resulting in a malfunction of glucose metabo-
lism. The disease has three main forms including type I
diabetes or insulin-dependent diabetes mellitus (IDDM),
type II diabetes or non-insulin-dependent diabetes melli-
tus (NIDDM), and gestational diabetes mellitus(Statistics
released by the World Health Organization showed that
228 million adults have diabetes. The prevalence of this
disease in Iran is reported to be 2%–3% and 3.7% in
individuals aged >30 years (Kabodi et al., 2016). Diabe-
tes is a silent disease that annually kills approximately
4 million people in the world (Aghayouse , et al., 2017
Aghayouse , Dehestani, & Salary, 2017).
Diabetic complications are generally divided into vas-
cular and non-vascular groups. Vascular complications
are further subdivided into microvascular & macrovas-
cular groups. Microvascular complications(MC) include
nephropathy, retinopathy,neuropathy, whereas in mac-
rovascular complications consist of coronary artery dis-
eases & peripheral vascular disease. Non-vascular com-
plications that may affect patients with diabetes include
gastroparesis, skin changes, and infections. Prevention
of these complications is necessary (Longo et al., 2014).
Since diabetes is a chronic disease that can cause
behavioral and emotional problems in patients, the
psychological aspects of diabetes are signi cant (Seye-
doshohadaee, Kaghanizade, Nezami, Hamedani, & Bar-
asteh, 2016). Because of the in uence of psychological
factors on the quality of lives of patients with diabetes,
the impact of these factors is of paramount importance.
Previous studies have shown the effects of temporal
aspects in the prevention of diabetes in patients with
pre-diabetes (Moayedi, Zare, & Nikbakht, 2015). Several
studies have been conducted in Iran and other coun-
tries concerning the factors that may affect resistance to
insulin therapy. These factors include a fear of reduced
independence, hypoglycemia complications (Funnell,
2007), increased body mass index (BMI) caused by insu-
lin therapy (Shari rad, Hazavehi, Baghianimoghadam,
& Mohebi, 2007), lifestyle changes, and resistance in
patients (Guler, Vaz, & Ligthelm, 2008).
The Health Belief Model is one of the health models,
which re ects the relationship between health beliefs
and health behaviors. This model places an emphasis on
the individual’s motivation in performing such health-
related (Glanz, Rimer, & Viswanath, 2008). In this model,
the desired behavior shall bene t the help-seekers in
various health aspects. Subsequently, educators iden-
tify barriers to a behavior and plan accordingly. Next,
a training program shall create the necessary sensitiv-
ity regarding the complications and risks of failure to
perform health behaviors. When patients understand the
disease and its complications, they would notice more
bene ts in performing preventive behaviors, be more
inclined to adopt such behaviors, and nally, apply
the behavior appropriately (Mohebi et al., 2012; Moodi,
Moasheri, & Amirabadi Zadeh, 2016). This model has
been considered in many studies to review and assess
the health behaviors (Kohdaveisi, Salehikha, Bashirian,
& Karami, 2016; Sahraee, Noroozi, & Tahmasebi, 2013a;
Soleymanian, Niknami, Hajizadeh, Shojaeizadeh, &
Montazeri, 2014; Walker & Jackson, 2015).
If insulin is injected properly and regularly at correct
dosages, then blood glucose levels will be controlled,
and diabetic complications will be reduced. According
to the results of many studies, only 25% of patients with
diabetes who need insulin to control diabetes complete
this type of therapy (Gough, Frandsen, & Toft, 2006;
Grant, Buse, & Meigs, 2005). Given the importance of
diabetes and its increasing prevalence, this study aimed
to examine the beliefs associated with the rejection of
insulin in patients with type II diabetes.
MATERIALS AND METHODS
This study was at descriptive cross-sectional study. This
study population consisted of patients with diabetes in
the hospitals of Ilam in 2017, of whom 300 patients were
included. Inclusion criteria were being affected by dia-
betes type II, taking insulin to control diabetes, un will-
ingness to take insulin despite doctors’ emphasis, having
the ability to answer questions, and lack of psychologi-
cal problems such as psychosis and severe depression or
intellectual disabilities.
This study was initiated after researchers had met the
study participants and obtained their informed consent.
The patients were assured that their personal information
would be kept con dential by the researchers. Given that
most patients were illiterate to ll out the questionnaires,
the interview method was used instead. The researchers
daily referred to Shahid Mostafa Khomeini and Imam
Khomeini hospitals in Ilam and completed the question-
naire by identifying patients with diabetes. Data were
collected using the Insulin Resistance Beliefs in Patients
with Type II Questionnaire, which was designed using
the constructs from the Health Belief Model accordance
with questionnaire developed by Kaboudi et al. (Kabodi
et al, 2016).
These constructs included perceived sensitivity (2
items) & perceived severity (6 items) & perceived ben-
e ts (9 items) & perceived self-ef cacy (6 items) &
BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS INSULIN RESISTANCE BELIEFS IN PATIENTS WITH TYPE II DIABETES 193
Milad Borji et al.
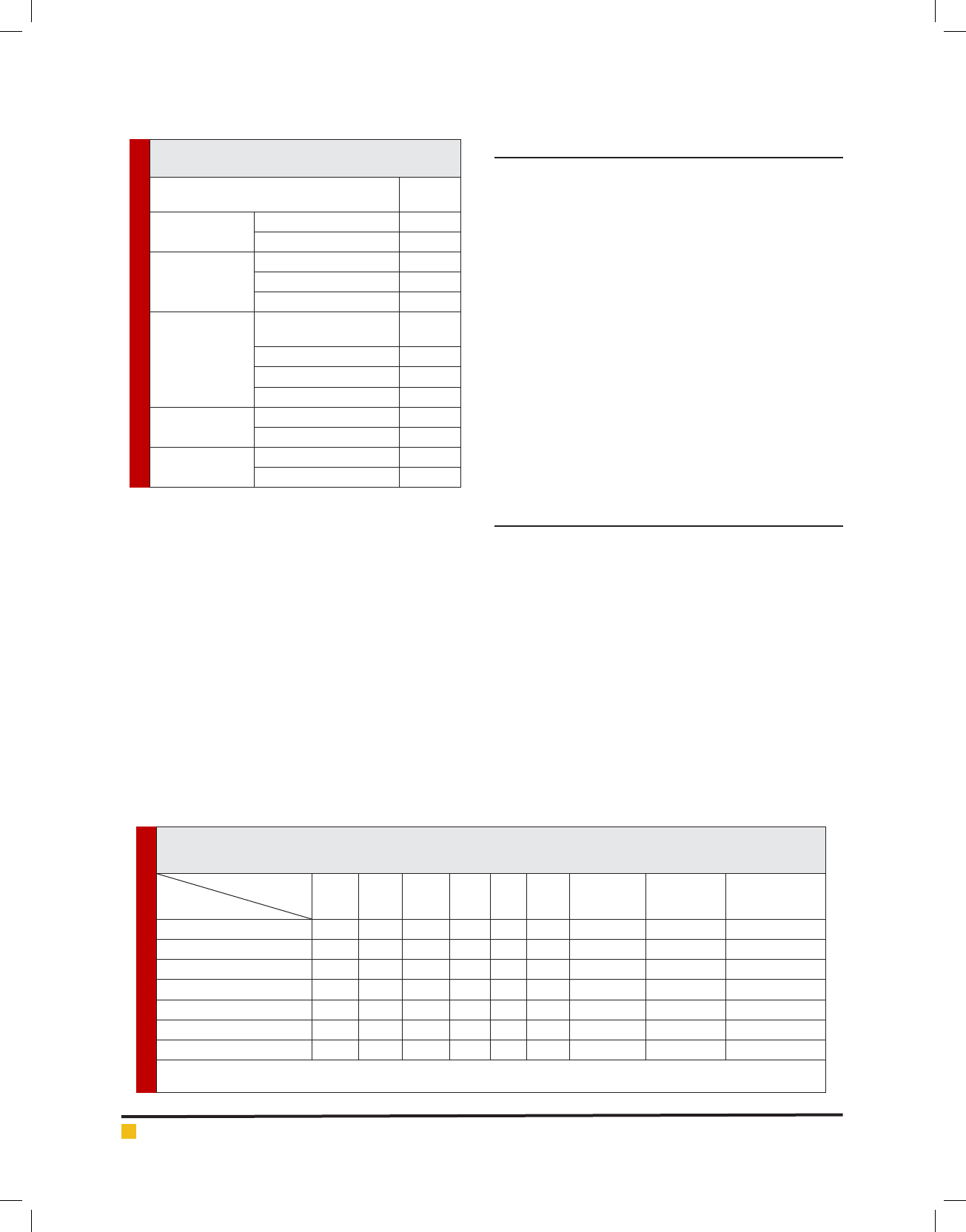
Table 2. Mean, standard deviation, and correlation between the health belief model constructs and their relationship
with the beliefs associated with rejection of insulin injections
S.D (Mean)MaximumMinimum6*5*4*3*2*1*
Structures
constructs
5.37(2.36)102------perceived sensitivity
16.79(5.07)306-----.64**perceived severity
27.53(7.06)459----.32.48perceived bene ts
30.83(5.11)5010---.10.06-.008-perceived barriers
19.51(5.44)306--.11-.24-.02.13-perceived self-ef cacy
27.51(5.63)408-.46.18-.20-.10-.13-operation guideline
127.20(13.91)2052.36.39.27.56.58.53awareness
**Correlation is signi cant at the 0.01 level (2-tailed)
*1- 6 (constructs 1 - 6 from the Health Belief Model )
perceived barriers (10 items) & and operation guide-
line (8 items). Responses provided for all questions
were based on a Five-point Likert scale ranging from
in One (strongly disagree) to Five (strongly agree). In
all aspects of the questionnaire (except the perceived
barriers), a high score indicated acceptance of insulin
therapy as an appropriate method for diabetes by the
patient; however, a high score in the perceived barri-
ers re ected numerous obstacles to the acceptance of
insulin therapy. A questionnaire a made researcher. But
questions of accordance with and on the model of was
made by Kaboudi et al 2016) .Reliability and validity of
the questionnaire obtained by the researcher. Following
data collection, the information obtained was entered
using the SPSS software (version 20; Kruskal-Wallis test,
Mann-Whitney test, and Pearson correlation coef cient
were adopted at a signi cance level of less than 0.05.
RESULTS
According to the study ndings, the mean age of the
study participants was 9.62 ± 47.77 years. Of these
patients, 95 (31.7%) were illiterate, 156 (52%) were mar-
ried, and 151 (50.3%) had an income level less than
500,000 Tomans per month (Table 1).
According to Table 2, the maximum and minimum
mean scores were related to the constructs operation guide-
line and perceived sensitivity, respectively. The Pearson
correlation coef cient suggested that education and level
of income had a statistically signi cant negative associa-
tion with a history of diabetes and beliefs associated with
lack of insulin injections so that older people with higher
levels of education and income had lower levels of nega-
tive beliefs about insulin rejection. However, no statisti-
cally signi cant relationship was observed between other
demographic characteristics such as age, occupation, mari-
tal status, and negative beliefs regarding insulin injection.
DISCUSSION
This study aimed to investigate the beliefs associated
with the rejection of insulin in patients with type II dia-
betes in Ilam, according to the Health Belief Model con-
structs. This model contains ve constructs, which are
discussed separately in the following section.
Regarding the rst construct (i.e., perceived sensitiv-
ity), the ndings of this study showed that most patients
were not sensitive enough to feel the need for insu-
lin injections. In Kaboudi’s et al. study of 2016, which
aimed to determine beliefs associated with insulin injec-
tion, the ndings showed that only 66.95% of the scores
revealed perceived sensitivity of patients in terms of
insulin injections. This nding was consistent with that
of the present study. Regarding the next construct (i.e.,
perceived severity, the ndings showed that most of the
Table 1. Demographic characteristics: School-age
children with diabetes
N(%)Variable
145(48.3)Male
Gender
155(51.7)Female
95(31.7)illiterate
Education
183(61)Diploma and low literate
22(7.3)Collegiate
151(50.3)
Less than 500 thousand
Rials
income
94(31.3)500 to 1 million
30(10)1 to 2 million
25(8.3)More than 1 million
156(52)Married
Married
144(48)No husband
133(44.3)yes
History of insulin
167(55.7)No
194 INSULIN RESISTANCE BELIEFS IN PATIENTS WITH TYPE II DIABETES BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS

Milad Borji et al.
BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS INSULIN RESISTANCE BELIEFS IN PATIENTS WITH TYPE II DIABETES 195
scores of the studied patients did not meet the necessary
severity regarding insulin injections.
Similarly, this study (Kabodi et al., 2016) indicated
that only 60.7% of scores re ected the severity of insulin
injections. In fact, when a person feels no threat regard-
ing the disease (perceived sensitivity and severity), he/
she cannot change a behavior appropriately(Dietrich,
1996). According to Patino et al., to enhance the level
of threat perceived by the patients (perceived sensitivity
and severity), more focus should be placed on the short-
term complications of diabetes (Patino, Sanchez, Eidson,
& Delamater, 2005).
Concerning other constructs in this model, the results
indicated that the scores obtained by most patients in
terms of perceived bene ts were at a low level and unde-
sirable. Regarding these perceived barriers, the scores
were also high and undesirable, resulting in the lack of
insulin injection. In a study conducted by Vahidi et al.,
the perceived barriers in comparison with The other con-
structs in the Health Belief Model(HBF) had the greatest
impact on the construct of self-ef cacy in patients with
diabetes so that an individual’s positive beliefs to follow
the prophylactic treatment of diabetes increases by rais-
ing their awareness regarding the psychological costs
of adopting a behavior (Vahidi, Shojaeizadeh, Esmaeili
Shahmirzadi, & Nikpour, 2014).
The ndings for the next construct (i.e., perceived
self-ef cacy) revealed that the patients’ self-ef cacy
levels were not at a desirable level. This result was in
line with the ones of Kaboudi et al (Kabodi et al., 2016),
Other studies suggested that self-ef cacy is an effective
and strong predictor of behavior (Avci, 2008; Noroozi,
Jomand, & Tahmasebi, 2011; Sahraee, Noroozi, & Tah-
masebi, 2013b; Tava an, Hasani, Aghamolaei, Zare, &
Gregory, 2009). In fact, the construct of self-ef cacy was
the best predictor of self-care behaviors. Findings asso-
ciated with the operation guidelines showed that this
construct received the highest score. According to its
relevant items, the medical staff and mass media played
the most critical roles, which was similar to the results of
previous studies indicating the signi cant impact of the
medical staff (Borhani, et al., 2010; Kabodi et al., 2016))
and mass media (Mahmoodabad et al.,2016; Taghdisi &
Nejadsadeghi, 2011) on patient awareness.
CONCLUSION
Training packages and appropriate nursing interven-
tions should be administered to reduce the negative
beliefs associated with insulin injection.
CONFLICT OF INTEREST
Ther e is no con ict of interest between authors.
SOURCE OF FUNDING
Ilam University of Medical Sciences.
REFERENCES
Aghayouse , A., Dehestani, M., & Salary, S. (2017). The Role
of Perceived Social Support and Resilience in Predicting the
Quality of Life in patients with Type 2 Diabetes. Iranian Jour-
nal of Endocrinology and Metabolism, 18(5), 334-342.
Avci, I. A. (2008). Factors associated with breast self-exam-
ination practices and beliefs in female workers at a Muslim
community. European Journal of Oncology Nursing, 12(2),
127-133.
Borhani, F., Abbaszadeh, A., Taebi, M., & Kohan, S. (2010). The
relationship between self-ef cacy and health beliefs among
type2 diabetic patients.
Dietrich, U. C. (1996). Factors in uencing the attitudes held
by women with type II diabetes: a qualitative study. Patient
education and counseling, 29(1), 13-23.
Esmaeili Shahmirzadi, S., Shojaeizadeh, D., Azam, K., Salehi,
L., Tol, A., & Moradian Sorkhkolaei, M. (2012). The impact of
chronic diseases on the quality of life among the elderly peo-
ple in the east of Tehran. Journal of Payavard Salamat, 6(3),
225-235.
Funnell, M. M. (2007). Overcoming barriers to the initiation of
insulin therapy. Clinical Diabetes, 25(1), 36-38.
Glanz, K., Rimer, B. K., & Viswanath, K. (2008). Health behav-
ior and health education: theory, research, and practice: John
Wiley & Sons.
Gough, S., Frandsen, K., & Toft, A. (2006). Failure of insulin
monotherapy in patients with type 2 diabetes. Diabetic Medi-
cine, 23, 551.
Grant, R. W., Buse, J. B., & Meigs, J. B. (2005). Quality of diabe-
tes care in US academic medical centers. Diabetes care, 28(2),
337-442.
Guler, S., Vaz, J. A., & Ligthelm, R. (2008). Intensi cation
lessons with modern premixes: from clinical trial to clini-
cal practice. Diabetes research and clinical practice, 81, S23-
S30.
Khodaveisi, M., Salehikha, M., Bashirian, S., & Karami, M.
(2016). Study Of Preventive Behaviors Of Hepatitis B Based On
Health Belief Model Among Addicts Af liated To Hamedan.
Longo, D. L., Fauci, A. S., Kasper, D. L., Hauser, S. L., Jameson,
J. L., & Loscalzo, J. (2014). Harrison’s Principles of Internal
Medicine 19th Ed: McGraw-Hill Medical.
Mahmoodabad, M S., KarimianKakolaki, Z., Enjezab, B., &
Soltani, T. (2016). Determinants of Preventive Behaviors of
Urinary Tract Infections in Pregnant Women Based on the
Constructs of Health Belief Model in Yazd. [Research]. Tolooe-
behdasht, 15(1), 138-149.
Moayedi, F., Zare, S., & Nikbakht, A. (2015). Anxiety and
depression in diabetic patient referred to Bandar Abbas dia-
betes clinic. Bimonthly Journal of Hormozgan University of
Medical Sciences, 18(1), 65-71.

Milad Borji et al.
196 INSULIN RESISTANCE BELIEFS IN PATIENTS WITH TYPE II DIABETES BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS
Mohebi, M., Shari rad, G., Rasekhi, H., Matlabi, M., Shahsiah,
M., & Tabaraie, Y. (2012). Effect of nutrition education pro-
gram on the recommended weight gain in during pregnancy
application of Health Belief Model: A randomaized cilinical
trial. Qom Univ Med Sci, 1(6), 23-30.
Moodi, M., Moasheri, B. N., & Amirabadi Zadeh, N. (2016).
Assessment of Health Belief Model (HBM) impact on knowl-
edge, beliefs, and self-ef cacy of women in need of genetic
counseling. [Original Article]. Journal of Birjand University of
Medical Sciences, 23(3), 246-256.
Noroozi, A., Jomand, T., & Tahmasebi, R. (2011). Determi-
nants of breast self-examination performance among Iranian
women: an application of the health belief model. Journal of
Cancer Education, 26(2), 365-374.
Patino, A. M., Sanchez, J., Eidson, M., & Delamater, A. M.
(2005). Health beliefs and regimen adherence in minority ado-
lescents with type 1 diabetes. Journal of pediatric psychology,
30(6), 503-512.
Kabodi S, Rahimi M, Niromand E, Ajami E, Egbalian A, Barati
M .(2016) Beliefs On Insulin Injection Non-Adherence Among
Type 2 Diabetic Patients: Assessment based On Health Belief
Model. Iranian Journal of Diabetes and Lipid Disorders. [Appli-
cable]. 2016;15(2):110-9.
Sahraee, A., Noroozi, A., & Tahmasebi, R. (2013a). Predicting
Factors of Breast Self-Examination based on Health Belief
Model and Locus of Control among Women Aged 20-50 Years.
Journal of hayat, 19(2), 27-39.
Sahraee, A., Noroozi, A., & Tahmasebi, R. (2013b). Predict-
ing Factors of Breast Self-Examination based on Health Belief
Model and Locus of Control among Women Aged 20-50 Years.
[Research]. Hayat, 19(2), 27-39.
Seyedoshohadaee, M., Kaghanizade, M., Nezami, M., Hamed-
ani, B., & Barasteh, S. (2016). The Relationship Between Health
Literacy And General Health In Patients With Type 2 Diabe-
tes. Iranian Journal of Diabetes and Metabolism, 15(5), 312-
319.
Shari rad, G., Hazavehi, M., Baghianimoghadam, M., &
Mohebi, S. (2007). The Effect of a Health Belief Model Based
Education Program for Foot Care in Diabetic Patients Type II
in Kermanshah, Iran (2005). [Original Article]. Int J Endocrinol
Metab, 5(2), 82-90.
Soleymanian, A., Niknami, S., Hajizadeh, E., Shojaeizadeh,
D., & Montazeri, A. (2014). Development and validation of a
health belief model based instrument for measuring factors
in uencing exercise behaviors to prevent osteoporosis in pre-
menopausal women (HOPE). BMC musculoskeletal disorders,
15(1), 61.
Taghdisi, M. H., & Nejadsadeghi, E. (2011). Evaluation of preg-
nant women in the eld of Urinary Tract Infection according
to the components of Health Belief Model.
Tava an, S. S., Hasani, L., Aghamolaei, T., Zare, S., & Gregory,
D. (2009). Prediction of breast self-examination in a sample
of Iranian women: an application of the Health Belief Model.
BMC women’s health, 9(1), 37.
Vahidi, S., Shojaeizadeh, D., Esmaeili Shahmirzadi, S., &
Nikpour, S. (2014). Assessing Self Ef cacy with Health Belief
Model component among type 2 diabetic patients referee to
Iranian Diabetes Association in 2012-2013. J Health Syst Res,
10(3), 538-547.
Walker, K., & Jackson, R. (2015). The health belief model and
determinants of oral hygiene practices and beliefs in preteen
children: a pilot study. Pediatric dentistry, 37(1), 40-45.