
Medical
Communication
Biosci. Biotech. Res. Comm. 10(2): 182-186 (2017)
The oral and maxillofacial manifestation and
surgical consideration in Maroteaux Lamy syndrome
(mucopolysaccharidosis VI): A case report
Farnoosh Mohammadi, DDS, OMFS
1
and Iman Tavakoli DDS
2
*
1
Assistant Professor, Department of Oral and Maxillofacial Surgery of Tehran University of Medical Sciences,
Tehran, Iran
2
Resident of Oral & Maxillofacial Surgery, Department of Oral and Maxillofacial Surgery, Craniomaxillofacial
Research Center, Tehran University of Medical Sciences, Tehran, Iran
ABSTRACT
The role of the genetic disorders in maxillofacial manifestations is well documented. Maroteaux Lamy syndrome
(mucopolysaccharidosis VI) is a metabolic and chromosomal abnormality which involving disturbances in mucopoly-
saccharide metabolism and storage of acid mucopolysaccharide in various tissues. The main factor for Maroteaux
Lamy syndrome is de ciency of arylsulfatase B. Deposition of mucopolysaccharides leads to a progressive disorder
which has several oral and dental manifestations including condylar hypoplasia, long-coarse face, anterior open bite,
cranial deformity, macroglossia, malposition teeth, gingival bromatosis and under-developed maxillary sinus. Also,
a large head, short neck and corneal opacity are the main characteristic features.In this study a case of 4 years old
girl with Maroteaux-Lamy syndrome with emphasis on oral and maxillofacial manifestations and practical surgical
hints for correction of maxillofacial deformity introduced.
KEY WORDS: MAXILLOFACIAL MANIFESTATION, SURGICAL CONSIDERATION, MAROTEAUX LAMY SYNDROME
182
ARTICLE INFORMATION:
*Corresponding Author: iman1122@gmail.com
Received 1
st
Feb, 2017
Accepted after revision 14
th
June, 2017
BBRC Print ISSN: 0974-6455
Online ISSN: 2321-4007 CODEN: USA BBRCBA
Thomson Reuters ISI ESC and Crossref Indexed Journal
NAAS Journal Score 2017: 4.31 Cosmos IF : 4.006
© A Society of Science and Nature Publication, 2017. All rights
reserved.
Online Contents Available at: http//www.bbrc.in/
INTRODUCTION
MaroteauxLamy syndrome or mucopolysaccharido-
sis (MPS) type VI is a rare genetic disorder with auto-
somal recessive transmissionswas rst described in 1963
(Maroteaux et al. 1963). This syndrome characteristic by
de ciency of arylsulfatase B (N-acetylgalactosamine-4-
sulfatase), which results in the accumulation of derma-
tan sulfate and chondroitin 4-sulfate within lysosomes
of the connective tissues occurs
(Azevedo et al. 2004;
Valayannopoulos et al. 2010). The somatic features of
in the Maroteaux-Lamy syndrome patients is similar to
Farnoosh Mohammadi and Iman Tavakoli
the other mucopolysaccharidosis (Roberts et al. 1984)
however it is distinguished by the existence of normal
intelligence, prominent metachromatic inclusions in
leukocytes as well as lack of arylsulfatase B (Alpoz et al.
2006). Arylsulfatase B plays critical role in degradation
of glycosaminoglycans (GAG) such as dermatan sulfate
and chondoitine sulfate (Neufeld et al. 1995; Valayan-
nopoulos et al. 2010).The etiology of MPS type VI is
mutation in arylsulfatase B gene which is located on the
chromosome 5q13-5q14 (Litjens et al. 1989). The ana-
tomic feature of the disease is characteristic with growth
retardation, hernias, typical facies, a large deformed
head with short neck and spinal abnormalities (Valayan-
nopoulos et al. 2010, Fonseca et al. 2014).
In the sever condition, death can happen in result of
cardiac disease or respiratory tract infection (Wiedemann
et al. 1992). In this study a case of 4 years old girl with
Maroteaux-Lamy syndrome with emphasis on oral and
maxillofacial manifestations and practical surgical hints
for correction of maxillofacial deformity introduced.
CASE REPORT
BASIC INFORMATION
A 4 yearand 6 months-old girl withMaroteaux-Lamy syn-
drome was admitted to the Children’s Medical Center of
Tehran University of Medical Science, Tehran, Iran. She
was the only child of a young couple with no consan-
guinity. They were aware of traits of syndrome since 3
years ago. Small size, disability in extension of upper and
lower limb and abnormal facial appearance were the ini-
tial symptoms mentioned by the parents. Investigations
revealed no cardiac, ophthalmic, mental or hearing dis-
order. She was not able to walk because of short stature,
generalized dysostosis and joint deformity. She had no
mental de cit but she was not able to speak. Huge gin-
gival overgrowth, macroglossia and abnormal anatomy
were contributed to her speechless. Oral and maxillofacial
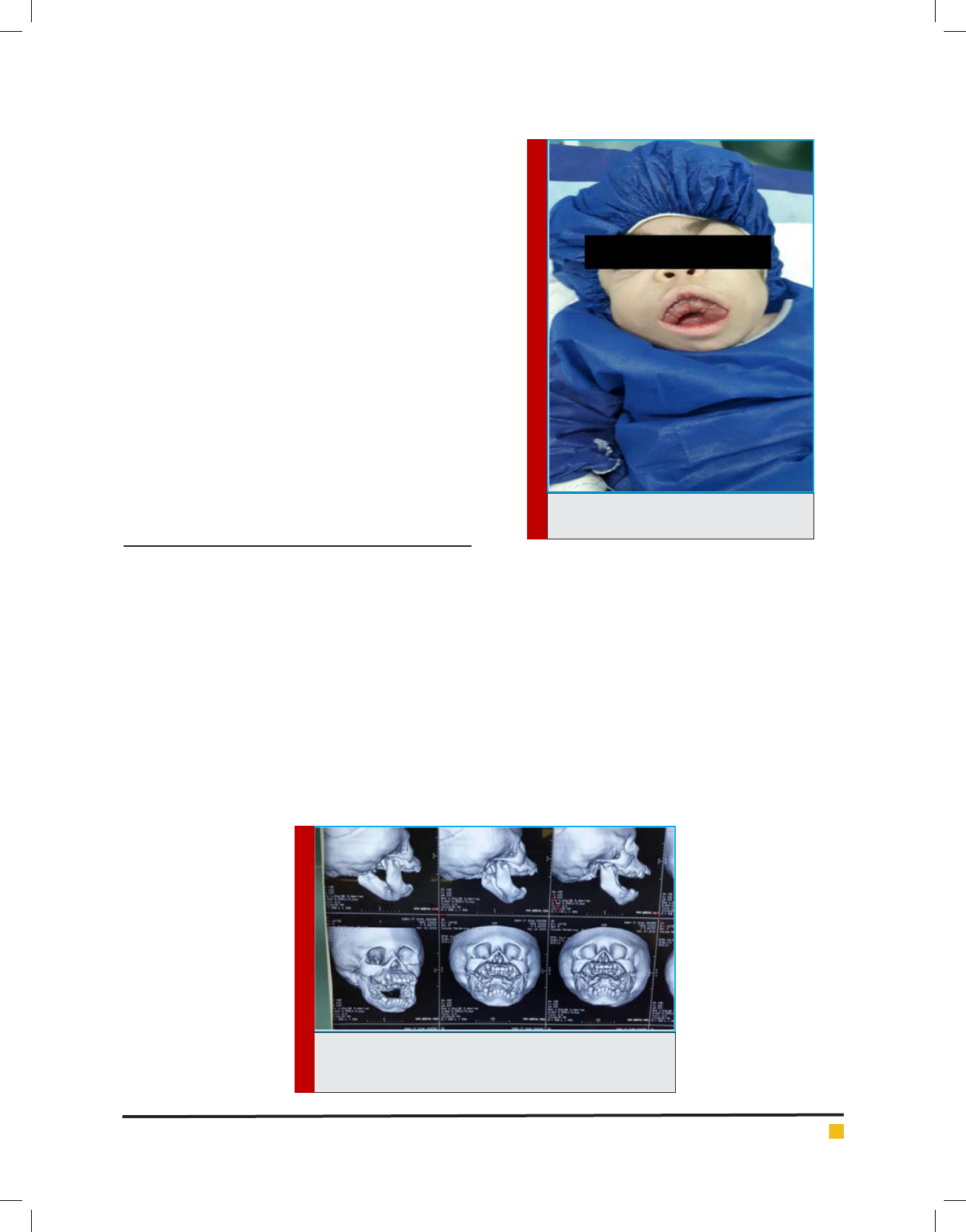
manifestations include large head, long coarse face, hyper-
telorism, bushy eyebrows, deep nasojugal fold, marked
open bite and open mouth breathing, infra-erupted teeth
and gross gingival bromatosis (Figure1). The weight of
the patient before the surgery was 7.8kg. The lysosomal
enzyme analysis showed decreased activity of arylsulfa-
tase B in blood sample was determine using arylsulfatase
B enzyme assay (normal 300-900 nmol/h/mg) (Baum et al.
1959). The blood arylsulfatase B was 0.14 - 0.70 nmol/21h.
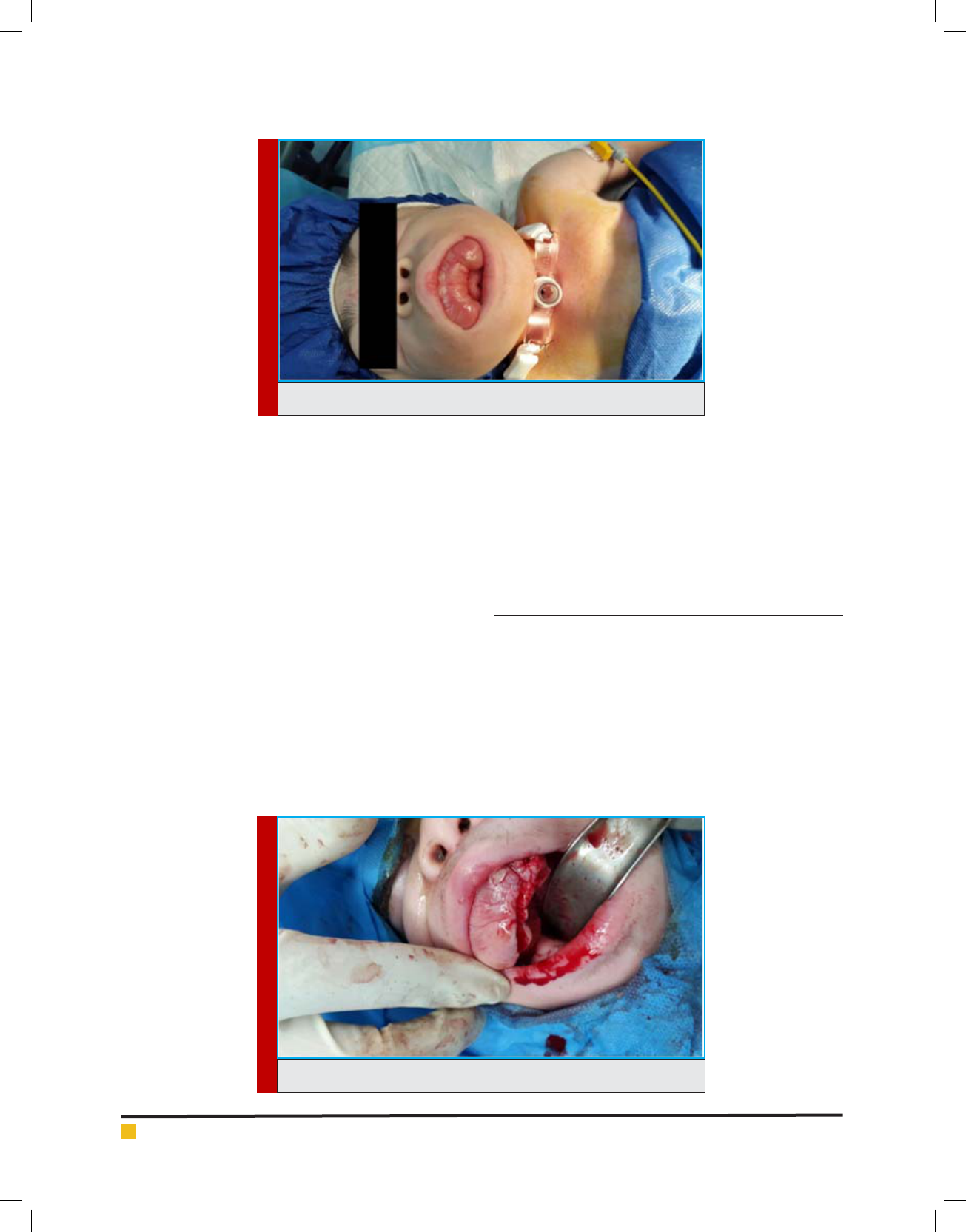
The 3D computed tomography (CT) scan showed displaced
position of teeth, hypoplastic condyle and dysmorpho-
genic cranio-maxillofacial skeleton (Figure 2, 3). An
FIGURE 1. Severe gingival overgrowth is
obvious in clinical examination.
FIGURE 2. 3D CT scan of the patient in frontal and sagittal
view, malposition teeth and skeletal open-bite are
considerable.
BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS THE ORAL AND MAXILLOFACIAL MANIFESTATION AND SURGICAL CONSIDERATION 183
Farnoosh Mohammadi and Iman Tavakoli
FIGURE 3. Tracheostomy was carried out to provide a secured air way.
FIGURE 4. Soft tissue removal for 1 quadrant of upper jaw.
elective tracheostomy was performed was done under
general anesthesia (Figure 4). Skin stiffness, rigidity of tra-
chea and narrowing of air passage during procedure were
considerable. Short neck and small stature made the pro-
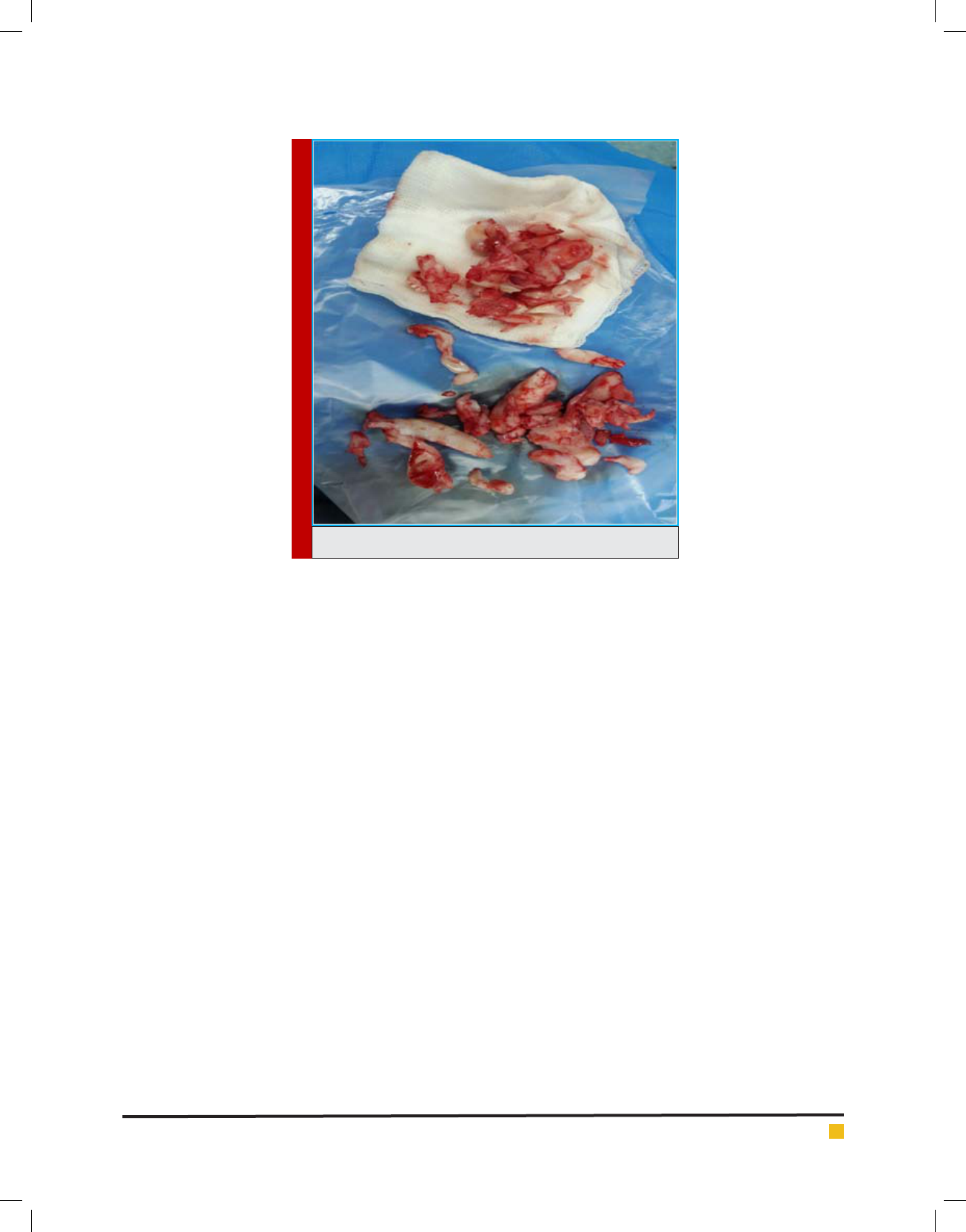
cedure more dif cult. Gingivectomy was done in a large
scale for each quadrant (Figure 5, 6).
SURGERY PROCEDURE
The blade no.15 followed by the blade no.10 was applied
for the last three quadrants due to thickness and inelas-
ticity of gingival tissue. Most of the incisor teeth were
infra-erupted because of gingival overgrowth and the
other teeth were impacted. Some teeth contained large
and thick follicle like a dentigerous cyst. Malposition-
ing of impacted teeth, underdeveloped maxillary sinus,
taurodontism and thin cortical bone in buccal area of
mandibular molar were revealed during surgical explo-
ration. After gingivectomy, all the teeth were extracted
and the bone was shaved and reshaped. After opera-
tion, the patient was admitted to the intensive care unit
(ICU) and intubated. 3 weeks after surgery when she was
ready to wean from mechanical ventilation, extubation
was carried out but a few minutes after extubation, oxy-
gen saturation decreased, she became cyanotic and the
ICU staffs were not able to re-intubate her because of
bronchospasm.
DISCUSSION
The MPS type VI is an inborn metabolic and autosomal
recessive disease caused by mutations in the arylsulfa-
tase B gene (Alpoz et al. 2006). A mutation in chro-
mosome 5 is responsible to this syndrome (Baehner et
al. 2005). This enzyme is called N-acetyl galactosamine
4-sulfatase which plays an important role in metabo-
lism of GAG (Malm et al. 2007).
This gene is required
for the degradation of dermatan sulfate and de ciency
leads to cumulation of undegraded or partially degraded
184 THE ORAL AND MAXILLOFACIAL MANIFESTATION AND SURGICAL CONSIDERATION BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS
Farnoosh Mohammadi and Iman Tavakoli
BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS THE ORAL AND MAXILLOFACIAL MANIFESTATION AND SURGICAL CONSIDERATION 185
mucopolysaccharides which results in large lips and
thick gingival tissue and corneal opacities (Alpoz et al.
2006). It is reported the frequency of the MPS type VI
ranges from 1:100 000 births to 1:1300 000 in various
populations (Meikle et al. 1999).
Diagnosis of the MPS type VI is based on clinical
manifestation and paraclinical evaluation. The cardiac
disease is common phenomenon in these patients. Based
on the previous reports in a population of 28 patients
with MPS type VI mitral valve stenosis was the most
common cardiac problem, however, patient showed a
normal cardiac function (Azevedoet al. 2004). Pulmo-
nary diseases are other important problems in this syn-
drome. Nasopharyngeal space is decreased due to verti-
cal facial skeleton overgrowth and deposition of GAG
which may lead to respiratory dif culty (Fonseca et al.
2014). Special consideration should be taken on airway
management in these patients during general anesthesia
because of dif cult intubation. Tracheostomy is recom-
mended in severe cases. Short and in exible neck, nar-
row trachea and tracheomalacia can make this procedure
more dif cult. Special note should be focused on extu-
bation in these cases. Although ophthalmological and
hearing problems are frequently seen in these patients,
in the current study, our patient had none of these prob-
lems. Severe skeletal problems and growth retardation
were observed in this case. She had bilateral xed exed
hips and also was not able to extend the neck or the
arms. Very small stature and low weight (7.8 kg) with
age of 4 years and 6months were remarkable.
Craniofacial dysmorphologyare characteristic in Mar-
oteaux Lamy syndrome. Large head, coarse facial appear-
ance, bushy eyebrow, deep nasojugal groove and hyper-
telorism are the main of these features. Dolichocephalic
growth pattern causes todecreasenasopharyngeal space
and leads do dyspnea (Fonseca et al. 2014). Also, under-
developed condyle, macroglossia and huge gingival
bromatosis were contributed to open bite. Magnetic
resonance imaging revealed cartilage proliferation in
the retrodiscal tissue and anterior disk displacement
(Cavaleiro et al. 2013). Several dental problems such as
impacted teeth, buccally inclined teeth, cyst-like follicle,
malposition teeth and taurodontism are reported (Alpoz
et al. 2006). In this case, extraction of most of the teeth
was inevitable. Huge gingival bromatosis and follicu-
lar formation around the crown of the teeth had made
the eruption of the teeth impossible. It is reported early
enzyme replacement therapy in siblings have bene cial
effects on facial morphology, joint mobility and cardiac
valve pathology (McGill et al. 2010).
In conclusion, despite Maroteaux-Lamy syndrome is
not encountered routinely in dental practice, such cases,
if properly managed, will maintain their oral and gen-
eral health for the remainder of their lives. So, this stud-
ied revealed the importance of screening in newborns
but surgical treatment in many cases is required.
FIGURE 5. Gingivectomy and tooth removal with attached cyst.

Farnoosh Mohammadi and Iman Tavakoli
186 THE ORAL AND MAXILLOFACIAL MANIFESTATION AND SURGICAL CONSIDERATION BIOSCIENCE BIOTECHNOLOGY RESEARCH COMMUNICATIONS
REFERENCES
Alpoz A, Coker M, Celen E, Ersin NK, Gokcen D, Diggelenc
OP, Jan G, Huijmansc M (2006). The oral manifestations of
Maroteaux-Lamy syndrome (mucopolysaccharidosis VI):
A case report. Oral Surg Oral Med Oral Pathol Oral Radiol
Endod.101:632-7.
Azevedo AC, Schwartz L IV, Kalakun L Brustolin S, Burin MG,
Beheregaray AP, Leistner S, Giugliani C, Rosa M, Barrios P,
Marinho D, Esteves P, Valadares E, Boy R, Horovitz D, Mabe P,
da Silva LC, de Souza IC, Ribeiro M, Martins AM, Palhares D,
Kim CA, Giugliani R (2004). Clinical and biochemical study of
28 patients with mucopolysaccharidosis type VI. Clin Genet.
66:208–13.
Baehner F, Schmiedeskamp C, Krummenauer F, Miebach E,
Bajbouj M, Whybra C, Kohlschütter A, Kampmann C, Beck M
(2005). Cumulative incidence rates of the mucopolysacchari-
doses in Germany. J Inherit Metab Dis. 28:1011-17.
Baum H, Dodgson KS, Spencer B (1959). The assay of aryl-
sulphatase A and B in human urine. Clin Chim Acta;4:453-5.
Cavaleiro RM, Pinheiro Md, Pinheiro LR, Tuji FM, Feio Pdo S,
de Souza IC, Feio RH, de Almeida SC, Schwartz IV, Giugliani
R, Pinheiro JJ, Santana-da-Silva LC (2013). Dentomaxillofa-
cial manifestations of mucopolysaccharidosis VI: clinical and
imaging ndings from two cases, with an emphasis on the
temporomandibular joint.116: 141-8.
Fonseca FR, de Santana Sarmento DJ, Vasconcelos Medeiros
PF, Diniz DN, dos Santos MT (2014). Patients with mucopoly-
saccharidosis have tendencies towards vertical facial growth. J
Oral Maxillofac Surg.72: 2539-46.
Litjens T, Baker EG, Beckmann KR, Morris CP, Hopwood JJ,
Callen DF (1989). Chromosomal localization of ARSB, the gene
for human N-acetylgalactosamine-4-sulphatase. Hum Genet.
82:67-8.
Malm G, Lund AM, Mansson JE, Heiberg A (2008). Mucopoly-
saccharidoses in the Scandinavian countries: incidence and
prevalence. Acta Paediatr. 97:1577-81.
Maroteaux P, Leveque B, Marie J, Lamy M (1963). A new
dysostosis with urinary elimination of chondroitin sulfate B.
Presse Med. 71:1849–52.
McGill JJ, Inwood AC, Coman DJ, Lipke ML, de Lore D, Swie-
dler SJ, Hopwood JJ (2010). Enzyme replacement therapy for
mucopolysaccharidosis VI from 8 weeks of age--a sibling con-
trol study. Clin Genet. 77:492-8.
Meikle PJ, Hopwood JJ, Clague AE, Carey WF (1999). Preva-
lence of lysosomal storage disorders. JAMA. 281:249-54.
Neufeld EF, Muenzer J (1995). The mucopolysaccharidoses. The
metabolic and molecular bases of inherited disease. New York:
McGraw-Hill. 2465-94.
Roberts MW, Barton NW, Constantopoulos G, Butler DP, Dona-
hue AH (1984). Occurrence of multiple dentigerous cysts in
a patient with the Maroteaux-Lamy syndrome (mucopoly-
saccharidosis, type VI). Oral Surg Oral Med Oral Pathol Oral
Radiol Endod. 58:169-75.
Valayannopoulos V, Nicely H, Harmatz P, Turbeville S (2010).
Mucopolysaccharidosis VI, Orphanet. J Rare Dis. 5:5–20.
Wiedemann HR, Kunze J, Grosse FR, Dibbern H (1992). An
atlas of clinical syndromes (a visual aid to diagnosis). Ayles-
bury: Wolfe Publishing Co. p. 58.